Abstract
Background:
Body temperature measurement is a crucial clinical assessment in the care of an acutely ill child, especially the under fives. Most temperature measurements in our hospital are done from the axilla.
Objective:
To study the relationship between temperatures taken in the axilla with those taken in the rectum in febrile and afebrile children less than 5 years.
Materials and Methods:
Rectal and axillary temperatures were taken concurrently in 400 febrile and 400 afebrile children aged less than 5 years using mercury-in-glass thermometers.
Result:
The rectal temperature measurements ranged from 38.0 to 41.4°C and 36.4 to 37.9°C in the febrile and afebrile groups of children respectively while the axillary temperatures ranged from 36.7 to 41.0°C and 35.9 to 37.5°C in the febrile and afebrile groups of children, respectively. There were significant differences between the temperatures measured at the two sites in all the age groups studied. There was good positive correlation between the rectal and axillary temperatures. A linear relationship between axillary and rectal temperatures was derived using the simple regression analysis. The equation is: rectal temperature = 0.94×axillary temperature+2.92.
Conclusion:
Although there's good correlation between axillary and rectal temperatures, significant difference exits between them that cannot be explained by the addition of any single value or any particular equation.
Keywords: Axillary, children, rectal, temperature, thermometry
INTRODUCTION
Body temperature measurement is one of the most common procedures carried out in the Pediatric clinic. It is a crucial clinical assessment in the care of an acutely ill child.
The best sites for measuring body temperature are those closest to the hypothalamus, the temperature regulating center that reflects the “core” temperature.1 Since the hypothalamus is inaccessible, the core temperature is generally defined as the temperature measured within the pulmonary artery.2 Other alternative sites which have been used, including distal esophagus, bladder, and nasopharynx, are accurate within 0.1-0.2°C of core temperature.3
However, since these sites are clinically inaccessible, clinicians have utilized the rectum as a practical site that most closely reflects core temperature despite some of its drawbacks like rectal perforation in neonates, spread of infections, and slow response to temperature changes3. Unfortunately, rectal thermometry has been resented by many children and their parents4, leaving axillary thermometry as the only option in many cases, especially the under-5 children.
The axillary temperature is easily accessible, safe, hygienic, and simple. Many clinicians have continued to use and recommend the site for fever screening5,6 One pertinent question is: Can the axillary temperature be used to predict rectal temperature? Traditional information handed on from different generations of health practitioners is that axillary temperature is 1°C less than rectal temperature. Several researchers have tried to do an intersite comparison of body temperatures with different outcomes in relationships. Several equations have been deduced to explain the relationship between axillary and rectal temperatures.
This study was therefore aimed at establishing the relationship between the two sites using children less than 5 years and also validating or otherwise some of these equations by comparing the temperatures taken simultaneously in these two sites.
MATERIALS AND METHODS
Eight hundred children aged less than 5 years (birth – 59 months) were recruited from the children's outpatient (CHOP), children emergency room (CHER) the follow-up clinics and the well baby/immunization clinic of the University of Nigeria Teaching Hospital, Enugu. They were grouped into two using their rectal temperatures: 400 febrile and 400 afebrile children.
Fever in this study was defined as rectal temperatures of ≥37.6°C in neonates and ≥38.0°C in the older children. While for axillary temperature fever was defined as ≥37.5°C for neonates and ≥37.6°C for children beyond the neonatal age group.5
Approval from the research and ethics committee of the hospital was obtained. Written consent was also obtained from the parents or guardians.
The rectal and axillary thermometers were placed simultaneously with the child lying on his/her side on the couch or prone on the mother's laps. The rectal mercury-in-glass thermometer was lubricated with a water-soluble lubricant and inserted to a depth of 2-3 cm in neonates and 5-6 cm in older children and left for 3 min and 5 min respectively in neonates and older children before removal for reading. The axillary mercury-in-glass thermometer was inserted with the tip at the apex of the axilla and the arm held firmly at the side by the mother/caregiver for 5 min in neonates and 7 min in older children. Care was taken in each case to prevent breakage of the thermometers. All thermometers were well reset before each measurement.
All the children with fever were investigated and treated as appropriate for each child.
The thermometers were standardized by placing in warm water bath and ensured that all readings were the same before use each day. Each rectal mercury-in-glass thermometer was used only once each day and properly cleaned thereafter by washing with detergent and soaking in bleach for several hours before rinsing properly and drying. The axillary mercury-in-glass thermometers were cleaned with cotton wool swab soaked in methylated spirit.
The data was analyzed with the computer, using the SPSS-15 software. Rectal temperature was used as a reference standard to compare axillary temperature. The mean differences between rectal and axillary temperatures were compared using the Student t-test. A P-value of less than 0.05 was considered statistically significant. The relationship between the two methods of temperature measurement was determined using the Pearson's correlation coefficient at 99% confidence limit. A simple regression was done.
RESULTS
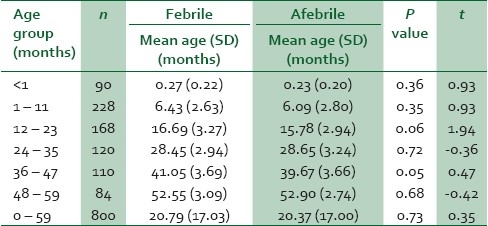
There were 429 males and 371 females, giving a male:female ratio of 1.2:1. The age distributions were compatible in both groups (P=0.35). The age distribution of the children studied is shown in Table 1: The total number of febrile and afebrile children in each age group was equal.
Table 1.
Age distribution of the total population studied
The rectal temperature measurements ranged from 38.0 to 41.4°C and from 36.4 to 37.9°C in the febrile and afebrile groups of children respectively while the axillary temperatures ranged from 36.7 to 41.0°C and from 35.9 to 37.5°C in the febrile and afebrile groups of children, respectively.
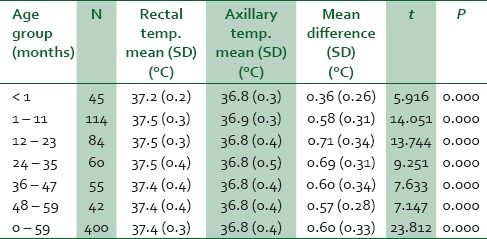
Tables 2 and 3 compare the mean rectal and axillary temperatures. The rectal temperatures were significantly higher than the axillary temperatures in all the age groups studied.
Table 2.
Comparison of the mean rectal and axillary temperatures in the febrile children
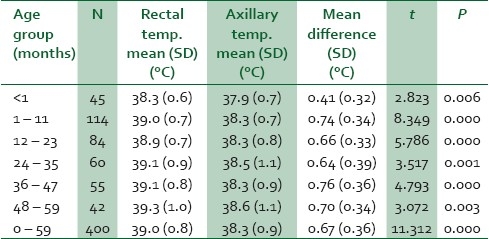
Table 3.
Comparison of the mean rectal and axillary temperatures in the afebrile children
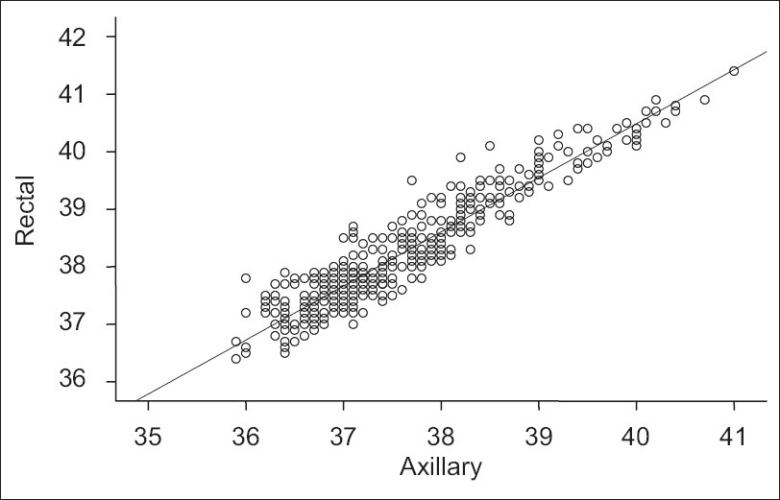
There was good positive correlation between the rectal and axillary temperatures in both the febrile and afebrile children. Correlation was stronger among febrile than afebrile children (r=0.91 vs. r=0.59, P<0.01). The combined correlation was even the strongest with r=0.94. Figures 1–3 show the relationship between the two temperatures in febrile, afebrile and all the children, respectively.
Figure 1.
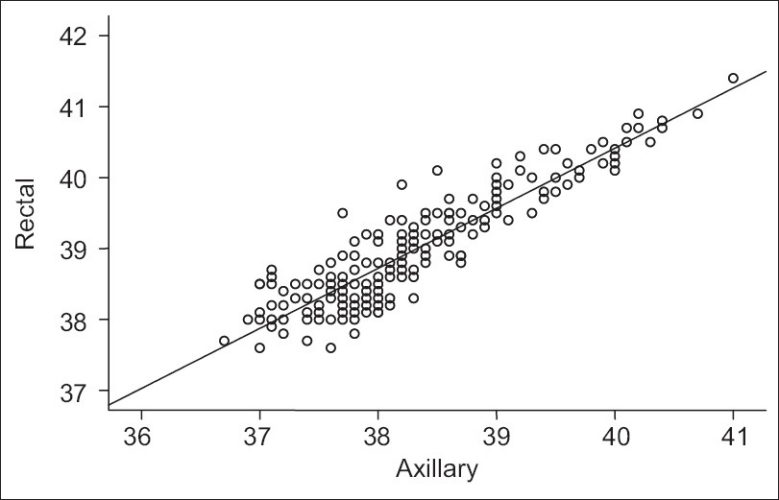
Scatter diagram showing the relationship between rectal and axillary temperatures (°C) in the 400 febrile children (r=0.91)
Figure 3.
Scatter diagram showing the relationship between rectal and axillary temperatures (°C) in the 800 children (r=0.94)
Figure 2.
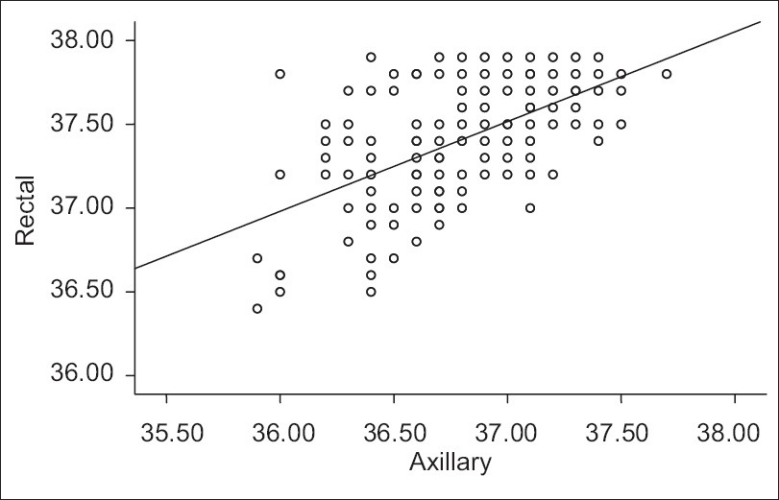
Scatter diagram showing the relationship between rectal and axillary temperatures (°C) in the 400 afebrile children (r=0.59)
A linear relationship between axillary and rectal temperatures was derived using the simple regression analysis. The equation is:
Rectal temperature = 0.94×axillary temperature+2.92
Table 4 shows the correlation coefficient of the axillary temperatures when analyzed with rectal temperature as the dependent variable.
Table 4.
Linear regression coefficient for axillary temperature
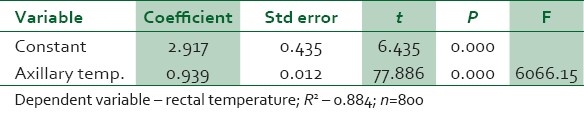
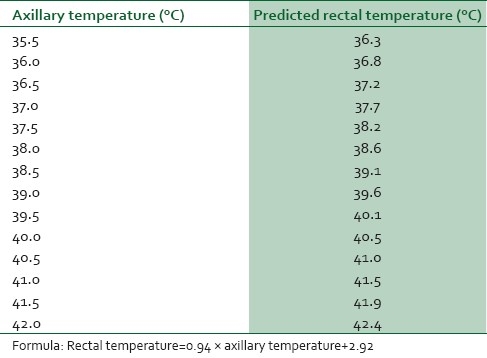
Using the equation above, a table for the prediction of rectal temperature from axillary temperature was designed [Table 5].
Table 5.
Rectal temperatures predicted from axillary temperatures using the formula
DISCUSSION
The mean axillary readings differed significantly from the mean rectal temperature readings across all age groups. The mean “recto–axillary” temperature difference was least in neonates. This may be explained by the smaller “core – shell” difference in neonates when compared to older children. These observations were consistent with the observations in a systematic review by Craig et al.7 In their own case, the pooled mean temperature difference for neonates was 0.17°C and for older children, it was 0.92°C. Like the present study, several studies1,8,9 are consistent with the lower temperature readings obtained using the axillary thermometers in children beyond the neonatal age when compared with rectal temperature readings. This may justify the lower cut-off for fever when using this site for temperature measurement. In the neonates, however, the findings are not uniform. While this present study and some other studies5,10 have found significant mean differences between the rectal and axillary temperatures in neonates, another11 found no significant difference. This raises another question as to whether the axillary route is accurate enough to be used as a surrogate to rectal thermometry in neonates in whom rectal thermometry is avoided because of accidents like perforations.12
Although there was good correlation between the temperatures measured at the two sites, the stronger correlation in the febrile group may imply a better accuracy at higher temperatures than at lower temperatures. Similarly, the rectal temperatures predicted from the measured axillary temperatures showed a narrowing of the axillary – rectal temperature difference with increasing axillary temperature. This further supports that axillary temperature may be more representative of core body temperature at higher temperatures.
It can also be shown that no particular value can be added to axillary temperature value to estimate the rectal temperature. Different studies have come up with different equations to predict rectal temperature from axillary temperature using regression analysis. Applications of these formulae give variable values. For instance, using the equation derived from this study to predict the rectal equivalent of an axillary temperature of 37.5°C gave a value of 38.2°C. On the other hand, using the equation by Chaturvedi et al.13 (Rectal temperature °C=0.98×Axillary temperature °C+0.8 °C) and Asadi-Pooya et al.14 (Rectal temperature °C=0.82×Axillary temperature °C+7.38°C) to predict rectal temperature from an axillary temperature of 37.5°C, values of 37.6°C and 38.1°C respectively will be obtained. Though the value in the later case appears to be close to that from this study, one can appreciate the variation in the two equations and so there's no particular equation to explain this relationship between axillary and rectal temperature.
In conclusion, although there's good correlation between axillary and rectal temperatures, a significant difference exits between them that cannot be explained by the addition of any single value or any particular equation. A harmonization of the different equations if possible, may help in predicting rectal temperature from a measured axillary temperature.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Schmitz T, Blair N, Falk M, Levine C. A comparison of five methods of temperature measurement in febrile intensive care patients. Am J Crit Care. 1995;4:286–92. [PubMed] [Google Scholar]
- 2.Milewski A, Ferguson KL, Terndrup TE. Comparison of pulmonary artery, rectal and tympanic membrane temperatures in adult intensive care unit patients. Clin Paediatr. 1991;30:13–6. doi: 10.1177/0009922891030004S05. [DOI] [PubMed] [Google Scholar]
- 3.El-Radhi AS, Barry W. Thermometry in paediatric practice. Arch Dis Child. 2006;91:351–6. doi: 10.1136/adc.2005.088831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terndrup TE, Crofton DJ, Mortelliti AJ, Kelley R, Rajk J. Estimation of contact tympanic membrane temperature with a noncontact infrared thermometer. Ann Emerg Med. 1997;30:171–5. doi: 10.1016/s0196-0644(97)70138-0. [DOI] [PubMed] [Google Scholar]
- 5.Osinusi K, Njinyam MN. Comparison of body temperatures taken at different sites and the reliability of axillary temperature in screening for fever. Afr J Med Sci. 1997;26:163–6. [PubMed] [Google Scholar]
- 6.Blainey CG. Site selection in taking body temperature. Am J Nurs. 1974;74:1859–61. [PubMed] [Google Scholar]
- 7.Craig JV, Lancaster GA, Williamson PR, Smyth RL. Temperature measured at the axilla compared with rectum in children and young people: Systemic review. BMJ. 2000;320:1174–8. doi: 10.1136/bmj.320.7243.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson JL, Seal RF, Spady DW, Joffres MR. Comparison of oesophageal, rectal, axillary, bladder, tympanic and pulmonary artery temperatures in children. J Pediatr. 1998;133:553–6. doi: 10.1016/s0022-3476(98)70067-8. [DOI] [PubMed] [Google Scholar]
- 9.Musumba CO, Griffiths KL, Ross A, Newton CR. Comparison of axillary, rectal and tympanic temperature measurements in children admitted with malaria. J Trop Paediatr. 2005;51:242–4. doi: 10.1093/tropej/fmh106. [DOI] [PubMed] [Google Scholar]
- 10.Hissink Muller PC, van Berkel LH, de Beaufort AJ. Axillary and rectal temperature measurements poorly agree in newborn infants. Neonatology. 2008;94:31–4. doi: 10.1159/000112840. [DOI] [PubMed] [Google Scholar]
- 11.Akinbami FO, Sowunmi A. Body temperature in the Nigeria neonate - comparison of axillary and rectal temperatures. Afr J Med Sci. 1991;20:49–52. [PubMed] [Google Scholar]
- 12.Young DG. Thermometers and rectal perforation in neonates. Arch Dis Child. 1979;93:255–8. doi: 10.1136/adc.54.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaturvedi D, Vilhekar KY, Charturvedi P, Bharambe MS. Comparison of axillary temperature with rectal or oral temperature and determination of optimum placing time in children. Indian Pediatr. 2004;41:600–3. [PubMed] [Google Scholar]
- 14.Asadi-Pooya A, Kashef S. Accuracy of axillary temperature compared with rectal temperature in sick children. Kuwait Med J. 2006;38:25–7. [Google Scholar]


