Abstract
BACKGROUND:
Interventions for obese adolescents in real-world, clinical settings need to be evaluated because most weight management care occurs in this context.
OBJECTIVES:
To determine whether a lifestyle intervention that includes motivational interviewing and cognitive behavioural therapy (Health Initiatives Program [HIP]) leads to weight management that is superior to a similar lifestyle intervention (Youth Lifestyle Program [YLP]) that does not include these techniques; and to determine whether the HIP and YLP interventions are superior to a wait list control (WLC) group.
METHODS:
Obese adolescents were randomly assigned to a YLP (n=15), HIP (n=17) or WLC (n=14) group. The YLP and HIP were 16-session, one-on-one interventions. The primary outcome was the percentage change of body mass index z-score.
RESULTS:
Completers-only analyses revealed 3.9% (YLP) and 6.5% (HIP) decreases in the percentage change of body mass index z-score compared with a 0.8% (WLC) increase (P<0.001). Levels of attrition did not differ among groups, but were relatively high (approximately 20% to 40%).
CONCLUSION:
Lifestyle interventions delivered in a real-world, clinical setting led to short-term improvements in the obesity status of adolescents.
Keywords: Adolescent, Intervention, Obesity
Abstract
HISTORIQUE :
Il faut évaluer les interventions auprès des adolescents obèses en milieu clinique réel parce que la plupart des soins de prise en charge de l’obésité se produisent dans ce contexte.
OBJECTIFS :
Déterminer si une intervention sur le mode de vie, incluant une entrevue motivationnelle et une thérapie cognitivocomportementale (Health Initiatives Program [HIP]), favorise une gestion du poids plus efficace qu’une intervention similaire sur le mode de vie (Youth Lifestyle Program [YLP]) qui exclut ces techniques; et déterminer si les interventions HIP et YLP sont plus efficaces qu’un groupe témoin sur une liste d’attente (TLA).
MÉTHODOLOGIE :
Les adolescents obèses ont été répartis au hasard entre un groupe d’YLP (n=15), de HIP (n=17) ou de TLA (n=14). Les groupes d’YLP et de HIP ont reçu 16 séances d’interventions individualisées. L’issue primaire était le changement en pourcentage de l’écart réduit d’indice de masse corporelle.
RÉSULTATS :
Les analyses de ceux qui avaient terminé l’étude ont révélé des diminutions de 3,9 % (YLP) et de 6,5 % (HIP) du changement en pourcentage de l’écart réduit d’indice de masse corporelle, par rapport à une augmentation de 0,8 % (TLA) (P<0,001). Les taux d’attrition, relativement élevés, demeuraient les mêmes entre les groupes (environ 20 % à 40 %).
CONCLUSION :
Les interventions sur le mode de vie offertes en milieu clinique réel entraînent une amélioration à court terme de l’état d’obésité des adolescents.
Approximately two million Canadian boys and girls are overweight or obese (1,2), which places them at increased risk for several chronic diseases. Overweight and obese children referred for weight management often exhibit suboptimal lifestyle behaviours (3) – a finding that highlights the potential for interventions to promote healthier habits. These observations, along with recent clinical practice guidelines (4) and best practice recommendations (5), underscore the importance of healthy lifestyle behaviours as the cornerstone of paediatric weight management. Even in situations for which more intensive therapy may be indicated, nutrition, physical activity and behavioural counselling remain foundational strategies (6,7).
Evidence supporting the successful treatment of paediatric obesity is primarily derived from group-based interventions, which tend to be more efficacious (8) and cost effective (9), and reduce attrition (10) versus one-on-one care. Alternately, one-on-one care is more feasible, appropriate (in some situations) and common in many Canadian paediatric weight management clinics (11). A key limitation of the aforementioned research is that most studies included community-based volunteers – a situation that differs for many paediatricians who refer obese boys and girls to multidisciplinary weight management clinics. Recently, the Canadian Institutes of Health Research (CIHR) emphasized the value of integrating research into practice-based settings as a way to enhance health services for Canadians (12). We believe that offering one-on-one interventions in clinics that provide paediatric weight management care and conduct applied research in real-world environments can inform health service delivery in Canada. Because there are a limited number of evaluations of one-on-one weight management interventions for adolescents, other areas of intervention research can provide guidance.
The Diabetes Prevention Program (DPP [13]), a multicentre clinical trial designed to prevent type 2 diabetes in adults, demonstrated that a lifestyle behavioural intervention delivered primarily through one-on-one counselling delays the onset of type 2 diabetes through weight management and behavioural changes (13,14). A developmentally appropriate version of the intervention may be well received by obese adolescents; creating an intervention that includes personalized goal setting and problem solving would also align with current recommendations. Accordingly, client-centred counselling approaches, such as motivational interviewing (15) and cognitive behavioural therapy (16), have become increasingly popular in obesity research (17,18). Evidence supporting motivational interviewing and cognitive behavioural therapy in weight management is predominantly adult oriented; however, the principles underlying these approaches (ie, addressing ambivalence, and increasing awareness of thoughts and feelings regarding lifestyle habits) are well suited to adolescents given their increasing capacity for introspection. The purpose of the present pilot study was to use the DPP as a starting point to develop two alternative treatment models (discussed below) for obese adolescents that were compared with a wait list control (WLC) group. We hypothesized that a lifestyle intervention that includes motivational interviewing and cognitive behavioural therapy would lead to superior weight management versus a similar lifestyle intervention that does not include these counselling techniques. We also hypothesized that both interventions would be superior to a WLC group. Because the present research was conducted in a multi-disciplinary paediatric weight management clinic, we also documented process-related outcomes including treatment initiation, attrition, feasibility and acceptability.
METHODS
Study design
The present pilot, randomized controlled trial was conducted in a weight management clinic in Edmonton, Alberta. Participants were enrolled in the study from January 2006 to September 2007, and were eligible if they were 13 to 17 years of age and possessed a body mass index (BMI) at the 85th percentile or greater (19). Preintervention testing occurred over two separate days (10 to 14 days apart) within four weeks of starting the treatment phase, which lasted 16 to 20 weeks. Postintervention testing was identical to the preintervention procedures; all measurements were completed within four weeks of ending the treatment phase. No follow-up data beyond the postintervention time point were presented. The primary outcome variable for the study was the percentage change (%Δ) in BMI z-score, and sample size was based on previous intervention studies with similar study designs and outcomes (20,21). The aim was to enrol 54 participants (n=18 per group). Several secondary outcome variables were also measured including anthropometry (body weight, BMI, BMI percentile and waist circumference [WC]), lifestyle-related behaviours (dietary intake, physical activity and aerobic fitness) and metabolic risk factors (blood cholesterol, insulin, glucose and blood pressure). Before beginning preintervention testing, a child psychiatrist or psychologist completed 45 min to 60 min standardized assessments to gauge whether any psychosocial or familial factors precluded potential participants from study inclusion. Based on these assessments, all boys and girls were deemed appropriate. The study biostatistician (CAA), who had no contact with either participants or intervention providers, performed all randomization and intervention allocation tasks. The research team and participants (but not intervention providers) were blinded to group allocation. Parents and adolescents completed informed consent and assent processes, respectively, and the University of Alberta/Alberta Health Services Health Research Ethics Board (Edmonton) approved the research.
Outcome measurements
Demographic data were provided by parental report. Height and weight were measured; BMI, BMI percentile and BMI z-score were subsequently calculated. WC was measured at the narrowest point between the xyphoid process and the iliac crest. Dietary intake was measured using a four-day food record (three weekdays plus one weekend day) and data were subsequently analyzed using a nutrition software program. Pedometers assessed physical activity over the same four-day period, and these data were supplemented by a seven-day physical activity recall survey that assessed moderate-to-vigorous physical activity (22). Information regarding sedentary activity (screen time) was also retrieved. Aerobic fitness was determined on a treadmill using a walking protocol (23). A fasting blood sample was collected to measure total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, insulin and glucose. Systolic and diastolic blood pressure were measured manually.
Intervention descriptions
Participants were randomly assigned to one of three intervention groups: Youth Lifestyle Program (YLP), Healthy Initiatives Program (HIP) or WLC. Key similarities and differences between YLP and HIP interventions are summarized in Table 1. Similar to the DPP (13), both interventions were 16 to 20 weeks in duration, and included content regarding nutrition, physical activity, sedentary activity, self-esteem and relapse prevention; they also included weekly case conferences for clinicians, pedometers for physical activity tracking and self-monitoring strategies. All sessions included (sequentially) rapport building, review of the previous session (content, lifestyle behaviour monitoring and goal setting), new curriculum content, session summary, and goal setting and planning for the upcoming week. The critical difference was that, unlike YLP, HIP included counselling and communication strategies consistent with motivational interviewing and cognitive behavioural therapy, which catered to adolescents’ motivations and readiness to change. This enabled clinicians to adapt communication and educational strategies based on participants’ motivation and stage of change. Leaders encouraged adolescents to discuss their thoughts and feelings regarding the HIP lifestyle goals to help teenagers set personal goals and address factors that could enable or impede cognitive and behavioural changes. Given concerns regarding unhealthy weight management practices during adolescence (24), both YLP and HIP did not include prescriptive energy intake or expenditure goals. Others have referred to similar lifestyle behavioural interventions as ‘nondiet’ because they promote the health benefits of lifestyle behaviour changes (25).
TABLE 1.
Overview of the similarities and differences between weight management interventions for obese adolescents: The Youth Lifestyle Program (YLP) versus the Healthy Initiatives Program (HIP)
| Similarities | Differences |
|---|---|
|
|
The curricula for YLP and HIP were developed by a multidisciplinary team. An external review panel with expertise in obesity and intervention development critiqued the interventions, and modifications were made based on their feedback before intervention delivery. Participants received intervention manuals that included age-appropriate information and educational resources. Interventions were delivered by health professionals (RD and RN) who completed two days of training that included both theoretical and practical aspects of motivational interviewing, cognitive behavioural therapy and behaviour change principles. Participants randomly assigned to the WLC group attended a single one-on-one counselling session and received educational materials (26,27). At the end of the intervention period, individuals in the WLC group were offered the choice of participating in either the YLP or HIP intervention.
Parental involvement is recommended when treating paediatric obesity (4,28), but the extent to which parents should be included is unclear. YLP and HIP were designed to capitalize on adolescents’ independence by focusing curriculum content and coaching strategies on the adolescents themselves. Parents of adolescents in YLP and HIP were invited to attend three parent-only sessions to learn about how they could support their teenagers. No parent-directed intervention was delivered to the WLC group.
Statistical analyses
Baseline differences between those who did (completers) and did not (noncompleters) attend postintervention measurements were explored using independent samples t tests. Intervention groups were compared pre-to-postintervention according to the %Δ in anthropometric, behavioural and metabolic risk factor variables using one-way ANOVA with Bonferroni post hoc comparisons; if assumptions for normality were not satisfied, comparisons were conducted using the nonparametric Kruskal-Wallis test with Mann-Whitney U test post hoc comparisons. Completers-only and intention-to-treat analyses were conducted. Covariate analyses were used to control for potential group differences (ie, age) at baseline. Group differences in proportions were examined using the χ2 statistic. Differences between groups were considered to be significant at P<0.05. Analyses were performed using SPSS version 14.0 (IBM Corporation, USA).
RESULTS
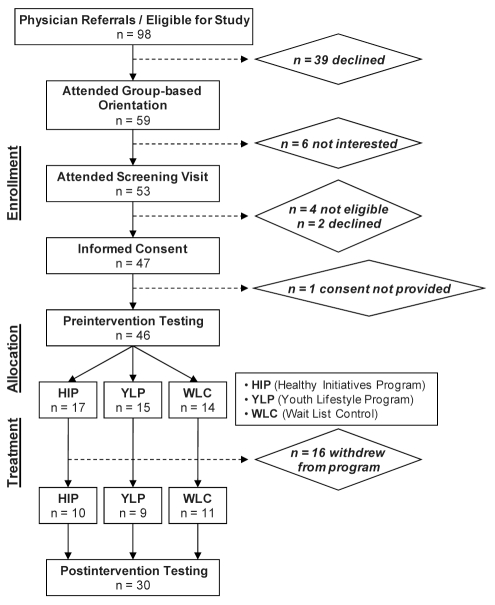
As shown in Figure 1, of the 98 possible study participants, 46 progressed through the enrollment steps to complete preintervention testing before group allocation. The main issue that limited the study sample size was the decision by many families (n=39) to not follow up after being referred for weight management. The recruitment goal (n=18 per group) could not be achieved because of logistical issues and resource limitations.
Figure 1).
Participant flow through the study stages
The demographic characteristics of adolescents are presented in Table 2. All participants were from middle- to high-income families. The YLP group was older than the HIP (by 1.6 years; P=0.002) and WLC (by 1.4 years; P=0.01) groups, and more sexually mature than the HIP group (P=0.01). Baseline differences between intervention completers (n=30) and non-completers (n=16) were examined. Compared with completers, noncompleters had higher low-density lipoprotein cholesterol levels (2.23±0.7 mmol/L versus 2.80±0.44 mmol/L, respectively; P=0.006). No other group differences were significant.
TABLE 2.
Demographic characteristics of the study groups at baseline
| YLP (n=15) | HIP (n=17) | WLC (n=14) |
P |
||||
|---|---|---|---|---|---|---|---|
| For trend | YLP versus HIP | HIP versus WLC | YLP versus WLC | ||||
| Sex, male:female, n | 4:11 | 7:10 | 7:7 | 0.4 | – | – | – |
| Age, years | 16.2±1.3 | 14.6±1.3 | 14.8±1.2 | 0.001* | 0.002* | 1.0 | 0.01* |
| Tanner stage | |||||||
| Pubic hair | 4.5±0.9 | 3.6±1.2 | 4.2±0.9 | 0.04* | 0.01* | 0.08 | 0.2 |
| Breasts/gonads | 4.4±0.9 | 3.5±1.2 | 3.8±1.0 | 0.06 | – | – | – |
| Ethnicity, Caucasian:non-Caucasian, n | 11:4 | 14:3 | 14:0 | 0.1 | – | – | – |
| Family history of type 2 diabetes, yes:no, n | 7:8 | 8:9 | 7:7 | 1.0 | – | – | – |
Data presented as mean ± SD unless otherwise indicated.
P<0.05. HIP Healthy Initiatives Program; WLC Wait List Control; YLP Youth Lifestyle Program
Attrition timing varied within each group, but did not differ between groups (Table 3). While approximately 40% of participants dropped out of YLP and HIP, completers in both groups had a high degree of participation; all 16 sessions were attended by 15 of 19 participants, and at least 14 sessions were attended by 18 of 19 adolescents. Parental attendance at the group sessions did not differ between groups.
TABLE 3.
Summary of intervention attendance data
| HIP | YLP | WLC* | P | |
|---|---|---|---|---|
| Preintervention sample size, n | 17 | 15 | 14 | 0.2 |
| Postintervention sample size, n (%) | 10 (41.8) | 9 (40.0) | 11 (21.4) | 0.5 |
| Week of drop out, mean (range) | 7.4 (1–12) | 9.2 (2–15) | – | 0.5 |
| Number of sessions attended by intervention completers, mean (range) | 15.9 (15–16) | 15.1 (11–16) | – | 0.2 |
All participants in the wait list control (WLC) group attended one counselling appointment with an exercise specialist and registered dietitian; three participants did not complete postintervention testing. HIP Healthy Initiatives Program; YLP Youth Lifestyle Program
Based on completers-only analyses, the pattern of %Δ of BMI z-score was similar to the changes for body weight, BMI and BMI percentile; these indexes improved in the YLP and HIP groups only (Table 4). Although the %Δ in WC did not achieve significance, changes were in the expected direction. Aside from group differences in the %Δ of aerobic fitness (YLP and HIP greater than WLC), significant differences in lifestyle behaviours and metabolic risk factors did not emerge before or after comparisons were adjusted for covariates. However, the %Δ in steps/day approached significance with YLP and HIP greater than WLC (P=0.07).
TABLE 4.
Anthropometric variables at preintervention and postintervention, and the percentage change from pre-to-postintervention for completers only
| Preintervention | Postintervention | Percentage change |
P |
||||
|---|---|---|---|---|---|---|---|
| For trend | YLP vs HIP | HIP vs WLC | YLP vs WLC | ||||
| Height, cm | |||||||
| YLP (n=9) | 168.4 (163.3 to 173.6) | 169.3 (163.7 to 174.9) | 0.5 (0.1 to 0.9) | 0.1 | – | – | – |
| HIP (n=10) | 167.5 (162.7 to 172.4) | 169.3 (164.4 to 174.3) | 1.1 (0.6 to 1.6) | ||||
| WLC (n=11) | 169.3 (166.0 to 172.7) | 170.4 (166.8 to 174.0) | 0.6 (0.2 to 1.1) | ||||
| Weight, kg | |||||||
| YLP (n=9) | 104.4 (89.5 to 119.3) | 103.3 (88.4 to 118.2) | −1.0 (−4.4 to 2.4) | 0.009 | 0.8 | 0.004 | 0.025 |
| HIP (n=10) | 98.1 (86.4 to 109.8) | 97.2 (84.2 to 110.2) | −1.1 (−4.0 to 1.7) | ||||
| WLC (n=11) | 106.4 (96.2 to 116.7) | 109.9 (99.1 to 120.7) | 3.2 (2.0 to 4.4) | ||||
| BMI, kg/m2 | |||||||
| YLP (n=9) | 36.6 (32.5 to 40.8) | 35.9 (31.9 to 39.9) | −1.9 (−5.0 to 1.1) | 0.002 | 1 | 0.002 | 0.03 |
| HIP (n=10) | 34.8 (31.6 to 38.0) | 33.7 (30.4 to 37.1) | −3.3 (−5.6 to −1.0) | ||||
| WLC (n=11) | 37.1 (33.8 to 40.4) | 37.9 (34.3 to 41.4) | 2.0 (0.4 to 3.6) | ||||
| BMI percentile | |||||||
| YLP (n=9) | 98.7 (98.1 to 99.4) | 98.4 (97.5 to 99.2) | −0.4 (−0.7 to −0.0) | 0.005 | 0.8 | 0.001 | 0.02 |
| HIP (n=10) | 98.2 (96.6 to 99.9) | 97.2 (94.0 to 100.3) | −1.1 (−2.8 to 0.5) | ||||
| WLC (n=11) | 99.0 (98.4 to 99.7) | 99.0 (98.4 to 99.6) | 0.0 (−0.1 to 0.2) | ||||
| BMI z-score | |||||||
| YLP (n=9) | 2.33 (2.09 to 2.57) | 2.24 (1.97 to 2.51) | −3.9 (−6.8 to −1.0) | 0.001 | 0.7 | 0.001 | 0.006 |
| HIP (n=10) | 2.28 (1.99 to 2.57) | 2.16 (1.80 to 2.52) | −6.5 (−11.8 to −1.2) | ||||
| WLC (n=11) | 2.43 (2.21 to 2.65) | 2.45 (2.22 to 2.68) | 0.8 (−0.5 to 2.1) | ||||
| Waist circumference, cm | |||||||
| YLP (n=9) | 104.6 (94.9 to 114.3) | 102.3 (92.8 to 111.8) | −2.1 (−4.6 to 0.4) | 0.3 | – | – | – |
| HIP (n=10) | 102.8 (95.3 to 110.4) | 102.0 (91.2 to 112.8) | −1.2 (−5.2 to 2.9) | ||||
| WLC (n=11) | 109.8 (102.7 to 116.9) | 110.6 (102.3 to 119.0) | 0.6 (−1.4 to 2.6) | ||||
Data presented as mean (95% CI). Group comparisons for height, weight, body mass index (BMI) and waist circumference are adjusted for age; BMI percentile and BMI z-score variables are corrected for age and sex. HIP Healthy Initiatives Program; vs Versus; WLC Wait List Control; YLP Youth Lifestyle Program
Intention-to-treat analyses showed more conservative group differences, with significant main effects for the %Δ of BMI z-score (F=3.8, P=0.03) and %Δ of BMI (F=6.3, P=0.004) only. Post hoc analyses revealed that WLC increased the %Δ of BMI z-score (0.65±1.76) versus HIP (−3.81±6.55). Although YLP decreased in the expected direction (−2.33±3.45), YLP and WLC were not different in the %Δ of BMI z-score (P=0.2). WLC also increased the %Δ of BMI (1.6±2.3), while YLP (−1.2±3.1) and HIP (−1.9±2.9) decreased. Aerobic fitness was no longer different between groups when intention-to-treat analyses were completed. Similar to the analyses for the completers-only group, lifestyle behaviours and metabolic risk factors did not differ between groups.
DISCUSSION
Several multidisciplinary clinics have been established in Canada in recent years to provide paediatric weight management care (11). This trend highlights the importance of deriving evidence from real-world clinical settings because most of what we know regarding paediatric weight management is based on efficacy studies with community-based volunteers (28) and because individuals referred for weight management tend to be less healthy than their nonclinical peers (29). Findings from the present pilot study demonstrate that challenges such as low participation and high intervention attrition levels can influence the effectiveness of weight management care for obese adolescents.
Both YLP and HIP demonstrated that one-on-one lifestyle coaching interventions can improve some short-term measures of obesity in adolescents. The magnitude of change in BMI z-score in the YLP and HIP groups was modest but consistent with recommendations (5). YLP and HIP were designed to improve lifestyle behaviours, but no significant differences were noted in diet and physical activity. As well, despite showing improvements in anthropometric measures, we did not observe concurrent changes in metabolic risk. We noted favourable patterns of change in systolic blood pressure, fasting insulin and triglycerides – measures that are often elevated in obese boys and girls (30); however, none of these changes achieved significance. The small sample size of the present study and the within-group variability likely explain our inability to detect group differences in these variables. In addition, beyond any short-term effects, it is possible that either YLP or HIP will prove to be the superior intervention over the long term – a finding that is not immediately evident.
Expert recommendations endorse the use of patient-centred, motivation-based approaches to weight management care (4,5). The HIP intervention included motivational interviewing and cognitive behavioural therapy to help participants address ambivalence and barriers to behaviour change as well as incorporate specific problem-solving techniques; however, treatment effects were not different from the YLP intervention, which simply emphasized techniques such as goal setting and self-monitoring. It is possible that the use of motivational interviewing and cognitive behavioural therapy for promoting behaviour change are not universally beneficial for all obese individuals (31). These approaches may be best applied when self-efficacy for making lifestyle changes is low or at later stages of an intervention after setbacks have occurred. Furthermore, testing different weight management approaches in expertise-based trials, whereby clinicians select their preferred intervention approach, would capitalize on individual skills and training (32) that tend to vary within and between disciplines.
Other variables may also explain the similar short-term benefits (in some outcomes) accrued by participants in the YLP and HIP interventions compared with the WLC group. For example, contact frequency has a positive influence on weight management success (33). The YLP and HIP groups had more than 20 clinical encounters, which included their intervention sessions as well as pre- and postintervention testing. Comparatively, adolescents in the WLC group had five to seven clinical encounters. In our clinic, we have cultivated a supportive, nonjudgemental setting to help families make healthy lifestyle changes. If participants received this support through our clinical environment, and benefitted from the structured curriculum and self-monitoring built into both interventions, it is possible that these benefits prevented us from differentiating between the YLP and HIP intervention effects.
Intention-to-treat analyses have become increasingly popular in weight management research to minimize study bias and retain methodological rigour (34,35), and were included in the present report; however, a qualification is required. In the present study, participants were in mid-to-late puberty; therefore, developmental height and weight increases were expected. Using intention-to-treat and data imputation to include participants who dropped out before study completion, we carried forward the last available measurements (preintervention) to the postintervention time point. We believe that this may have provided a somewhat misleading estimate of the intervention effects. With intention-to-treat analyses, imputing noncompleters’ baseline data confers some degree of treatment success because they appear to be weight stable during the intervention period, which is a laudable treatment goal (5). However, in the absence of an intervention or with poor intervention adherence, weight gain would be expected over the study period, and its trajectory would vary according to developmental stage. Based on these issues, we analyzed our data using both completers-only and intention-to-treat techniques.
Several research challenges and clinically relevant observations emerged from the present study. The long-term maintenance of weight loss is the true benchmark of weight management success. While our data do not meet this standard, we provide evidence that YLP and HIP are feasible in the short term. A lack of long-term follow-up data limits our ability to comment on the sustainability of weight management or lifestyle behaviour changes. Effective retention strategies for children with chronic illnesses may provide insight into how best to remain engaged with obese adolescents and their families because attrition is common in paediatric weight management (36). The level of attrition of our study was similar to other weight management interventions delivered in an outpatient setting (37) and highlights what happens under real-world conditions. While issues regarding attrition have been examined to a limited degree in the treatment of paediatric obesity (38–40), none have explored families’ reasons for lack of engagement after being referred for multidisciplinary care. Given the high number of adolescents who failed to initiate care, gaining a better understanding of factors that explain why some families initiate care while others do not represents a knowledge gap. Intra- and/or interpersonal factors (ie, depression or anxiety) may underlie the lack of engagement and initiation of some individuals in weight management care. While our mental health professionals’ screening assessment provided a clinical perspective of participants at baseline, the absence of validated surveys to measure any psychosocial constructs precluded us from exploring these factors in detail.
When we performed the present study, our clinic offered the YLP and HIP interventions exclusively; therefore, the 13 adolescents who attended our group-based orientation session, but did not continue on to complete preintervention testing, may have benefitted from alternative treatments. As our clinic evolved, we developed additional therapeutic options (ie, psychological counselling and personal fitness training) to complement our structured interventions, which were enabled by funding and infrastructure – two issues that can limit program growth and development (11,36). We were also interested in the experiences of our clinicians who delivered YLP and HIP, as well as the adolescents who completed the interventions. Anecdotally, both groups found YLP and HIP to be acceptable, but recommended adding interactive group-based activities. In our experience, many boys and girls referred for weight management have small social networks; therefore, creating an opportunity for adolescents to interact with peers may satisfy adolescents’ desire for fun, social interactions while achieving our clinical aims to minimize intervention attrition, maintain family engagement and improve health outcomes.
CONCLUSION
With the high prevalence of paediatric obesity in Canada, there is an urgent need to deliver and evaluate health services for weight management. Our study showed that structured interventions can have a positive, albeit modest, impact on weight management for some obese boys and girls. However, to best support obese adolescents, initiatives to optimize the initiation of care, develop flexible, multidisciplinary treatment models and reduce intervention attrition are required. Conducting this research in real-world settings will help to build on existing weight management evidence and generate information that will be most meaningful to paediatricians and other clinicians.
Acknowledgments
The authors thank all of the adolescents and families who participated in this study, as well as the clinicians at the Pediatric Centre for Weight and Health (Stollery Children’s Hospital, Edmonton) for their clinical and administrative support. Dr Lonnie Zwaigenbaum provided a critique of an earlier version of this manuscript; his time and feedback are sincerely appreciated. Statistical analyses were supported by the Women and Children’s Health Research Institute (Edmonton). Funding for this research was provided through an Establishment Grant (awarded to GDCB) by the Alberta Heritage Foundation for Medical Research (AHFMR) and the Alberta Health Services’ Weight Wise program. GDCB was supported by a Population Health Investigator Award from AHFMR and a New Investigator Award from the CIHR. MSN was supported by a Career Development Award from the Canadian Child Health Clinician Scientist Program (a CIHR-funded program). RCP was supported by a Health Scholar Award from AHFMR and an Applied Public Health Chair from CIHR. MIG was supported by the Dr Robert C and Veronica Atkins Endowed Chair in Childhood Obesity and Diabetes.
Footnotes
CONFLICTS OF INTEREST: The authors have no conflicts of interest to declare.
REFERENCES
- 1.Shields M. Overweight and obesity among children and youth. Health Rep. 2006;17:27–42. [PubMed] [Google Scholar]
- 2.Statistics Canada . Annual Demographic Statistics, 2005. Ottawa: Statistics Canada; 2006. [Google Scholar]
- 3.Ball GD, Lenk JM, Barbarich BN, et al. Overweight children and adolescents referred for weight management: Are they meeting lifestyle behaviour recommendations? Appl Physiol Nutr Metabol. 2008;33:936–45. doi: 10.1139/H08-088. [DOI] [PubMed] [Google Scholar]
- 4.Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E. Canadian clinical practice guidelines on the management and prevention of obesity in adults and children. CMAJ. 2006;2007;176:S1–13. doi: 10.1503/cmaj.061409. (Summary) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S254–88. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- 6.Sinha A, Kling S. A review of adolescent obesity: Prevalence, etiology, and treatment. Obes Surg. 2009;19:113–20. doi: 10.1007/s11695-008-9650-4. [DOI] [PubMed] [Google Scholar]
- 7.Inge TH, Krebs NF, Garcia VF, et al. Bariatric surgery for severely overweight adolescents: Concerns and recommendations. Pediatrics. 2004;114:217–23. doi: 10.1542/peds.114.1.217. [DOI] [PubMed] [Google Scholar]
- 8.Wilfley DE, Tibbs TL, Van Buren DJ, Reach KP, Walker MS, Epstein LH. Lifestyle interventions in the treatment of childhood overweight: A meta-analytic review of randomized controlled trials. Health Psychol. 2007;26:521–32. doi: 10.1037/0278-6133.26.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldfield GS, Epstein LH, Kilanowski CK, Paluch RA, Kogut-Bossler B. Cost-effectiveness of group and mixed family-based treatment for childhood obesity. Int J Obes Relat Metab Disord. 2001;25:1843–9. doi: 10.1038/sj.ijo.0801838. [DOI] [PubMed] [Google Scholar]
- 10.Minniti A, Bissoli L, Di Francesco V, et al. Individual versus group therapy for obesity: Comparison of dropout rate and treatment outcome. Eat Weight Disord. 2007;12:161–7. doi: 10.1007/BF03327593. [DOI] [PubMed] [Google Scholar]
- 11.Chanoine JP, Ambler KA, Ball GDC. Pediatric weight management programs in Canada: Where, what and how? Int J Pediatr Obes. 2010. Aug 30, [Epub ahead of print] [DOI] [PubMed]
- 12.Canadian Institutes of Health Research Strategy for Patient-Oriented research: A discussion paper for a 10-year plan to change health care using the levers of research. Feb, 2010. < www.cihr-irsc.gc.ca/e/41232.html> (Accessed on April 29, 2011).
- 13.Diabetes Prevention Program Investigators The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25:2165–71. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wing RR, Hamman RF, Bray GA, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res. 2004;12:1426–34. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller WR. Motivational interviewing: Research, practice, and puzzles. Addict Behav. 1996;21:835–42. doi: 10.1016/0306-4603(96)00044-5. [DOI] [PubMed] [Google Scholar]
- 16.Beck AT. The current state of cognitive therapy: A 40-year retrospective. Arch Gen Psychiatry. 2005;62:953–9. doi: 10.1001/archpsyc.62.9.953. [DOI] [PubMed] [Google Scholar]
- 17.Flattum C, Friend S, Neumark-Sztainer D, Story M. Motivational interviewing as a component of a school-based obesity prevention program for adolescent girls. J Am Diet Assoc. 2009;109:91–4. doi: 10.1016/j.jada.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tsiros MD, Sinn N, Brennan L, et al. Cognitive behavioral therapy improves diet and body composition in overweight and obese adolescents. Am J Clin Nutr. 2008;87:1134–40. doi: 10.1093/ajcn/87.5.1134. [DOI] [PubMed] [Google Scholar]
- 19.US Centers for Disease Control and Prevention . CDC BMI Growth Charts. Atlanta: US Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 20.Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics. 2005;115:e443–9. doi: 10.1542/peds.2004-2172. [DOI] [PubMed] [Google Scholar]
- 21.Eliakim A, Kaven G, Berger I, Friedland O, Wolach B, Nemet D. The effect of a combined intervention on body mass index and fitness in obese children and adolescents – a clinical experience. Eur J Pediatr. 2002;161:449–54. doi: 10.1007/s00431-002-0980-2. [DOI] [PubMed] [Google Scholar]
- 22.Sallis JF, Buono MJ, Roby JJ, Micale FG, Nelson JA. Seven-day recall and other physical activity self-reports in children and adolescents. Med Sci Sports Exerc. 1993;25:99–108. doi: 10.1249/00005768-199301000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Marinov B, Kostianev S, Turnovska T. Modified treadmill protocol for evaluation of physical fitness in pediatric age group – comparison with Bruce and Balke protocols. Acta Physiol Pharmacol Bulg. 2003;27:47–51. [PubMed] [Google Scholar]
- 24.Haines J, Neumark-Sztainer D, Wall M, Story M. Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obesity. 2007;15:2748–60. doi: 10.1038/oby.2007.327. [DOI] [PubMed] [Google Scholar]
- 25.Bacon L, Keim NL, Van Loan MD, et al. Evaluating a ‘non-diet’ wellness intervention for improvement of metabolic fitness, psychological well-being and eating and activity behaviors. Int J Obes Relat Metab Disord. 2002;26:854–65. doi: 10.1038/sj.ijo.0802012. [DOI] [PubMed] [Google Scholar]
- 26.Health Canada . Eating Well with Canada’s Food Guide. Ottawa: Health Canada; 2007. [Google Scholar]
- 27.Health Canada . Canada’s Physical Activity for Youth. Ottawa: Health Canada; 2002. [Google Scholar]
- 28.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;(1):CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Braet C, Mervielde I, Vandereycken W. Psychological aspects of childhood obesity: A controlled study in a clinical and nonclinical sample. J Pediatr Psychol. 1997;22:59–71. doi: 10.1093/jpepsy/22.1.59. [DOI] [PubMed] [Google Scholar]
- 30.Bokor S, Frelut ML, Vania A, et al. Prevalence of metabolic syndrome in European obese children. Int J Pediatr Obes. 2008;3(Suppl 2):3–8. doi: 10.1080/17477160802404509. [DOI] [PubMed] [Google Scholar]
- 31.Befort CA, Nollen N, Ellerbeck EF, Sullivan DK, Thomas JL, Ahluwalia JS. Motivational interviewing fails to improve outcomes of a behavioral weight loss program for obese African American women: A pilot randomized trial. J Behav Med. 2008;31:367–77. doi: 10.1007/s10865-008-9161-8. [DOI] [PubMed] [Google Scholar]
- 32.Devereaux PJ, Bhandari M, Clarke M, et al. Need for expertise based randomised controlled trials. BMJ. 2005;330:88. doi: 10.1136/bmj.330.7482.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pontiroli AE, Fossati A, Vedani P, et al. Post-surgery adherence to scheduled visits and compliance, more than personality disorders, predict outcome of bariatric restrictive surgery in morbidly obese patients. Obes Surg. 2007;17:1492–7. doi: 10.1007/s11695-008-9428-8. [DOI] [PubMed] [Google Scholar]
- 34.Golley RK, Magarey AM, Baur LA, Steinbeck KS, Daniels LA. Twelve-month effectiveness of a parent-led, family-focused weight-management program for prepubertal children: A randomized, controlled trial. Pediatrics. 2007;119:517–25. doi: 10.1542/peds.2006-1746. [DOI] [PubMed] [Google Scholar]
- 35.Reinehr T, Hebebrand J, Friedel S, et al. Lifestyle intervention in obese children with variations in the melanocortin 4 receptor gene. Obesity. 2009;17:382–9. doi: 10.1038/oby.2008.422. [DOI] [PubMed] [Google Scholar]
- 36.Edwards NM, Schwarzenberg SJ. Designing and implementing an effective pediatric weight management program. Rev Endocr Metab Disord. 2009;10:197–203. doi: 10.1007/s11154-009-9110-z. [DOI] [PubMed] [Google Scholar]
- 37.Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: A randomized controlled trial. JAMA. 2007;297:2697–704. doi: 10.1001/jama.297.24.2697. [DOI] [PubMed] [Google Scholar]
- 38.Barlow SE, Ohlemeyer CL. Parent reasons for nonreturn to a pediatric weight management program. Clin Pediatr. 2006;45:355–60. doi: 10.1177/000992280604500408. [DOI] [PubMed] [Google Scholar]
- 39.Zeller M, Kirk S, Claytor R, et al. Predictors of attrition from a pediatric weight management program. J Pediatr. 2004;144:466–70. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 40.Cote MP, Byczkowski T, Kotagal U, Kirk S, Zeller M, Daniels S. Service quality and attrition: An examination of a pediatric obesity program. Int J Qual Health Care. 2004;16:165–73. doi: 10.1093/intqhc/mzh015. [DOI] [PubMed] [Google Scholar]