Abstract
This study examined whether children who become homeless differ from other low-income children in their mental health service use before and after their first homeless episode, and to what extent homelessness is associated with an increased likelihood of mental health service use. Differences between children with and without new onset of sheltered homelessness in the use of mental health services emerged following homelessness and widened over time. Sheltered homelessness and foster care placement history were associated with increased odds of receiving inpatient and ambulatory mental health services. Findings underscore the importance of collaborations between homeless assistance, foster care, and mental healthcare in efforts to mitigate family homelessness and collateral needs among homeless children.
Introduction
Between 12% and 47% of children in homeless families experience mental health problems, a proportion that changes depending on the age of children, assessment measures, and geographic area (Bassuk et al., 1997; Buckner, Bassuk, Weinreb, & Brooks, 1999; Grant et al., 2007; San Agustin et al., 1999; Yu, LaVesser, Osborne, & Spitznagel, 2008; Zima, Wells, & Freeman, 1994). While the extent of mental health problems among homeless children is greater than that of the general population, there is mixed evidence as to whether children experiencing homelessness differ from low-income housed children on mental health outcomes. Children in poverty, regardless of their housing status, share many of the same risk factors that contribute to their risk for mental disorders (Masten, Miliotis, Graham-Bermann, Ramirez, & Neeman, 1993; Rafferty & Shinn, 1991), and it is, therefore, difficult to tease out any additional risk for such disorders that might be attributed to experiencing homelessness (Rog & Buckner, 2007). A comprehensive review of published studies between 1987 and 2004 shows that five studies reported more mental health problems among homeless children compared to the low-income housed group, whereas four studies found no significant differences between the two groups (Buckner, 2008).
Assessing the impact of homelessness on the receipt of mental health services among children adds an additional level of complexity. The large majority of poor, urban children judged to be in need of mental health care do not receive these services (Flisher et al., 1997; Harrison, McKay, & Bannon, 2004; Kataoka, Zhang, & Wells, 2002). While the need for mental health services can be assumed to be at least as great for homeless children as for their poor, housed counterparts, the impact of homelessness on receiving mental health services remains unclear. In the only previous study on this issue of which the authors are aware, Buckner & Bassuk (1997) found that, among small samples of both homeless and housed poor children who were diagnosed with mental disorders, there was no difference among the two groups in their use of mental health services.
In contrast, several dynamics could potentially lead to differences in children’s use of mental health services based on housing status. On one hand, the residential instability that accompanies homelessness can make accessing mental health service more difficult for homeless children (Kazdin, Holland, & Crowley, 1997). Conversely, the use of mental health services may increase with the onset of homelessness for several reasons. The stresses of homelessness may have adverse effects on children’s emotional and behavioral health and may compromise a parent’s capacity to address their children’s basic emotional and physical needs. All of these factors can create the need for more mental health services after children become homeless. There may be a “fishbowl effect” where otherwise overlooked mental health problems among homeless children come to the attention of attendant social and medical providers in shelters (Park, Metraux, Brodbar, & Culhane, 2004). Additionally, the attendant higher risk among children in homeless families for entering foster care or being involved with child protective services (Park, Metraux, Brodbar, & Culhane, 2004; Zlotnick, 2009), which often functions as a gateway into specialty mental health services for many children (Hurlburt et al., 2004; Leslie et al., 2005), can lead to more frequent use of mental health services.
This study examines 1) whether children who become homeless differ from low-income housed children in their use of inpatient and ambulatory mental health services, both before and after their first homeless episode, and 2) to what extent homelessness is associated with an increased likelihood of mental health service use. Given the range of possible trajectories, a better understanding of the extent to and the occasions on which children in homeless families use mental health services facilitates both understanding the role of homelessness in children’s use of mental health services and in making service systems more responsive for children who are at risk for homelessness or already homeless.
To investigate this, administrative records from a cohort of Medicaid enrolled children in a large metropolitan area are examined over a six-year period. Both sheltered and housed children are followed through records of their Medicaid claims, shelter use, and child welfare history. This longitudinal dataset allows for comparison of outcomes for sheltered and never-sheltered children, and the temporal sequencing of homelessness and mental health service use among the homeless children.
Methods
Data and Sample
Data for this study came from three sources. The first source was Medicaid records obtained from Community Behavioral Health, the managed care organization that covers all Medicaid-reimbursed behavioral health care in Philadelphia, Pennsylvania. Two Medicaid datasets were used for this study. One Medicaid dataset was an eligibility file containing records for 169,516 children in Philadelphia who were enrolled in Medicaid for 18 months or more from July 2000 through June 2002 (i.e., the index period). This file included all children who met these criteria, regardless of whether they received mental health services or not. The second Medicaid dataset was a claims file with records for all Medicaid-reimbursed mental health services that were consumed by persons in the eligibility dataset from July 1998 through June 2004.
The eligibility criteria ensured that the children in the study had access to mental health services during most of the study period, and accommodated lapses in Medicaid eligibility. Medicaid claims from July 1998 to June 2004 (i.e., the study period) were used so that claims could be observed in the 24 months before and after the sample selection index period. Medicaid eligibility files, separately maintained for inpatient and ambulatory claims, included information on enrollment status in Medicaid, individual identifiers (including unique Medicaid number), demographic characteristics, basis of eligibility, and the benefit start and end dates. Medicaid claims files provided information about dates of service, diagnosis codes, place of service, and costs reimbursed by Medicaid.
Identifiers for the children were matched to records from the City of Philadelphia’s Office of Supportive Housing (OSH), which funds or administers over 85% of all shelter beds for families in Philadelphia. OSH maintains records for all of the families and their stays in its shelter system. Children in families that entered the municipal shelter system for the first time during the two year period were identified as newly homeless, and children who entered the shelter system in the 24 months before the start of the index period were excluded from the study. A total of 3,011 children met the inclusion criteria for the homeless group and these children accounted for 71% of all children located in the shelter records over the index period. The remaining 162,810 children, who were enrolled in Medicaid and had no history of homeless shelter stay by the end of June 2004, comprised the comparison group.
Finally, child welfare records from the City of Philadelphia’s Department of Human Services (DHS) were matched with both the homeless and comparison groups to provide information on foster care placement. DHS is Philadelphia’s municipal child welfare agency, whose services include investigation of reports of abuse and neglect, in-home preventative services, and foster care. Foster care records from the DHS were matched, using common identifiers, to both the homeless and comparison groups to identify children with foster care placement history during the time period from July 1998 to January 2004.
Variables
The dependent variable, mental health service use, was identified through Medicaid claims in which the primary diagnosis at intake was an International Classification of Diseases-Ninth Revision (ICD-9) code between 290 through 319. Type of treatment was categorized as inpatient or ambulatory care. The number of claims and corresponding payment amounts accrued during the observation period, and any use of inpatient and ambulatory services were calculated. Psychiatric diagnoses were also examined to see if there were any differences in the type of diagnosis for children with and without homeless episodes. Psychiatric diagnoses were grouped into four categories according to primary ICD-9 diagnostic codes at intake: psychotic disorders (organic psychotic conditions (294), schizophrenic disorders (295), and affective psychoses (296)); externalizing disorders (i.e., conduct disorders (312), oppositional defiant disorders (313), and attention deficit hyperactivity disorders (314)); internalizing disorders (i.e., neurotic disorders (300), acute reaction to stress (308), and adjustment disorder (309), depressive disorders (311)); and other diagnoses (other ICD-9 codes between 290 and 319).
The independent variables included sociodemographic and foster care related variables. Foster care history was measured as having been placed in out-of-home care in a relative or non-relative foster home, treatment/specialized foster home, group home, or residential institution. An interaction term of homelessness and foster care history was included in multivariate analyses to see if the effects of homelessness were different by foster care placement history. Race and ethnicity were classified as Black (non-Hispanic), Hispanic, White (non-Hispanic), and other. Age (in 2002) was measured as a continuous variable. Children were also grouped into three age categories: less than 6, 6–11, and more than 12 years of age. Gender of children was included in the analyses. Medicaid eligibility was under the auspices of four possible categories: Temporary Assistance to Needy Families (TANF), General Assistance (GA), Supplemental Security Income (SSI), and a residual “other” category.
Analysis
Descriptive analyses were the basis for addressing the first research question, whether use of inpatient and ambulatory mental health services differed between children who become homeless and low-income housed children before and after their first homeless episode. Specifically, chi-square analyses were used to assess differences in demographic characteristics, and the use and cost of mental health services between children with and without homeless episodes. The proportions of children who received psychiatric inpatient and ambulatory treatment per year were calculated to examine differences cumulative rates of service use over the study period between the two groups. Then, logistic regression analyses were used to address the second research question examining the extent that homelessness is associated with a likelihood of receiving inpatient and ambulatory mental health services. Separate logistic regression models were run for receipt of inpatient and ambulatory mental health services. All analyses were performed with SAS software, version 9 for UNIX. The institutional review board of the University of Illinois approved this study before data analyses were conducted.
Results
Demographic, Eligibility and Foster Care Characteristics
The demographic characteristics of children who became homeless differed from other low-income housed children (Table 1). The homeless group was proportionately more of Black race (89% to 67%), and was significantly younger (mean 7.5 years to 8.6 years). Underlying this difference in means of 1.1 years was an age distribution where considerably more children in the homeless group were preschool aged (under 6; 38% to 29%) and, in turn, less were adolescent aged (12–16 years old; 21% to 31%). This disproportionate representation in both race/ethnicity and age among homeless children has been documented in other studies (Culhane & Metraux, 1999). Children in the homeless group were also much more frequently Medicaid eligible due to the family’s receipt of TANF benefits (84% to 69%). The non-homeless group had a higher percentage of persons eligible for Medicaid through “other” means – most among this group were Medicaid-eligible through the Healthy Beginning programs, which serve low-income pregnant women and their children. Finally, homeless children compared to non-homeless children had a much higher rate of foster care placements during the study period – 15% to 9%.
Table 1.
Characteristics of Medicaid-enrolled children, by new onset of sheltered homelessness (N=165,821)
| Homeless Group (N=3,011) |
Non-homeless Group (N=162,810) |
|||
|---|---|---|---|---|
| Characteristic | N | % | N | % |
| Gender | ||||
| Male | 1,524 | 50.7 | 83 | 51.2 |
| Female | 1,487 | 49.4 | 79 | 48.8 |
| Race/Ethnicity*** | 0 | |||
| Black | 2,689 | 89.4 | 109 | 67.4 |
| White | 111 | 3.7 | 19 | 11.9 |
| Hispanic | 163 | 5.4 | 24 | 14.8 |
| Other | 48 | 1.6 | 9 | 5.9 |
| Age in 2002 (mean ± SD)*** | 7.5 ± 4.1 | 8.6 ± 4.4 | ||
| Under 6 | 1,147 | 38.1 | 47,703 | 29.3 |
| 6–11 years | 1,244 | 41.3 | 64 | 29.3 |
| 12–16 years | 620 | 20.6 | 50 | 39.7 |
| Eligibility status***a | ||||
| TANF | 2,523 | 83.9 | 112 | 68.9 |
| GA | 48 | 1.6 | 3,256 | 2.0 |
| SSI | 84 | 2.8 | 6,838 | 4.2 |
| Other | 355 | 11.8 | 40,703 | 25.0 |
| Has History of Foster care *** | 449 | 14.9 | 14,327 | 8.8 |
| Inpatient psychiatric treatment** | 154 | 5.1 | 6,350 | 3.9 |
| Days of inpatient care (group meanb)** | 3.0 | 4.9 | ||
| Cost for inpatient care (group meanb) | $1,205 | $1,370 | ||
| Days of inpatient care (user meanc)*** | 85 | 130 | ||
| Cost for inpatient care (user meanc)* | $23,723 | $34,811 | ||
| Ambulatory psychiatric treatment*** | 26.8 | 21.8 | ||
| No. of ambulatory visit (group meanb) | 17.4 | 15.5 | ||
| Cost for ambulatory visit (group meanb)* | $1,551 | $1,286 | ||
| No. of ambulatory visit (user meanc) | 62.3 | 68.7 | ||
| Cost for ambulatory visit (user meanc) | $5,724 | $5,846 | ||
p<.001,
p<.01,
p<.05
TANF, Temporary Assistance to Needy Families; GA, General Assistance; SSI, Supplemental Security Income
group mean, a mean value for the group, was based on the total number of days of inpatient care, total number of ambulatory visit and total costs for care divided by the total number of subjects in each group of the sample.
user mean, a mean value for per user, was calculated for study subjects who received services during the study period.
Use of Mental Health Services
Overall, 5.1% of the homeless children received psychiatric inpatient treatment during the observation period compared to 3.9% among the non-homeless group (Table 1). No significant difference was observed in the proportion of the type of diagnosis between the two groups. Among service users, both the average days and costs were substantially higher among non-homeless children. Additional analysis showed that this gap was mainly attributed to more frequent service use among children with foster care history in the non-homeless group compared to those in the homeless group. Use of ambulatory mental health services was more common in both groups, with 26.8% of the homeless group and 21.8% of the non-homeless group using ambulatory mental health services during the study period. Looking only at service users, those in the non-homeless group had, on average, more ambulatory visits, at a slightly higher cost, than the homeless group.
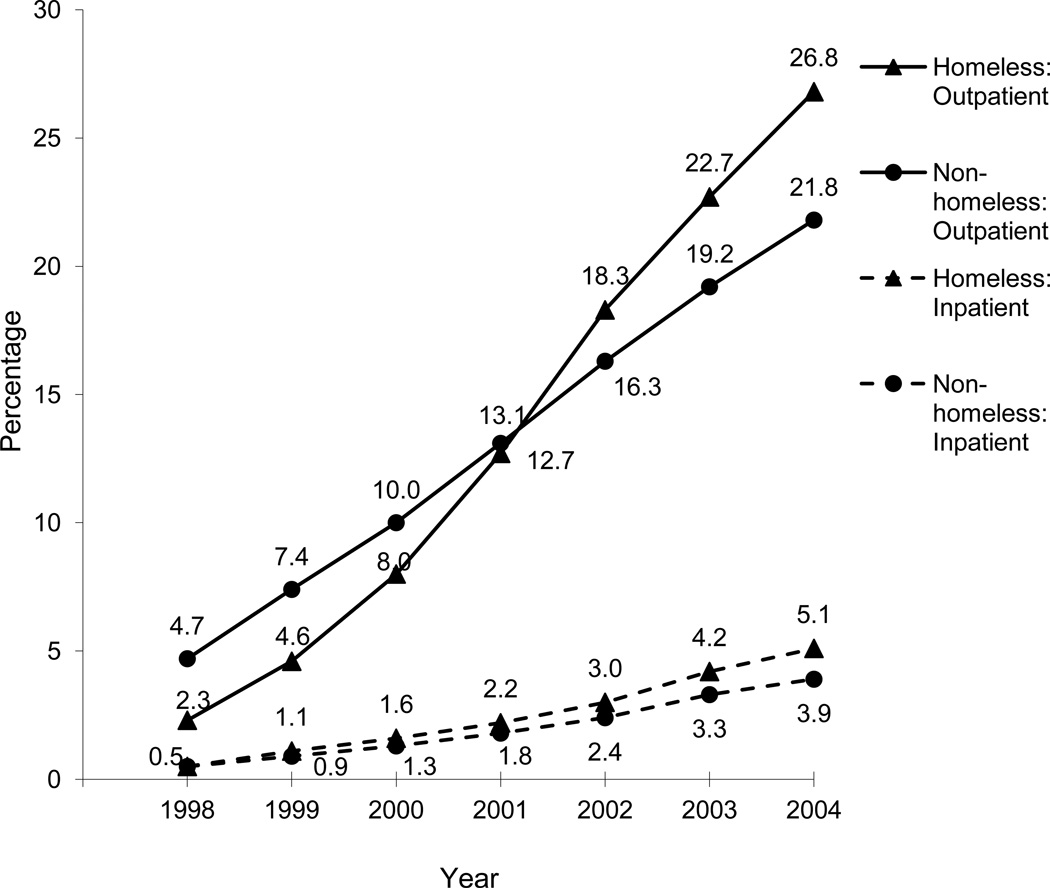
Figure 1 shows cumulative rates of children who had records of inpatient and ambulatory mental health services. What started as a non-significant difference in inpatient hospitalization rates at the beginning of the study period grew into significantly different cumulative rates six years later. The cumulative rate for the homeless group starts increasing markedly at the start of the index period (i.e., at the point when shelter stays start), overtaking and exceeding the cumulative rate for the non-homeless. In order to see if the observed discrepancies were due to the compositional differences between the homeless and comparison groups, we also compared rates of mental health services use between the homeless group and a subset of 3,011 matched controls who were selected from the non-homeless group using propensity score matching techniques, based on race/ethnicity, age, gender, and the number of days they were eligible for Medicaid. The differences in inpatient and ambulatory mental health services between the homeless and the matched non-homeless groups remained similar or became greater (not shown).
Figure 1.
Cumulative rates of inpatient and ambulatory mental health service use for a cohort of Medicaid-enrolled children by sheltered homelessness between 1998 and 2004
Likelihood of Mental Health Services Use
Table 2 shows logistic regression models with estimated odds ratios for receiving inpatient mental health hospitalization and ambulatory mental health services. For both types of services, there were substantial independent associations with homelessness (OR=1.88 for inpatient; OR=1.43 for ambulatory). These effects were much lower, however, than the comparable odds ratios for foster care (OR=5.62 for inpatient; OR=7.42 for ambulatory). Adding homelessness on to foster care (i.e., the interaction term) resulted in an insubstantial additional risk for inpatient mental health services. In contrast, having records of both foster care and homelessness substantially increased likelihood of receiving ambulatory mental health services as compared to experiencing either foster care or homelessness. The receipt of SSI, being male, non-Hispanic white, and Hispanic were also associated with higher odds ratios in both models.
Table 2.
Logistic regression analysis of mental health service use among Medicaid-enrolled children (N=165,821)
| Inpatient treatment | Ambulatory treatment | |||
|---|---|---|---|---|
| ORa | 95% CIb | OR | 95% CI | |
| Homelessness (no foster care)c | 1.88*** | 1.52–2.32 | 2 43*** | 1.29–1.57 |
| Foster care (no homelessness)c | 5.62*** | 5.31–5.95 | 7.42*** | 7.13–7.72 |
| Homelessness* Foster carec | 5.57*** | 4.17–7.44 | 9 39*** | 7.66–11.50 |
| Male | 1. 33*** | 1.26–1.40 | 1.85*** | 1.80–1.90 |
| Race/Ethnicity | ||||
| White | 1.40*** | 1.29–1.51 | 1.31*** | 1.26–1.36 |
| Hispanic | 1.12*** | 1.04–1.20 | 2 94*** | 1.88–2.00 |
| Other | 29*** | .24– .37 | .27*** | .24– .29 |
| Black (Ref) | 1.00 | 1.00 | ||
| Age (per year) | 1.18*** | 1.18–1.19 | 1.11*** | 1.11–1.11 |
| Eligibility statusd | ||||
| GA | 1.12 | .94–1.33 | 1.14*** | 1.04–1.24 |
| SSI | 2.38*** | 2.19–2.59 | 2.50*** | 2.37–2.64 |
| Other | .82*** | .76–.88 | .69*** | .67– .71 |
| TANF (Ref) | 1.00 | 1.00 | ||
OR, Odds ratio
CI, Confidence interval
Reference group: Non-homeless, Non-foster care history
TANF, Temporary Assistance to Needy Families; GA, General Assistance; SSI, Supplemental Security Income
p<.001
Discussion
Based on these findings, children were more likely to receive mental health services once they enter a homeless shelter. Children who experienced homelessness were similar to low-income housed children in mental health service use prior to their first homeless episode, after which a greater number used mental health services, particularly ambulatory services. Yet it is also clear that one cannot properly assess relationships between mental health care and homelessness without taking foster care (and child welfare system involvement more generally) into account. This finding can be related to the fact that a substantially higher proportion of homeless children had foster care placements than did low-income housed children, and foster care had a strong association on the odds of receiving mental health services (Park, Metraux, Brodbar, & Culhane, 2004; Hurlburt et al., 2004; Leslie et al., 2005; Cowal, Shinn, Weitzman, Stojanovic, & Labay, 2002). Nonetheless, multivariate analyses showed that, even after controlling for history of foster care placement and other covariates, homelessness still was associated with an increased likelihood of receiving mental health services.
One explanation for these findings is that homelessness, measured as entry into shelter, increased risk for poor mental health due to its magnifying effect on familial dysfunctions and difficulties with fitting into the shelter life, resulting in increased need for mental healthcare. Another explanation is that children in homeless families received increased attention from service providers in homeless shelters. This would have made them more likely to receive referrals to health and social service professionals and given them greater access to mental health services after they entered a shelter. Taking both of these explanations together, shelter can function as a gateway to mental health services for children who present the need for such. This is regardless of whether this need stems from untreated conditions that the children brought with them into the shelter, conditions that became acute only upon entering shelter, or care brought on by an increased level of surveillance.
Foster care placement appeared to be a primary conduit to mental health services for children in shelters. Foster care history played a substantial role in increasing the likelihood of both inpatient and ambulatory mental health service use, independent of homeless experiences. This finding is consistent with literature showing that children in foster care, because of the circumstances leading to their placement, have a high level of need for mental health services, and that foster care placement facilitates children’s access to such services (Hurlburt et al., 2004; Leslie et al., 2005). This elevated risk, along with sheltered children having much higher rates of foster care placement than the low-income housed children, combined to leave more children facing a greater likelihood of receiving mental health services. These findings indicate that foster care is intertwined with both homelessness and mental health services for children, and that it would be critical to coordinate these three systems of care to provide treatment and support services based on inter-agency collaboration and families’ active involvement. Providing supportive housing options through the child welfare system to facilitate family unity and reunification would be one such approach that holds promise in mitigating homelessness as well as providing better mental health and child welfare outcomes (Farrell, Britner, Guzzardo, & Goodrich, 2010; Culhane & Metraux, 2008; Harburger & White, 2004).
The finding that children eligible for SSI were more likely to use mental health services than those receiving TANF was somewhat expected, given their mentally or physically disabling conditions. A lower likelihood of mental health services use among Black children compared with white and Hispanic children may result from limited access to and underutilization of mental health services among Black children as reported by prior research (Miller & Lin, 1988; Zahner & Daskalakis, 1997) or possibly their greater likelihood of being placed in juvenile detention facilities (Leiber & Johnson, 2008) in lieu of psychiatric facilities. Differences in mental health service use by gender and age align with previous findings that girls are more likely to be undertreated than boys, older children may be more severely impaired when they pursue psychiatric treatment, and older children tend to more frequently use psychiatric services than younger children (Zahner & Daskalakis, 1997).
This study has several limitations. First, this study selected its sample from Medicaid-eligible children. Although this feature made the sample homogeneous regarding the type of health insurance, it should be noted that not all homeless or low-income children are enrolled in Medicaid. Thus, the interpretations of the findings should be limited to those enrolled in Medicaid. Second, the homeless shelter records used to identify the homeless group do not include all shelters in the city. Privately operated emergency and transitional shelters account for approximately 15% of total shelter beds in Philadelphia (Metraux et al., 2001). Moreover, while the vast majority of families with children enter the shelter system (Burt, Aron, Lee, & Valente, 2001), some families with children may be homeless outside of the shelter system (e.g., staying on street locations or vacant buildings, staying with relatives or friends). If children in non-shelter or private shelter arrangements were more likely than others to receive psychiatric treatments, then the study findings would be an underestimate of the relationship between homelessness and mental health service use. Third, this study relied on Medicaid claims to identify the receipt of mental health services. Given that children in the sample were Medicaid-eligible, most psychiatric treatments were likely to be paid for through Medicaid. Nevertheless, it is possible that some psychiatric treatment was paid for through other sources. If the low-income housed group was more likely than the homeless group to receive mental health services outside Medicaid, then the association between sheltered homelessness and mental health services use would be attenuated.
This study finds an association between shelter use and the increased likelihood of children’s use of mental health services. Furthermore, it outlines the interactions between homelessness, foster care, and mental health care. While this study is unable to provide specifics of how these interactions work, it does underscore the need for collaborative efforts across systems in addressing family homelessness and attending to collateral needs among children.
Highlights.
Children who became homeless were similar to low-income housed children in mental health service use prior to their first homeless episode.
Differences between homeless and non-homeless children in mental health service use emerged following new onset of homelessness and widened over time.
Sheltered homelessness and foster care placement history were associated with increased odds of receiving inpatient and ambulatory mental health services.
Foster care placement appeared to be a primary conduit to mental health services for children in shelters.
Acknowledgments
This study was supported by National Institute of Child Health and Human Development (R03HD055293-01A1).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jung Min Park, School of Social Work, University of Illinois at Urbana-Champaign
Stephen Metraux, Department of Health Policy & Public Health, University of the Sciences in Philadelphia
Dennis P. Culhane, School of Social Policy and Practice, University of Pennsylvania
David S. Mandell, Department of Psychiatry, University of Pennsylvania
References
- Bassuk EL, Buckner JC, Weinreb LF, Browne A, Bassuk S, Dawson R, Perloff J. Homelessness in female-headed families: Childhood and adult risk and protective factors. American Journal of Public Health. 1997;87:241–248. doi: 10.2105/ajph.87.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JC, Bassuk EL. Mental disorders and service utilization among youth from homeless and low-income housed families. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:890–900. doi: 10.1097/00004583-199707000-00010. [DOI] [PubMed] [Google Scholar]
- Buckner JC, Bassuk EL, Weinreb LF, Brooks MG. Homelessness and its relation to the mental health and behavior of low-income school-age children. Developmental Psychology. 1999;35:246–257. doi: 10.1037//0012-1649.35.1.246. [DOI] [PubMed] [Google Scholar]
- Buckner JC. Understanding the impact of homelessness upon children: Challenges and future research directions. American Behavioral Scientist. 2008;51:721–736. [Google Scholar]
- Burt MR, Aron L, Lee E, Valente J. Helping America’s homeless: emergency shelter or affordable housing? Washington DC: The Urban Institute Press; 2001. [Google Scholar]
- Cowal K, Shinn M, Weitzman BC, Stojanovic D, Labay L. Mother-child separations among homeless and housed families receiving public assistance in New York City. American Journal of Community Psychology. 2002;30:711–730. doi: 10.1023/A:1016325332527. [DOI] [PubMed] [Google Scholar]
- Culhane DP, Metraux S. Assessing relative risk for homeless shelter usage in New York City and Philadelphia. Population Research and Policy Review. 1999;18:219–236. [Google Scholar]
- Culhane DP, Metraux S. Rearranging the deck chairs or the lifeboats? Homelessness assistance and its alternatives. Journal of the American Planning Association. 2008;74:111–121. [Google Scholar]
- Farrell AF, Britner PA, Guzzardo M, Goodrich S. Supportive housing for families in child welfare: Client characteristics and their outcomes at discharge. Children and Youth Services Review. 2010;32(2):145–154. [Google Scholar]
- Flisher AJ, Kramer RA, Grosser RC, Alegria M, Bird HR, Bourdon KH, Hoven CW. Correlates of unmet need for mental health services by children and adolescents. Psychological Medicine. 1997;27:1145–1154. doi: 10.1017/s0033291797005412. [DOI] [PubMed] [Google Scholar]
- Grant R, Bowen S, McLean DE, Berman D, Redlener K, Redlener I. Asthma among homeless children in New York City: An update. American Journal of Public Health. 2007;97:448–450. doi: 10.2105/AJPH.2005.070482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harburger DS, White RA. Reunifying families, cutting costs: housing-child welfare partnerships for permanent supportive housing. Child Welfare. 2004;83:493–508. [PubMed] [Google Scholar]
- Harrison ME, McKay MM, Bannon WM. Inner-city child mental health service use: The real question is why youth and families do not use services. Community Mental Health Journal. 2004;40:119–131. doi: 10.1023/b:comh.0000022732.80714.8b. [DOI] [PubMed] [Google Scholar]
- Hurlburt MS, Leslie LK, Landsverk J, Barth RP, Burns BJ, Gibbons RD, Zhang J. Contextual predictors of mental health service use among children open to child welfare. Archives of General Psychiatry. 2004;61:1217–1224. doi: 10.1001/archpsyc.61.12.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. American Journal of Psychiatry. 2002;159:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M. Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology. 1997;65:453–463. doi: 10.1037//0022-006x.65.3.453. [DOI] [PubMed] [Google Scholar]
- Leiber MJ, Johnson JD. Being young and black: What are their effects on juvenile justice decision making? Crime Delinquency. 2008;54:560–581. [Google Scholar]
- Leslie LK, Hurlburt MS, James S, Landsverk J, Slymen DJ, Zhang J. Relationship between entry into child welfare and mental health service use. Psychiatric Services. 2005;56:981–987. doi: 10.1176/appi.ps.56.8.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Miliotis D, Graham-Bermann SA, Ramirez ML, Neemann J. Children in homeless families: Risks to mental health and development. Journal of Consulting and Clinical Psychology. 1993;61:335–343. doi: 10.1037//0022-006x.61.2.335. [DOI] [PubMed] [Google Scholar]
- Metraux S, Culhane D, Raphael S, White M, Pearson C, Hirsch E, Cleghorn JS. Assessing homeless population size through the use of emergency and transitional shelter services in 1998: results from the analysis of administrative data from nine US jurisdictions. Public Health Reports. 2001;116:344–352. doi: 10.1016/S0033-3549(04)50056-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller DS, Lin EHB. Children in sheltered homeless families: reported health status and use of health services. Pediatrics. 1988;81:668–673. [PubMed] [Google Scholar]
- Park JM, Metraux S, Brodbar G, Culhane DP. Child welfare involvement among children in homeless families. Child Welfare. 2004;83:423–436. [PubMed] [Google Scholar]
- Rafferty Y, Shinn M. The impact of homelessness on children. American Psychologist. 1991;46:1170–1179. doi: 10.1037//0003-066x.46.11.1170. [DOI] [PubMed] [Google Scholar]
- Rog D, Buckner JC. Homeless families and children. In: Dennis D, Locke G, Khadduri J, editors. Toward understanding homelessness: The 2007 National Symposium on Homelessness Research. Washington, DC: U.S. Department of Health and Human Services and US Department of Housing and Urban Development; 2007. pp. 5.1–5.33. [Google Scholar]
- San Agustin M, Cohen P, Rubin D, Cleary S, Erickson C, Allen JK. The Montefiore Community Children's Project: A controlled study of cognitive and emotional problems of homeless mothers and children. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 1999;76:39–50. doi: 10.1007/BF02344460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M, North CS, LaVesser PD, Osborne VA, Spitznagel EL. A comparison study of psychiatric and behavior disorders and cognitive ability among homeless and housed children. Community Mental Health Journal. 2008;44:1–10. doi: 10.1007/s10597-007-9100-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahner GEP, Daskalakis C. Factors associated with mental health, general health, and school-based service use for child psychopathology. American Journal of Public Health. 1997;87:1440–1448. doi: 10.2105/ajph.87.9.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zima BT, Wells KB, Freeman HE. Emotional and behavioral problems and severe academic delays among sheltered homeless children in Los Angeles County. American Journal of Public Health. 1994;84:260–264. doi: 10.2105/ajph.84.2.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotnick C. What research tells us about the intersecting streams of homelessness and foster care. American Journal of Orthopsychiatry. 2009;79:319–325. doi: 10.1037/a0017218. [DOI] [PubMed] [Google Scholar]