Abstract
This paper analyzes the workflow and implementation of electronic health record (EHR) systems across different functions in small physician offices. We characterize the differences in the offices based on the levels of computerization in terms of workflow, sources of time delay, and barriers to using EHR systems to support the entire workflow. The study was based on a combination of questionnaires, interviews, in situ observations, and data collection efforts. This study was not intended to be a full-scale time-and-motion study with precise measurements but was intended to provide an overview of the potential sources of delays while performing office tasks. The study follows an interpretive model of case studies rather than a large-sample statistical survey of practices. To identify time-consuming tasks, workflow maps were created based on the aggregated data from the offices. The results from the study show that specialty physicians are more favorable toward adopting EHR systems than primary care physicians are. The barriers to adoption of EHR systems by primary care physicians can be attributed to the complex workflows that exist in primary care physician offices, leading to nonstandardized workflow structures and practices. Also, primary care physicians would benefit more from EHR systems if the systems could interact with external entities.
Introduction
Healthcare is a continuously evolving industry facing major challenges: increasing costs, unacceptably high error rates, and dissatisfied patients and providers.1 Spending on healthcare in the United States continues to grow at the rate of more than 7 percent per year, expecting to reach $2.8 trillion, around 17 percent of the gross domestic product, by 2011. Information technology (IT) is becoming essential in managing the healthcare enterprise.2 Many hospital systems have adopted electronic health record (EHR) systems, but the rate of adoption has been very slow in the case of individual or small-group offices. A 2007 National Ambulatory Medical Care Survey reports that in more than 161,200 medical practices in the United States, there were 311,200 physicians practicing in office-based environments.3 The report also identifies that 69.2 percent of practices consisted of individual practitioners. According to preliminary estimates from a 2009 mail survey, 43.9 percent of the physicians reported using entire or partial EHR systems (not including systems solely for billing) in their office-based practices. About 20.5 percent reported having systems that met the criteria of a basic system, and 6.3 percent reported having a fully functional system.4 Another study found that less than 2 percent of physicians in solo or two-physician (small) practices reported having a fully functional EHR system.5
Various studies conducted across a variety of healthcare settings have claimed that the introduction of EHR systems can lead to an improvement in quality and can improve operational efficiency and workflow.6 In spite of these claims, the overall adoption rates of EHR systems have been reported to be as low as 17 percent.7 A report on the “adoption gap” claims that less than 11.3 percent of the small physician offices have fully implemented EHR systems.8 Given that 88 percent of all medical offices are small practices, the report also identifies barriers to adoption. One of the main barriers identified is the nature and variety of the workflow in small physician offices, leading to resistance to incorporating EHR systems that offer little flexibility. The report also found that successful adoption requires close attention to office workflow, the way tasks are organized, and the resources used to achieve outcomes, along with appropriate change management, planning, and process reengineering.9 Finally, the report urges a more detailed case study of workflows. In the spirit of the questions raised by this previous study with respect to the use of EHR systems, our article complementarily summarizes case studies of workflows conducted in 13 physician offices (four primary care and nine specialist offices) over a three-month period.
Studies in the area of EHR system use vary from those that estimate huge costs savings to those that disagree with the cost savings estimates and discuss problems with adoption.10, 11, 12 Some studies point to poor current incentive structures and argue for new incentives to physicians so as to overcome the problems associated with inadequate capital, numerous vendors, lack of interoperability, misaligned incentive structures, fears of privacy, and perception of economic benefits related to the adoption of EHR systems.13, 14, 15, 16, 17 While these studies point to the diversity of barriers to adoption, the focus of this paper is to develop a deeper insight into understanding the workflow, the operational mode used in completing a task, the effect of context (primary care vs. specialty offices), and the interactions with external entities that are part of the workflow. Based on our observations, this article identifies the nature of the workflow and the information management problems in individual or small-group practices. In our study, an EHR consisted of a secure, real-time, point-of-care, patient-centric electronic resource for the physicians. These observations are intended to aid in the reengineering of office organizations that will affect the adoption of EHR systems.
The article is organized as follows: In the following section, we elaborate on the study focus and design, including the research questions addressed. The next section describes and provides an analysis of the workflow for a typical primary care office and draws generalizations from this specific case to the rest of the cases. In the subsequent section, we summarize the results in terms of the research questions that were framed in the study focus section. The final section presents some general conclusions.
Study Focus and Design
Several approaches have been used to study work practices and productivity of physicians’ offices. Most of the studies reported in the literature use standard survey methods to generate statistically significant conclusions related to adoption, costs, barriers, and other aspects of the implementation of EHR systems.18, 19, 20, 21, 22, 23 Some other studies are qualitative in nature. In the study presented in this article, we have taken an interpretive case study approach so as to get an in-depth understanding of the workflows, the current role of EHR technology, and the external factors or interactions that affect workflow automation. Interpretive case studies have been used extensively in social science and management literature. Yin has developed a set of guidelines on the role of interpretive case studies in the social sciences.24 Case studies are used not to create a statistically based hypothesis-testing exploration but as a means to answer specific research questions through a combination of methods such as questionnaires, interviews, and observations of the object of study. Generally, the goal of interpretive case studies is to answer an identified set of questions in the context of previous studies conducted by other researchers. Our intent in using the interpretive approach is to additionally provide a deeper understanding of similar research questions.
To set the stage for reporting on the data collected and the methods used in the study, we clarify the definition of workflow used in this paper. We choose the definition of workflow as “defining the interaction patterns among a practice's staff as they fulfill tasks and produce outcomes using available resources.”25 Using this definition, we identify the tasks conducted in the entire physician office from the arrival of the patient to his or her departure. We also identify the tasks that are sources of delay, either due to the nature of the task or due to external events such as additional unanticipated transactions required to complete the task. This approach to studying small physician offices allows us to understand the nature and variety of workflow in different types of offices, the time delays inherent in the processes, and the resources available to complete tasks. We also identify those tasks where automation led or can lead to specific benefits for small practices.
Given the above perspective of our study, the research questions asked are as follows:
What are the variations among specialist and primary care offices in terms of workflow?
What are the sources of delay or the most time-consuming tasks that are part of the workflow?
What are the reasons for the differences in the extent of computerization in specialist and primary care offices?
We address the above research questions by combining questionnaires with in situ observations and interviews. The design of the questionnaire was meant to facilitate elicitation of the workflow in as clear a fashion as possible to account for the interaction patterns of the staff and the physician in the offices. We used the data and observations to create workflow maps for each office that indicated the mode (e.g., paper, telephone, computer) used in achieving the tasks in the workflow. We also identified the tasks that used some form of computerization. In our interviews, we verified the workflow constructed from the questionnaire and probed the causes of delays in the time-consuming tasks through staff interviews.
The workflow diagrams were visualized using Universal Modeling Language (UML) activity diagrams to provide a common scheme for representing them across offices.26 The names of the tasks, if different names were used by the different offices, were normalized to mean the same across all cases. Once all of the data were organized and analyzed, we used the interview notes to elaborate on the answers to specific questions. Subsequently, we placed the results of our study in the context of other studies reported in the literature.
The interviews and observations were conducted in situ to validate the tasks and workflow patterns in the physician offices. This study was done at 13 small-practice physician offices in the Baltimore and New York areas. A number of physician offices were randomly contacted for consent to participate in this study. The final set of physicians’ offices included both primary care providers (four) and specialty providers (nine) who consented to participate in this study. A total of 77 additional person-hours were spent with the staff to interview them, observe their work, and capture the present work practices of these offices. In the offices where we conducted detailed studies, the workflow was generalized, and the time taken for tasks was noted and averaged for about 10 patients. The study is not intended to be a full-scale time-and-motion study with precise measurements but is rather intended to provide an overview of the potential sources of delays and the proportion of time taken by the different activities in the workflow.
The subsequent sections present the background data of the study and the workflow analysis for the physician offices studied. Here, we also try to compare the physician offices studied and note variations among the offices in terms of workflow.
Background Data
For a uniform presentation format, the first step in the study was to identify the tasks performed in the offices and establish a consistent term for each task across the practices. This is essential because the questionnaires were designed to give the respondents maximum freedom in their responses and did not constrain the answers to a particular terminology. The standardized terms for various tasks were then verified during questionnaire analysis to have the same meaning as the ones provided by respondents in all of the offices under study. Table 1 shows the composition of staff people by function and facility in the physicians’ offices. On average, there are two staff people per physician in primary care offices (columns 1 to 4) and about three staff people per physician in specialty care offices (columns 5 to 13), as specialty care offices tend to perform additional services in-house. In some cases, the front desk tasks (such as registration, billing, and information organization) are performed by the same person, and in other cases there are specialized staff people for billing and record keeping. These variations seem to arise from the manner in which a physician's office evolved. Table 2 provides the tasks and task handling modes across different offices. In our study, four offices had implemented EHR systems, three offices had no computerized approach whatsoever, and the other six offices had some form of minimal computer usage (partial implementation). It must be noted, however, that the four offices with an EHR implementation were in their initial stages (less than six months since implementation). As can be seen in Table 2, only one of the family practice or primary care physicians had some form of computerization. In offices that provide specialty services, the range of computerization of tasks varied. Some offices were in the process of implementation by computerizing a partial set of tasks. In general, the use of paper and telephone was pervasive across the offices when dealing with external entities such as insurance companies, referrals to other doctors, and laboratories. (See Table 1 and Table 2.)
Table 1.
Physician Office Composition and Facilities
| Role or Facility | Primary Care 1 | Primary Care 2 | Faily Practice 1 | Family Practice 2 | Neurology | Multispecialty | Obstetrics/Gynecology | Gastroenterol | Cardiology | Hematology/Oncol | Ophthaimol | Nephrol | ENT | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physicians | 2 | 1 | 2 | 1 | 2 | 10 | 1 | 1 | 2 | 2 | 1 | 6 | 1 | ||
| FrontdeskStaff | 2 | 2 | 2 | 2 | 2 | 2 | 1+1 | 2 | 3 | 2 | 2 | 3 | 2 | ||
| Nurse s | 1 | 1 | 1 | 1 | 1 | 10 | 1 | 1 | 1 | 3 | 1 | 2 | 1 | ||
| Billing managers | 0 | 0 | 1 | 0 | 0 | 2 | 1billing/office manager | 0 | 2 | 0 | 0 | 3 | 1 | ||
| Other | 0 | 0 | 0 | 0 | 1office manager | 2record keepers | 0 | 1 | 1physicaltherapist | 0 | 0 | 1 | 1audiologist | ||
| Lab/other facilities | 0 | 0 | 0 | 0 | EM G/EEGfacility | Sample collection, x-ray, & pharmacy | Samplecollection&simpletests | Endoscopy/colonoscopy | ECO/physicaltherapy/stress test | Samplecollection & chemotherapy | Vision testing | 0 | Audiometry/ultrasound/minimalprocedures |
Table 2.
Small-Office Tasks and Mode of Work
| Tasks | Primary Care 1 | Primary Care 2 | Faily Practice 1 | Family Practice 2 | Neurology | Multispecialty | Obstetrics/Gynecology | Gastroenterol | Cardiology | Hematology/Oncol | Ophthaimol | Nephrol | ENT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Registration | 1 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Insurance verification | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1/0 | 1/0 | 0 | 0 |
| Vitals | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 |
| History | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 3/2 |
| Consultation | 1 | 1 | 1 | 1 | 1/3 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 2 |
| Prescription | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Procedure | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 1 | 2 | 2 | 2 |
| Referral | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 | 0/1 |
| Certificates | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 2 | 2 | 2 |
| Appointments | 1 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Labs | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Billing | 4/1 | 4/2 | 1 | 1 | 4/3/2 | 2 | 2 | 4/1 | 2 | 2 | 2 | 2 | 3/2 |
Key: 0: telephone; 1: paperwork; 2: computer support; 3: transcription; 4: external billing.
Workflow Analysis
In this section we describe the work pattern observed in a primary care office and discuss observations across other specialty offices. We present the workflow using UML activity diagrams. This specific case serves as an exemplar of the type of workflow that exists. It must be noted that some of the offices have not yet implemented EHRs at all, some have implemented EHRs only to carry out certain tasks, and some have completely implemented EHRs efficiently. Also, while the offices have certain characteristics in common, they have slightly different organizational structures based on the combination of services offered within the office and externally, leading to variations in the workflow, especially when contrasting primary care physician and specialist offices. This observation is not meant to imply that there are no differences among the offices within each category, but rather that the differences across the categories are much more significant. We have chosen only certain offices for discussion in this section based on the complexity of their workflow. These offices’ workflows serve to explain the common workflow in the other offices of the same category. The analysis of the workflows in the physician offices are subjective and are based on the observations made. After presenting the individual cases, we explore the differences. In addition, we also discuss the variances observed in the workflows among offices at different locations, implying that the offices adapt to the available resources and the practices of the external services. In the subsequent sections, we present the case studies in detail with respect to the tasks performed and the sources of delay.
Work Practices and Workflow in a Primary Care Provider Office
The workflow in the primary care offices is generally difficult to capture in its entirety with respect to the time taken for each specific task related to each patient. This particular office (Primary Care 1 in Table 2) embodies one end of the spectrum, where there is no computerized support for any task. The office has two primary care physicians with different weekly visiting schedules and is staffed with two full-time front desk clerks and one nurse. There is no computer facility in the office, and hence everything is done manually. The nurse also manages the front desk activities when needed. The staff works amid heaps of forms, files, and paper. There appears to be a significant chance for important reports to get lost among the paperwork (this happened once during the observation study: a lab report that had previously been received was missing; hence, the clerk had to collect the report from the laboratory again and spent considerable time on the telephone).
Description of Tasks
The descriptions of the tasks listed below are based on the roles played by participants. Variation among primary care offices with respect to these roles was minimal or nonexistent.
The tasks of the front desk clerk involve scheduling appointments, registering new patients, registering repeat patients, verifying insurance, dealing with referrals, organizing and collating received reports and information, performing prescription-related activities, organizing the charts, mailing letters, copying, faxing, attending to telephone calls, and issuing certificates.
The tasks of the nurse are to document brief illness histories, record vital signs, collect copayments, and perform some other front desk activities.
The physician is involved with performing routine histories and examinations, entering progress notes, entering codes and other billing information, communicating with fellow consultants and hospitals, and reviewing faxes and issuing follow-up actions.
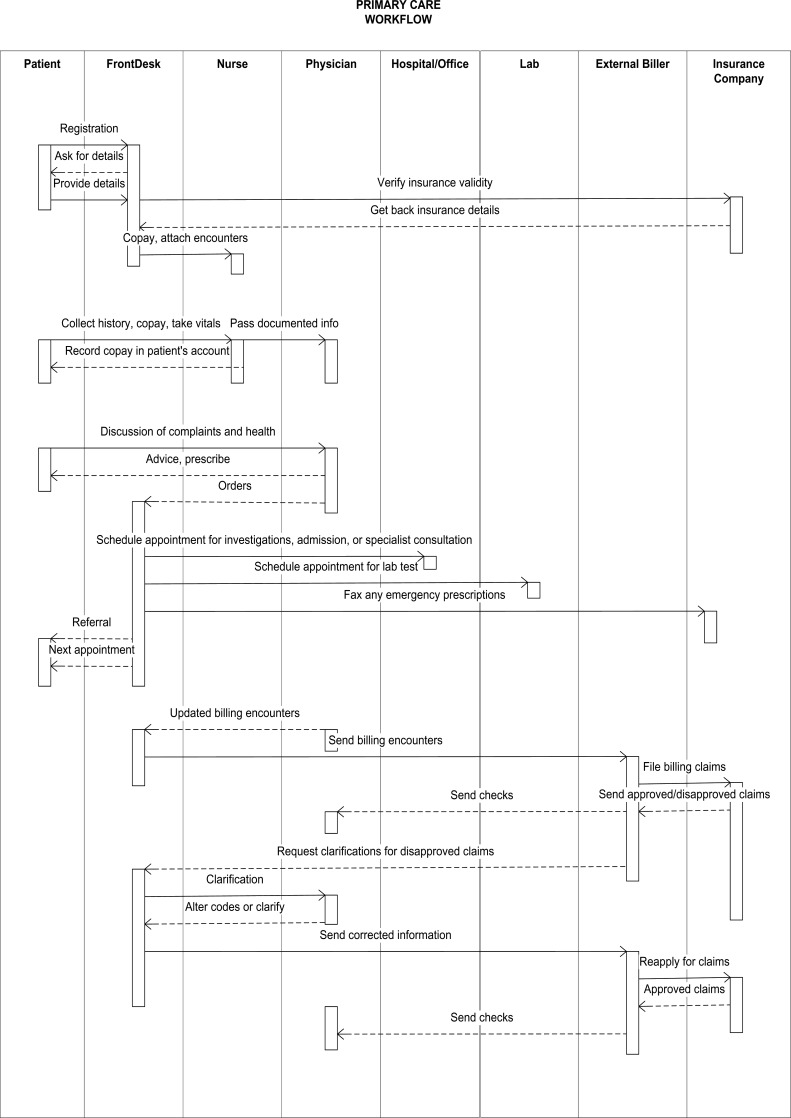
Figure 1 depicts the workflow diagram of this physician's office using a UML activity diagram. One important caveat is that some of the tasks, such as the collection/collation of records are arranged in a non-contiguous way across patients, thus making precise measurements of time taken for each task and for each individual patient difficult. Data on the time taken for each task were not collected because some of the tasks were performed at the same time. For example, while waiting for the insurance company to answer a telephone call, the front desk clerk may process another application. This type of multitasking takes place throughout the day, especially with the organization and clearing of documents for distribution within and outside the office.
Figure 1.
UML-based Activity Diagram for Primary Care Office
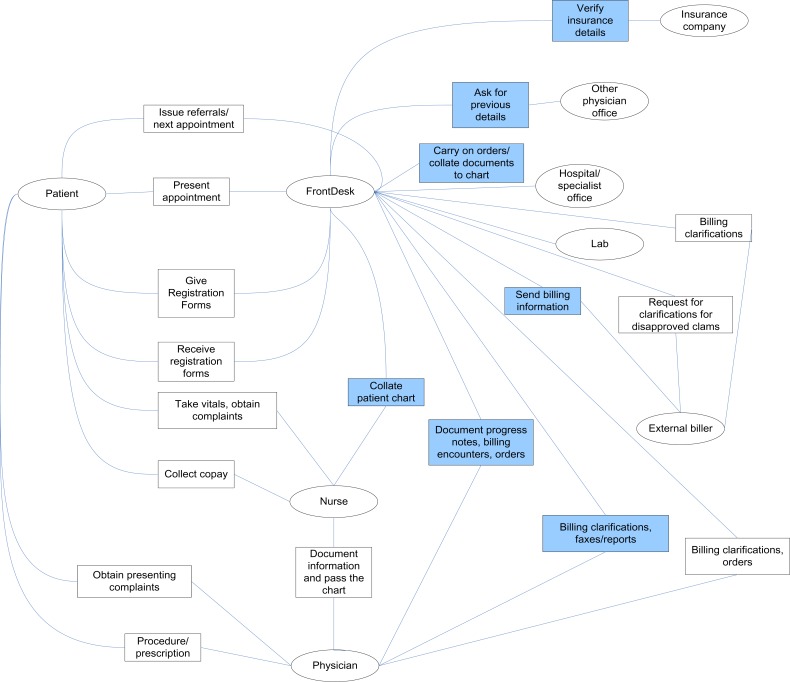
A second view of the workflow is shown in Figure 2. The diagram in Figure 2 illustrates the interaction and information flow, identifying the time-consuming tasks and some of the external and internal interactions.
Figure 2.
Interaction Diagram Showing the Primary Sources of Delay in a Primary Care Office
Sources of Delay in the Workflow by Task
The following are the primary sources of delay in the workflow of the office studied:
1. Scheduling. The office maintains two paper-based planners, one for each physician. There is the potential to enter the appointment in the wrong physician's planner due to oversight. The use of paper-based planners, the use of specific physician-based entries, and the searching for and rescheduling of appointments lead to a time-consuming scheduling process. For example, if a patient forgets the appointment date, the clerk has to meticulously search through the planner to find the patient's appointment.
2. New patient/repeat patient registration. In this step, the physician is limited by the information he or she receives from the patient and its validity until he or she receives the entire record, leading to possible incorrect diagnoses and quality-of-service problems. Furthermore, the process of collecting information from previous physicians who have examined the patient is time consuming, often requiring follow-up telephone calls.
For a repeat patient, making copies of a prior chart for update maintains the continuity in the patient's record; however, this wastes both time and paper. Maintaining multiple copies of the record over time could lead to misfiling or loss of documents.
For the registration task, the primary problem is again organization and management of information. All the information delivered to the doctors is delivered on paper and hence has to be organized and collated; new information from the patient has to be gathered for registration. The front desk clerk spends a lot of time organizing information on paper, leading to a propensity for errors and incomplete information. During our observation, we observed an instance where the demographic details were not updated; thus, a letter sent to the patient was not received and the prescribed test was not performed.
3. Insurance verification. The existence of multiple insurance companies and the variability in coverage and participation of the physicians in a particular insurance company program increase the complexity of insurance verification. The front desk clerk has to maintain and search multiple insurance lists that may or may not be up to date at the time of registration. This leads to a very time-consuming and error-prone process.
The physician spends additional time obtaining approval for tests and engaging in further consultations with doctors working for the insurance companies, even after the examination of the patient. This interaction with insurance companies is a major bottleneck, creating confusion and conflicts in small offices such as this one.
4. Referrals. The referral process is cumbersome, time consuming, and error prone because a number of factors play a role in determining the workflow for a particular case. The clerk not only has to identify the laboratory or physician to be contacted but also must determine whether a given insurance company certifies the laboratory or physician as an authorized supplier of the service.
5. Organization and collation of received reports. Organizing and prioritizing reports and other information is a very time-consuming task requiring attention on the part of the front desk clerk and the physician. While a front desk clerk may be able to organize and prioritize information to some extent, he or she generally does not have the competency to make a judgment on the prioritization of patient appointments. Once the physician has reviewed the information, a number of possible workflow items may need to be generated depending on the information received on a given patient. Delays in reviewing the reports and information could lead to errors and delays in care.
6. Progress notes. In this office, as in many others, the documentation of the physician's interaction with a patient is not immediately entered into the charts. It is normally done after all the consultations for the day or may take two to three days. The delay in documentation of the consultation, despite its being the most salient feature in the chart, could lead to information loss and mistakes.
7. Prescription-related activities. Pharmacists often need clarification from the physician. This task results in considerable interruptions for the physicians.
8. Other unscheduled tasks (mailing, organizing patient charts, copying, faxing, issuing of certificates, and attending to telephone calls). This class of tasks is inherently scheduled in an ad hoc manner. These tasks are done when required or when time permits. Clearly, the tasks of faxing, copying, and issuing certificates require manual work and in a paper-based office require moving, writing, and filling forms and performing tasks that take time. Not all of these tasks can be completely reengineered, especially managing telephone calls.
Observations across Primary Care Offices
We studied three additional primary care or family practice physician offices in a manner similar to that used for the case presented above. We observed heterogeneity among primary care offices as well as in the functioning of individual offices. The following are our observations across these offices:
Each office functions in a unique way. Therefore, the workflow is not uniform even though tasks and some processes match. Further, the workflow is different in different regions, depending on the practices and protocols adopted by the laboratories and insurance companies of that region. In addition, the insurance companies follow different protocols ranging from using telephone calls for the verification of patient information to using a verification machine (similar to a credit card processing terminal) for obtaining approval using the patient's insurance card.
In all of the primary care offices, the workflow pattern is different for different patients depending on their condition. The patient with any physical condition or symptom first comes to the primary care physician. Each patient may have a different treatment protocol. Hence, there are different workflow patterns and different kinds of referrals. The workflow pattern also differs for regular patients, for patients referred from nursing homes, and for patients who come through Medicare. The tasks of registering a patient and referring to a patient a hospital vary due to the differences in the patient's requirements.
In the primary care and family practice offices studied, there was no computerization or a minimal amount of computerization. In some cases, the billing process was outsourced to a billing agent for creating comprehensive reports and providing follow-up monitoring. While this does reduce some paperwork, it still requires manual processing (Table 2).
Our observations confirm the results from previous studies on the low adoption of EHR systems in primary care physician offices.27 In our interviews in various physician facilities, the primary reasons cited for not adopting EHR systems were the lack of IT experience and the uncertainty of the time and costs involved. However, the physicians expressed a belief that they would be able to improve their operations with IT. The general feeling among these offices is that using EHR systems would not result in reduced physician interaction time. The observation is in agreement with the results of time-and-motion studies of physicians in a primary care office, which show that very little decline in the time spent by the physician with a patient occurs with EHR implementation.28 Hence, from a primary care point of view, unless the incentive structure for reimbursements is changed and interfaces to external entities are made seamless, it is unlikely that EHR systems will be widely adopted.
Observations from Specialty Care Offices
Nine specialty care offices were studied. They included specialty practices in neurology, obstetrics/gynecology, gastroenterology, cardiology, hematology/oncology, ophthalmology, nephrology, and ENT (ear, nose, and throat), plus a multispecialty office.
A significant aspect of a specialty care office is that it deals with a specific human system. Hence, the range of workflow is often limited. With a narrow focus on a specialty, in spite of the multiple sources of patient input (primary care physicians, internists, etc.) these offices have more limited external interactions and are less varied in their transactions. All of the specialty care offices we studied had scheduling software with varying degrees of automation of tasks, as shown in Table 2.
Table 2 illustrates the level of computerization in the offices, with the ENT office being the most computerized. Nevertheless, even in the ENT office, tasks involving external interactions, such as those involving insurance verification, prescriptions, external referrals, and laboratory test requests, are still paper based. The only exception is the multispecialty office, which has a computer-based interface with the laboratory because the office is connected to a hospital that provides the laboratory service. In all of the specialty offices, the appointment scheduling and registration tasks were computerized. The other task that was mostly computerized is the billing task, except for the two offices (neurology and gastroenterology) that used external billing services.
A significant difference between the specialty offices and the primary care offices is that most of the specialty offices tend to have diagnostic testing services or other outpatient therapy services in house. For example, the oncology specialty has facilities for outpatient chemotherapy service in house, and the ophthalmology specialist performs ophthalmic procedures on site. In addition, the multispecialty office includes a sample collection center for laboratory samples, as well as x-ray and pharmacy centers. While each specialty office is different, they seem to provide some of these services in house for the convenience of patients as well as for better management of the treatment and diagnosis.
Discussion of the Research Questions
In this section we discuss the research questions under study.
1. What are the variations among specialist and primary care offices in terms of workflow?
The variations among the primary care and specialist offices can be identified along two dimensions. One dimension is the variability in patient population served, and the second is the organizational structure of the offices themselves. In general, primary care physician offices encounter higher patient variety and often do not have many in-house services for sample collection, x-rays, or other services. On the other hand, specialty offices tend to include other services that they see as integral to providing care, for example, sample collection, x-rays, or chemotherapy. The variations in the tasks and task flow in specialty offices tend to be low compared to that found in a primary care office, due to the prescreening by the primary care physician and the more standardized set of transactions. Furthermore, the primary care offices seem to have more external interactions than the specialist offices do.
UML diagrams are insufficient to provide a comparison between primary care and specialty offices because they do not reflect the number of entities of a particular type that the physicians interact with. The interactions that a primary care office participates in are much richer and more varied in contrast to those of specialty offices. Most often, specialty offices are connected to a hospital, where they have access to hospital information systems.
2. What are the sources of delay or the most time-consuming tasks that are part of the workflow?
In Table 2, we present the mode of operation for each task. Clearly all paper-based work requires considerable time to collate and file the various documents. Due to the interleaved nature of many tasks, there is considerable room for error, resulting in possible rework later. The blue boxes in Figure 2 indicate a general overview of the tasks that are the most time consuming. There are multiple reasons for the time-consuming nature of these tasks, but the primary problem is the lack of adequate computer-based interfaces with external entities. Additionally, the external entities may not have a proper information infrastructure themselves, resulting in the need to use telephone calls, faxes, and other manual means of getting information, which consume a great deal of time. This time delay is most evident in the lack of computer-based insurance verification. The other time-consuming tasks include communicating with laboratories and requesting release of prior patient records from other physicians, both requiring telephone calls and unpredictable and time-consuming request-to-receipt cycles.
Further time-consuming interactions include patient scheduling and follow-up of appointments, gathering prior patient histories, handling referrals, and conducting other external interactions that take place through faxes, mail, and sometimes e-mail. Further, these interactions necessitate the use of paper-based systems augmenting the EHR system, even when an EHR system is in use.
One major hurdle for computerization is the lack of understanding of the IT issues involved. Further, most external interactions are not clearly defined, and there is a lack of standard interfaces with external entities. This results in paper-based and manual interactions, which are impediments to computerization. The cost of maintaining information in multiple forms and in multiple repositories leads to additional time-consuming effort in organizing and charting tasks.
3. What are the reasons for the differences in the extent of computerization in specialist and primary care offices?
Most of the previous studies have shown low EHR adoption rates in small offices without much differentiation between primary care and specialty offices. Our case studies show that many of the specialty offices are more advanced with respect to use of computerization than the primary care offices are. The main reason identified is that most of the specialty care offices either have introduced scheduling software or have introduced EHR systems augmented to varying extent by paper-based systems, with the exception of the ENT office, which relies on the EHR system for organization and retrieval of information on patient charts.
The lack of computerization in primary care offices may be attributed to the complexity of the transactions due to the variety in patient populations and the lack of standardized transactions across external agencies (insurance companies, hospitals, and other specialists). Given the complexity of the transactions, most offices often tend to adopt minimal and fragmented computerization for tasks such as billing that are separated from medical records. With an increase in the number of entities with which a physician's office interacts, the problems of interoperability and the level of computerization of interacting entities come into play in estimating the usefulness and effectiveness of the EHR system. It was found in a time-and-motion study that the overall median time saved by a physician was 0.5 minutes, a decrease from 27.55 minutes to 27.05 minutes, with EHR implementation,29 which may be due to inadequate interfaces with external entities.29 Until a tipping point is reached with respect to the economics of a given office, EHR adoption will be slow. This finding is borne out by a study that claims that EHR implementation is generally viewed from a financial dimension and not from a quality-of-care point of view by physicians.30 A cause of the low rate of EHR adoption is clearly the lack of network effects, which reinforces the perception and reality of high capital investment and low potential returns in implementing EHR systems.
There are considerable benefits of implementing EHR systems in a physician's office, such as increased overall operational efficiency, reduced medical error rate (which will significantly contribute to national healthcare savings), the ability to generate templates and reminders, decreased staff utilization, less space consumption with the elimination of paper charts, and easier production of “audit trails” for insurance coding. The financial costs and benefits of EHR systems can affect the rate at which healthcare providers adopt them, while quality improvement benefits can affect patients’ health, which may in turn result in financial benefit to payers from avoiding “downstream” expenditures, especially for hospital and emergency room services.31
Discussion and Conclusion
There are several conclusions to be drawn from this study on workflow and EHR systems in small medical practices. First, the physician offices that had implemented EHR systems, mainly specialty offices, were fully satisfied with the process and claimed to have improved their efficiency. However, they felt that an upgrade in appropriate interfaces with external entities would lead to further time saving. For primary care offices, the major sources of work delays came from interactions with external entities, including entities that had previously provided care to the patient, multiple insurance companies, laboratories, hospitals, and outside entities to whom patients were referred. Currently, none of these tasks can be done easily through the computer. Hence, paper-based systems remain the norm for these tasks in primary care settings. A specialty office operates through referrals from primary care physicians. The primary care office clears the patient for initial insurance claims and sends all the relevant records with the referral, hence reducing the task faced by primary care offices of chasing prior records and other information. Thereby, the time-consuming external interactions are reduced in the specialty offices. Mapping and correlation of patient identifiers and standards-based information interchange facilities can enable large healthcare enterprises to provide a virtual patient record that overlies the fragmented records of the patient in the different healthcare facilities.32
From an economic point of view, a primary care physician's cost of computerization is directly related to the ability to exploit network effects while interacting with external entities. The number of external entities that the physician's office has to interact with, and their level of computerization are crucial factors to consider in choosing the appropriate EHR system. The lack of computerization or inadequate interfaces of external participants reduces the economic benefits as the transaction cost for dealing with the external entities outweighs the benefits that could be accrued from computerization within the office. Also, there is fear about the initial delay and potential loss of patients in the months after EHR implementation, when the staff needs to be trained on the new system. Further, the old information has to be entered into the new system, and concerns about the security of the information need to be addressed. Hence, physicians need to be prepared for the extra financial burden associated with EHR implementation.33
The Nationwide Health Information Network (NHIN) program currently being designed and tested by Department of Health and Human Services is an important activity that could increase adoption of EHRs. The goal of the program is to aid the use and development of standards to enable the interoperability of the healthcare system. Without a network infrastructure available to link different healthcare entities, EHR adoption rates will remain relatively low in spite of possible advantages of EHR systems for the internal operation of offices. The linkages of the specialty offices in our study to hospitals through laboratory information systems or other computerized systems allowed them to schedule and order laboratory tests and also to receive reports electronically. This encouraged them to use at least a simple EHR system, which also helped them to integrate internal information. On the other hand, primary care offices that have numerous interactions with a variety of entities are not able to rid themselves of paper-based systems, leading to reluctance in adopting EHR systems.
Some strategies that small physician offices can use to implement EHR systems are as follows:
Start small and grow. There are several low-cost EHR systems on the market that can be installed with considerable ease. One of the offices in this study, which was totally paper-based, installed a low-cost EHR system. However, this EHR system was only being used by the front office for scheduling and appointments because the physician was reluctant to spend time entering patient interactions due to time constraints. A possible solution is to use a voice recognition system specifically developed for the medical field. Once the physician is comfortable with using the EHR system, then appropriate linkages can be made to external entities, such as through the use of billing software, a requisite for small practices, where billing is generally outsourced.
Seek help from Regional Extension Centers (RECs). Physicians can seek the help of RECs for implementation of EHR systems in their offices.
Participate in government-funded programs. Considerable emphasis is being placed by the federal government on using health information technology. For example, the Center for Medicare and Medicaid Services (CMS) has announced a demonstration initiative in which selected physician offices will be provided with monetary incentives for implementing EHR systems and confirming to quality metrics established by CMS. The results of this five-year demonstration will provide useful data on EHR adoption.
Disclaimer
Certain commercial software systems are identified in this paper. Such identification does not imply recommendation or endorsement by the National Institute of Standards and Technology (NIST); nor does it imply that the products identified are necessarily the best available for the purpose. Further, any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of NIST or any other supporting US government or corporate organizations.
Contributor Information
Mala Ramaiah, the National Institute of Standards and Technology in Gaithersburg, MD..
Eswaran Subrahmanian, the Collegiate Science and Technology Entry Program in Bangalore, India.
Ram D Sriram, the National Institute of Standards and Technology in Gaithersburg, MD..
Bettijoyce B Lide, the National Institute of Standards and Technology in Gaithersburg, MD..
Notes
- 1.Bock, C., L. Carnahan, S. Fenves, M. Gruninger, V. Kashyap, B. Lide, J. Nell, R. Raman, and R. D. Sriram. Healthcare Strategic Focus Area: Clinical Informatics (NISTIR 7263). Gaithersburg, MD: National Institute for Standards and Technology, September 2005.
- 2.Hillestad R, Bigelow J, Bower A, Girosi F, Meili R, Scoville R, Taylor R. “Can Electronic Medical Record Systems Transform Health Care? Potential Health Benefits, Savings, and Costs”. Health Affairs. 2005;24(no. 5):1103–17. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 3.Hing, E., and C. W. Burt. “Office-based Medical Practices: Methods and Estimates from the National Ambulatory Medical Care Survey.” Advance Data from Vital and Health Statistics, no. 383. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, March 2007. [PubMed]
- 4.Hsiao, C., P. C. Beatty, E. S. Hing, D. A. Woodwell, E. A. Rechtsteiner, and J. E. Sisk. “Electronic Medical Record/Electronic Health Record Use by Office-based Physicians: United States, 2008 and preliminary 2009.” Health e-Stats, December 2009.
- 5.Rao S.R, DesRoches C. M, Donelan K, Campbell E. G, Miralles P. D, Jha A. K. “Electronic Health Records in Small Physician Practices: Availability, Use, and Perceived Benefits”. Journal of the American Medical Informatics Association. 2011;18:271–75. doi: 10.1136/amiajnl-2010-000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao S.R, Des C. M, Roches K, Donelan E. G, Campbell P. D. Miralles, Jha A. K. “Electronic Health Records in Small Physician Practices: Availability, Use, and Perceived Benefits”. Journal of the American Medical Informatics Association. 2011;18:271–75. doi: 10.1136/amiajnl-2010-000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burt C.W, Sisk J. E. “Which Physicians and Practices Are Using Electronic Medical Records?”. Health Affairs. 2005;24(no. 5):1334–43. doi: 10.1377/hlthaff.24.5.1334. [DOI] [PubMed] [Google Scholar]
- 8.Burt C.W, Sisk J. E. “Which Physicians and Practices Are Using Electronic Medical Records?”. Health Affairs. 2005;24(no. 5):1334–43. doi: 10.1377/hlthaff.24.5.1334. [DOI] [PubMed] [Google Scholar]
- 9.Lee J.N, Cain C, Young S, Chockley N, Burstin H. “The Adoption Gap: Health Information Technology in Small Physician Practices”. Health Affairs. 2005;24(no. 5):1364–66. doi: 10.1377/hlthaff.24.5.1364. [DOI] [PubMed] [Google Scholar]
- 10.Lee J.N, Cain C, Young S, Chockley N, Burstin H. “The Adoption Gap: Health Information Technology in Small Physician Practices”. Health Affairs. 2005;24(no. 5):1364–66. doi: 10.1377/hlthaff.24.5.1364. [DOI] [PubMed] [Google Scholar]
- 11.Himmelstein D.U, Woolhandler S. “Hope and Hype: Predicting the Impact of Electronic Medical Records”. Health Affairs. 2005;24(no. 5):1121–23. doi: 10.1377/hlthaff.24.5.1121. [DOI] [PubMed] [Google Scholar]
- 12.Wang S.J, et al. “A Cost-Benefit Analysis of Electronic Medical Records in Primary Care”. American Journal of Medicine. 2003;114(no. 5):397–403. doi: 10.1016/s0002-9343(03)00057-3. [DOI] [PubMed] [Google Scholar]
- 13.Bates D.W. “Physicians and Ambulatory Electronic Health Records”. Health Affairs. 2005;24(no. 5):1180–89. doi: 10.1377/hlthaff.24.5.1180. [DOI] [PubMed] [Google Scholar]
- 14.Loomis G.A, Ries S, Saywell R. M, Jr., Thakker N. R. “If Electronic Medical Records Are So Great, Why Aren't Family Physicians Using Them?”. Journal of Family Practice. 2002;51(no. 7):636–41. [PubMed] [Google Scholar]
- 15.Morrissey, J. “A Day in the Life of a Medical Record.” National Alliance for Health Information Technology. 2006. http://www.healthsharemontana.org/A_Day_in_the_Life.pdf (accessed March 15, 2012).
- 16.Sidorov J. “It Ain't Necessarily So: The Electronic Health Record and the Unlikely Prospect of Reducing Health Care Costs”. Health Affairs. 2006;25(no. 4):1079–85. doi: 10.1377/hlthaff.25.4.1079. [DOI] [PubMed] [Google Scholar]
- 17.Miller R, Sim I. “Physicians’ Use of Electronic Records: Barriers and Solutions”. Health Affairs. 2004;23(no. 2):116–26. doi: 10.1377/hlthaff.23.2.116. [DOI] [PubMed] [Google Scholar]
- 18.Miller R, Sim I. “Physicians’ Use of Electronic Records: Barriers and Solutions”. Health Affairs. 2004;23(no. 2):116–26. doi: 10.1377/hlthaff.23.2.116. [DOI] [PubMed] [Google Scholar]
- 19.Miller R.H, West C, Brown T. M, Sim I, Ganchoff C. “The Value of Electronic Health Records in Solo or Small Group Practices”. Health Affairs. 2005;24(no. 5):1127–37. doi: 10.1377/hlthaff.24.5.1127. [DOI] [PubMed] [Google Scholar]
- 20.Pizziferri L, Kittler A. F, Volk L. A, Honour M. M, Gupta S. R, Wang S, Wang T, Lippincott M, Qi L, Bates D. W. “Primary Care Physician Time Utilization Before and After Implementation of an Electronic Health Record: A Time-Motion Study”. Journal of Biomedical Informatics. 2005;38(no. 3):176–88. doi: 10.1016/j.jbi.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 21.Poon E.G, Jha A. K, Christino M, Honour M, Fernandopulle R, Middleton B, Newhouse J, Leape L, Bates D. W, Blumenthal D, Kaushal R. “Assessing the Level of Healthcare Information Technology Adoption in the United States”. BMC Medical Informatics and Decision Making. 2006;6:1. doi: 10.1186/1472-6947-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Valdes I, Kibbe D. C, Tolleson G, Kunik M. E, Petersen L. A. “Barriers to Proliferation of Electronic Medical Records”. Informatics in Primary Care. 2004;12(no. 1):3–9. doi: 10.14236/jhi.v12i1.102. [DOI] [PubMed] [Google Scholar]
- 23.Simon S.R, Kaushal R, Cleary P. D, Jenter C. A, Volk L. A, Poon E. G, Orav E. J, Lo H. G, Williams D. H, Bates D. W. “Correlates of Electronic Health Record Adoption in Office Practices: A Statewide Survey”. Journal of the American Medical Informatics Association. 2007;14(no. 1):110–17. doi: 10.1197/jamia.M2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yin R.K. Case Study Method: Design and Methods. 3rd ed. Thousand Oaks, CA: Sage; 2003. [Google Scholar]
- 25.Yin R.K. Case Study Method: Design and Methods. 3rd ed. Thousand Oaks, CA: Sage; 2003. [Google Scholar]
- 26.Booch G, Rumbaugh J, Jacobson I. The Unified Modeling Language User Guide. Reading, MA: Addison-Wesley; 1998. [Google Scholar]
- 27.Booch G, Rumbaugh J, Jacobson I. The Unified Modeling Language User Guide. Reading, MA: Addison-Wesley; 1998. [Google Scholar]
- 28.Booch G, Rumbaugh J, Jacobson I. The Unified Modeling Language User Guide. Reading, MA: Addison-Wesley; 1998. [Google Scholar]
- 29.Lo H.G, Newmark L. P, Yoon C, Volk L, Carlson V. L, Kittler A. F, Lippincott M, Wang T, Bates D. W. “Electronic Health Records in Specialty Care: A Time-Motion Study”. Journal of American Medical Informatics Association. 2007;14(no. 5):609–15. doi: 10.1197/jamia.M2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lo H.G, Newmark L. P, Yoon C, Volk L, Carlson V. L, Kittler A. F, Lippincott M, Wang T, Sidorov J. “It Ain't Necessarily So: The Electronic Health Record and the Unlikely Prospect of Reducing Health Care Costs”. Health Affairs. 2006;25(no. 4):1079–85. doi: 10.1377/hlthaff.25.4.1079. [DOI] [PubMed] [Google Scholar]
- 31.Lo H.G, Newmark L. P, Yoon C, Volk L, Carlson V. L, Kittler A. F, Lippincott M, Wang T, Sidorov J. “It Ain't Necessarily So: The Electronic Health Record and the Unlikely Prospect of Reducing Health Care Costs”. Health Affairs. 2006;25(no. 4):1079–85. doi: 10.1377/hlthaff.25.4.1079. [DOI] [PubMed] [Google Scholar]
- 32.Lo H.G, Newmark L. P, Yoon C, Volk L, Carlson V. L, Kittler A. F, Lippincott M, Wang T, Sidorov J. “It Ain't Necessarily So: The Electronic Health Record and the Unlikely Prospect of Reducing Health Care Costs”. Health Affairs. 2006;25(no. 4):1079–85. doi: 10.1377/hlthaff.25.4.1079. [DOI] [PubMed] [Google Scholar]
- 33.Lo H.G, Newmark L. P, Yoon C, Volk L, Carlson V. L, Kittler A. F, Lippincott M, Wang T, Sidorov J. “It Ain't Necessarily So: The Electronic Health Record and the Unlikely Prospect of Reducing Health Care Costs”. Health Affairs. 2006;25(no. 4):1079–85. doi: 10.1377/hlthaff.25.4.1079. [DOI] [PubMed] [Google Scholar]