Abstract
Background:
Hydatidiform mole is a relatively common gynecological problem which could present like spontaneous abortion, one of the commonest gynecological emergencies. It has the propensity to become malignant but can easily be identified and treated. The aim of this study was to determine the demographics, clinical features, treatment options and outcome of patients with hydatidiform mole in our environment.
Materials and Methods:
This was a retrospective review of all the cases of hydatidiform mole seen at the Jos University Teaching Hospital (JUTH), Jos, Nigeria over a 5-year period.
Results:
There were 34 cases of hydatidiform mole giving an incidence of 1 in 357 deliveries. However only 25 case notes were available for analysis and the mean age of patients was 28±3 years. Vaginal bleeding (92%), honeycomb appearance on ultrasound scan (84%), and passage of vesicles (60%) were the most common clinical findings while suction curettage was the mode of treatment for all the patients in this study. Twenty-eight percent of cases were confirmed by histology. No patient came for follow-up after the third month of diagnosis. Twenty percent of the patients booked for antenatal care within 9 months of diagnosis while 12% of patients presented as gynecological emergencies with features of malignant disease within six months of diagnosis.
Conclusion:
Hydatidiform mole is common in Jos, North Central Nigeria, and presents most commonly with vaginal bleeding with over 10% becoming malignant. Hence all patients who present with vaginal bleeding should be screened for HM. None of the patients completed the recommended duration of follow-up and only about ¼ had histology reports. Concerted efforts need to be made to address the challenges of patients adhering to recommended follow-up protocols and having to pay first before investigations are done.
Keywords: Follow-up, hydatidiform mole, Jos, malignant, Nigeria
INTRODUCTION
The history of the management of gestational trophoblastic disease (GTD) can be considered as one of the success stories of modern medicine as the majority, if not all, are potentially curable with the retention of reproductive function, once the correct diagnosis is made and treatment is commenced early enough.1–4 GTD constitutes a spectrum of tumors and tumor-like conditions characterized by abnormal proliferation of pregnancy associated trophoblastic tissues of varying propensities for invasion and spread.1,5–7 They include hydatidiform mole (HM), invasive mole, placental-site trophoblastic tumor, and choriocarcinoma.5,6 HM is the commonest GTD.5,6
The incidence of HM varies greatly throughout the world ranging from 0.5 to 8.3 per 1000 live births and occurs more frequently in Asia compared with Western countries.1,5,6 Studies from various parts of Nigeria have reported incidence ranging from 1.7 to 6 per 1000 births.1,8–12 HM presents with amenorrhoea, vaginal bleeding and spontaneous passage of grape-like vesicles, high serum and urinary β human chorionic gonadotrophin (βHCG) levels. There may also be hyperemesis gravidarum, doughy uterus, inappropriate uterine size, bilateral theca lutein cyst and rarely, features of thyrotoxicosis and pre-eclampsia in the first half of pregnancy.13–15
The disease could also present as spontaneous abortion which is one of the commonest gynaecological emergencies.7,13,14 There have been few reports on HM in our environment and none from Jos in over 10 years. This study was carried out to determine the incidence of hydatidiform mole, the clinical features and management outcome at the Jos University Teaching Hospital, Jos, Nigeria.
MATERIALS AND METHODS
This was a retrospective descriptive study carried out at the Jos University Teaching Hospital, Jos, North Central Nigeria. The demographic and clinical data as well as management outcome of all the consecutive patients with hydatidiform mole managed between January, 2001 and December, 2005 were retrieved and entered into prepared proformas.
Analysis of data was done using simple percentages. The number of deliveries during the study period was obtained from the labour ward register.
RESULTS
Study charactertistics
During the study period there were 12,129 deliveries with thirty-four (0.28%) cases of hydatidiform mole managed during the period. This gave an incidence of 1 in 357 or 2.8 per 1000 deliveries. Adequate information for analysis was available in 25 case notes giving a retrieval rate of 74%. Data analysis and subsequent results and discussions were based on this sample. Table 1 shows the age distribution of the patients. Their ages ranged between 16 and 42 years with a mean age of 28±3 years.
Table 1.
Clinical characteristics of study subjects
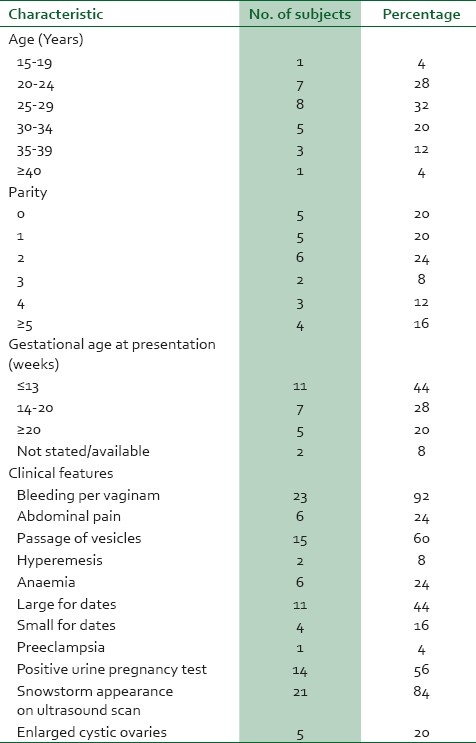
The distribution of patients by parity is shown in Table 1. Those of low parity (0-2) constituted 64% while patients of high parity constituted 36%. The peak parity was two which accounted for 24% of the patients.
Clinical presentation
Twelve (48%) patients had a history of previous spontaneous abortions. The clinical presentation of the study subjects was as shown in Table 1. Bleeding per vaginam occurred in 92%, honeycomb appearance on ultrasound scan in 84% and passage of vesicles in 60%; they constituted the most common clinical findings in this study. Six (24%) patients had anaemia and of these 4 (16%) received blood transfusion.
The blood grouping of only 5 patients (20%) was done and they were all Group A rhesus D positive. Two of the patients (8%) had a previous history of molar pregnancy. Twelve (48%) patients had a history of previous spontaneous abortions and 44% of the patients presented in the first trimester [Table 1].
Treatment and outcome
Two (8%) patients had spontaneous abortion for which they had manual vacuum aspiration of retained products, while the other 23 (92%) had suction curettage.
Seventeen (68%) patients came for at least one follow up visit within the first three months of treatment. However, none of the patients came for follow up after three months [Figure 1] and seven (28%) patients had histology report.
Figure 1.
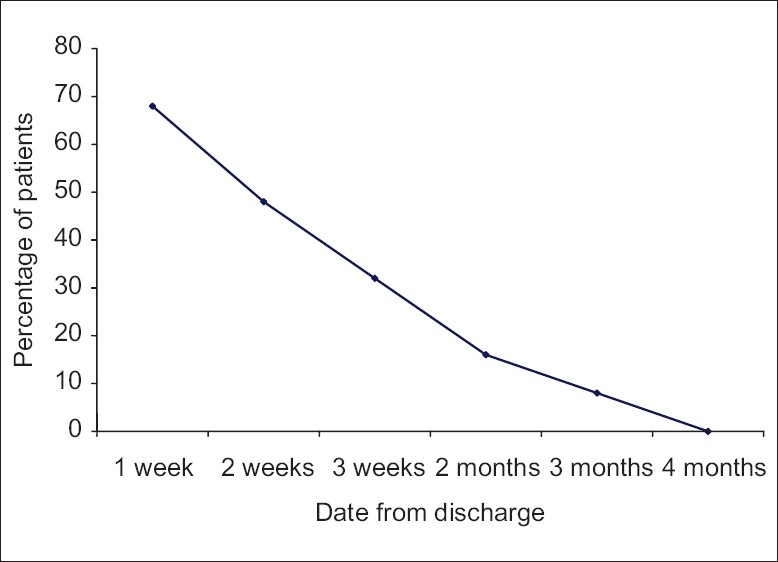
Follow-up of patients
Three (12%) of the patients lost to follow-up presented in the gynaecological emergency unit with persistent gestational trophoblastic disease within six months while another five (20%) patients lost to follow-up were found to have booked for antenatal care within nine months of diagnosis.
DISCUSSION
The incidence of hydatiform mole of 1:357 (2.8/1000 deliveries) in this study further confirms that the condition is common in our environment. It is lower than the incidence of 1:172 and 1:184 deliveries reported from Ibadan and Lagos –both in Nigeria, but comparable to the incidence reported from Onitsha and Ilorin.8–11 It is however higher than the incidence of 1:588 deliveries reported from Ile-Ife.12 The reason for this geographical variation is unknown but the fact that these are hospital-based studies in tertiary referral centres in an environment with varying degrees of hospital utilization may be contributory.
Maternal age has been found to influence the risk of hydatidiform mole; the incidence being increased in women under the age of 20 years and rising sharply after the age of 40 years.5,6,11 The findings in this study do not support this; it is however in conformity with experience of some other authors.12,14 Those aged less than 20 years and 40 years and above accounted for just 8% of the patients.
A large proportion of the patients (64%) were of low parity (0-2) and this is at variance with reports from some authors where most patients were of high parity.11,14 However, other authors have reported that hydatidiform mole has no significant association with parity.1,6 A previous history of molar pregnancy has consistently been shown to influence the risk of HM.2,7,15 However, in this study only 8% of patients in this study had a previous history of HM. Several studies have indicated that a history of previous abnormal gestations increased the risk for HM. In this study, 48% of the patients had a history of previous spontaneous abortions.
As in many other reports, vaginal bleeding is the commonest clinical presentation of hydatidiform mole in this study.8,13,14,16 It is therefore necessary for all patients with such complaints in early pregnancy to have an ultrasound scan which is reliable in the diagnosis of the condition.7,13,14 Ultrasound scan was used to diagnose 84% of the cases in this study. This is similar to other reports where more than 70% of cases were detected via ultrasound scan. This has also aided earlier diagnosis in the first trimester.7,17 Other common clinical features include passage of vesicles (60%) and excessive uterine enlargement (44%) which is similar to findings by some authors.13,15,18
The current trend in developed countries is that most cases of molar pregnancy are diagnosed in the first trimester due to availability of accurate and sensitive tests for the detection of hCG and early ultrasonographic examination, often before classical signs and symptoms develop.1,7,19 Only 44% of the patients in our study were diagnosed in the first trimester. However, 72% of patients were diagnosed before 20 weeks duration as has been reported in previous studies though most of them had developed symptoms prior to diagnosis.6,13
The measurement of serum βhCG by radioimmunoassay is crucial in the diagnosis and follow-up of patients with hydatidiform mole and choriocarcinoma.1,6,7 This measures the βhCG which is specific and more sensitive for diagnosis. In this study, urinary βhCG as determined by pregnancy test in neat and dilution was relied upon for lack of facilities for radioimmunoassay and 44% of the patients had a negative pregnancy test. The low sensitivity of the test could account for this. Also, as has been reported with the more sensitive serum and urine βHCG immunoassays, false negatives could occur when there are extremely high levels of βHCG which overwhelms the assay system.20,21
Suction curettage was the method of treatment in this study. This method is currently advocated because it allows for rapid evacuation of the uterus irrespective of the uterine size with minimal blood loss.1,3,5 It also provides specimen for histological assessment of the products of conception, reduces the danger of uterine perforation, minimizes injury to the blood vessels and therefore reduces the chance of trophoblastic tissue embolization.1,5,7 It is associated with a low risk of chemotherapy usage for gestational malignancy.1,6,7 Because the RhD antigen is present in trophoblasts, patients with an Rh-negative blood type should receive Rh immune globulin at the time of evacuation of the uterus.6,7 Hence, is important to check the blood group of these patients but in the study only 20% had blood grouping done and they were all rhesus D positive.
Despite the fact that patients with molar pregnancy are strongly advised to avoid pregnancy during the period of follow up because the occurrence of new gestation would interfere with follow-up testing of hCG levels, at least 20% of the patients became pregnant within nine months of diagnosis.6,7,13 These patients are likely not to have used contraceptives as advised probably not understanding the consequences. Mbamara et al. also reported low contraceptive compliance amongst women being followed up for HM in Nnewi.1
About 20% of patients with complete hydatidiform mole would develop malignant sequelae.6,13 In this review, 12% of the patients developed this sequelae but this could have been more since a large proportion were lost to follow-up. The follow-up clinic rate in this study was low as 32% had no follow-up visit and no patient continued follow up after three months. The findings of other authors in Nnewi, Ibadan and Ile-Ife corroborate the fact that follow-up of patients in our environment is poor.1,22,23
Histopathological examination of uterine specimen is important to confirm diagnosis or make primary diagnosis in unsuspected case of molar pregnancy but only 28% of patients in this study had histopathology reports.1,6,7,13 At the Jos University Teaching Hospital, patients have to pay before investigations are done hence financial constraints would affect patients’ ability to have such important investigations as histopathological examinations, blood group etc done. This is not ideal and efforts, such as introduction of health insurance, should be made to change the practice so that all investigations can be done.
The limitations of this study include the fact that it is a retrospective study with its attendant setbacks. There was also the poor follow up of patients, small sample size and histologic confirmation was possible in only 28% of the cases reported.
Hydatidiform mole is common in Jos, North Central Nigeria and presents most commonly with vaginal bleeding with over 10% becoming malignant. Hence all patients who present with vaginal bleeding should be screened for HM. Diagnosis is easily made using clinical features, ultrasound scan and urinary HCG levels and treatment is by suction curettage. None of the patients completed the recommended duration of follow up and only about ¼ had histology reports. Concerted efforts need to be made to address the challenges of patients adhering to recommended follow-up protocols and having to pay first before investigations are done.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mbamara SU, Obiechina NJ, Eleje GU, Akabuike CJ, Umeononihu OS. Gestational trophoblastic disease in a Tertiary Hospital in Nnewi, Southeast Nigeria. Niger Med J. 2009;50:87–9. [Google Scholar]
- 2.Garrett LA, Garner EI, Feltmate CM, Goldstein DP, Berkowitz RS. Subsequent pregnancy outcomes in patients with molar pregnancy and persistent gestational trophoblastic neoplasia. J Reprod Med. 2008;53:481–6. [PubMed] [Google Scholar]
- 3.Ben-Arie A, Deutsch H, Volach V, Peer G, Husar M, Lavie O, et al. Reduction of post molar gestational trophoblastic neoplasm by early diagnosis and treatment. J Reprod Med. 2009;54:151–4. [PubMed] [Google Scholar]
- 4.Chakrabarti BK, Mondal NR, Chatterjee T. Gestational trophoblastic tumour at a tertiary level cancer center: A retrospective study. J Reprod Med. 2006;51:875–8. [PubMed] [Google Scholar]
- 5.Nevin J. Gestational trophoblastic disease. In: Bloch B, Dehaeck K, Soeters R, editors. Manual of Practical Gynecological Oncology. London: Chapman and Hall Medical; 1995. pp. 130–46. [Google Scholar]
- 6.Moore LE, Hernandez E. Hydatidiform mole. eMedicine Journal. [Last accessed on 2010 Sep 14]. Available from: http://emedicine.medscape.com/article/254657 .
- 7.Berkowitz RS, Goldstein DP. Clinical practice. Molar pregnancy. N Engl J Med. 2009;360:1639–45. doi: 10.1056/NEJMcp0900696. [DOI] [PubMed] [Google Scholar]
- 8.Aboyeji AP, Ijaiya MA. Hydatidiform mole in Ilorin, Nigeria: A ten-year review. Niger J Med. 2000;9:56–9. [PubMed] [Google Scholar]
- 9.Ogunbode O. Benign hydatidiform mole in Ibadan, Nigeria. Int J Gynecol Obstet. 1978;15:387–90. doi: 10.1002/j.1879-3479.1977.tb00715.x. [DOI] [PubMed] [Google Scholar]
- 10.Agboola A, Abudu O. Some epidemiological aspects of Trophoblastic disease in Lagos. Niger Med Pract. 1984;8:29–31. [Google Scholar]
- 11.Obiechina NJ, Udigwe GO, Obi RA. Molar pregnancy: A ten year review at Onitsha, Nigeria. J Med Invest Pract. 2001;3:26–31. [Google Scholar]
- 12.Ayangade O. Gestational trophoblastic disease in Nigeria: A 10-year review. East Afr Med J. 1979;56:278–82. [PubMed] [Google Scholar]
- 13.Evans AC, Soper JT, Hammond CB. Clinical features of molar pregnancies and gestational trophoblastic tumours. Obstet Gynaecol. 2003;87:182–205. [Google Scholar]
- 14.Goldstein DP, Berkowitz RS. Philadephia: W.B Saunders; 1982. Gestational trophoblastic neoplasms: Clinical principles of diagnosis and treatment; pp. 1–301. [PubMed] [Google Scholar]
- 15.Bagshawe KD, Dent J, Webb J. Hydatidiform mole in England and Wales 1973-1983. Lancet. 1986;2:673–7. doi: 10.1016/s0140-6736(86)90179-0. [DOI] [PubMed] [Google Scholar]
- 16.Curry SL, Hammond CB, Tyrey L, Creasman WT, Parker RT. Hydatidiform mole: Diagnosis, management and long-term follow-up of 347 patients. Obstet Gynecol. 1975;45:1–8. [PubMed] [Google Scholar]
- 17.Benson CB, Genest DR, Bernstein MR, Soto-Wright V, Goldstein DP, Berkowitz RS. Sonographic appearance of first trimester complete hydatidiform moles. Ultrasound Obstet Gynecol. 2000;16:188–91. doi: 10.1046/j.1469-0705.2000.00201.x. [DOI] [PubMed] [Google Scholar]
- 18.Kohorn EI. Molar pregnancy: presentation and diagnosis. Clin Obstet Gynecol. 1984;27:181–91. doi: 10.1097/00003081-198403000-00025. [DOI] [PubMed] [Google Scholar]
- 19.Hou JL, Wan XR, Xiang Y, Qi QW, Yang XY. Changes of clinical features in hydatidiform mole: analysis of 113 cases. J Reprod Med. 2008;53:629–33. [PubMed] [Google Scholar]
- 20.Tabas JA, Strehlow M, Isaacs E. A false negative pregnancy test in a patient with a hydatidiform molar pregnancy. N Engl J Med. 2003;349:2172–3. doi: 10.1056/NEJM200311273492221. [DOI] [PubMed] [Google Scholar]
- 21.Wolf BA, Garrett NC, Nahm MH. The “hook effect”: high concentrations of prostate-specific antigen giving artifactually low values on one-step immunoassay. N Engl J Med. 1989;320:1755–6. doi: 10.1056/NEJM198906293202614. [DOI] [PubMed] [Google Scholar]
- 22.Osamor JO, Oluwasola AO, Adewole IF. The clinico-pathological study of complete and partial hydatidiform moles in a Nigerian population. J Obstet Gynaecol. 2002;22:423–5. doi: 10.1080/01443610220141425. [DOI] [PubMed] [Google Scholar]
- 23.Eniola OA, Mabayole P, Oguniyi SO. Hydatiform mole in Ile-Ife, Nigeria: A 10 year review. J Obstet Gynaecol. 2001;21:405–7. doi: 10.1080/01443610120063739. [DOI] [PubMed] [Google Scholar]


