Abstract
Purpose
The cuff volume of the Cobra perilaryngeal airway (CobraPLA) is larger than that of other alternative airway devices and makes it difficult to predict the effect of cuff pressure on the perilaryngeal mucosa. We tested the hypothesis that adjustment of the cuff pressure of the CobraPLA could reduce the incidence of postoperative sore throat (POST).
Methods
After induction of general anesthesia and insertion of the CobraPLA by standardized method, the cuff pressure was set to 60 cmH2O (group C, n = 87) or adjusted to minimal seal-up pressure +5 cmH2O (group A, n = 87). The frequency and severity (0, none; 1, mild; 2, moderate; 3, severe) of throat soreness, pain, discomfort, and adverse effects were evaluated 1 and 24 h after removal of the CobraPLA.
Results
Incidence of moderate POST in group C was higher than that in group A (11% vs. 2%, P = 0.021) whereas the overall POST incidence was not different between the two groups (31% vs. 20%, P = 0.092). The inflated air volume of group A was different from that of group C (41 vs. 50 ml, P = 0.009).
Conclusions
Adjustment of cuff pressure reduces the incidence of moderate POST after use of the CobraPLA.
Keywords: Cobra perilaryngeal airway, Cuff pressure, Sore throat
Introduction
Postoperative sore throat (POST) is one of the most common avoidable complications after using an airway device [1]. The reported incidences of sore throat after general anesthesia using tracheal intubation, laryngeal mask airway (LMA), and the Cobra perilaryngeal airway (CobraPLA) are 10–8%, 0–34%, and 0–50%, respectively [1–4].
The CobraPLA is widely used for emergent airway management or during short-duration surgery because it can be inserted easily even in a patient with neck contracture and can be used as a conduit for tracheal intubation [5–9].
The cuff volume of the CobraPLA is larger than that of the LMA. However, there is no report about the association between cuff pressure and the incidence of POST after using CobraPLA. High volume or high pressure of the cuff is associated with high incidence of POST after tracheal intubation and the use of LMA [1, 10–13]. Measurement of the cuff pressure of the airway device can provide reliable information about the pressurizing force to the pharyngeal mucosa, which is the main cause of sore throat after the use of an airway device [14].
We tested the hypothesis that adjustment of the cuff pressure could reduce the incidence of POST after use of the CobraPLA.
Materials and methods
This study was performed after obtaining approval from the Institutional Review Board and written informed consent from patients. Patients (n = 174) with American Society of Anesthesiologists (ASA) physical status 1–2, 15–65 years old, and undergoing elective short-duration orthopedic surgery (<2 h) under general anesthesia were recruited into this study. Patients with aspiration risk and known airway disease, Mallampati class >3, mouth opening <3 cm, thyromental distance <6 cm, body mass index (BMI) >35 kg/m2, and recent history of throat soreness and discomfort, dysphagia, and dysphonia were excluded from the study.
All patients were premedicated with 0.004 mg/kg glycopyrrolate given intravenously 20 min before anesthesia. After the standard monitors (ECG, pulse oximetry, noninvasive arterial pressure, and capnography) were installed and preoxygenation with oxygen 8 l/min was administered through a facemask, anesthesia was induced intravenously with thiopental 5 mg/kg, fentanyl 1.5 μg/kg, and rocuronium 0.6 mg/kg. Anesthesia was maintained with sevoflurane 1.5–2.0%, FiO2 0.4 with air, and mechanical ventilation with a tidal volume of 8 ml/kg and respiratory rate of 10 breaths/min. Respiratory rate was adjusted to maintain normocapnia (end-tidal carbon dioxide, 35–40 mmHg). An experienced anesthesiologist confirmed the full relaxation of the jaw and inserted the Cobra perilaryngeal airway (CobraPLA®, Pulmodyne, IN, USA) with the following standardized insertion techniques: lubricate the head and fold back the cuff, extend the head and neck, open the mouth, insert the head of the CobraPLA into the oral cavity, thrust the jaw with the left hand, insert the ventilating tube with the right hand until resistance is felt, and slightly withdraw. Cuff size of the CobraPLA was selected by body weight: size 3 for 35–69 kg or size 4 for 70–100 kg. The head position of the CobraPLA was optimized with a flexible fiberoptic bronchoscope (PortaView LF-GP; Olympus, Tokyo, Japan) to avoid a folding or herniation of the epiglottis and arytenoid cartilage through the anterior grill of the CobraPLA head. Patients were randomly assigned to the two groups using presealed opaque envelopes (Table 1). After insertion of the CobraPLA, the cuff pressure was set to 60 cmH2O (group C, n = 87) or adjusted to minimal seal-up pressure +5 cmH2O (group A, n = 87). The cuff pressure was measured and regulated by means of the Digital P-V Gauge (Mallinckrodt, Athlone, Ireland). The cuff volume was measured with a 50-ml syringe (Korea Vaccine, Ansan, Korea) after setting the cuff pressure. Leaks between the cuff and peri-cuff mucosa were detected by stethoscopic auscultation on the neck and observation of intraoral bubble during positive pressure ventilation. The minimal seal-up pressure was determined as the least cuff pressure when the leaks disappeared during inspiratory phase while inflating the cuff. The airway pressure and hemodynamic data were collected before and immediately after insertion of the CobraPLA. A blinded investigator evaluated the frequency and severity of POST at 1 and 24 h after removal of the CobraPLA. For clarity, we defined POST as throat soreness, pain, or any discomfort without bloody secretion regardless of rest, swallowing, and phonation. Severity scores were graded as follows: no symptom, 0; mild throat soreness, pain, or any discomfort, 1; moderate, 2; and severe, 3. After inflating the cuff to preset level, each patient’s tongue was observed to determine whether it protruded or became cyanotic. In case of tongue cyanosis, the trachea was intubated after removal of the CobraPLA. If the patient could not be ventilated effectively (high airway pressure >35 cmH2O, low inspired tidal volume <5 ml/kg, and low SpO2 <95%) and epigastric areas were expanded with bubble sounds, tracheal intubation and gastric suction were performed to protect the airway. At the end of anesthesia, the cuff was deflated completely and removed after careful suction of secretion while checking for the presence of bloody secretion. Adverse effects such as bloody secretion, ineffective ventilation, gastric expansion, and tongue protrusion-linked cyanosis were excluded from the data (Fig. 1).
Table 1.
Demographics and anesthetic data in the two groups
| Group C n = 83 |
Group A n = 85 |
P value | |
|---|---|---|---|
| Gender (male/female) | 44/39 | 49/36 | 0.55 |
| Age (years) | 36 ± 13 | 36 ± 17 | 0.97 |
| Weight (kg) | 66 ± 11 | 64 ± 12 | 0.58 |
| Height (cm) | 167 ± 8 | 167 ± 9 | 0.85 |
| BMI (kg/m2) | 24.1 ± 5.3 | 23.2 ± 4.7 | 0.89 |
| ASA (1/2) | 67/16 | 70/15 | 0.79 |
| Mallampati class (1/2) | 75/8 | 71/14 | 0.19 |
| Device size (3/4) | 55/28 | 55/30 | 0.83 |
| Duration of ventilation (min) | 54 ± 21 | 57 ± 24 | 0.56 |
Data are expressed as mean ± SD and numberCuff pressure was set to 60 cmH2O (group C) or adjusted to minimal seal-up pressure +5 cmH2O (group A)
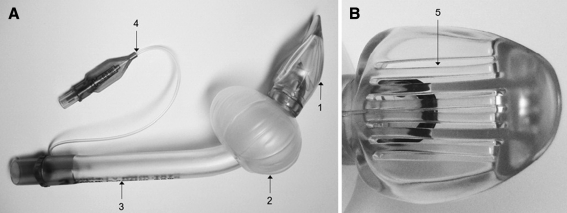
Fig. 1.
Cobra perilaryngeal airway (CobraPLA) has three components: head (1) (which looks like a cobra snake); cuff (2) with large volume; ventilation tube (3); and inflating valve (4). Lateral view of CobraPLA (a) and anterior view (b) of the head with anterior grill (5)
Previous data demonstrated that the incidence of POST after use of the CobraPLA was about 40% when cuff pressure was set to 60 cmH2O [5]. The sample size was determined according to the assumption that cuff adjustment could reduce the incidence of POST to half (from 40% for group C to 20% for group A) at a loss rate of 0.1, power of 0.8, and α of 0.05. Data analysis was performed using SPSS (version 12.0; SPSS, Buffalo, NY, USA). Quantitative data such as demographic, anesthetic, cuff, and respiratory variables were compared using the two-sided independent Student’s t-test or Mann–Whitney U-test. Qualitative data such as gender, ASA, Mallampati class, device size, and overall incidence of POST were compared with Pearson’s chi-square test or Fisher’s exact test. The severity of POST was compared with a linear by linear association. A P value less than 0.05 was considered statistically significant.
Results
The inflated air volume of group A was less than that of group C (41 vs. 50 ml, P = 0.009) (Table 2).
Table 2.
Cuff and respiratory data in the two groups
| Group C n = 83 |
Group A n = 85 |
P value | |
|---|---|---|---|
| P seal (cmH2O) | N/C | 20 ± 5 | |
| P cuff (cmH2O) | 60 | 24 ± 9 | <0.01 |
| V cuff (ml) | 50 ± 8 | 41 ± 13 | 0.01 |
| P peak (cmH2O) | 21.4 ± 4.5 | 21.5 ± 5.5 | 0.99 |
| P plat (cmH2O) | 12.3 + 2.6 | 12.7 ± 2.8 | 0.47 |
Data are expressed as mean ± SD. Cuff pressure was set to 60 cmH2O (group C) or adjusted to minimal seal-up pressure +5 cmH2O (group A)
P seal seal-up pressure, P cuff intra-cuff pressure, V cuff cuff volume, P peak airway peak pressure, P plat airway plateau pressure
The overall POST incidence of the two groups (31% of group C vs. 20% of group A, P = 0.092) was not different. However, the incidence of moderate POST in group C was higher than that of group A (11% vs. 2%, P = 0.021). The proportion of moderate degree POST of all POST cases in group C (35%) was threefold that in group A (12%). Most POST in group A was mild (Table 3).
Table 3.
Incidences of postoperative sore throat after Cobra perilaryngeal airway
| Time (h) | Severity | POST (%) | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||
| Group C (n = 83) | 1 | 57 | 16 (19) | 9 (11)* | 1 (1) | 26 (31) |
| 24 | 80 | 3 (3) | 0 | 0 | 3 (3) | |
| Group A (n = 85) | 1 | 68 | 15 (18) | 2 (2) | 0 | 17 (20) |
| 24 | 84 | 1 (1) | 0 | 0 | 1 (1) | |
Data are expressed as numbers of patients and proportion (%). Severity scores are graded as follows: 0, none; 1, mild; 2, moderate; or 3, severe throat soreness, pain, or discomfort. Cuff pressure was set to 60 cmH2O (group C) or adjusted to minimal seal-up pressure +5 cmH2O (group A)
POST postoperative sore throat
* P = 0.021 compared with group A
Six patients were excluded from analysis because of adverse effects (Table 4). All cases of tongue protrusion-linked cyanosis were associated with difficult ventilation. Hemodynamic data were not different before and after insertion of the CobraPLA.
Table 4.
Adverse effects after using Cobra perilaryngeal airway
| Group | Sex/age (years) | Height/ weight (cm/kg) |
BMI (kg/cm2) | Bloody secretion | Ineffective ventilation | Gastric expansion | Tongue cyanosis/ protrusion |
|||
|---|---|---|---|---|---|---|---|---|---|---|
|
C (n = 4) |
1 | M/40 | 174/85 | 28.1 | o | o | o | |||
| 2 | M/19 | 170/62 | 21.5 | o | ||||||
| 3 | M/39 | 165/84 | 30.9 | o | o | o | o | |||
| 4 | F/54 | 158/72 | 28.8 | o | o | o | ||||
|
A (n = 2) |
5 | M/45 | 180/89 | 27.5 | o | o | o | |||
| 6 | M/49 | 169/70 | 24.5 | o | o | |||||
Cuff pressure was set to 60 cmH2O (group C) or adjusted to minimal seal-up pressure +5 cmH2O (group A). Most sizes of the CobraPLA are #4 except case 2
Discussion
We have shown that individual adjustment of cuff pressure is associated with significant reduction of moderate POST compared with a fixed value such as 60 cmH2O after using CobraPLA.
When the cuff pressures were set to 60 cmH2O, the incidence of POST was reported to range from 0 to 43% [3, 5, 15, 16]. It has been as high as 50% in another study not reporting their cuff pressure value [4]. These varying results suggest that several factors could affect the evaluation of the result. These factors could include insertion method, duration of operation, definition of sore throat, and individual variation of airway space. Of all these factors, only airway space variation could not be controlled in our study. Standard deviation of the cuff volume in both groups is large, which indicates that the volume of hypopharyngeal airway space is individually very varied. Therefore, it is difficult to predict the actual cuff pressure pressing on the surrounding pharyngeal mucosa. If cuff pressure is not adjusted according to the individual size of the upper airway space, we cannot decrease the incidence of POST.
In a previous study using cuffed oropharyngeal airway (COPA), mucosal perfusion was reduced, especially in the posterior pharynx, if the mucosal pressure was over a specific limit value [14]. If it is uncontrolled, a certain part of the cuff pressure might be more forceful to relatively small and less compliant airway space or prominent structures such as the palatine tonsil, tubercles, or folds. If the cuff pressure is more than 34 cmH2O, it could induce a harsher degree of POST [14]; this is one possible explanation of the higher incidence of moderate degree POST in group C. In the clinical setting, change of head position could occur at any time during the surgery, either intentionally or unintentionally. Position change of the head, from neutral to other directions, provokes a cuff pressure change, ranging from 4 to 6 cmH2O [17]. We intended to prevent the leak accompanied by a change of head position during the operation time by increasing the cuff pressure by 5 cmH2O. However, additional cuff pressure might increase the POST incidence in group A.
However, this study cannot completely rule out the effect of the CobraPLA head on the incidence of POST. The CobraPLA head is rigid and bulky enough not to become kinked, which makes its insertion easier but more traumatic, as it may cause a bloody scratch at the pharyngeal mucosa or tonsil. Therefore, we lubricated the head, cuff, and tube with water-soluble gels before insertion, standardized the insertion method, and inspected for the presence of bloody secretions to rule out mucosal injury in both groups. The traumatic effect of the device head might be equally influential in both groups.
It seems that mechanical trauma frequently occurs during the use of the CobraPLA, as most CobraPLA studies are associated with bloody secretions in 10–50% of cases [3–5, 15]. The cuff can produce a bloody scratch as a result of incomplete backward folding during insertion or thorny folding during removal. However, the head of the CobraPLA can also cause a bloody abrasion because it is sharp and bulky. The effect of the head on the incidence of throat lesions needs to be investigated.
We expected that the overall incidence of group A would be lower than that of group C. However, there was a difference only in the moderate degree of POST. This result may have come from our relaxed criteria. Any discomfort and soreness were included in the category of mild degree. When a patient undergoes a short-duration or ambulatory procedure, even mild degree pain or discomfort in the throat area can delay the discharge time and increase the cost because the throat is a part of the airway and swallowing passage. Fortunately, most sore throats are not serious, are not sustained, and are self-limited without needing a special remedy, as in these cases. Only one case in group C had severe degree POST, and the symptom subsided after 8 h without remaining symptoms.
The CobraPLA is increasingly being used for emergent airway management because it is useful as an airway rescuer in patients with limited head extension and it can act as a conduit for tracheal intubation through a large ventilating tube [7–9]. However, the CobraPLA is not recommended for patients with gastroesophageal reflux disease because it is a supraglottic airway device without esophageal sealing capacity [6]. We verified the optimal position of the head with a bronchoscope because herniation of the epiglottis and arytenoid cartilage through the anterior grill of head can occur [18]. Despite this confirmation, five patients had complications such as ineffective ventilation and gastric expansion. In these events, the trachea was immediately intubated to prevent regurgitation and pulmonary aspiration [5]. Possible mechanisms of these adverse effects are position change or rotation of the CobraPLA head, kinked ventilating tube because of warming combined with the heavy corrugated tube or tight bandaging, and relatively larger tongue size compared with the hypopharyngeal space. Fiberoptic scores of the CobraPLA are worse when changing neck position from extension to neutral, flexion, or rotation [17]. In other words, the optimal position of the CobraPLA head can be altered by changing neck position. To prevent these adverse effects, the head position should be maintained at midline as optimized. Use of a bite blocker and less firm bandage fixation of the tube can also help prevent these complications.
The anterior–posterior diameter of the cuff of the CobraPLA is larger than those of other alternative airway devices [17]. Hypopharyngeal location of the huge cuff can provoke tongue protrusion and compress the lingual venous drainage or hypoglossal nerve, causing eventual tongue cyanosis and paresthesia, especially in patients with a small hypopharyngeal airway space [19, 20]. It is therefore necessary to evaluate the size of the hypopharyngeal space and tongue before use of the CobraPLA and to investigate the association of the upper airway measurement with tongue protrusion. Finally, it is important for the anesthesiologist to pay attention to the patient’s head position and the ventilating tube.
Cuff pressure is an excellent predictor of mucosal pressure. If the cuff pressure is higher than 30 cmH2O, mucosal compressing pressure rapidly increases and mucosal color starts to fade [14]. However, care must be taken even in the case of low cuff pressure, as mucosal pressure, can be high especially in the posterior pharynx area [14]. Uncontrolled high cuff pressure combined with large volume can also decrease blood flow in the common carotid artery bulb, especially in the old age group with atheromatous disease [21]. Therefore, even if the incidence of POST is low and self-limited, individual adjustment of cuff pressure is very important, especially in old people, when using the alternative airway device with a large volume cuff.
In conclusion, adjustment of cuff pressure reduces the incidence of moderate POST after use of the CobraPLA.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia. 1999;54(5):444–453. doi: 10.1046/j.1365-2044.1999.00780.x. [DOI] [PubMed] [Google Scholar]
- 2.Reier CE. Bleeding, dysphagia, dysphonia, dysarthria, severe sore throat, and possible recurrent laryngeal, hypoglossal, and lingual nerve injury associated with routine laryngeal mask airway management: where is the vigilance? Anesthesiology 2004;101(5):1241–2; author reply 1242–4. [DOI] [PubMed]
- 3.Galvin EM, van Doorn M, Blazquez J, Ubben JF, Zijlstra FJ, Klein J, Verbrugge SJ. A randomized prospective study comparing the Cobra perilaryngeal airway and Laryngeal Mask Airway-Classic during controlled ventilation for gynecological laparoscopy. Anesth Analg. 2007;104(1):102–105. doi: 10.1213/01.ane.0000246812.21391.d1. [DOI] [PubMed] [Google Scholar]
- 4.Turan A, Kaya G, Koyuncu O, Karamanlioglu B, Pamukcu Z. Comparison of the laryngeal mask (LMA) and laryngeal tube (LT) with the new perilaryngeal airway (CobraPLA) in short surgical procedures. Eur J Anaesthesiol. 2006;23(3):234–238. doi: 10.1017/S0265021505002243. [DOI] [PubMed] [Google Scholar]
- 5.Cook TM, Lowe JM. An evaluation of the Cobra perilaryngeal airway: study halted after two cases of pulmonary aspiration. Anaesthesia. 2005;60(8):791–796. doi: 10.1111/j.1365-2044.2005.04261.x. [DOI] [PubMed] [Google Scholar]
- 6.Jolliffe L, Jackson I. Airway management in the outpatient setting: new devices and techniques. Curr Opin Anaesthesiol. 2008;21(6):719–722. doi: 10.1097/ACO.0b013e328316bb57. [DOI] [PubMed] [Google Scholar]
- 7.Lee JJ, Kim JA, Gwak MS, Kim MH. Evaluation of the Cobra perilaryngeal airway (CPLA) as an airway conduit. Eur J Anaesthesiol. 2007;24(10):852–855. doi: 10.1017/S0265021507000877. [DOI] [PubMed] [Google Scholar]
- 8.Khan RM, Maroof M, Johri A, Ashraf M, Jain D. Cobra PLA can overcome LMA failure in patients with face and neck contractures. Can J Anaesth. 2005;52(3):340. doi: 10.1007/BF03016081. [DOI] [PubMed] [Google Scholar]
- 9.Mezzetti M, Lindenberg P, Rizzi F, Alfery D, Szmuk P. Airway rescue using an “undersized” CobraPLA during cardiopulmonary resuscitation. J Clin Anesth. 2008;20(5):404–405. doi: 10.1016/j.jclinane.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 10.Jensen PJ, Hommelgaard P, Sondergaard P, Eriksen S. Sore throat after operation: influence of tracheal intubation, intracuff pressure and type of cuff. Br J Anaesth. 1982;54(4):453–457. doi: 10.1093/bja/54.4.453. [DOI] [PubMed] [Google Scholar]
- 11.Brimacombe J, Holyoake L, Keller C, Brimacombe N, Scully M, Barry J, Talbutt P, Sartain J, McMahon P. Pharyngolaryngeal, neck, and jaw discomfort after anesthesia with the face mask and laryngeal mask airway at high and low cuff volumes in males and females. Anesthesiology. 2000;93(1):26–31. doi: 10.1097/00000542-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Burgard G, Mollhoff T, Prien T. The effect of laryngeal mask cuff pressure on postoperative sore throat incidence. J Clin Anesth. 1996;8(3):198–201. doi: 10.1016/0952-8180(95)00229-4. [DOI] [PubMed] [Google Scholar]
- 13.Wong JG, Heaney M, Chambers NA, Erb TO, von Ungern-Sternberg BS. Impact of laryngeal mask airway cuff pressures on the incidence of sore throat in children. Paediatr Anaesth. 2009;19(5):464–469. doi: 10.1111/j.1460-9592.2009.02968.x. [DOI] [PubMed] [Google Scholar]
- 14.Brimacombe J, Keller C, Puhringer F. Pharyngeal mucosal pressure and perfusion: a fiberoptic evaluation of the posterior pharynx in anesthetized adult patients with a modified cuffed oropharyngeal airway. Anesthesiology. 1999;91(6):1661–1665. doi: 10.1097/00000542-199912000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Gaitini L, Carmi N, Yanovski B, Tome R, Resnikov I, Gankin I, Somri M, Alfery D. Comparison of the CobraPLA (Cobra Perilaryngeal Airway) and the Laryngeal Mask Airway Unique in children under pressure controlled ventilation. Paediatr Anaesth. 2008;18(4):313–319. doi: 10.1111/j.1460-9592.2008.02449.x. [DOI] [PubMed] [Google Scholar]
- 16.van Zundert A, Al-Shaikh B, Brimacombe J, Koster J, Koning D, Mortier EP. Comparison of three disposable extraglottic airway devices in spontaneously breathing adults: the LMA-Unique, the Soft Seal laryngeal mask, and the Cobra perilaryngeal airway. Anesthesiology. 2006;104(6):1165–1169. doi: 10.1097/00000542-200606000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Park SH, Han SH, Do SH, Kim JW, Kim JH. The influence of head and neck position on the oropharyngeal leak pressure and cuff position of three supraglottic airway devices. Anesth Analg. 2009;108(1):112–117. doi: 10.1213/ane.0b013e318192376f. [DOI] [PubMed] [Google Scholar]
- 18.van Zundert A, Brimacombe J, Kamphuis R, Haanschoten M. The anatomical position of three extraglottic airway devices in patients with clear airways. Anaesthesia. 2006;61(9):891–895. doi: 10.1111/j.1365-2044.2006.04745.x. [DOI] [PubMed] [Google Scholar]
- 19.Nam SB, Chang CH, Lee YW, Lee JS, Yang HG, Jang DJ. Hypoglossal nerve injury following the use of the CobraPLA. Eur J Anaesthesiol. 2007;24(6):556–557. doi: 10.1017/S026502150600216X. [DOI] [PubMed] [Google Scholar]
- 20.Twigg S, Brown JM, Williams R. Swelling and cyanosis of the tongue associated with use of a laryngeal mask airway. Anaesth Intensive Care. 2000;28(4):449–450. doi: 10.1177/0310057X0002800417. [DOI] [PubMed] [Google Scholar]
- 21.Colbert SA, O’Hanlon DM, Flanagan F, Page R, Moriarty DC. The laryngeal mask airway reduces blood flow in the common carotid artery bulb. Can J Anaesth. 1998;45(1):23–27. doi: 10.1007/BF03011987. [DOI] [PubMed] [Google Scholar]