Abstract
Objective:
The objective of this study was to assess whether the concern about halitosis influence oral health attitude and practices among young literate adults in Nigeria.
Materials and Methods:
This cross-sectional survey of 400 randomly selected temporary camp resident adults in Anambra state, South Eastern Nigeria was conducted using a modified version of the Hiroshima University-Dental Behavioral Inventory questionnaire.
Results:
Out of the 400 questionnaires distributed, only 294 were filled and returned giving an overall response rate of 73.5%. Half (50.0%) of the participants in this study expressed concern about halitosis. The participants that expressed concern about halitosis were mostly in the 25- to 27-year-old age group, females, known smoker, regular dental floss, and mouth wash users, had incorrect tooth brushing knowledge, brushed teeth more frequently and more forcefully, had no previous dental treatment, prefer symptomatic dental visit, experienced gingival bleeding, expressed worry about the color of their gingiva and teeth but were satisfied with the dental appearance.
Conclusion:
Data from this study showed that concerns about halitosis-triggered behavioral reaction in oral self-care practices namely tooth brushing frequency, tooth brushing force, mouth wash, and dental floss use. Also revealed were poorer oral health and lower preventive dental visit practices among participants concerned about halitosis. There is need for improved public knowledge and awareness about halitosis by the dentist in Nigeria.
Keywords: Concern, halitosis, oral hygiene practices
INTRODUCTION
The pattern of health behavior contributes to the variation of disease affection among individuals exposed to similar environmental risk factor for a disease. One of the underlying factors that influence the pattern of health behavior is individuals’ concern about their health. Heightened concern is associated with improved health status and practices while low concern is associated with poor health status and practices.1 A previous study revealed that the most persuasive reasons for adopting preventive dental practice behaviors are susceptibility to disease and social and esthetic benefits.2 It is expected that the concern of individuals toward their mouth and the attitude to dentists who provide dental care would play an important role in determining their oral health condition.
Halitosis, a common reason for dentist consultation raises a lot of concern among sufferer as it negatively impacts on daily life activities like communication with other persons,3 self-esteem, self-confidence, social and intimate relationship like dating and marriage, employability, and career aspirations.4,5 It causes embarrassment, inhibits social interaction, and also decreases quality of life among afflicted individuals. The effect of halitosis extends beyond the afflicted individuals, as it is also a source of embarrassment for relatives and friends of individuals afflicted with halitosis. These effects alongside erroneous beliefs and worldwide spread stand out halitosis and concern about it as a major health issue.
The concern about halitosis triggers behavioral reaction namely increased oral self-care, self-consciousness, social isolation, suicide attempts, and suicide, mostly because of social, psychological, and relationship impediments.4 The fact that oral sources are majorly responsible for bad breath complaints6 indicates that oral self-care and lifestyle are the main contributors to the onset of this condition and early expected behavioral response would be changes in an individual's oral hygiene practices. Although, there has been established association between inadequate oral hygiene practices and halitosis,7 the influence on oral health practices by concern about halitosis appear not to have been investigated scientifically in the literature. The objective of this study was to assess whether the concern about halitosis influences oral health attitude and practices among young literates in Nigeria.
MATERIALS AND METHODS
Anambra state is one of five states that make up the South East geopolitical zone of Nigeria. A Nigerian graduate below the age of 30 years undergoing mandatory 1-year-national service in a State other than their State of origin and schooling is known as a youth corper. A cross-section of 2010 batch a youth corpers posted to Anambra state were studied during their orientation camp.
The stratified random sampling technique was utilized in selecting the youth corpers. In the first stage, the youth corpers were stratified according to platoons which is the basic group used in orientation camps for parade and other activities. In the second stage, randomization was done to select 40 participants from each platoon bringing the total sample size to 400. The corpers absent from the morning parade on the day of data collection for any reason were excluded from this study. The corpers were informed that to participate in the study was voluntary and were assured of strict confidentiality of their responses.
Informed consent was obtained from the participants before onset of the study. The questionnaires were distributed, filled, and returned during the regular morning parade. Data on oral health behavior were collected using the modified English version of the Hiroshima University-Dental Behavioral Inventory questionnaire, which was originally developed by Kawamura.8 The final tool of data collection was a 21-item self-administered which was a modification of Hiroshima University oral health questionnaire. The first four questionnaires assessed information on demography which included age, gender, qualification, and geopolitical region of origin. The remaining 17 questions which are closed ended with a dichotomous yes or no response assessed dentist visit, tooth brushing, worry about symptoms of oral diseases, satisfaction with the appearance of teeth, and smoking behaviors. Two questions assessed if respondents have visited the dentist and if they visited the dentist only when they have toothache. The eight questions assessed whether they brush their teeth twice-daily or more, whether their gums bleed while brushing, whether they have never being taught the ways to brush their teeth by professionals, their opinion about the status of their despite daily tooth brushing, their feeling about proper tooth brushing in reference to strong brushing strokes, their feeling about the amount of time spent on tooth brushing, their thought about teeth cleaning without toothpaste, and their opinion about prevention of gum disease with tooth brushing alone. Two questions assessed the use of dental floss and mouthwash on a regular basis. Two questions assessed the worry about the color of their gum and teeth. The question that assessed concern about halitosis was as follows: “Do you worry about having bad breath?” One question assessed whether they are satisfied with the appearance of their teeth. One question on smoking was as follows: “Are you a smoker?” The questionnaires were hand delivered and completed in the parade ground. Data were analyzed by using statistical packages for the social science version 15.0. Data were subjected to descriptive statistics like frequencies, percentages, cross-tabulation, and chi-square statistics with odd ratio (OD), and confidence interval (CI) reported. The higher frequencies were considered influence in this study. The results were presented in tabular and graphic forms.
RESULTS
Out of the 400 questionnaires distributed, only 294 were filled and returned giving an overall response rate of 73.5%. Majority 139 (47.3%) of the participants were in the 25- to 27-year-old age group. Among the participants, 146 (49.7%) were males while 148 (50.3%) were females. Two-thirds 196 (66.7%) had a bachelor degree while the remaining one-third 98 (33.3%) had a Higher National Diploma. About three-quarters 213 (72.4%) of the participants were from southern part of Nigeria [Table 1]. Half 147 (50.0%) of the respondents expressed concern about halitosis. The participants that expressed concern about halitosis were mostly in the 25- to 27-year-old age group; 73 (52.5), females; 76 (51.3%) (OD=0.90 CI 95%: 0.55–1.45), bachelor degree holders; 113 (57.7%) (OD=2.56, 95%: 1.51–4.39), and origins of southern part of Nigeria; 124 (58.2%) (OD=0.28, C.I 95%: 0.16–0.51) [Table 2]. The participants that expressed concern about halitosis had incorrect tooth brushing knowledge, brushed teeth more frequently and more forcefully, and experienced gingival bleeding during tooth brushing [Figure 1]. The participants that expressed concern about halitosis had not visited the dentist for treatment, preferred symptomatic dental visit, are known smokers, use dental floss, and mouth wash regularly [Figure 2]. The participants that expressed concern about halitosis reported more satisfied with their dental appearance but more expressed worried about the color of their gingiva and teeth [Figure 3].
Table 1.
Demographic characteristics and concerns about halitosis among the participants
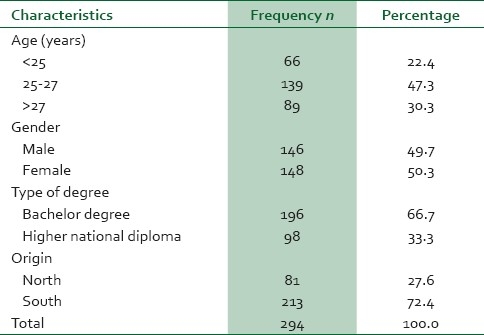
Table 2.
Demographic characteristics and concerns about halitosis among the participants
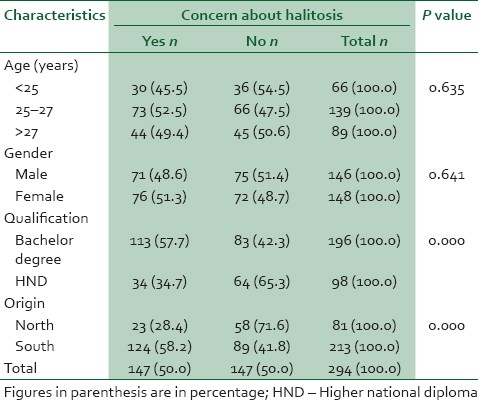
Figure 1.
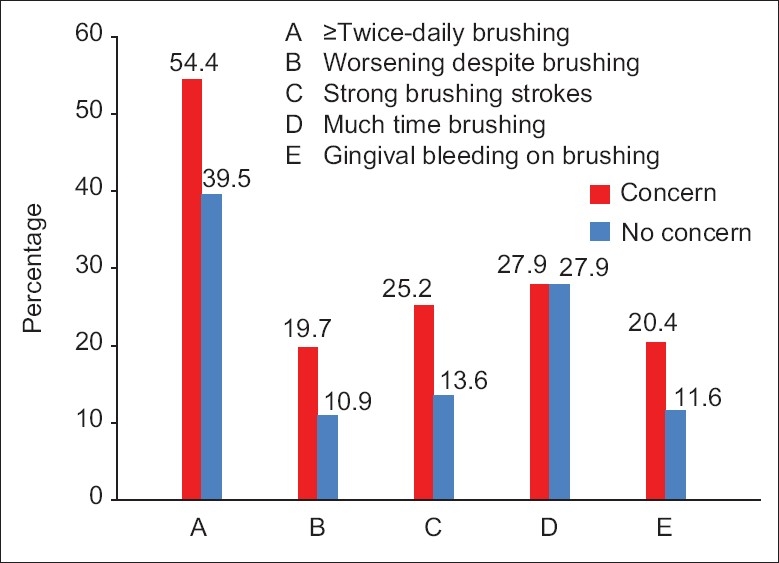
Tooth brushing behavior among the participants
Figure 2.
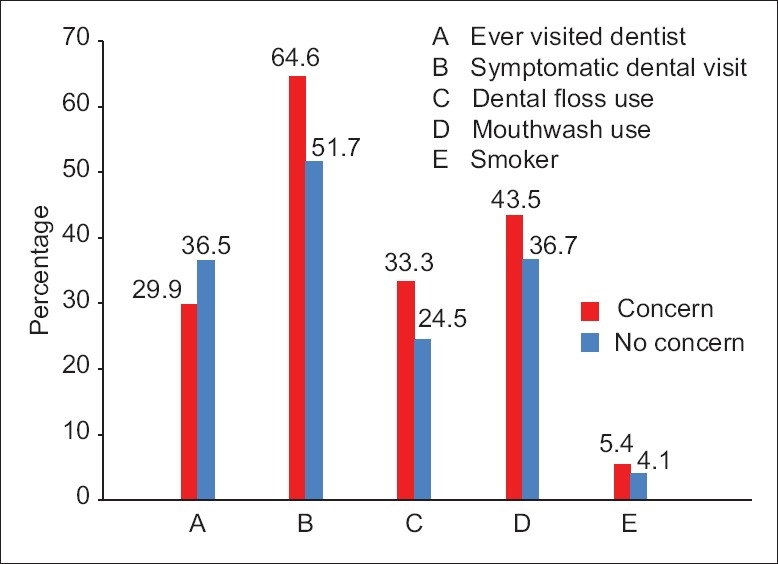
Dental visit pattern and other oral health behavior among the participants
Figure 3.
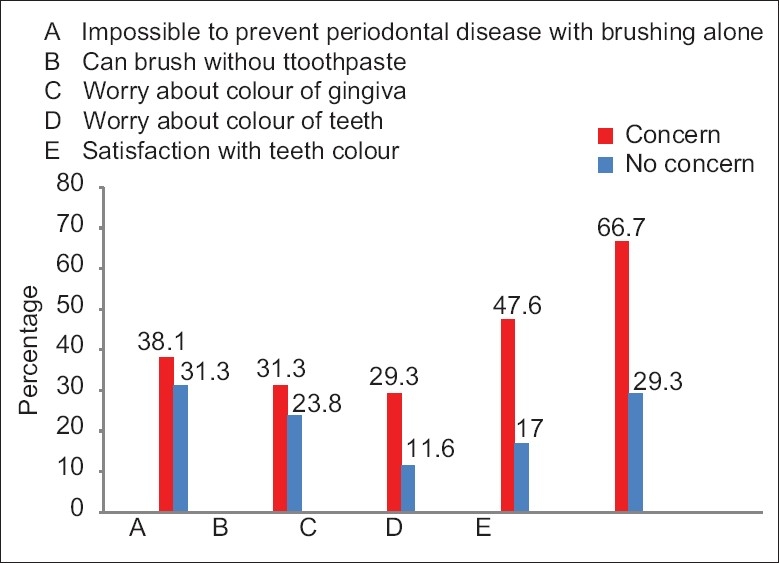
Attitude and worry toward oral health among the participants
DISCUSSION
Halitosis is a cause of concern, embarrassment, and frustration and can lead to social isolation, divorce, and even contemplation of suicide.4,9 In this study, the proportion of participants (50.0%) concerned about halitosis was high. This is similar to a study among the junior and senior high schools male students in Tokyo who expressed concern about halitosis3 but lower than 66.3% documented among dental students in India.10 This reflected the huge inert behavioral reaction to halitosis among the participants because of the psychosocial, intimate, and emotional impediment it poses to the afflicted individuals. The reason for high concern in this study is in threefold: Firstly, the stress and anxiety of living in a temporary camp among the participants may have contributed to the heightened concern about halitosis; secondly, lower dental visit among participants concerned about halitosis Figure 1 because dentists are primarily responsible for disseminating accurate information and diagnosis of halitosis;11 and thirdly, lack of exposure to the advertisements on halitosis, though not assessed in this study, may have generated erroneous and unwarranted concerns.12 The data from this study also showed that concern about halitosis was higher than self-reported halitosis documented in several studies7,13–17 conducted in Africa; 42 (14.0%), Middle East; 312 (23.3%), and Europe; 134 (32.0%), with a few exceptions like the studies among Thai dental patients18 523 (61.1%) and adolescents secondary children19 288 (72%) where the prevalence of perceived halitosis were higher.
The concern about halitosis was higher among females than males, although this was not significant (P=0.641). The fact that females are more concerned about their oral hygiene and appearance20 may explain the over-exaggerated concern. In paternalistic society like Nigeria, the relationship problem exemplified in dating, intimate relationship, marriage associated with halitosis4 may be the obvious reason why more females were more concerned than males. The increased anxiety about halitosis,21 increased capability of females in detecting malodour22 and higher receipt of complaints of halitosis from relatives13 in comparison to their male counterparts may be contributory. All the studied participants had tertiary education and mostly those in 25- to 27-year-old age group, bachelor degree holder, of southern region expressed concern about halitosis. The concern and self-reporting obviously differ as self-perceived halitosis in the literature was significantly associated with being ≥30 years, having high school education or less.7 Settineri et al. reported it to be linked with being 30 years of age or older.2
The participants who expressed concern about halitosis had poor oral health and exhibited poor preventive dental visit practices as exemplified by being smokers, never visited the dentist, preferred symptomatic dental visit, never received professional instruction on tooth brushing, and had gingival bleeding on brushing. This is tandem with the fact that individuals with halitosis averagely place less importance both on their mouth and that of others, exhibit poor oral hygiene, gingival problems, and dentist relational anxiety.2,23 The increased anxiety level from heightened concern about halitosis may ultimately resulting in halitosis.2,23 Nalcaci et al.24 reported self-reported halitosis as being significantly associated with inadequate oral hygiene practice and smoking. The striking association found between organoleptic halitosis scores and the bleeding index25 and also self-reported halitosis with gingival bleeding14,26,27 in the literature conforms to more concern about halitosis among participants with gingival bleeding on brushing in this study. Unadjusted logistic regressions also revealed that perceived halitosis is more likely in adolescent experiencing gingival bleeding during brushing.19 This is anchored on the fact that blood decomposition products produce sulfur-containing peptides and amino acids that are source of Volatile sulphur compounds (VSCs) responsible for halitosis.28
In most instances, halitosis stems from putrefactive microbial activity within the oral cavity itself and can be alleviated by proper oral hygiene and dental care29 yet concerned participants in this study never visited the dentist and preferred symptomatic dental visit option. The lower contact among participants concerned about halitosis and the dentist explained their higher non-receipt of professional instruction on tooth brushing and overall satisfaction with appearance of their teeth in this study.
Halitosis whose main oral causes are tongue coating and periodontal diseases30 is a complaint that often creates personal discomfort and social embarrassment.31,32 Mechanical cleaning of teeth in the form of tooth brushing and flossing is essential mechanical means of oral hygiene that lead to reduced amount of oral bacteria and substrates and presumably reducing halitosis.33,34 However, mechanical methods’ inability to effectively reach and remove VSC-producing bacteria from all oral ecological sites has been noted. Mouth washes and rinses considered more effective in reaching the less accessible parts of the oral cavity, with greater social acceptance and ease of use availability as over the counter medication.35,36 In people with rigorous oral hygiene, clean and sound dentition and a healthy periodontium, the source of bad breath is likely to be the back of the tongue.
Although poor self-care has been implicated in halitosis7 participants concerned about halitosis in this study reported increased tooth brushing frequency and force, mouth wash use and dental floss use. This conforms from evidence in the literature where a significant association was found between halitosis and the use of a toothbrush on a daily basis.11 Bosy,31 reported the desperate attempts to mask oral malodor with mints and chewing gum, compulsive brushing, and repeated use of mouth rinses. However, this contrasted with Liu et al.'s finding where social and behavioral factors did not contribute to halitosis in the Chinese population.25 The attempt to self-manage the concern about halitosis may have triggered increased tooth brushing frequency and force, mouth wash use, and dental floss use and this may be connected with the fact that individuals concerned about their bad breath are often embarrassed to ask others whether they actually suffer from it37 and that halitosis has a distressing effect which uniquely inhibiting afflicted individuals socialization.11
CONCLUSION
Data from this study showed that concerns about halitosis-triggered behavioral reaction in oral self-care practices namely tooth brushing frequency, tooth brushing force, mouthwash, and dental floss use. Also revealed were poorer oral health and lower preventive dental visit practices among participants concerned about halitosis. There is need for improved public knowledge and awareness about halitosis by dentists.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bolden AJ, Logan HL, Jakobsen JR, Evans TA. Perception of oral health needs by Southeast Iowa non-dental health care providers. Spec Care Dentist. 1994;14:194–7. doi: 10.1111/j.1754-4505.1994.tb01130.x. [DOI] [PubMed] [Google Scholar]
- 2.Settineri S, Mento C, Gugliotta SC, Saitta A, Terranova A, Trimarchi G, et al. Self-reported halitosis and emotional state: Impact on oral conditions and treatments. Health Qual Life Outcomes. 2010;8:34. doi: 10.1186/1477-7525-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yanagisawa T, Shinada K, Kawaguchi Y. The questionnaire survey on oral malodor and teeth stains of male high school students. Kokubyo Gakkai Zasshi. 2005;72:56–61. doi: 10.5357/koubyou.71and72.56. [DOI] [PubMed] [Google Scholar]
- 4.Azodo CC, Osazuwa-Peter N, Omili M. Psychological and social impacts of halitosis: A review. J Soc Psychol Sci. 2010;3:74–91. [Google Scholar]
- 5.Ongole R, Shenoy N. Halitosis: Much beyond oral malodor. Kathmandu Univ Med J (KUMJ) 2010;8:269–75. doi: 10.3126/kumj.v8i2.3574. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg M. Clinical assessment of bad breath: Current concepts. J Am Dent Assoc. 1996;127:475–82. doi: 10.14219/jada.archive.1996.0239. [DOI] [PubMed] [Google Scholar]
- 7.Al-Ansari JM, Boodai H, Al-Sumait N, Al-Khabbaz AK, Al-Shammari KF, Salako N. Factors associated with self-reported halitosis in Kuwaiti patients. J Dent. 2006;34:444–9. doi: 10.1016/j.jdent.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Kawamura M. Dental behavioral science: The relationship between perceptions of oral health and oral status in adults. Hiroshima Daigaku Shigaku Zasshi. 1988;20:273–86. [PubMed] [Google Scholar]
- 9.Rosenberg M. Halitosis – the need for further research and education. J Dent Res. 1992;71:424. doi: 10.1177/00220345920710021301. [DOI] [PubMed] [Google Scholar]
- 10.Dagli RJ, Tadakamadla DS, Dhanni C, Duraiswamy P, Kulkarni S. Self reported dental health attitude and behavior of dental students in India. J Oral Sci. 2008;50:267–72. doi: 10.2334/josnusd.50.267. [DOI] [PubMed] [Google Scholar]
- 11.Eldarrat AH. Influence of oral health and lifestyle on oral malodour. Int Dent J. 2011;61:47–51. doi: 10.1111/j.1875-595X.2011.00010.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenberg M, Kozlovsky A, Gelernter I, Cherniak O, Gabbay J, Baht R, et al. Self-estimation of oral malodor. J Dent Res. 1995;74:1577–82. doi: 10.1177/00220345950740091201. [DOI] [PubMed] [Google Scholar]
- 13.Eldarrat A, Alkhabuli J, Malik A. The prevalence of self-reported halitosis and oral hygiene practices among Libyan students and office workers. Libyan J Med. 2008;3:170–6. doi: 10.4176/080527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mumghamba EG, Manji KP, Michael J. Oral hygiene practices, periodontal conditions, dentition status and self-reported bad mouth breath among young mothers, Tanzania. Int J Dent Hyg. 2006;4:166–73. doi: 10.1111/j.1601-5037.2006.00186.x. [DOI] [PubMed] [Google Scholar]
- 15.Almas K, Al-Hawish A, Al-Khamis W. Oral hygiene practices, smoking habits, and self-perceived oral malodor among dental students. J Contemp Dent Pract. 2003;4:77–90. [PubMed] [Google Scholar]
- 16.Meningaud JP, Bado F, Favre E, Bertrand JC, Guilbert F. Halitosis in 1999. Rev Stomatol Chir Maxillofac. 1999;100:240–4. [PubMed] [Google Scholar]
- 17.Bornstein MM, Kislig K, Hoti BB, Seemann R, Lussi A. Prevalence of halitosis in the population of the city of Bern, Switzerland: A study comparing self-reported and clinical data. Eur J Oral Sci. 2009;117:261–7. doi: 10.1111/j.1600-0722.2009.00630.x. [DOI] [PubMed] [Google Scholar]
- 18.Youngnak-Piboonratanakit P, Vachirarojpisan T. Prevalence of self-perceived oral malodor in a group of Thai dental patients. J Dent (Tehran) 2010;7:196–204. [PMC free article] [PubMed] [Google Scholar]
- 19.Kida IA, Manyori C, Masalu JR. Prevalence and correlates of perceived oral malodor among adolescents in Temeke district, Dar es Salaam. East Afr J Public Health. 2010;7:49–53. doi: 10.4314/eajph.v7i1.64675. [DOI] [PubMed] [Google Scholar]
- 20.Sanz M, Roldán S, Herrera D. Fundamentals of breath malodour. J Contemp Dent Pract. 2001;2:1–17. [PubMed] [Google Scholar]
- 21.Oho T, Yoshida Y, Shimazaki Y, Yamashita Y, Koga T. Characteristics of patients complaining of halitosis and the usefulness of gas chromatography for diagnosing halitosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:531–4. doi: 10.1067/moe.2001.112543. [DOI] [PubMed] [Google Scholar]
- 22.Stuck BA, Frey S, Freiburg C, Ho¨rmann K, Zahnert T, Hummel T. Chemosensory event-related potentials in relation to side of stimulation, age, sex, and stimulus concentration. Clin Neurophysiol. 2006;117:1367–75. doi: 10.1016/j.clinph.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 23.Calil CM, Marcondes FK. Influence of anxiety on the production of oral volatile sulfur compounds. Life Sci. 2006;79:660–4. doi: 10.1016/j.lfs.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 24.Nalcaci R, Baran Factors associated with self-reported halitosis (SRH) and perceived taste disturbance (PTD) in elderly. Arch Gerontol Geriatr. 2008;46:307–16. doi: 10.1016/j.archger.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Liu XN, Shinada K, Chen XC, Zhang BX, Yaegaki K, Kawaguchi Y. Oral malodor-related parameters in the Chinese general population. J Clin Periodontol. 2006;33:31–6. doi: 10.1111/j.1600-051X.2005.00862.x. [DOI] [PubMed] [Google Scholar]
- 26.Levin L, Rosenberg M. Oral hygiene, caries status and bad breath among young Israeli recruits. (85).Refuat Hapeh Vehashinayim. 2005;22:27–31. [PubMed] [Google Scholar]
- 27.Migliario M, Rimondini L. Oral and non oral diseases and conditions associated with bad breath. Minerva Stomatol. 2011;60:105–15. [PubMed] [Google Scholar]
- 28.Romano F, Pigella E, Guzzi N, Aimetti M. Patients’ self-assessment of oral malodour and its relationship with organoleptic scores and oral conditions. Int J Dent Hyg. 2010;8:41–6. doi: 10.1111/j.1601-5037.2009.00368.x. [DOI] [PubMed] [Google Scholar]
- 29.Yaegaki K, Sanada K. Volatile sulfur compounds in mouth airfrom clinically healthy subjects and patients with periodontal disease. J Periodontal Res. 1992;27:233–8. doi: 10.1111/j.1600-0765.1992.tb01673.x. [DOI] [PubMed] [Google Scholar]
- 30.Delanghe G, Ghyselen J, van Steenberghe D, Feenstra L. Multidisciplinary breath-odour clinic. Lancet. 1997;350:187. doi: 10.1016/S0140-6736(05)62354-9. [DOI] [PubMed] [Google Scholar]
- 31.Bosy A. Oral malodor: philosophical and practical aspects. J Can Dent Assoc. 1997;63:196–201. [PubMed] [Google Scholar]
- 32.Delanghe G, Ghyselen L, Feenstra L, van Steenberghe D. Experiences of a Belgian multidisciplinary breath odour clinic. In: Van Steenberghe D, Rosenberg M, editors. A multidisciplinary approach. Leuven: Leuven University Press; 1996. pp. 199–208. [Google Scholar]
- 33.Quirynen M, Zhao H, van Steenberghe D. Review of the treatment strategies for oral malodour. Clin Oral Investig. 2002;6:1–10. doi: 10.1007/s00784-002-0152-9. [DOI] [PubMed] [Google Scholar]
- 34.Tanaka M, Anguri H, Nishida N, Ojima M, Nagata H, Shizukuishi S. Reliability of clinical parameters for predicting the outcome of oral malodor treatment. J Dent Res. 2003;82:518–22. doi: 10.1177/154405910308200706. [DOI] [PubMed] [Google Scholar]
- 35.Richter JL. Diagnosis and treatment of halitosis. Compend Contin Educ Dent. 1996;17:370–2. 374-6 passim; quiz 388. [PubMed] [Google Scholar]
- 36.Ayers KM, Colquhoun AN. Halitosis: causes, diagnosis, and treatment. N Z Dent J. 1998;94:156–60. [PubMed] [Google Scholar]
- 37.Rosenberg M, Knaan T, Cohen D. Association among bad breath, body mass index, and alcohol intake. J Dent Res. 2007;86:997–1000. doi: 10.1177/154405910708601015. [DOI] [PubMed] [Google Scholar]


