Abstract
Context
Cognitive behavior therapy (CBT) is effective for late-life generalized anxiety disorder (GAD), but, only pilot studies have been conducted in primary care, where older adults most often seek treatment. .
Objective
To examine effects of CBT relative to enhanced usual care (EUC) in older adults with GAD in primary care.
Design, Setting, and Participants
A randomized clinical trial with 134 older adults (mean age, 66.9 years) recruited from March 2004 to August 2006 in two primary care settings. Treatment was provided for 3 months; assessments were conducted at baseline, post-treatment (3 months), and over a 12-month follow-up (6, 9, 12, and 15 months).
Intervention
CBT (n = 70) was conducted in the primary care clinics. Treatment included education and awareness, relaxation training, cognitive therapy, exposure, problem-solving skills training, and behavioral sleep management. Patients assigned to EUC (n = 64) received biweekly calls to ensure patient safety and provide minimal support.
Main Outcome Measures
Primary outcomes included worry severity (Penn State Worry Questionnaire) and GAD severity (GAD Severity Scale).. Secondary outcomes included anxiety (Hamilton Anxiety Rating Scale, Beck Anxiety Inventory), coexistent depressive symptoms (Beck Depression Inventory II), and physical/mental health quality of life (SF-12).
Results
CBT significantly improved worry severity [45.6; 95% CI 44.4 to 47.8; vs. 54.4; 95% CI 51.4 to 57.3; p < .0001), depressive symptoms (10.2; 95% CI 8.5 to 11.9; vs. 12.8; 95% CI 10.5 to 15.1; p = .02), and general mental health (49.6; 95% CI 47.4 to 51.8; vs. 45.3; 95% CI 42.6 to 47.9; p=.008) compared with EUC. . According to intent-to-treat analyses, response rates defined according to worry severity were higher following CBT than EUC at 3 months (40.0% [28/70] vs. 21.9% [14/64], p = .02).
Conclusion
Compared to EUC, CBT resulted in greater improvement in worry severity, depressive symptoms, and general mental health for older patients with GAD in primary care.
Generalized anxiety disorder (GAD) is common in late life, with prevalence up to 7.3%1 in the community and 11.2% in primary care.2 Late-life anxiety predicts increased physical disability; 3 memory difficulties;4 decreased quality of life;5 increased service utilization,6 and mortality.7 Coexistent depressive disorders are common.8 GAD often precedes depression, suggesting it as a risk factor.9
Late-life anxiety is treated usually with medication. Benzodiazepines and antidepressants are effective,10 but associated risks (e.g., falls, hip fractures, memory problems) and patient fear of side-effects limit their utility.11 Older patients also prefer psychosocial interventions.12 Initial outcome studies of cognitive behavior therapy (CBT) for late-life GAD focused on group-based interventions in academic settings.13, 14 Effects were moderate relative to wait-list and minimal-contact controls (d = .71 to .75) and small relative to alternative psychotherapy (d = .20 – .29).14 Treatment response rates were low (28% to 45%)14 but increased over follow-up. Individually administered CBT produced higher effect sizes (.78 to 1.3) and improved response, although sample sizes in these trials were smaller.15, 16
Generalizability of these findings is limited because participants were mostly white, well educated, and healthy. Results also may not be relevant for patients in primary care, where older adults typically present for treatment. CBT within a collaborative-care framework in primary care has been effective for younger patients with panic disorder and/or GAD17 and older patients with depression,18 although effect sizes and treatment-response rates were lower than in academic clinical trials. The late-life anxiety literature lags behind these other areas, with only two pilot studies addressing treatment in primary care.19, 20 These studies suggest benefits for CBT, but sample sizes are small (n = 12 and 31), and conclusions are limited.
We report results of the first randomized clinical trial of CBT for late-life GAD in primary care. We hypothesized that CBT would improve outcomes relative to enhanced usual care (EUC) at post-treatment (3 months) and that gains would be maintained or enhanced over long-term follow-up (from 3 to 15 months).
Method
The study was approved by institutional review boards at The University of Texas Health Sciences Center – Houston (UTHSC-H) and Baylor College of Medicine (BCM). Participants provided written informed consent for all procedures and received compensation of $20 for each completed assessment.
Patient Population
From March 2004 to August 2006, we recruited participants of 60 years or older. Total recruitment duration, however, was for only 26 months because of two 2-month interruptions: (1) in 8/04, the primary academic affiliation of the project changed from UTHSC-H to BCM, and recruitment resumed in 10/04; (2) recruitment was discontinued from 9/05 through 10/05 because of the significant impact of hurricanes Katrina and Rita in the Houston area.
Most recruitment occurred through Kelsey-Seybold Clinic, a large, multi-specialty medical organization in the greater Houston, Texas, area. For 6 months, participants were also recruited from the BCM Family Medicine Clinic (Houston, TX). Recruitment occurred through patient self-referral and physician referral. Educational brochures were placed in waiting and exam rooms, Health Information Centers, and patient newsletters. Informational letters also were mailed to randomly selected patients in the appropriate age range. Physician referrals were encouraged by presentations at staff meetings, electronic communications with providers, and individual networking.
Referred patients were asked two anxiety screening questions from the PRIME-MD.21 Individuals responding affirmatively were scheduled to review informed consent, collect demographic data, and administer the Mini Mental State Exam 22 and the Structured Diagnostic Interview for DSM-IV (SCID).23 Race and ethnicity were identified by the patient according to categories provided by research staff. These data were collected to facilitate conclusions about generalizability of the data. All interviewers administering the SCID (psychology staff, graduate students, interns and fellows) received extensive training. In addition, all interviews were audio- taped, and a second clinician rated 20%. Kappa coefficients suggested adequate diagnostic agreement: GAD (.64); depression (major depression and dysthymia, .75); social phobia (.81); specific phobia (.64). Patients with a principal or co-principal diagnosis of GAD according to DSM-IV were included. Patients with Mini Mental State Exam scores less than 24 were excluded, as were patients with active substance abuse, psychosis, or bipolar disorder.
Measures and Data Collection
Primary Outcomes
Primary outcomes assessed worry and GAD severity. Worry severity was measured with the Penn State Worry Questionnaire (PSWQ),24 a 16-item, self-report scale. GAD severity was evaluated with the Generalized Anxiety Disorder Severity Scale (GADSS),25 a six-item, clinician-rated scale. The PSWQ has good psychometrics among older adults26 and is a primary outcome in psychosocial trials of late-life GAD.27, 28 No minimal clinically significant difference (MCID) has been established for the PSWQ, but prior positive clinical trials have demonstrated a change of 8.5 points on the measure following CBT.28, 29 This value was used here to indicate meaningful change. The GADSS also has adequate psychometric support for older adults, 29 although no data from this measure have been reported from clinical trials of GAD. Here, a change of 2.0 points on the GADSS was considered meaningful, given that a difference of 2 points significantly differentiated patients referred to a clinical trial who did and did not meet criteria for GAD.29
Secondary outcomes
Secondary outcomes assessed coexistent anxiety and depressive symptoms and physical/mental health status. Anxiety severity was measured with the Structured Interview Guide for the Hamilton Anxiety Scale (SIGH-A).30 The SIGH-A has adequate psychometric support among older adults.31 Severity of depressive symptoms was measured with the Beck Depression Inventory, Second Edition (BDI-II).32 The BDI-II has been used with community samples of older adults33 and older adults with anxiety.20 Health quality of life was measured with the 12-item Medical Outcomes Study Short Form, which yields two summary scores developed from the original measure,34 the mental (MCS) and physical component scores .35 Reliability and validity have been established in older adults.36
Usual Care
Medication use was assessed with patient self-report questions about the type and frequency of medications used over the prior 3 months.37, 38 Medications classified as antianxiety (benzodiazepine, buspirone, or other) or antidepressant (selective serotonin reuptake inhibitor, nonselective serotonin reuptake inhibitor, tricyclic antidepressant, or other) were considered. Patients also were asked to report the number of outpatient medical and mental health visits and to indicate whether they had spoken with their doctor about emotional issues or received a mental health referral over the past 3 months.
Data Collection
All outcome measures were administered via telephone by a Masters- or Postdoctoral-level independent evaluator (IE) unaware of treatment assignment. (Given the nature of the intervention and control conditions, patients and therapists were not blind to study condition.) IEs readministered outcome evaluations at 3 months (post-treatment) and at 3-month intervals over a 12-month follow-up. The third author (DN) held regular calibration meetings with IEs. All assessment sessions were audiotaped, and a random 10% were reviewed by a different independent rater. Interrater agreement was excellent (SIGH-A31; GADSS29). Psychometric properties for telephone-based assessment instruments were comparable to in-person versions.39
Intervention
Five experienced therapists provided CBT in up to 10 individual sessions over 12 weeks. Therapists were three Masters-level therapists with at least 2 years of prior CBT experience, one pre-doctoral intern with over 3 years of CBT-anxiety experience, and one post-Bachelor’s-level therapist (PW) with 5 years experience in CBT for late-life anxiety.
Therapist training involved treatment of two nonstudy patients, with competence and adherence ratings of at least 6 on a 0 to 8 scale. CBT included education and awareness, motivational interviewing, relaxation training, cognitive therapy, exposure, problem-solving skills training, and behavioral sleep management.40 Brief telephone booster sessions were offered at 4, 7, 10, and 13 months. Sessions were audiotaped, and 20% were rated by two independent treatment-integrity experts, Drs. Derek Hopko and Gretchen Diefenbach, who co-authored the treatment manual upon which CBT in this study was based. Neither participated in the study in other ways. Ratings suggested excellent adherence (7.7, SD = 0.55; range = 0 to 8) and competence (7.3, SD = 0.67; range = 0 to 8).
Patients in EUC were called biweekly during the first 3 months of the study by the same therapists to provide support and ensure patient safety. Calls last approximately 15 minutes. Therapists reminded patients to call project staff if symptoms worsened and suggested contacting their primary care physician (PCP) for medical problems. A supervisor (MS, NW, MK) and the patient’s PCP were notified of patients needing immediate psychiatric care. All calls were audiotaped, and 20% (n = 93) were reviewed by the first author. Only three protocol deviations were identified.
CBT patients completed an average of 7.4 sessions in the primary care clinic (SD = 1.91). EUC participants received an average of 4.3 telephone check-ins (SD = 1.26). After the first session in each condition, patient expectancy was assessed with a single item asking patients to rate the amount of improvement they expected (0%= none; 100%=complete improvement).41 Communication with the PCP occurred via notes filed in the research section of the written medical record. Initial notes indicated diagnoses assigned and inclusion/exclusion status. For excluded patients, potential referrals were provided to the PCP and the patient. For included patients, notes encouraged care as usual and indicated whether patients had received a CBT session or an EUC contact.
Randomization
Patients were randomized initially according to a 1:1 ratio within blocks of 10 to CBT or EUC. More patients were randomized to CBT (n=70) than EUC (n=64). Inspection of data at study mid-point (50% recruitment completed) revealed a disproportionate random assignment of Hispanic patients to EUC. A stratified randomization schedule was then instituted for Hispanic patients, with 80% assignment to CBT, to ensure equivalence across groups. Non-Hispanic patients were maintained on the original 1:1 randomization schedule. The randomization scheme was generated by the study statistician (HR) using a random number generator; and assignments were placed in numbered, sealed envelopes. Upon completion of baseline assessment, a study research assistant opened the next envelope in sequence and assigned the participant to a treatment condition.
Data Analysis
Before conducting outcome analyses, we compared patients in the CBT and EUC subgroups on pretreatment demographic variables, clinical characteristics, and medication utilization, using Chi-square analyses and t-tests. Primary analyses then examined post-treatment outcomes by comparing group differences at 3 months, using a between-groups analysis of covariance (ANCOVA), with pretreatment assessment as the covariate. Initial analyses were intent-to-treat (ITT), using the SAS multiple imputation procedures, Proc MI and MIANALYZE, version 9.2, to address missing data. Another set of analyses repeated these comparisons only with observed data, using random regression methods (i.e., completer analysis using SAS’s Proc Mixed). Secondary analyses examined long-term outcomes with a repeated-measures–analysis-of-covariance procedure (SAS’s Proc Mixed), again with the pretreatment assessment as the covariate. To control for multiple comparisons within clusters of outcomes (primary outcomes, coexistent anxiety-depression, health quality of life), each of which included two variables, critical alpha was set at p< .025. All significance testing was two-sided.
Because three couples participated in the study (with both partners randomized to the same condition; n = 2 in CBT, n = 1 in EUC), all analyses were rerun with one individual from each couple randomly removed to assess the possible influence of correlated data. These analyses did not result in different findings and therefore are omitted. Finally, changes in the use of antidepressant and antianxiety medications during the trial were examined with Chi-square analyses, and exploratory analyses examined the role of expectancies in predicting outcome.
Treatment response was defined by meaningful change on the PSWQ and GADSS, as defined earlier (PSWQ=8.5; GADSS=2.0); see Primary Outcomes). The proportions of patients classified as treatment responders according to these cut-offs were determined at 3 and 15 months. Group differences in ITT and completer samples were tested, using Chi-square analyses. For ITT analyses, patients with missing data were classified as nonresponders.
Power calculations were based on the PSWQ, which is a primary outcome in CBT trials of late-life GAD. Median standard deviation across these trials is 10.1. This figure was considered in combination with an expected moderate effect size (d=.60, minimal detectable difference = 6.2), desired 80% power, and alpha of .025. Given these parameters and a potential 30% attrition, our goal was to include 150 participants so that 53 per group would be available for analysis. The included sample (n = 148) was 99% of this target. The randomized sample (n = 70 CBT, n = 64 EUC) and the completer sample (n = 115) both exceeded the required 53 per group.
Results
Sample Selection and Attrition
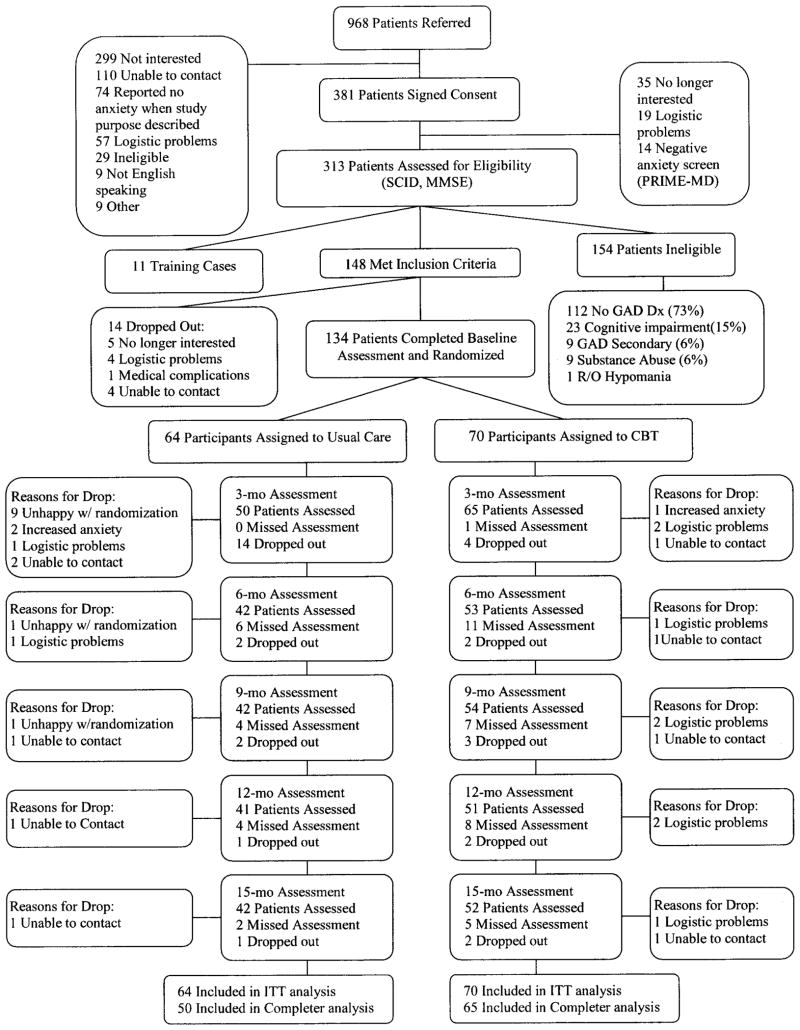
A total of 968 potential participants were referred (75% self-referred), and 381 provided consent (see Figure 1). Of these, 68 (18%) dropped out or were excluded before diagnostic evaluation because of negative responses to PRIME-MD screening questions (n = 14), lack of interest (n = 35), or logistic problems (n = 19). Of the remaining 313 patients, 11 were included as nonstudy clinical-training cases, and 154 were excluded. A total of 148 patients met inclusion criteria (95% self-referred); 14 (9%) dropped out before randomization, leaving 134 patients with principal (n = 86) or co-principal (n = 48) GAD for randomization.
Figure 1.
Diagram of flow of participants through each phase of the study. Patients who dropped out of the study did not participate in subsequent assessments, but patients who could not be contacted at one assessment were allowed to participate in subsequent assessments.
Relative to patients who provided consent but were not randomized (n=247), randomized patients (n=134) were younger (66.9 years; 95% confidence interval [CI], 65.9 to 67.9; vs. 69.0 years; 95% CI, 68.2 to 69.9; p=.002), more educated (15.9 years; 95% CI, 15.4 to 16.4; vs. 15.1 years; 95% CI, 14.7 to 15.5; p=.02), and more likely to be women (75% [105/134] vs. 68% [168/246]; p<.04). Randomized patients also had higher baseline PSWQ scores than other patients for whom baseline severity data were available (n=167) (57.2; 95% CI, 55.4 to 59.0; 46.5; 95% CI, 44.6 to 48.3; p<.0001).
Dropout during active treatment (0 to 3 months) was significantly lower for CBT than EUC (5.9% [4/70] vs. 21.9% [14/64]; p=.006] primarily because of self-reported dissatisfaction with random assignment (EUC: n = 9; CBT: n = 0). Attrition over long-term follow-up (3 to 15 months) was comparable for CBT and EUC (CBT: 12.9% [9/70]; EUC: 9.4% [6/64], ns). Total attrition over 15 months was 24.6% (n = 33) and did not differ significantly between groups (18.6% [13/70]; ; EUC: 31.3% [20/64]; p=.09) . Reasons for drop are described in Figure 1. ANOVAs revealed no group (CBT, EUC) x drop status differences on any baseline measure.
Sample Characteristics and Pretreatment Comparisons
Sample characteristics are included in Table 1. Patients in CBT and EUC differed with regard to baseline PSWQ scores (see Table 1). Analyses of primary outcomes (PSWQ, GADSS) included baseline PSWQ as a covariate.
Table 1.
Baseline sociodemographic and clinical characteristics by intervention status
| Overall (N = 134) | CBT (n = 70) | EUC (n = 64) | pValue | |
|---|---|---|---|---|
| Age (SD) | 66.9 (5.79) | 66.6 (5.93) | 67.3 (5.66) | .54 |
| Education (SD) | 15.9 (3.01) | 16.1 (2.93) | 15.7 (3.10) | .47 |
| Female, No. (%) | 105 (78.4) | 56 (80) | 49 (76.6) | .63 |
| Race and Ethnicity, No. (%) | .40 | |||
| Non-Hispanic Caucasian | 94(70.2) | 49(70.0) | 45(70.3) | |
| African American | 25 (18.7) | 12(17.1) | 13(20.3) | |
| Hispanic | 11(8.2) | 5(7.1) | 6(9.4) | |
| Asian | 3(2.2) | 3(4.3) | 0(0.0) | |
| Mixed | 1(6.8) | 1(1.4) | 0(0.0) | |
| Marital Status, No. (%) | .16 | |||
| Never Married | 2 (1.49) | 0 | 2 (3.13) | |
| Married | 83 (61.9) | 40 (57.14) | 43 (67.19) | |
| Separated/Divorced | 31 (23.1) | 17 (24.29) | 14 (21.88) | |
| Widowed | 18 (13.43) | 13 (18.57) | 5 (7.81) | |
| Job Status, No. (%) | .54 | |||
| Retired | 74 (55.2) | 42 (60) | 32 (50) | |
| Employed Full-time or Part-time | 48 (35.8) | 23 (32.9) | 25 (39.1) | |
| Homemaker | 7 (5.2) | 4 (5.7) | 3 (4.7) | |
| Unemployed | 5 (3.7) | 1 (1.4) | 4 (6.3) | |
| PSWQ (SD)** | 55.3 (10.90) | 53.3 (10.57) | 57.6 (10.91) | .02 |
| GADSS (SD)** | 11.3 (3.50) | 11.4 (3.60) | 11.3 (3.42) | .88 |
| SIGH-A (SD)** | 19.3 (7.77) | 19.4 (7.72) | 19.1 (7.89) | .79 |
| BDI (SD)** | 16.4 (8.72) | 16.3 (8.00) | 16.4 (11.51) | .95 |
| SF-12 MCS (SD)++ | 42.0 (9.69) | 42.4 (9.96) | 41.7 (9.45) | .69 |
| SF-12 PCS (SD)++ | 44.1 (8.35) | 44.0 (8.51) | 44.2 (8.24) | .84 |
| Presence of Coexistent Diagnosis, No. (%) | 96 (71.6) | 55 (78.6) | 41 (64.1) | .06 |
| Any Coexistent Anxiety, No (%) | 54 (40.3) | 33 (47.1) | 21 (32.8) | .09 |
| Any Coexistent Depression, No (%) | 60 (44.8) | 33(47.1) | 27(42.2) | .56 |
| Number of Medical Diagnoses (SD) | 2.6 (1.82) | 2.7 (1.77) | 2.5 (1.89) | .73 |
| Use of Psychotropic Medications, No. (%) | 56 (42) | 28 (40) | 28 (43.8) | .66 |
| Antianxiety Medication, No. (%) | 23 (17) | 12 (17) | 11 (17) | .99 |
| Antidepressant Medication, No. (%) | 41 (31) | 24 (34) | 17 (27) | .33 |
Abbreviations: CBT, cognitive behavior therapy; EUC, enhanced usual care; PSWQ, Penn State Worry Questionnaire; GADSS, Generalized Anxiety Disorder Severity
Scale; SIGH-A, Structured Interview Guidelines for the Hamilton Anxiety
Rating Scale; BDI, Beck Depression Inventory; SF-12 MCS,
Medical Outcomes Study Short Form Mental Component Scale; SF-12 PCS, Medical Outcomes Study
Short Form Physical Component Scale
Higher scores indicate more severe symptoms.
Higher scores indicate better health-related quality of life.
p value indicates comparison of participants in CBT and EUC groups (t-tests or Chi-square tests)
Post-treatment Outcomes (0 to 3 months)
Mean observed scores at 0 and 3 months are presented in Table 2. Imputed means and CI were not statistically or substantially different from observed values.
Table 2.
Mean scores (and standard deviations) on measures of secondary outcomes across time for patients in CBT or EUC.
| Treatment Effect | Treatment Effect | Time Effect | Treatment x Time Effect | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline (N = 134) | 3-Mo (N = 115) | F | p | d (95 % CIs) | 6-Mo (N = 95) | 9-Mo (N = 96) | 12-Mo (N = 92) | 15-Mo (N = 94) | F | p | F | p | F | p | ||
| PSWQ | CBT | 53.3 (10.6) | 45.6 (8.9) | 19.01 | <.00 01 | .85 (.49, 1.20) | 44.1 (9.4) | 44.0 (8.1) | 42.5 (9.3) | 42.8 (9.1) | 15.12 | .0002 | 4.53 | .002 | 1.88 | .12 |
| EUC | 57.6 (10.9) | 54.4 (10.6) | 52.7 (10.7) | 50.4 (11.0) | 50.9 (12.0) | 50.8 (11.8) | ||||||||||
| GADSS | CBT | 11.4 (3.6) | 8.6 (3.6) | 1.77 | .19 | .27 (−.07, .61) | 8.6 (3.9) | 8.6 (4.3) | 8.5 (3.8) | 8.7 (4.7) | 1.75 | .19 | .10 | .98 | .14 | .97 |
| EUC | 11.3 (3.4) | 9.9 (4.5) | 9.7 (4.7) | 9.6 (5.1) | 9.2 (4.7) | 9.5 (4.5) | ||||||||||
| SIGH-A | CBT | 19.4 (7.7) | 15.1 (7.5) | 1.45 | .23 | .13 (−.21, .47) | 14.5 (7.7) | 13.6 (8.0) | 13.2 (6.6) | 13.9 (8.2) | 2.64 | .11 | .70 | .60 | .77 | .55 |
| EUC | 19.1 (7.9) | 16.1 (7.4) | 16.2 (8.6) | 15.9 (8.8) | 15.7 (7.9) | 15.1 (8.0) | ||||||||||
| BDI | CBT | 16.3 (8.0) | 10.2 (7.0) | 5.9 | .02 | .34 (.00, .68) | 9.3 (7.1) | 9.7 (7.2) | 8.5 (6.8) | 8.3 (7.3) | 4.67 | .03 | 2.11 | .08 | 1.66 | .16 |
| EUC | 16.4 (9.5) | 12.8 (8.3) | 10.9 (8.4) | 10.3 (7.0) | 10.1 (6.9) | 11.4 (7.3) | ||||||||||
| SF-12 MCS | CBT | 42.4 (10.0) | 49.6 (8.9) | 7.45 | .008 | .48 (.14, .83) | 51.2 (8.4) | 48.4 (9.3) | 50.2 (8.0) | 50.3 (8.4) | 5.42 | .02 | 1.61 | .18 | .81 | .52 |
| EUC | 41.7 (9.5) | 45.3 (9.4) | 47.4 (10.4) | 48.1 (10.3) | 47.5 (10.2) | 47.0 (10.6) | ||||||||||
| SF-12 PCS | CBT | 44.0 (8.5) | 41.6 (7.9) | .03 | .87 | .08 (−.26, .42) | 42.4 (7.7) | 42.7 (7.6) | 41.5 (6.7) | 42.1 (7.1) | .20 | .66 | .56 | .69 | .26 | .90 |
| EUC | 44.3 (8.2) | 41.8 (9.6) | 40.5 (10.2) | 42.6 (8.5) | 41.7 (8.3) | 41.8 (7.9) | ||||||||||
Abbreviations: CBT, cognitive behavior therapy; EUC, enhanced usual care; BDI, Beck Depression Inventory – 11; Medical Outcomes Study Short Form; MCS, Mental Component Scale; PCS, Physical Component Scale; QOLI; Quality of Life Intervention.
NOTE: All means are observed means (corresponding Ns are noted).
Primary outcomes
ITT analyses indicated significantly greater improvement in CBT than EUC on the PSWQ [45.6; 95% CI 41.3 to 47.8; vs. 54.4; 95% CI 51.4 to 57.3; p<.0001; see Table 2]. Mean change was 7.7 points in CBT and 3.2 points in EUC. Group differences on the GADSS were not significant, with mean change of 2.8 points in CBT and 1.4 points in EUC. Completer analyses resulted in the same pattern of statistical results.
Secondary outcomes
ITT analyses suggested significantly greater improvement in CBT than EUC on the BDI [10.2; 95% CI 8.5 to 11.9; vs. 12.8; 95% CI 10.5 to 15.1; p=.02] and MCS [49.6; 95% CI 47.4 to 51.8; vs. 45.3; 95% CI 42.6 to 47.9; p=.008] (see Table 2). Changes on the SIGH-A and PCS were not significantly different between groups. Completer analyses suggested similar patterns of results.
Usual Care
Patients who completed CBT and EUC did not differentially add or increase dosages of anti-anxiety medication during active treatment (4.6% [3/65] vs. 2.0% [1/50], ns). Rates of discontinuation or reduced dosages of these medications also were equivalent across groups (7.7% [5/65] vs. 4.0% [2/50], ns). Similarly, rates of increased doses or new antidepressant medication (12.3% [8/65] vs. 6.0% [3/50], ns) and decreased doses or medication discontinuation (7.7% [5/65] vs. 2.0% [1/50], ns) were similar in CBT and EUC. Patients in the two groups also had equivalent numbers of outpatient medical visits (2.7, 95% CI, 2.1 to 3.2; vs. 2.3, 95% CI, 1.6 to 3.0, p=.85) and similarly infrequent mental health visits (0.5, 95% CI, 0.0 to 1.0; vs. 0.7, 95% CI, 0.2 to 1.3, p=.82). Very few patients in either condition received a mental health referal (7.7% [5/65] vs. 8.0% [4/50]; p=.95) or talked with their doctor about emotional problems (20.0% [13/65] vs. 18.0% [9/50], p=.82).
Long-term Outcomes (3 to 15 Months)
Primary outcomes
Analyses indicated continued improvement in PSWQ scores over long-term follow-up for patients in both groups [time effect: see Table 2]. Covariate-adjusted post-treatment group differences also continued over the long term for the PSWQ [group effect: see Table 2]. These differences suggest that no additional, differential group response was seen and that the initial treatment effectiveness at the end of active treatment was improved throughout the 12-month follow-up.
Secondary outcomes
Post-treatment effects on the BDI and MCS were maintained over the subsequent 12 months (Group effects; see Table 2). Patients who completed CBT and EUC did not increase doses or add antianxiety medication at different rates over 3 to 15 months (12.5% [8/64] vs. 16.7% [8/48]; p=.53). Rates of decreasing doses or discontinuation of these medications also were equivalent (14.1% [9/64] vs. 16.7% [8/48], p=.70). Antidepressant medications also were added or doses increased (18.8% [12/64] vs. 14.6% [7/48], p=.56) and discontinued or doses reduced (18.8% [12/64] vs. 12.5% [6/48], p=.37) at similar rates over long-term follow-up.
Treatment Response Rates
Mean percentages of treatment responders according to ITT analyses of meaningful change scores (PSWQ=8.5; GADSS=2.0) are reported in Table 3. Treatment response rates according to the PSWQ were higher in CBT than EUC at 3months. Completer analyses revealed no group differences at 3 or 15 months.
Table 3.
Mean percentages of patients classified as treatment responders according to meaningful change scores on the PSWQ (8.5) and the GADSS (2.0) at 3 and 15 months
| CBT (n = 70) | EUC (n = 64) | X2 | P Value | |
|---|---|---|---|---|
| PSWQ | ||||
| 3 months | 28 (40.0% | 14 (21.9%) | 5.10 | .02 |
| 15 months | 29 (41.4%) | 17 (26.6%) | 3.28 | .07 |
| GADSS | ||||
| 3 months | 38 (54.3%) | 31 (48.4%) | .46 | .50 |
| 15 months | 29 (41.4%) | 24 (37.5%) | .22 | .64 |
CBT, cognitive behavior therapy; EUC, enhanced usual care; PSWQ, Penn State Worry Questionnaire; GADSS, Generalized Anxiety Disorder Severity Scale.
Treatment Expectancies
Average treatment expectancies were significantly higher for patients who completed CBT than for those who completed EUC (78% expected improvement, 95% CI, 74 to 83; vs. 66% expected improvement, 95% CI, 58 to 74, p=.007). When expectancies were added to the previously tested models as covariates, effects for treatment remained significant for PSWQ (p<.001), but group differences on the BDI (p=.05) and MCS (p=.04) only approached significance.
Comment
This study is the first to suggest that CBT can be useful for managing worry and associated symptoms among older patients in primary care. Patients in CBT had greater reductions in worry, depressive symptoms and general mental health than patients in EUC. Mean change in worry severity over time was slightly lower than in other clinical trials of CBT for late-life anxiety.28, 29 Mean change in GAD severity following CBT was meaningful but not significantly different than usual care. Effect sizes for symptom improvement were comparable to or greater than those in primary care studies of younger adults with GAD or panic disorder 17, 42 and older adults with depression.18 Positive findings in this trial are particularly notable, given that other primary care studies involve full collaborative-care models incorporating both medication and cognitive behavioral treatments. Here, comparable effects were found with CBT alone, as in a subset of data from the IMPACT trial.43 Findings here also are the first to demonstrate positive effects of treatment for GAD in primary care. A subset of data from Rollman, et al.17 showed no significant benefits of collaborative care for young patients with GAD only (without coexistent panic disorder) relative to UC. In the current trial, post-treatment symptom improvements were maintained or improved over one-year follow-up.
Treatment response rates based on worry severity (PSWQ) were higher in CBT than EUC at 3 months, but treatment-group differences were not maintained at 15 months. Patterns of response suggest maintenance of gains in CBT but a slight increase in treatment response for usual care. Increased booster sessions over the long term might be beneficial for continued improvement following CBT.
The GADSS failed to demonstrate treatment effects, suggesting a potential limitation of this measure for late-life GAD. Exploratory analysis also suggested a meaningful role of expectances on secondary outcomes. Future work is needed to examine more fully possible moderator and mediator variables in response to CBT.
Significant strengths of this study include careful selection and diagnosis of patients, breadth of outcome assessment, excellent treatment integrity, low attrition in CBT (6%), and significant improvement in both primary and secondary outcomes. Certain design features, however, limit translational value and potential sustainability for primary care settings. First, the sample was not representative of older patients in primary care with regard to age, gender and education. Moreover, randomized patients were younger, more, highly educated, and more likely to be women than non-randomized patients.. These characteristics may reflect both the recruitment setting (insurance-based care) and the self-referred nature of most participants. Primary care patients with anxiety recruited through physician referral using electronic–medical-record (EMR) prompts are more diverse demographically and have higher levels of anxiety.44 Second, clinicians providing CBT and EUC had significant expertise in late-life anxiety and CBT. Treatment also was delivered during weekly in-person sessions of approximately 1 hour. This type of service is rarely available in primary care. Finally, communication with PCPs was limited to written notes in a research section of the medical record. No EMR was available to facilitate treatment integration with ongoing care.
CBT is useful for older adults with GAD in primary care. This study paves the way for future research to test sustainable models of care in more demographically heterogeneous groups. In future studies, it will be important to examine the impact of treatment delivered by providers without specialized CBT expertise. Improved integration with ongoing care would be facilitated through use of an EMR to identify patients and communicate with providers,39 and collaborative models of care that incorporate both CBT and medication need to be tested.
Acknowledgments
Funding/Support:
This research was supported by a grant from the National Institute of Mental Health (NIMH) (R01-MH53932) to the first author and by the Houston VA HSR&D Center of Excellence (Houston Center for Quality of Care & Utilization Studies [HFP90-020]). The authors would like to thank Gretchen Diefenbach, Ph.D., Hartford Institute of Living, and Derek Hopko, Ph.D., University of Tennessee–Knoxville,, who provided ratings of treatment integrity; and Bruce Rollman, M.D., University of Pittsburgh, and Patricia Areán, Ph.D., University of California – San Francisco, who served as consultants for this study. These individuals received financial compensation from the grants for their contributions. The authors also appreciate the input of three anonymous reviewers, who received no compensation.
Role of Sponsor:
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH, the National Institutes of Health, or the Veterans Administration or Baylor College of Medicine. The NIMH had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript.
Footnotes
Financial Disclosures:
None of the authors has any conflict of interest to disclose.
Trial Registration: clinicaltrials.gov Identifier: NCT00308724
Author Citations:
Dr. Stanley had full access to all data in the study and takes responsibility for its integrity and the accuracy of the data analyses.
Study Concept and Design: Stanley, Wilson, Novy, Rhoades, Kunik.
Acquisition of the Data: Stanley, Wilson, Novy, Wagener, Greisinger, Kunik.
Analysis and Interpretation of the Data: Stanley, Novy, Rhoades, Wagener, Cully, Kunik.
Drafting of the Manuscript: Stanley, Rhoades, Wagener.
Critical Revision of the Manuscript for Important Intellectual Content: Stanley, Wilson, Novy, Rhoades, Wagener, Greisinger, Cully, Kunik.
Statistical Analysis: Rhoades, Wagener.
Obtained Funding: Stanley, Wilson, Kunik.
Administrative, Technical, or Material Support: Wagener, Greisinger.
Study Supervision: Stanley, Wilson, Novy, Kunik.
Final review of manuscript: Stanley, Wilson, Novy, Rhoades, Wagener, Greisinger, Cully, Kunik
Reference List
- 1.Beekman AT, Bremmer MA, Deeg DJ, et al. Anxiety disorders in later life: report from the Longitudinal Aging Study Amsterdam. Int J Geriatr Psychiatry. 1998 Oct;13(10):717–26. doi: 10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 2.Tolin DF, Robison JT, Gaztambide S, Blank K. Anxiety disorders in older Puerto Rican primary care patients. Am J Geriatr Psychiatry. 2005 Feb;13(2):150–6. doi: 10.1176/appi.ajgp.13.2.150. [DOI] [PubMed] [Google Scholar]
- 3.Brenes GA, Guralnik JM, Williamson JD, et al. The influence of anxiety on the progression of disability. J Am Geriatr Soc. 2005 Jan;53(1):34–9. doi: 10.1111/j.1532-5415.2005.53007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mantella RC, Butters MA, Dew MA, et al. Cognitive impairment in late-life generalized anxiety disorder. Am J Geriatr Psychiatry. 2007 Aug;15(8):673–9. doi: 10.1097/JGP.0b013e31803111f2. [DOI] [PubMed] [Google Scholar]
- 5.Wetherell JL, Thorp SR, Patterson TL, Golshan S, Jeste DV, Gatz M. Quality of life in geriatric generalized anxiety disorder: A preliminary investigation. J Psychiatr Res. 2004 May;38(3):305–12. doi: 10.1016/j.jpsychires.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Stanley MA, Roberts RE, Bourland SL, Novy DM. Anxiety disorders among older primary care patients. J Clin Geropyschology. 2001;(7):105–16. [Google Scholar]
- 7.Brenes GA, Kritchevsky SB, Mehta KM, et al. Scared to death: results from the Health, Aging, and Body Composition study. Am J Geriatr Psychiatry. 2007 Mar;15(3):262–5. doi: 10.1097/JGP.0b013e31802e21f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beekman AT, de Beurs E, van Balkom AJ, Deeg DJ, van Dyck R, van Tilburg W. Anxiety and depression in later life: Co-occurrence and communality of risk factors. Am J Psychiatry. 2000 Jan;157(1):89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- 9.Schoevers RA, Deeg DJ, van Tilburg W, et al. Depression and generalized anxiety disorder: Co-occurrence and longitudinal patterns in elderly patients. Am J Geriatr Psychiatry. 2005 Jan;13(1):31–9. doi: 10.1176/appi.ajgp.13.1.31. [DOI] [PubMed] [Google Scholar]
- 10.Pinquart M, Duberstein PR. Treatment of anxiety disorders in older adults: a meta-analytic comparison of behavioral and pharmacological interventions. Am J Geriatr Psychiatry. 2007 Aug;15(8):639–51. doi: 10.1097/JGP.0b013e31806841c8. [DOI] [PubMed] [Google Scholar]
- 11.Allain H, tue-Ferrer D, Polard E, Akwa Y, Patat A. Postural instability and consequent falls and hip fractures associated with use of hypnotics in the elderly: a comparative review. Drugs Aging. 2005;22(9):749–65. doi: 10.2165/00002512-200522090-00004. [DOI] [PubMed] [Google Scholar]
- 12.Gum AM, Arean PA, Hunkeler E, et al. Depression treatment preferences in older primary care patients. Gerontologist. 2006;46(1):14–22. doi: 10.1093/geront/46.1.14. [DOI] [PubMed] [Google Scholar]
- 13.Hendricks GJ, Oude Voshaar RC, Keijsers GP, Hoogduin CA, van Balkom AJ. Cognitive-behavioural therapy for late-life anxiety disorders: a systematic review and meta-analysis. Acta Psychiatr Scand. 2008 Jun;117(6):403–11. doi: 10.1111/j.1600-0447.2008.01190.x. [DOI] [PubMed] [Google Scholar]
- 14.Wetherell JL, Lenze EJ, Stanley MA. Evidence-based treatment of geriatric anxiety disorders. Psychiatr Clin North Am. 2005 Dec;28(4):871–96. doi: 10.1016/j.psc.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Mohlman J, Gorenstein EE, Kleber M, de JM, Gorman JM, Papp LA. Standard and enhanced cognitive-behavior therapy for late-life generalized anxiety disorder: Two pilot investigations. Am J Geriatr Psychiatry. 2003 Jan;11(1):24–32. [PubMed] [Google Scholar]
- 16.Mohlman J, Gorman JM. The role of executive functioning in CBT: A pilot study with anxious older adults. Behav Res Ther. 2005 Apr;43(4):447–65. doi: 10.1016/j.brat.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 17.Rollman BL, Belnap BH, Mazumdar S, et al. A randomized trial to improve the quality of treatment for panic and generalized anxiety disorders in primary care. Arch Gen Psychiatry. 2005;62(12):1332–41. doi: 10.1001/archpsyc.62.12.1332. [DOI] [PubMed] [Google Scholar]
- 18.Gilbody S, Bower P, Fletcher J, et al. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006 Nov 27;166(21):2314–21. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 19.Stanley MA, Hopko DR, Diefenbach GJ, Bourland SL, Rodriguez H, Wagener P. Cognitive-behavior therapy for late-life generalized anxiety disorder in primary care: Preliminary findings. Am J Geriatr Psychiatry. 2003 Jan;11(1):92–6. [PubMed] [Google Scholar]
- 20.Wetherell JL, Ayers CR, Sorrell JT, et al. Modular psychotherapy for anxiety in older primary care patients. American Journal of Geriatric Psychiatry. 2009 doi: 10.1097/JGP.0b013e3181a31fb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994 Dec 14;272(22):1749–56. [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.First MB, Spitzer RL, Miriam G, Williams JBW. Structured clinical interview for DSM-IV axis I disorders, research version, patient edition with psychotic. New York: Biometrics Research, New York State Psychiatric Institute; 1997. [Google Scholar]
- 24.Meyer T, Metzger R, Borkovec TD. Development and validity of the Penn State Worry Scale. Behav Res Ther. 1990;28(6):487–95. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 25.Shear MK, Belnap BH, Mazumdar S, Houck P, Rollman BL. Generalized anxiety disorder severity scale (GADSS): A preliminary validation study. Depress Anxiety. 2006;23(2):77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- 26.Hopko DR, Stanley MA, Reas DL, et al. Assessing worry in older adults: Confirmatory factor analysis of the Penn State Worry Questionnaire and psychometric properties of an abbreviated model. Psychol Assess. 2003 Jun;15(2):173–83. doi: 10.1037/1040-3590.15.2.173. [DOI] [PubMed] [Google Scholar]
- 27.Stanley MA, Beck JG, Novy DM, et al. Cognitive-behavioral treatment of late-life generalized anxiety disorder. J Consult Clin Psychol. 2003;71(2):309–19. doi: 10.1037/0022-006x.71.2.309. [DOI] [PubMed] [Google Scholar]
- 28.Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003 Feb;71(1):31–40. doi: 10.1037//0022-006x.71.1.31. [DOI] [PubMed] [Google Scholar]
- 29.Weiss B, Calleo J, Rhoades H, et al. The utility of generalized anxiety disorder severity scale (GADSS) with older adults in primary care. Depress Anxiety. 2009;26(1):E10–E15. doi: 10.1002/da.20520. Ref Type: Generic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shear MK, Vander BJ, Rucci P, et al. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depress Anxiety. 2001;13(4):166–78. [PubMed] [Google Scholar]
- 31.Skopp NA, Novy D, Kunik ME, et al. Investigation of cognitive behavior therapy. Am J Geriatr Psychiatry. 2006;14(3):282. doi: 10.1097/01.JGP.0000192505.56434.7e. [DOI] [PubMed] [Google Scholar]
- 32.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 33.Segal DL, Coolidge FL, Cahill BS, O’Riley AA. Psychometric properties of the Beck Depression Inventory II (BDI-II) among community-dwelling older adults. Behav Modif. 2008 Jan;32(1):3–20. doi: 10.1177/0145445507303833. [DOI] [PubMed] [Google Scholar]
- 34.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–83. [PubMed] [Google Scholar]
- 35.Jenkinson C, Layte R, Jenkinson D, et al. A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med. 1997 Jun;19(2):179–86. doi: 10.1093/oxfordjournals.pubmed.a024606. [DOI] [PubMed] [Google Scholar]
- 36.McHorney CA. Measuring and monitoring general health status in elderly persons: practical and methodological issues in using the SF-36 Health Survey. Gerontologist. 1996 Oct;36(5):571–83. doi: 10.1093/geront/36.5.571. [DOI] [PubMed] [Google Scholar]
- 37.Wells KB. The design of partners in care: evaluating the cost-effectiveness of improving care for depression in primary care. Soc Psychiatr Epidemiol. 1999;34:20–9. doi: 10.1007/s001270050107. [DOI] [PubMed] [Google Scholar]
- 38.Wells KB, Sherbourne CD, Schoenbaum M, et al. Five-year impact of quality improvement for depression: results of randomized controlled trial. Arch of Gen Psychiatry. 2004;61:378–85. doi: 10.1001/archpsyc.61.4.378. [DOI] [PubMed] [Google Scholar]
- 39.Senior AC, Kunik ME, Rhoades HM, Novy DM, Wilson NL, Stanley MA. Utility of telephone assessments in an older adult population. Psychol Aging. 2007 Jun;22(2):392–7. doi: 10.1037/0882-7974.22.2.392. [DOI] [PubMed] [Google Scholar]
- 40.Stanley MA, Diefenbach GJ, Hopko DR. Cognitive behavioral treatment for older adults with generalized anxiety disorder. A therapist manual for primary care settings. Behav Modif. 2004 Jan;28(1):73–117. doi: 10.1177/0145445503259259. [DOI] [PubMed] [Google Scholar]
- 41.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy. 1972;3:257–60. [Google Scholar]
- 42.Roy-Byrne PP, Craske MG, Stein MB, et al. A randomized effectiveness trial of cognitive-behavioral therapy and medication for primary care panic disorder. Arch Gen Psychiatry. 2005 Mar;62(3):290–8. doi: 10.1001/archpsyc.62.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arean PA, Hegel MT, Vannoy S, Fan M-Y, Unutzer J. Effectivness of problem-solving therapy for older primary care patients with depression. Gerontologist. 2008;48(3):311–23. doi: 10.1093/geront/48.3.311. [DOI] [PubMed] [Google Scholar]
- 44.Rollman BL, Fischer GS, Zhu F, Belnap BH. Comparison of electronic physician prompts versus waitroom case-finding on clinical trial enrollment. J Gen Intern Med. 2008 Apr;23(4):447–50. doi: 10.1007/s11606-007-0449-0. [DOI] [PMC free article] [PubMed] [Google Scholar]