To the Editor
Commotio Retinae is a transient opacification of the retina due to outer retinal disruption occurring in a contre-coup fashion after blunt trauma injury.1,2 Histological studies in animals and humans after ocular blunt trauma have revealed that disruption occurs at the level of the photoreceptor outer segments and retinal pigment epithelium (RPE).2,3 Recent reports using optical coherence tomography (OCT) have shown detectable disruption at the level of photoreceptor inner segment/outer segment junction and RPE 4-6 and that these changes may be reversible overtime with restoration of normal outer retinal architecture.5 However, resolution of existing OCT technology may not be sensitive enough to detect photoreceptor disruption. Adaptive optics (AO) imaging systems enable cellular-resolution imaging of the human retina, and there is a growing number of cases where deficits have been visible on AO images but not on OCT. Here we present a case of subclinical photoreceptor disruption after head trauma as seen by adaptive optics scanning ophthalmoloscope (AOSO) not apparent clinically or on spectral domain-OCT.
Report of a Case
A 43-year-old male described a 5-year history of a stable, crescent-shaped purple scotoma nasal to central fixation in his right eye that developed after an industrial accident in which he sustained significant head and body trauma. A complete ophthalmic examination revealed best-corrected vision of 20/20 OU and no fundus findings or abnormalities. Fluorescein angiogram (FA) and spectral domain optical coherence tomography (SD-OCT) (Spectralis SD-OCT, Heidelberg Engineering, Carlsbad, CA) were unremarkable. (Figure 1) Humphrey Visual Field 10-2 testing and microperimetry revealed a small nonspecific area of functional visual loss near fixation in the right eye. Images of the photoreceptor mosaic near the fovea were acquired using a newly developed AOSO. Images were processed and registered using custom MatLab software (The Math works, Natwick, MA). While foveal cone density was normal, the AOSO images revealed a well-defined crescent-shaped area of photoreceptor disruption just temporal to the fovea. (Figure 2A – large arrows) Other focal areas of photoreceptor irregularities were also seen superior, temporal and inferior temporal to the fovea. (Figure 2A- small arrows) Both cone and rod photoreceptors were visualized with this AOSO imaging, and both cell types appear to be disrupted. (Figure 2 A, B)
Figure 1. Clinical imaging, right eye.
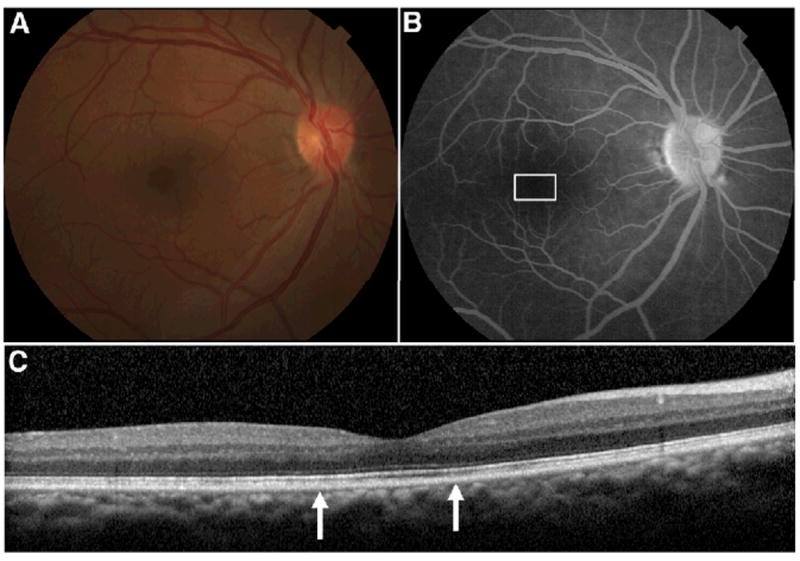
A. Color fundus photo showing no macular abnormalities. B. Late frame fluorescein angiogram showed no window defect, staining or leakage. White box indicates area imaged by adaptive optics scanning ophthalmoscope (AOSO) as seen in figure 2. C. Spectralis SD-OCT horizontal scan through the fovea showing no outer retinal abnormalities. Area between arrows indicates region imaged by AOSO as seen in figure 2.
Figure 2. Disrupted photoreceptor mosaic, macula, right eye.
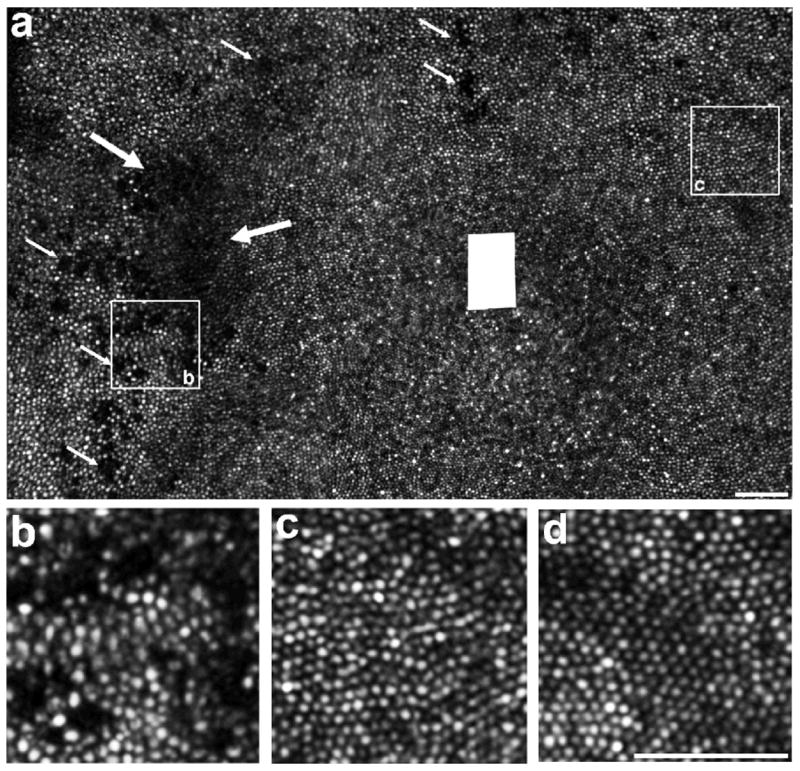
A. Adaptive optics scanning ophthalmoscope montage shows a large, crescent-shaped area of photoreceptor disruption (edges indicated by large arrows) temporal to fovea. Multiple other areas of photoreceptor disruption are also present (small arrows). Foveal center was not imaged, and is marked by the solid white rectangle. B. Magnified view of a patch of retina 1-degree temporal from the fovea, centered on an area of significant photoreceptor disruption. C. Magnified view of a patch of retina 1-degree nasal from the fovea, showing regularly packed cone photoreceptor mosaic. D. Image from a normal control, about 1-degree temporal from the fovea. Scale bar for all images is 50 microns.
Comment
AOSO detected photoreceptor disruption resulting from head trauma not apparent clinically or by other standard imaging modalities, including SD-OCT. Restoration of outer retinal appearance in SD-OCT has been reported after commotio retinae5, suggesting recovery of outer retinal structure. Our data demonstrate photoreceptor disruption may still exist. SD-OCT axial resolution is likely not sensitive enough to reveal the full extent of photoreceptor disruption that may occur after ocular or head trauma. AOSO imaging may prove useful in improved detection and understanding of photoreceptor involvement in ocular or head trauma. In addition, patients with traumatic brain injury often report visual symptoms. AOSO may be of value to help differentiate retinal versus cortical contributions to vision loss in these patients.
Acknowledgments
Support for this project comes from Clinical and Translational Science Institute and the Biotechnology Innovation Center, Medical College of WI, CTSA Grant UL1 RR 031973, Thomas M. Aaberg Sr. Retina Research Fund, E. Matilda Ziegler Foundation for the Blind, RD and Linda Peters Foundation, Research to Prevent Blindness, and NIH (EY017607, EY001931, EY014537). J.C. is the recipient of a Career Development Award from RPB. Alfredo Dubra Ph.D. holds a Career Award at the Scientific Interface from the Burroughs Wellcome Fund. This investigation was conducted in a facility constructed with support from the Research Facilities Improvement Program, grant number C06 RR-RR016511, from the National Center for Research Resources, National Institutes of Health.
Footnotes
Author Contributions: Dr. Stepien had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Presented at the Association for Research in Vision and Ophthalmology annual meeting 2011, Fort Lauderdale, FL, poster session, May 3rd, 2011.
References
- 1.Liem AT, Keunen JE, van Norren D. Reversible cone photoreceptor injury in commotio retinae of the macula. Retina. 1995;15(1):58–61. doi: 10.1097/00006982-199515010-00011. [DOI] [PubMed] [Google Scholar]
- 2.Sipperley JO, Quigley HA, Gass DM. Traumatic retinopathy in primates. The explanation of commotio retinae. Arch Ophthalmol. 1978 Dec;96(12):2267–2273. doi: 10.1001/archopht.1978.03910060563021. [DOI] [PubMed] [Google Scholar]
- 3.Mansour AM, Green WR, Hogge C. Histopathology of commotio retinae. Retina. 1992;12(1):24–28. doi: 10.1097/00006982-199212010-00006. [DOI] [PubMed] [Google Scholar]
- 4.Bradley JL, Shah SP, Manjunath V, Fujimoto JG, Duker JS, Reichel E. Ultra-high-resolution optical coherence tomographic findings in commotio retinae. Arch Ophthalmol. 2011 Jan;129(1):107–108. doi: 10.1001/archophthalmol.2010.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Itakura H, Kishi S. Restored photoreceptor outer segment in commotio retinae. Ophthalmic Surg Lasers Imaging. 2011;42:e29–31. doi: 10.3928/15428877-20110217-03. Online. [DOI] [PubMed] [Google Scholar]
- 6.Seider MI, Lujan BJ, Gregori G, Jiao S, Murray TG, Puliafito CA. Ultra-high resolution spectral domain optical coherence tomography of traumatic maculopathy. Ophthalmic Surg Lasers Imaging. 2009 Sep-Oct;40(5):516–521. doi: 10.3928/15428877-20090901-16. [DOI] [PubMed] [Google Scholar]


