Summary
The hypoglossal canal contains a venous plexus that connects the inferior petrous sinus, condylar vein, jugular vein and paravertebral plexus. The venous plexus is one of the venous drainage routes of the posterior skull base. Only a few cases of dural arteriovenous fistulas (AVFs) involving the hypoglossal canal have been reported.
We describe three cases (a 62-year-old female, a 52-year-old male, and an 83-year-old male) of dural AVFs involving the hypoglossal canal. Symptoms were pulse-synchronous bruit in two cases and proptosis/chemosis in one. All dural AVFs were mainly fed by the ipsilateral ascending pharyngeal artery. Two of three dural AVFs involving the hypoglossal canal mainly drained through the anterior condylar confluence into the inferior petrosal sinus retrogradely with antegrade drainage through the lateral condylar vein. The other one drained through the lateral and posterior condylar veins into the suboccipital cavernous sinus. All dural AVFs were completely occluded by selective transvenous embolization without any complications, and the symptoms disappeared within one week in all cases.
Dural AVFs involving the hypoglossal canal can be successfully treated by selective transvenous embolization with critical evaluation of venous anatomy in each case.
Key words: dural AVShunt, posterior fossa
Introduction
The hypoglossal canal is one of the most important canals of the posterior skull base. It is located inferior-medially to the jugular foramen, and contains the hypoglossal nerve, hypoglossal branch of the ascending pharyngeal artery, and venous plexus so called the anterior condylar vein. The posterior condylar vein arises at the most medial portion of the sigmoid sinus and drains through the posterior condylar canal into the suboccipital cavernous sinus posteriorly.
A few cases of dural arteriovenous fistulas (AVFs) involving the hypoglossal canal have been reported. We present three cases of dural AVF involving the hypoglossal canal treated with transvenous embolization, and discuss the characteristics and treatment of these subgroups of dural AVFs.
Case Reports
Case 1
A 62-year-old female presented with left pulse synchronous bruit for six months. MR angiography showed abnormal vascular signal of the left inferior petrosal sinus. Diagnostic angiography showed the dural AVF locating medially to the jugular vein (figure 1A), fed by the left ascending pharyngeal artery and left posterior meningeal artery. Selective angiography of the left ascending pharyngeal artery clearly showed the dural AVF drains through the anterior condylar confluence retrogradely into the inferior petrosal sinus, and antegradely to the jugular vein and the lateral condylar vein to the suboccipital cavernous sinus (figure 1B).
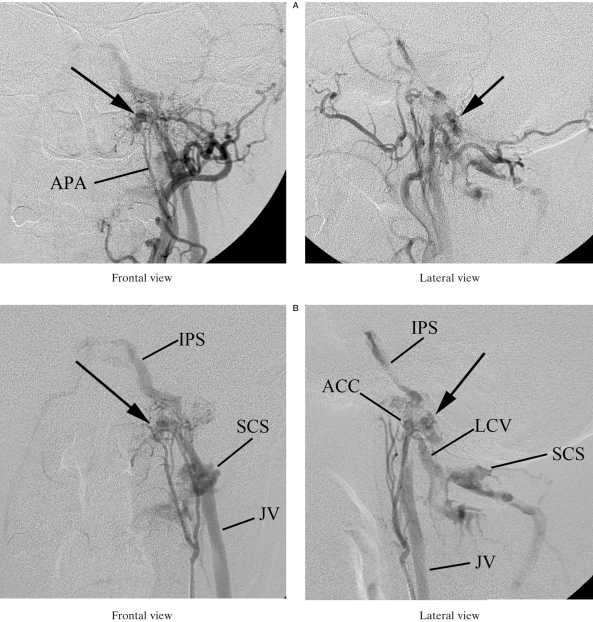
Figure 1.
A) Left external carotid angiography (Lt ECAG) shows DAVF (arrows) locating medially to left jugular vein, fed by the left ascending pharyngeal artery (APA). B) Selective angiography of the left ascending pharyngeal artery clearly shows DAVF (arrow) drains through the left anterior condylar confluence (ACC) retrogradely into the left inferior petrosal sinus (IPS), and antegradely to the left jugular vein (JV) and lateral condylar vein (LCV) to the suboccipital cavernous sinus (SCS). C) After the microcatheter was advanced through the jugular vein and anterior condylar confluence into the anterior condylar vein, selective venous embolization was performed using detachable coils (Detach coil system, Cook). D) Left external carotid arteriogram shows complete disappearance of DAVF. E) CT shows coils located in the left hypoglossal canal (arrow).
The patient was treated by transvenous embolization. A microcatheter (Excelsior, Boston Scientific Japan, Tokyo, Japan) was advanced through the jugular vein and the anterior condylar confluence into the anterior condylar vein (figure 1C).
Selective venous embolization was performed with coils (Detach-11/18, William Cook Europe, Bjaerverskov, Denmark), and the dural AVF was completely occluded (figure 1D). CT after embolization shows the coils in the hypoglossal canal (figure 1E). The symptom was cured and no recurrence was observed during a six-month follow-up period.
Case 2
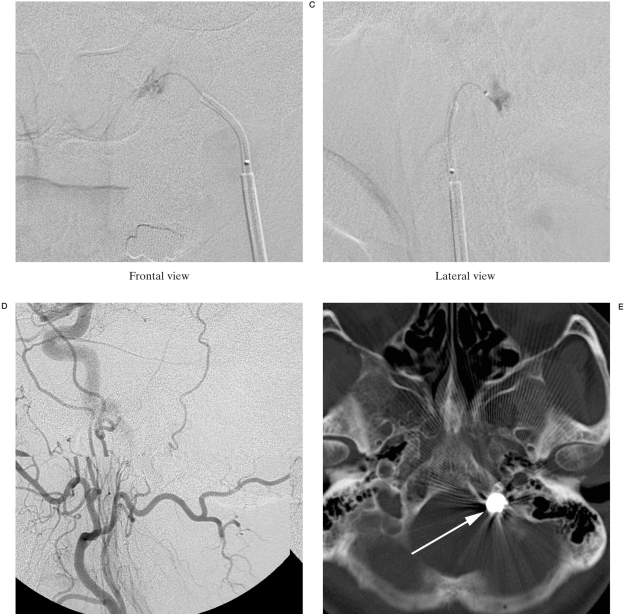
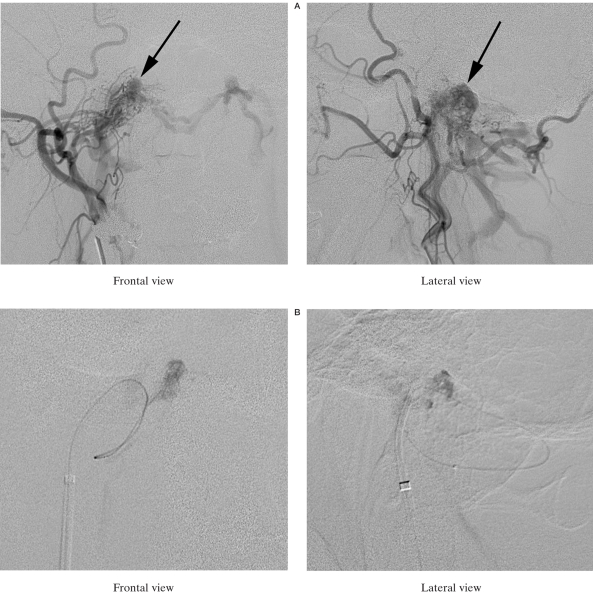
A 52-year-old male presented with a two month history of right pulse synchronous bruit. MR angiography showed an abnormal signal postero-medially to both carotid arteries. Diagnostic angiography showed the dural AVF fed mainly by the right ascending pharyngeal artery and the right occipital artery and draining through the lateral and posterior condylar veins into the suboccipital cavernous sinus and the contralateral condylar veins (figure 2A). The dural AVF was also supplied by the right dorsal clival artery, the left ascending pharyngeal artery and the odontoid arteries. Transvenous embolization was performed. At first, we tried to advance a microcatheter (Excelsior, Boston Scientific Japan, Tokyo, Japan) via the jugular vein and the anterior condylar confluence into the anterior condylar vein, but failed because of the significant narrowing of the anterior outlet of the confluence. Then, we successfully introduced the microcatheter into the anterior condylar vein through the sigmoid sinus, posterior condylar vein, suboccipital cavernous sinus, and the lateral condylar vein (figure 2B,C). The anterior condylar vein was packed with coils (Detach-11, William Cook Europe, Bjaerverskov, Denmark) and the dural AVF was completely occluded. CT after embolization showed coils in the hypoglossal canal (figure 2D). The symptom disappeared and no recurrence was observed during a ten month follow-up period (figure 2E).
Figure 2.
A) Right external carotid angiography shows DAVF (arrows) fed by the ascending pharyngeal artery and occipital artery. This DAVF drained into the suboccipital cavernous sinus and contralateral condylar veins via the lateral and posterior condylar veins. B) The microcatheter was introduced into the anterior condylar vein via the sigmoid sinus, posterior condylar vein, suboccipital cavernous sinus and lateral condylar vein. C) Schematic drawing of the catheterization route from the sigmoid sinus to the anterior condylar vein. IPS: inferior petrosal sinus, ACC: anterior condylar confluence, ACV: anterior condylar vein, PCV: posterior condylar vein, LCV: lateral condylar vein, SCS: suboccipital cavernous sinus, HGC: hypoglossal canal, JV: jugular vein. D) Right external carotid arteriogram shows complete disappearance of DAVF. E) CT shows coils located in the right hypoglossal canal (arrow).
Case 3
An 83-year-old male presented with right sudden proptosis, chemosis and diplopia. MRI T2 weighted images showed dilated superior ophthalmic vein and inferior petrosal sinus, and signal void in the right hypoglossal canal.
The dural AVF was fed by the right ascending pharyngeal artery and the occipital artery, and drained mainly into the inferior petrosal sinus to the superior ophthalmic vein, and into the lateral condylar vein and the jugular vein. Left carotid angiography clearly demonstrated a shunting venous pouch.
Transvenous embolization was performed with catheterization through the jugular vein and anterior condylar confluence into the venous pouch.
Angiography after embolization showed complete occlusion of the dural AVF, and CT showed coils in the hypoglossal canal. The symptoms disappeared within a week and no recurrence was observed during the eight-month follow-up period.
Discussion
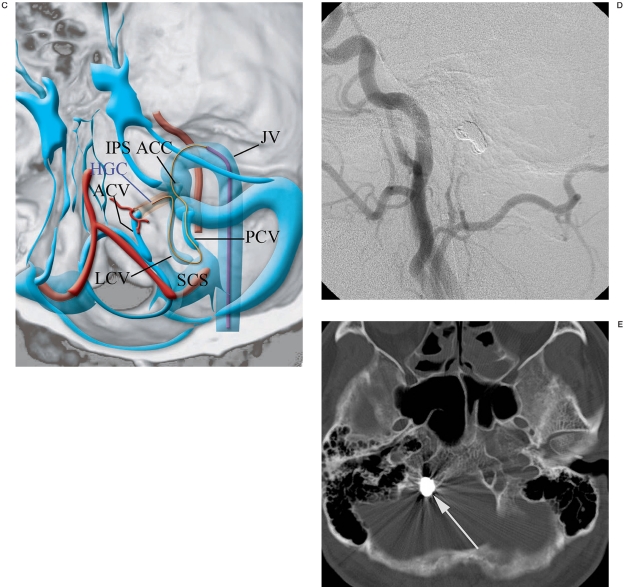
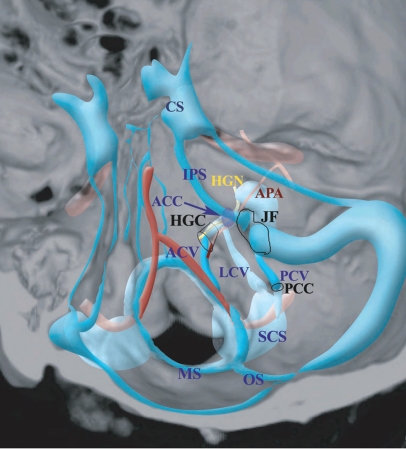
The hypoglossal canal (anterior condylar canal) is one of the most important canals of the posterior skull base. It is located inferior-medially to the jugular foramen, and contains the hypoglossal nerve, neuromeningeal branch of the ascending pharyngeal artery, and venous plexus so called the anterior condylar vein (figure 3). The anterior condylar vein connects with the jugular vein laterally and with the marginal sinus medially. It connects with the suboccipital sinus inferiorly via the lateral condylar vein and posterior condylar vein. Each condylar vein drains to the jugular vein at almost same site anterocaudally. It is called the anterior condylar confluence. These veins form one of the important venous drainage routes of the skull base and it is known that many normal variations exist1. Takahashi et Al evaluated the venous anatomy and variation of the craniocervical junction using contrast-enhanced 3D fast SPGR2. This technique is useful for evaluating the venous structures before transvenous embolization for dural AVFs.
Figure 3.
See also figure 2C. CS: cavernous sinus, APA: ascending pharyngeal artery, JF: jugular foramen, MS: marginal sinus, OS: occipital sinus.
Only nine cases of dural AVFs (including our three cases) involving the hypoglossal canal have been described in previous reports3-7. Many cases may be diagnosed as dural AVFs of the marginal sinus or cranio-cervical junction because of similar appearance on angiography 3.
In the last six years, we experienced 58 cases of dural AVF. Hypoglossal canals dural AVF found in 5.1% of cases is the fourth frequent location in our series (Table 1). Table 2 shows the summary of nine cases of hypoglossal canal dural AVF previously reported and presented cases. There is a tendency of female dominance. Bruit is the most frequent symptom, but ophthalmic symptoms were also found in three out of nine cases. The ipsilateral ascending pharyngeal artery always fed the AVFs with additional feeders from the occipital artery or posterior meningeal branch of the vertebral artery. Furthermore the contralateral ascending pharyngeal artery and occipital artery frequently fed the dural AVFs. Arteriography of the contralateral carotid artery is useful for description of shunt point4. Regarding the draining veins, retrograde drainage via the inferior petrosal sinus was often seen.
Table 1.
Occurrence of DAVs in our institution during 1999-2005.
| Location | N° of cases | |
|---|---|---|
| Cavernous sinus | 25 | (43.1%) |
| Trans-sigmoid sinus | 16 | (27.6%) |
| Tentorial sinus | 5 | (8.6%) |
| Hypoglossal canal | 3 | (5.1%) |
| Marginal sinus | 2 | (3.4%) |
| Superior sagittal sinus | 1 | (3.4%) |
| Convexity | 2 | (3.4%) |
| Anterior fossa | 1 | (1.7%) |
| Superior petrosal sinus | 1 | 1.7%) |
| Posterior condylar canal | 1 | (1.7%) |
Table 2.
Previous reports of hypoglossal canal Dural AVF
| Case | Sympton | Feeding artery | Draining vein | Treatment / Result | TVE access route |
|---|---|---|---|---|---|
| 1. 65 F | Bruit, Chemosis | APA & OA | IPS-CS-SOV | TVE/Cured | SOV-CS-IPS |
| 2. 74 F | Bruit, Chemosis | Bilt.APA | JV, IPS-CS-SOV |
TAE/Recurred —►TVE/Cured |
JV-ACC |
| 3. 74 F | Headache, Bruit | Bilt.APA | JV, TSS |
TAE + SRT/Failed —►TVE/Cured |
JV-ACC |
| 4. 57 F | Headache, Bruit | APA & OA | JV | TVE/Cured | JV-ACC |
| 5. 67 F | Bruit | Bilt. APA & VA | JV, IPS,MS | TVE/Cured | JV-ACC |
| 6. 64 F | Bruit, Chemosis | Bilt. APA, VA | IPS-CS-SOV | TVE /Cured | JV-ACC |
| 7. 62 F | Bruit | APA, Bilt. VA | IPS, JV, VPlx | TVE/Cured | JV-ACC |
| 8. 54 M | Bruit | Bilt.APA, OA, DCA,VA | VPlx, MS, JV | TVE /Cured | PCV-SCS-LCV-ACC |
| 9. 83 M | Chemosis, Diplopia | Bilt. APA & OA, DCA | IPS-CS-SOV, JV | TVE/Cured | JV-ACC |
|
APA: ascending pharyngeal artery, OA: occipital artery, VA: vertebral artery, DCA: dorsal clival artery, IPS: inferior petrosal sinus, CS: cavernous sinus, SOV: superior orbital vein, JV: jugular vein, TSS: transverse-sigmoid sinus, VPlx: vertebral plexus, MS: marginal sinus, OS: occipital sinus, ACC: anterior condylar confluence, SCS: suboccipital cavernous sinus, LCV: lateral condylar canal, TAE: transarterial embolization, TVE: transvenous embolization, SRT: stereotactic radiation therapy. Case 1: Ref 7, Case 2-4: Ref 3, Case 5: Ref 5, Case 6: Ref 6, Case 7-9: Present cases | |||||
When retrograde drainage reaches the ophthalmic vein via the cavernous sinus, ophthalmic symptoms are seen. Although not mentioned in previous reports, we found the dural AVF frequently draining through the suboccipital cavernous sinus into the vertebral plexus on source images from MR angiography. This would be important for determination of the access routes of the transvenous approach. Cases of dural AVFs with cortical reflux or aggressive symptoms must be treated as soon as possible. Symptomatic patients with severe bruit or ocular symptoms are also indicated for treatment.
Two cases initially treated by transarterial embolization failed or recurred. All cases could be successfully treated by selective transvenous embolization without any complications. Transvenous embolization is an acceptable treatment for dural AVFs, and has a high rate of cure and low morbidity. Careful assessment of the location of the fistula in addition to the venous drainage is essential to ensure preservation of normal venous drainage. Placement of the coils in an inadequate site may cause worsening venous hypertension and may lead to an unfavorable outcome. Hypoglossal nerve palsy is a potential complication of transvenous embolization due to compression of the nerve by coils placed in the canal.
Seven out of nine cases of hypoglossal canal dural AVF were treated by transvenous approach through the jugular vein and anterior condylar confluence into the anterior condylar veins. It is considered that this is the simplest approach for the anterior condylar vein. However, this approach is difficult in some cases such as hypoplasty, tortuosity or stenosis because of hypertensive vasculopathy of this approach route. In one presented case, we successfully introduced the microcatheter into the anterior condylar vein through the sigmoid sinus, posterior condylar vein, suboccipital cavernous sinus and the lateral condylar vein.
Ernst et Al mentioned that source images of MR angiography were useful for description of the fistulous pouch to be embolized 3.
Knowledge of the venous anatomy of the craniocervical junction and critical evaluation of the location and drainage veins of the dural AVF can contribute to the successful endovascular treatment of dural AVF at cervicocranial junction.
Conclusions
Dural AVFs involving the hypoglossal canal can be successfully treated by selective transvenous embolization with critical evaluation of the venous anatomy of each case.
References
- 1.San Millan Ruiz D, Gailloud P, et al. The craniocervical venous system in relation to cerebral venous drainage. Am J Neuroradiol. 2002;23:1500–1508. [PMC free article] [PubMed] [Google Scholar]
- 2.Takahashi S, Sakuma I, et al. Craniocervical junction venous anatomy around the suboccipital cavernous sinus: evaluation by MR imaging. Eur Radiol. 2005;15:1694–1700. doi: 10.1007/s00330-004-2597-5. [DOI] [PubMed] [Google Scholar]
- 3.Ernest R, Bulas R, et al. Three cases of dural arteriovenous fistula of the anterior condylar vein within the hypoglossal canal. Am J Neuroradiol. 1999;20:2016–2020. [PMC free article] [PubMed] [Google Scholar]
- 4.Kiyosue H, Tanoue S, et al. Ocular symptoms associated with a dural arteriovenous fistula involving the hypoglossal canal: selective transvenous coil embolization. J Neurosurg. 2001;94:630–632. doi: 10.3171/jns.2001.94.4.0630. [DOI] [PubMed] [Google Scholar]
- 5.Komiyama M, Ishiguro T, et al. Intense pulse-synchronous tinnitus caused by dural arteriovenous fistula at the hypoglossal canal. No To Shinkei. 2002;54(9):830–831. [PubMed] [Google Scholar]
- 6.Arai Y, Ishii H, et al. Dural arteriovenous fistula within the hypoglossal canal successfully treated by transvenous embolization. Interventional Neuroradiology. 2004;10:59–62. doi: 10.1177/159101990401000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tanoue S, Goto K, Oota S. Endovascular treatment for dural arteriovenous fistula of the anterior condylar vein with unusual venous drainage: report of two cases. Am J Neuroradiol. 2005;26(8):1955–1959. [PMC free article] [PubMed] [Google Scholar]