Abstract
An intrahepatic arterioportal fistula is a rare cause of portal hypertension and variceal bleeding. We report on a patient with an intrahepatic arterioportal fistula following liver biopsy who was successfully treated by hepatectomy after unsuccessful arterial embolization. We also review the literature on symptomatic intrahepatic arterioportal fistulas after liver biopsy. A 48-year-old male with bleeding gastric varices and hepatitis B virus-associated liver cirrhosis was transferred to our hospital; this patient previously underwent percutaneous liver biopsies 3 and 6 years ago. Abdominal examination revealed a bruit over the liver, tenderness in the right upper quadrant, and splenomegaly. Ultrasonographic examination, computed tomography, and angiography confirmed an arterioportal fistula between the right hepatic artery and the right portal vein with portal hypertension. After admission, the patient suffered a large hematemesis and developed shock. He was treated with emergency transarterial embolization using microcoils. Since some collateral vessels bypassed the obstructive coils and still fed the fistulous area, embolization was performed again. Despite the second embolization, the collateral vessels could not be completely controlled. Radical treatment involving resection of his right hepatic lobe was performed. For nearly 6 years postoperatively, this patient has had no further episodes of variceal bleeding.
Keywords: Intrahepatic arterioportal fistula, Liver biopsy, Portal hypertension, Arterial embolization, Hepatectomy
Introduction
It is not surprising that intrahepatic arterioportal fistula (APF) occurs following interventional procedures to the liver. Most small, peripheral APFs caused by liver biopsy are usually asymptomatic and generally thrombose within 1 month [1]; however, an APF is a rare cause of portal hypertension and gastric variceal bleeding.
At present, radiologic intervention is the treatment of first choice for most APFs, and surgery is needed only rarely. We report on a patient with APF following liver biopsy who was successfully treated by hepatectomy after unsuccessful arterial embolization. We also review the literature about symptomatic APFs after liver biopsy.
Case report
A 48-year-old male was admitted to a local hospital complaining of hematemesis and melena. The patient was diagnosed as having bleeding gastric varices and hepatitis B virus-associated liver cirrhosis. The gastric varices were obliterated by an injection of isobutyl 2-cyanoacrylate and ethanol. After clinical stabilization, he was transferred to our hospital for further treatment.
At 42 and 45 years of age, this patient underwent percutaneous liver biopsies from the right anterosuperior area using a Tru-cut needle under ultrasound guidance before interferon therapy; however, no complications were encountered during the procedures. He had been regularly followed up at another regional clinic after interferon therapy but no abnormal findings were detected on ultrasonographic examination of the liver.
At the time of admission to our hospital he was not icteric, had a pulse rate of 72/min, and was normotensive (BP 116/66 mmHg). Abdominal examination revealed a bruit over the liver, tenderness in the right upper quadrant, and splenomegaly. Laboratory examination showed hemoglobin 11.2 g/dL, platelets 7.5 × 104/μL, serum albumin 3.8 g/dL, total serum bilirubin 0.69 mg/dL, aspartate aminotransferase 30 IU/L, alanine aminotransferase 25 IU/L, prothrombin time 11.2 s (control 10.5 s), and α-fetoprotein in the normal range. Endoscopy showed severe esophagogastric varices (Li, F2, Cw, RC0, Lg-f, F3, Cb, RC2) (Fig. 1).
Fig. 1.
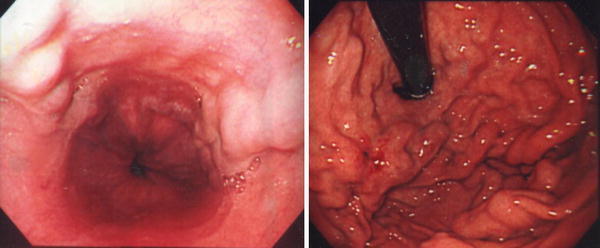
Endoscopy showing severe esophagogastric varices (Li, F2, Cw, RC0, Lg-f, F3, Cb, RC2)
Ultrasonographic examination of the liver revealed a dilated tubular vascular structure with a diameter of 17 mm in the right anterosuperior area (Fig. 2a) and a dilated right hepatic artery.
Fig. 2.
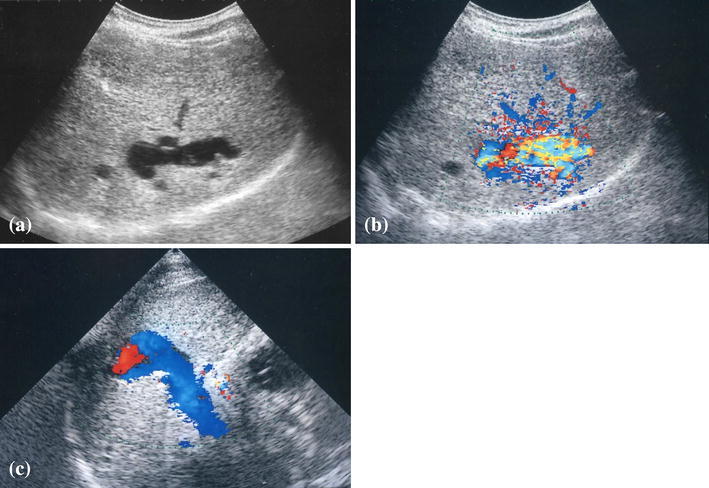
a Conventional B-mode ultrasonography showing a dilated tubular vascular structure (diameter 17 mm) in the right anterosuperior area; b color Doppler ultrasound of the tubular vascular structure demonstrates an area of color cloud with turbulence; c color Doppler ultrasound showing hepatofugal flow in the portal vein
Color Doppler ultrasound of the tubular vascular lesion demonstrated an area of color cloud with turbulence (Fig. 2b) and localized high velocity blood flow; the direction of the flow in the portal vein was hepatofugal (Fig. 2c).
A triphasic computed tomography (CT) scan showed an enlarged right hepatic artery and pooling of contrast material in the right anterosuperior area of the liver. The pooling image had pronounced enhancement in the arterial phase (Fig. 3). The diagnosis of an intrahepatic APF was suggested.
Fig. 3.

Triphasic CT scan in the arterial phase shows an enlarged right hepatic artery and pooling of contrast material in the right anterosuperior area of the liver
Angiography confirmed an APF between the right hepatic artery and the right portal vein (Fig. 4a), with immediate retrograde filling of the portal vein and reflux to the left gastric vein, as well as extensive collateral circulation through the esophagogastric and perisplenic vascular beds (Fig. 4b).
Fig. 4.
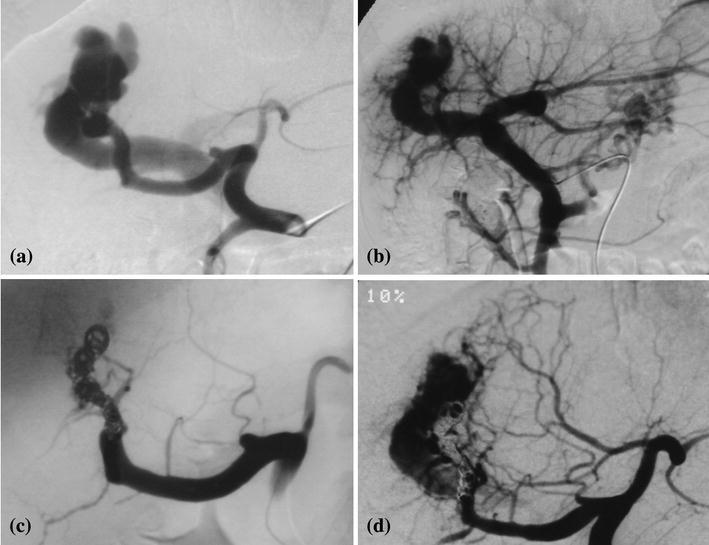
a Angiography shows an arterioportal fistula between the right hepatic artery and the right portal vein; b angiography shows immediate retrograde filling of the portal vein and reflux to the left gastric vein, as well as extensive collateral circulation through the esophagogastric and perisplenic vascular beds; c complete occlusion of the distal right hepatic artery is seen after emergency coil embolization; d some collateral vessels from the right and left hepatic artery are bypassing the obstructive coils and feeding the area of the fistula
On the 23rd day after admission, the patient suffered a large hematemesis and developed shock. He was treated with blood transfusions and a Sengstaken–Blakemore tube. Since the right hepatic fistula feeder seemed rather narrow, emergency coil embolization was performed with 19 fibered platinum microcoils (VortX®, Boston Scientific, Natick, MA, USA). Control hepatic arteriography at the end of the procedure showed complete occlusion of the distal right hepatic artery (Fig. 4c) and hepatopetal flow in the portal vein.
When the patient was reviewed 29 days later, he was asymptomatic, and endoscopy revealed less prominent esophagogastric varices. The second angiography showed revascularization of the APF. Since some collateral vessels from the right and left hepatic arteries bypassed the obstructive coils and still fed the fistulous area (Fig. 4d), transarterial embolization was performed again with 9 fibered platinum microcoils. Despite the second embolization, the collateral vessels could not be controlled completely. After the second procedure, color Doppler ultrasound of the left portal vein demonstrated hepatopetal flow, but the direction of the flow in the right portal vein was hepatofugal.
Since the remaining APF had a risk of variceal bleeding, the patient underwent an uncomplicated resection of his right hepatic lobe to remove the fistula shortly thereafter. Surgical findings of the liver showed mild blunt edge, slight irregular surface, atrophic right lobe and enlarged left lobe. Because the general condition of the patient worsened due to repeated hematemesis and treatments, portal vein pressure was not measured before and after surgery.
An endoscopy performed 7 months postoperatively showed the esophageal varices had disappeared and the gastric varices (Lg-f, F1, Cw, RC0) had improved (Fig. 5). For nearly 6 years postoperatively, this patient has had no further episodes of variceal bleeding.
Fig. 5.
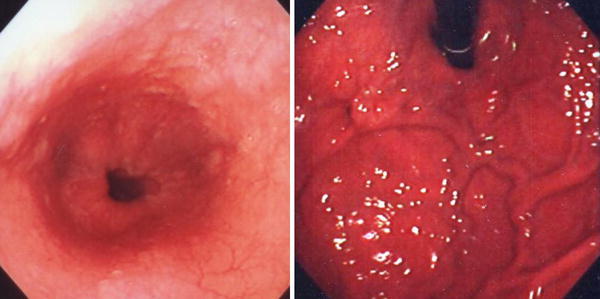
Endoscopy showing disappeared esophageal varices and improved gastric varices (Lg-f, F1, Cw, RC0)
Discussion
Sachs [2], in 1892, was the first to report an intrahepatic APF which had been found at autopsy in a patient who died of hemorrhage from esophageal varices. APFs have been said to result from congenital arteriovenous malformation, ruptured hepatic aneurysm, trauma, iatrogenic causes, liver cirrhosis, or liver tumor. Preger [3] first described an APF occurring after liver biopsy in 1967.
APFs probably develop following liver biopsy when the biopsy needle causes a branch of the high-pressure hepatic artery and a branch of the low-pressure portal vein to communicate [4]. The frequency of APFs following liver biopsy was reported to be 5.4% by Okuda et al. [5] when they performed hepatic arteriography within 4 weeks of the procedure. Most of these APFs were small in size and closed spontaneously; none of these shunts caused portal hypertension. In rare cases, as in the present patient, the fistula grows in size and becomes clinically symptomatic with portal hypertension.
We searched PubMed and the Igaku-chuou-zassi (Japana Centra Reveuo Medicina) database (1983–2010) using keywords ‘arterioportal fistula’, ‘arteriovenous fistula’ and ‘liver biopsy’ for reports documenting APFs following liver biopsy. From among the English language reports, clinically symptomatic cases following percutaneous liver biopsy were selected (Table 1) [4, 6–29]. A case observed in our unit was also added to the review.
Table 1.
Reported cases of symptomatic intrahepatic arterioportal fistulas following percutaneous liver biopsy
| Case | Year | Age/sex | Background | Needle | Number of passes | US guided | Clinical delay | Symptoms | Abdominal bruit | Treatment | Outcome | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1977 | 52/M | Alcoholism | Menghini (1.4 mm) | 1 | NA | 4 months | VB | + | Portocaval shunt | D | [6] |
| 2 | 1983 | 71/F | Obesity, hematemesis | NA | NA | NA | 2 days | VB | + | Embolization, mesocaval shunt | A | [7] |
| 3 | 1983 | 49/F | Chronic liver disease (SLE) | NA | NA | NA | NR | VB | + | Embolization | A | [8] |
| 4 | 1987 | 48/F | Histiocytic lymphoma | NA | NA | NA | 3 days | Abdominal pain | NA | – | A | [9] |
| 5 | 1987 | 59/M | Rectal cancer | NA | NA | NA | 2 months | Hematochezia | NA | – | A | [9] |
| 6 | 1989 | 51/F | PSC, ulcerative colitis | NA | NA | NA | 5 years | VB | + | Transplantation | A | [10] |
| 7 | 1989 | 64/F | Liver dysfunction | Tru-cut | 1 | NA | 75 min | Back pain, shock | NA | Embolization | D | [11] |
| 8 | 1991 | 35/F | Chronic hepatitis B | NA | NA | NA | 4 years | VB | NA | CE | A | [12] |
| 9 | 1993 | 21/F | LTR (BCS) | NA | NA | NA | 70 days | Ascites | NA | CE | A | [13] |
| 10 | 1994 | 67/M | Chronic hepatitis C | Klatskin (16G) | 2 | NA | 17 days | Chest pain, back pain | NA | CE | A | [14] |
| 11 | 1995 | 2.5/F | LTR (biliary atresia) | Tru-cut (14G) | NA | Yes | 3 months | Ascites | NA | CE, surgical division | D | [15] |
| 12 | 1996 | 65/F | Intrahepatic cholestasis | NA | NA | NA | 1 h | Abdominal pain, hematemesis | NA | CE | A | [16] |
| 13 | 1996 | 65/F | POEMS syndrome | Surecut (1.6 mm) | 1 | Yes | 18 h | Abdominal pain | NA | Embolization | A | [17] |
| 14 | 1998 | 59/F | LTR | NA | NA | NA | 15 years | Abdominal pain, pyrexia | NA | Embolization, CE | A | [18] |
| 15 | 2001 | 67/F | Chronic cholestasis | NA | NA | Yes | 2 days | Abdominal pain, jaundice | NA | Embolization | A | [19] |
| 16 | 2001 | 71/F | Liver dysfunction | NA | NA | NA | 18 years | VB | + | CE | A | [20] |
| 17 | 2002 | 49/M | Chronic hepatitis C | Biopsy gun (18G) | 1 | Yes | 9 days | Abdominal pain, hematochezia | NA | CE | A | [21] |
| 18 | 2004 | 32/M | Liver dysfunction (Crohn’s disease) | Tru-cut (14G) | 2 | NA | 4 days | Abdominal pain, pyrexia | NA | CE | A | [22] |
| 19 | 2005 | 61/F | LTR (PBC) | NA | NA | NA | 7 months | Ascites | NA | Embolization | A | [23] |
| 20 | 2005 | 55/F | Liver dysfunction, arthralgia, skin rash | NA | NA | NA | 26 years | Decompensation, sepsis | NA | CE | A | [24] |
| 21 | 2005 | 68/F | Chronic hepatitis C | Menghini (2.8 mm) | NA | Yes | 2 days | Abdominal pain | NA | Embolization | A | [25] |
| 22 | 2006 | 46/F | LTR (HBV related liver failure) | NA | NA | NA | 2 years | Edema | + | CE | A | [26] |
| 23 | 2006 | 51/M | Wilson’s disease | NA | NA | NA | 43 years | Ascites | NA | Embolization, transplantation | NA | [4] |
| 24 | 2007 | 13/M | LTR (biliary atresia) | NA | NA | NA | 7 years | Ascites, VB | NA | CE, embolization | A | [27] |
| 25 | 2007 | 14/F | LTR (biliary atresia) | Monopty (18G) | 1 | No | 6 months | Ascites, VB | NA | CE | A | [28] |
| 26 | 2007 | 6/M | LTR (acute liver failure) | Monopty (18G) | 1 | No | 6 months | Ascites, VB | NA | CE | A | [28] |
| 27 | 2007 | 9/M | LTR (liver failure) | Monopty (18G) | 1 | No | 3 months | Ascites, VB | NA | CE | A | [28] |
| 28 | 2007 | 5/F | LTR | Monopty (18G) | 1 | No | 4 months | Abdominal pain, ascites | NA | CE | A | [28] |
| 29 | 2008 | 80/F | Liver dysfunction | NA | NA | NA | 35 years | Ascites | NA | CE | A | [29] |
| 30 | 2011 | 48/M | HBV related liver cirrhosis | Tru-cut | NA | Yes | 3 or 6 years | VB | + | CE, hepatectomy | A | Our case |
A alive, BCS Budd–Chiari syndrome, CE coil embolization, D died, HBV hepatitis B virus, LTR liver transplant recipient, NA not available, PBC primary biliary cirrhosis, PSC primary sclerosing cholangitis, POEMS polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes, SLE systemic lupus erythematous, US ultrasonography, VB variceal bleeding
The common manifestations of intrahepatic APFs include gastrointestinal bleeding (33%), ascites (26%), congestive heart failure (4.5%), and diarrhea (4.5%) [30]. In the present review of cases after percutaneous liver biopsy, gastrointestinal bleeding occurred in 14 of 30 cases (47%), with ascites in 10 of 30 cases (33%). While most documented cases of gastrointestinal bleeding occurred with esophageal varices, this is the first report of gastric variceal bleeding caused by APF following percutaneous liver biopsy. Intrahepatic APF, although rare, should be kept in mind as one of the differential diagnoses when there are cirrhotic bleeding varices with a past history of liver biopsy. On physical examination, the presence of an abdominal bruit or thrill is often an important clue [1]. In the present review, a bruit was detected in 7 of 30 cases (23%).
Since the biopsy needle, specimen, site, and procedure were not stated in detail in most case reports, the trends about them are unclear; as can be seen in Table 1, some important factors are missing. However, some reports demonstrated that biopsy was performed without ultrasonography, and biopsy specimen revealed the structure of vessels. For safety, liver biopsy under ultrasonography would be desirable [31]. The use of ultrasound-guided needle biopsy can avoid laceration of vessels and formation of APFs. Examination of puncture site by Color Doppler ultrasound is useful in addition to B-mode ultrasound before the procedure [32]. In the present review of cases, liver transplant recipients were shown in 10 of 30 cases (33%). Needle biopsy is a useful and indispensable procedure for assessment and diagnosis of liver damage in patients after liver transplantation as well as other liver diseases.
It has been reported that the interval between the formation of an APF and its recognition can range from hours to 42 years [33]. In the present review, the interval was from 1 h to 43 years. Careful long-term follow-up is recommended for patients after liver biopsy.
Recently, transarterial embolization has been attempted as the first-choice treatment because of its low invasiveness and success in some cases. Some unsuccessful cases following transarterial embolization have been reported. In the unsuccessful cases, a surgical procedure, such as ligation of the hepatic artery, a mesocaval or portocaval shunt, or hepatic resection, was chosen. To avoid the risk of hepatic infarction in the present case, radical treatment involving right hepatic lobe resection was performed because of the two failed attempts to close the fistula by transarterial embolization. Since the recurrence rate after transarterial embolization for intrahepatic APFs is unclear, close long-term observation is needed after treatment.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Guzman EA, McCahill LE, Rogers FB. Arterioportal fistulas: introduction of a novel classification with therapeutic implications. J Gastrointest Surg. 2006;10:543–550. doi: 10.1016/j.gassur.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 2.Sachs R. Zur casuisitik der gefasserkrankungen. Deutsche Medizinische Wochenschr. 1892;18:443–447. doi: 10.1055/s-0029-1199146. [DOI] [Google Scholar]
- 3.Preger L. Hepatic arteriovenous fistula after percutaneous liver biopsy. Am J Roentgenol Radium Ther Nucl Med. 1967;101:619–620. doi: 10.2214/ajr.101.3.619. [DOI] [PubMed] [Google Scholar]
- 4.Duman JD, Johnson SP, Trotter JF. Arterioportal fistula requiring liver transplantation. Liver Transpl. 2006;12:1904–1905. doi: 10.1002/lt.20989. [DOI] [PubMed] [Google Scholar]
- 5.Okuda K, Musha H, Nakajima Y, Takayasu K, Suzuki Y, Morita M, et al. Frequency of intrahepatic arteriovenous fistula as a sequel to percutaneous needle puncture of the liver. Gastroenterology. 1978;74:1204–1207. [PubMed] [Google Scholar]
- 6.Baer JW. Hepatic arterioportal fistula related to a liver biopsy. Gastrointest Radiol. 1977;20:297–299. doi: 10.1007/BF02256508. [DOI] [PubMed] [Google Scholar]
- 7.Agha FP, Raji MR. Successful transcatheter embolic control of significant arterioportal fistula: a serious complication of liver biopsy. Br J Radiol. 1983;56:277–280. doi: 10.1259/0007-1285-56-664-277. [DOI] [PubMed] [Google Scholar]
- 8.Kerlan RK, Bank WO, Hoddick WK, Pogany AC, Sollenberger RD. Occlusion of a hepatic artery to portal vein fistula with bucrylate. Cardiovasc Intervent Radiol. 1983;6:138–140. doi: 10.1007/BF02552765. [DOI] [PubMed] [Google Scholar]
- 9.Strodel WE, Eckhauser FE, Lemmer JH, Whitehouse WM, Jr, Williams DM. Presentation and perioperative management of arterioportal fistulas. Arch Surg. 1987;122:563–571. doi: 10.1001/archsurg.1987.01400170069010. [DOI] [PubMed] [Google Scholar]
- 10.Hashimoto E, Ludwig J, MacCarty RL, Dickson ER, Krom RA. Hepatoportal arteriovenous fistula: morphologic features studied after orthotopic liver transplantation. Hum Pathol. 1989;20:707–709. doi: 10.1016/0046-8177(89)90160-3. [DOI] [PubMed] [Google Scholar]
- 11.Korula J, Fried J, Weissman M, Greaney G, Liew CT, Finck E. Fatal hemorrhage from an arterio-portal-peritoneal fistula after percutaneous liver biopsy. Gastroenterology. 1989;96:244–246. doi: 10.1016/0016-5085(89)90788-9. [DOI] [PubMed] [Google Scholar]
- 12.Romeo JM, Herrera N, Perez Picouto L. Angiographic embolization of intrahepatic arterioportal fistula. Br J Surg. 1991;78:736–737. doi: 10.1002/bjs.1800780632. [DOI] [PubMed] [Google Scholar]
- 13.Chavan A, Harms J, Pichlmayr R, Galanski M. Transcatheter coil occlusion of an intrahepatic arterioportal fistula in a transplanted liver. Bildgebung. 1993;60:215–218. [PubMed] [Google Scholar]
- 14.Kowdley KV, Aggarwal AM, Sachs PB. Delayed hemorrhage after percutaneous liver biopsy. Role of therapeutic angiography. J Clin Gastroenterol. 1994;19:50–53. doi: 10.1097/00004836-199407000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Otobe Y, Hashimoto T, Shimizu Y, Nakamura T, Yamamori N, Hayashi S, et al. Formation of fatal arterioportal fistula following needle liver biopsy in a child with a living-related liver transplant: report of a case. Surg Today. 1995;25:916–919. doi: 10.1007/BF00311759. [DOI] [PubMed] [Google Scholar]
- 16.Cacho G, Abreu L, Calleja JL, Prados E, Albillos A, Chantar C, et al. Arterioportal fistula and hemobilia with associated acute cholecystitis: a complication of percutaneous liver biopsy. Hepatogastroenterology. 1996;43:1020–1023. [PubMed] [Google Scholar]
- 17.Grieco A, Bianco A, Pieri S, Costamagna G, Flammia G, Greco AV. Massive haemobilia after percutaneous liver biopsy in a patient with POEMS syndrome successfully treated by arterial embolization. Eur J Gastroenterol Hepatol. 1996;8:595–598. doi: 10.1097/00042737-199606000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Wong JK, Gray RR. Soft tissue case 24: arteriovenous fistula secondary to liver biopsy. Can J Surg. 1998;41:423–438. [PMC free article] [PubMed] [Google Scholar]
- 19.Gómez-Valero JA, Sardi J, Vilaseca J, Pérez Lafuente M, Malagelada JR. Pancreatitis and haemobilia due to arterioportal fistula after percutaneous liver biopsy resolved by selective arterial embolization. Eur J Gastroenterol Hepatol. 2001;13:727–730. doi: 10.1097/00042737-200106000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Pohle T, Fischbach R, Domschke W. Arterioportal fistula: a rare cause of portal hypertension and abdominal pain. Scand J Gastroenterol. 2001;36:1227–1229. doi: 10.1080/003655201300191932. [DOI] [PubMed] [Google Scholar]
- 21.Machicao VI, Lukens FJ, Lange SM, Scolapio JS. Arterioportal fistula causing acute pancreatitis and hemobilia after liver biopsy. J Clin Gastroenterol. 2002;34:481–484. doi: 10.1097/00004836-200204000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Hodgson RS, Taylor-Robinson SD, Jackson JE. Haematochezia in Crohn’s disease caused by late-onset haemobilia following percutaneous liver biopsy. Eur J Gastroenterol Hepatol. 2004;16:229–232. doi: 10.1097/00042737-200402000-00018. [DOI] [PubMed] [Google Scholar]
- 23.Botelberge T, Vlierberghe H, Voet D, Defreyne L. Detachable balloon embolization of an arterioportal fistula following liver biopsy in a liver transplant recipient: a case report and review of literature. Cardiovasc Intervent Radiol. 2005;28:832–835. doi: 10.1007/s00270-004-0193-3. [DOI] [PubMed] [Google Scholar]
- 24.Guha IN, Stedman B, Iredale JP, Sheron N. Case report of an arterioportal fistula, presenting with accelerated decompensation and sepsis, twenty-six years after initial liver biopsy. Hepatol Res. 2005;32:252–255. doi: 10.1016/j.hepres.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 25.Lin CL, Chang JJ, Lee TS, Lui KW, Yen CL. Gallbladder polyp as a manifestation of hemobilia caused by arterial-portal fistula after percutaneous liver biopsy: a case report. World J Gastroenterol. 2005;11:305–307. doi: 10.3748/wjg.v11.i2.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dentry O, Roover A, Delwaide J, Dondelinger RF, Meurisse M, Honoré P. Selective coil occlusion of a large arterioportal fistula in a graft. Liver Transpl. 2006;12:888–889. doi: 10.1002/lt.20695. [DOI] [PubMed] [Google Scholar]
- 27.Racadio JM, Sheyn DD, Neely JC, Racadio JM, Vu DN. Embolization of an arterioportal fistula by injection of D-stat into the portal venous outflow. J Vasc Interv Radiol. 2007;18:781–784. doi: 10.1016/j.jvir.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 28.Falkenstein K, Flynn L, Dunn S, Baldridge A. Arterial-venous fistulas following pediatric liver transplant case studies. Pediatr Transplant. 2007;11:683–688. doi: 10.1111/j.1399-3046.2007.00742.x. [DOI] [PubMed] [Google Scholar]
- 29.Oza N, Mizuta T, Egashira Y, Nojiri J, Ario K, Akiyama T, et al. A case of portal hypertension caused by intrahepatic arterio-portal fistula formed after percutaneous liver biopsy 35 years previously, markedly improved by transcatheter arterial embolization against the fistula. Kanzo. 2008;49:506–511. doi: 10.2957/kanzo.49.506. [DOI] [Google Scholar]
- 30.Vauthey JN, Tomczak RJ, Helmberger T, Gertsch P, Forsmark C, Caridi J, et al. The arterioportal fistula syndrome: clinicopathologic features, diagnosis, and therapy. Gastroenterology. 1997;113:1390–1401. doi: 10.1053/gast.1997.v113.pm9322535. [DOI] [PubMed] [Google Scholar]
- 31.Papini E, Pacella CM, Rossi Z, Bizzarri G, Fabbrini R, Nardi F, et al. A randomized trial of ultrasound-guided anterior subcostal liver biopsy versus the conventional Menghini technique. J Hepatol. 1991;13:291–297. doi: 10.1016/0168-8278(91)90071-I. [DOI] [PubMed] [Google Scholar]
- 32.Polakow J, Ladny JR, Dzieciol J, Puchalski Z. Ultrasound guided percutaneous fine-needle biopsy of the liver: efficacy of color doppler sonography. Hepatogastroenterology. 1998;45:1829–1830. [PubMed] [Google Scholar]
- 33.Ryan KG, Lorber SH. Traumatic fistula between hepatic artery and portal vein. Report of a case. N Engl J Med. 1968;279:1215–1216. doi: 10.1056/NEJM196811282792208. [DOI] [PubMed] [Google Scholar]


