Abstract
As the use of information technology within the healthcare setting increases, the impact of bridging registry data with electronic health records (EHRs) must be addressed. Current EHR implementation may create benefits as well as challenges to cancer registries in areas such as policies and regulations, data quality, reporting, management, staffing, and training. The purpose of this study was to assess 1) the status of EHR usage in cancer registries, 2) the impact of EHR usage on cancer registries, and 3) the benefits and challenges of EHR usage for cancer registries in Alabama. The study method consisted of a voluntary survey provided to participants at the Alabama Cancer Registry Association 2009 annual conference. Forty-three respondents completed the survey. Data indicated that the major benefits of EHR use for the cancer registry included more complete treatment information available to clinicians and researchers, more time for retrieving and analyzing data for clinicians and researchers, and better tracking of patient follow-up. The major challenges included lack of adequate resources, lack of medical staff support, and changing data standards. The conclusion of the study indicates that understanding the impacts and challenges of EHR usage within cancer registries has implications for public health data management, data reporting, and policy issues.
Key words: electronic health records, cancer registry, information technology
Background
Established in 1992 through the Cancer Registries Amendment Act, the National Program of Cancer Registries (NPCR) administered by the Centers for Disease Control and Prevention (CDC) collects data on a number of variables associated with cancer, such as occurrence, type, extent, location, and initial treatment,1 from state cancer registries. Summary state- and federal-level statistics provided through the NPCR facilitate informed decision making that impacts healthcare policy and regulations as well as education and training of healthcare professionals.2
State cancer registries provide a wide array of functions, including monitoring cancer trends over time; determining cancer patterns in various populations; guiding planning and evaluation of cancer control programs (such as determining whether prevention, screening, and treatment efforts are making a difference); helping set priorities for allocating health resources; advancing clinical, epidemiologic, and health services research; and providing information for a national database of cancer incidence.3 Two types of national programs provide leadership for systematical collection, dissemination, and interpretation of cancer data and serve as a resource for research to address the cancer burden in the United States. The National Hospital-based Cancer Program focuses on cancer data from hospital cancer registries, while the National Population-based Cancer Program focuses on geographically defined cancer registries such as those focusing on regional or state populations.4
Historically, the process for data entry into cancer registries was completed by a certified cancer registrar using a manual or electronic process for documentation into paper or electronic forms. The path for data abstracting within a cancer registry begins with the initial patient evaluation and diagnosis followed by entry into a hospital registry database. A hospital-based cancer registry collects information on all cancer patients who receive services from a healthcare organization.5 Annual follow-up via phone or mail is conducted to update the patient's status. The case is reported to the state cancer registry for research and incidence reporting.6
However, as the use of information technology within the healthcare setting increases,7, 8 the impact of bridging registry data with electronic health records (EHRs) must be addressed. Traditionally, the cancer registry has maintained cancer case records in paper format. Current EHR implementation may create benefits as well as challenges for cancer registries in areas such as policies and regulations, data quality, reporting, management, staffing, and training. The purpose of this study was to assess 1) the status of EHR usage in cancer registries, 2) the impact of EHR usage on cancer registries, and 3) the benefits and challenges of EHR usage for cancer registries in the state of Alabama.
Methods
Survey Sample and Procedure
A convenience sample was drawn from participants of the Alabama Cancer Registry Association's 2009 annual conference held in Birmingham, Alabama. The annual conference is open to all cancer registrars and other cancer-related and health information management professionals from the state.9 A self-completed survey was distributed during the two-day conference. Sixty cancer registrars attended this conference. All conference attendees were eligible to participate in the survey. The survey was included in each participant's program package along with an informed-consent document and written instructions regarding the study purpose and procedures. In addition, a five-minute introduction and explanation of the study and survey procedures was given by the study investigator each day prior to the start of the conference sessions. Institutional review board approval was obtained prior to conducting the survey. Study participants were instructed to complete their surveys during the conference and return them to a sealed drop box located at the conference registration desk. The survey was anonymous, and no self-identifying information was collected or disclosed.
Survey Development and Measures
A survey was designed based upon a literature review pertaining to cancer registries and the implementation of EHRs10 as well as interviews with local cancer registrars. The survey questions focused on individual perceptions of the impact of the EHR use in cancer registries. Using a five-point Likert scale (1 = strongly disagree, 5 = strongly agree), participants were asked to rate their perceptions of impacts (10 items), benefits (9 items), and challenges (9 items) of using EHRs in a cancer registry (see Table 1). Demographic information such as job title, credentials, type of work setting, and healthcare facility location were also collected. (See Table 2.)
Table 1.
Mean and Standard Deviation of Impacts, Benefits, and Challenges to Cancer Registry with Electronic Health Record (EHR) Usage (N = 43)
| A. Impacts | Mean(Standard Deviation) |
|---|---|
| On a scale of 1 to 5 (1= Strongly Disagree and 5 = Strongly Agree), please rate how important the following IMPACTS are in using the EHR in Cancer Registry in healthcare facility. | |
| 1. Fulfill the Need to Share the Patient Record Information among Healthcare Professionals | 4.33 (0.72) |
| 2. Reduce Healthcare Delivery Costs | 3.89 (0.85) |
| 3. Improve Quality in Data Documentation | 4.24 (0.80) |
| 4. Improve Clinical Process or Workflow Efficiency | 4.28 (0.66) |
| 5. Improve Monitoring Cancer Trends Over Time | 4.19 (0.89) |
| 6. Determine Cancer Patterns in Various Populations | 4.14 (0.96) |
| 7. Guide Planning and Evaluation of Cancer Control Programs | 3.73 (0.98) |
| 8. Help Set Priorities for Allocating Health Resources | 3.71 (0.97) |
| 9. Advance Clinical, Epidemiologic, and Health Services Research | 3.82 (0.94) |
| 10. Provide Information for a National Database of Cancer Incidence | 3.97 (1.00) |
| 11. Other (please specify) | NA |
| B. Benefits | |
| On a scale of 1 to 5 (1= Strongly Disagree, and 5 = Strongly Agree), please rate how important the following BENEFITS are in using the EHR in Cancer Registry in healthcare facility. | |
| 1. Improves Quality of Report Data to Internal and External Users | 4.11 (0.83) |
| 2. Improve Workflow | 4.11 (0.79) |
| 3. Allow the Registrar More Time for Retrieving and Analyzing Data for Clinicians and Researchers | 4.22 (0.80) |
| 4. Decrease the Time Needed for Case Finding and Entering Data | 4.17 (0.85) |
| 5. Provide More Complete Treatment Information to Clinicians and Researchers | 4.26 (0.78) |
| 6. Allow Physician to Retrieve Consolidated Cancer Information Electronically from Cancer Registry | 3.92 (0.94) |
| 7. Resolve Intra-Community Standardization Issues | 3.86 (0.87) |
| 8. Helps to Improve the Completeness, Accuracy, and Timeliness of the Registry | 4.22 (0.90) |
| 9. Helps to Track Patients for Better Follow-Up | 4.28 (0.74) |
| 10. Other (please specify) | NA |
| C. Challenges | |
| On a scale of 1 to 5 (1= Strongly Disagree, and 5 = Strongly Agree), please rate how important the following CHALLENGES are in using the EHR in Cancer Registry in healthcare facility. | |
| 1. Lack of Adequate Funding or Resources | 3.73 (1.07) |
| 2. Lack of Medical Staff Support | 3.70 (1.10) |
| 3. Inadequate or Incomplete Healthcare Information Standards or Code Sets across Registries | 3.36 (1.17) |
| 4. Lack of Full-Time Commitment to Improvements | 3.55 (1.20) |
| 5. Lack of Unique Patient ID Makes National Surveillance Data Impossible | 3.33 (1.19) |
| 6. Becomes More Challenging to Achieve with Changing Data Standards | 3.67 (0.96) |
| 7. Unknown Availability, Accessibility, Reliability and Validity of EHR Data | 3.33 (0.99) |
| 8. Lack of Employee Training and Knowledge | 3.48 (1.12) |
| 9. Lack of Standardized Data Exchange for Non-Cancer Registry Data Sources | 3.55 (1.09) |
| 10. Other (please specify) | NA |
Note: Response totals do not always equal 43 due to missing values.
Table 2.
Characteristics of Survey Respondents (N = 43)
| Variable | n | % |
|---|---|---|
| Position | ||
| HIM director/administrator/manager | 8 | 19 |
| Cancer registrar/abstractor/analyst/coordinator | 28 | 65 |
| Other | 7 | 16 |
| Work setting | ||
| Acute care hospital | 27 | 63 |
| Cancer center/clinic | 4 | 9 |
| State cancer registry | 6 | 14 |
| Educational institution | 4 | 9 |
| Other | 2 | 5 |
| Hospital bed size | ||
| <300 beds | 5 | 12 |
| 300–499 beds | 14 | 33 |
| ≥500 beds | 9 | 21 |
| Does not apply | 15 | 35 |
Note: Percentage totals may not equal 100 due to rounding.
The survey was designed to query the respondents’ implementation of EHRs within their healthcare facilities. We first asked: “Has your healthcare facility implemented electronic health record (EHR) in the Cancer Registry?” Five possible answers were listed: 1) “Yes, EHR has already been implemented, and is accessed in cancer registry”; 2) “Yes, EHR has already been implemented, but is not accessed by cancer registry”; 3) “No, EHR has not already been implemented, but it is in progress”; 4) “No, EHR has not already been implemented, but it is being considered”; 5) “No, EHR has not already been implemented, and there are no plans to implement EHR.” Respondents who marked “yes” for the first question were asked for additional details. For example, respondents were asked the length of time that EHRs had been implemented in their facility. In addition, these respondents were asked to describe the basic functions of EHR usage for cancer registries within their healthcare facilities. They were instructed to select all listed functions that applied to their usage of complete or partial EHRs within their cancer registry. Listed functions included review of patient clinical data and results, care plans, physician and other care provider's clinical documentation, care coordination documentation, and regulatory reports. Table 3 provides the list of surveyed functions for EHR usage within a cancer registry.
Table 3.
Functions of Electronic Health Record Usage in Cancer Registry (N = 43)
| Function | Percentage of Usage |
|---|---|
| Physician and clinical documentation | 56% |
| Patient clinical data and results review | 54% |
| Care plans | 28% |
| Care coordination | 28% |
| Clinical and outcomes measurement | 28% |
| Quality reporting | 23% |
| Patient education | 23% |
| Clinical decision support | 21% |
| Medication reconciliation | 18% |
| Regulatory reporting | 18% |
Analysis
Excel and SPSS version 18 were used for data entry and data analyses. Descriptive analyses were applied for the demographic information and Likert-scale data summaries. By design, the unit analysis was based on individual respondents instead of on health facilities.
Results
Characteristics of Respondents
We distributed 60 surveys, and 43 surveys were completed for a 71 percent response rate. The conference attendees represented 12 counties in Alabama and 25 health facilities (we obtained a count of health facilities from the registration list at the conference). Despite the fact that 55 of the 67 counties in Alabama are designated as “rural,”11 nearly all study participants (97 percent) were from urban facilities, compared to only 3 percent from rural areas. Almost two-thirds (65 percent) of the respondents held the position of cancer registrar, cancer abstractor, or cancer analyst. More than half were from acute care hospitals (63 percent); the remaining respondents were from the state cancer registry, a cancer center, or an educational institution (see Table 2).
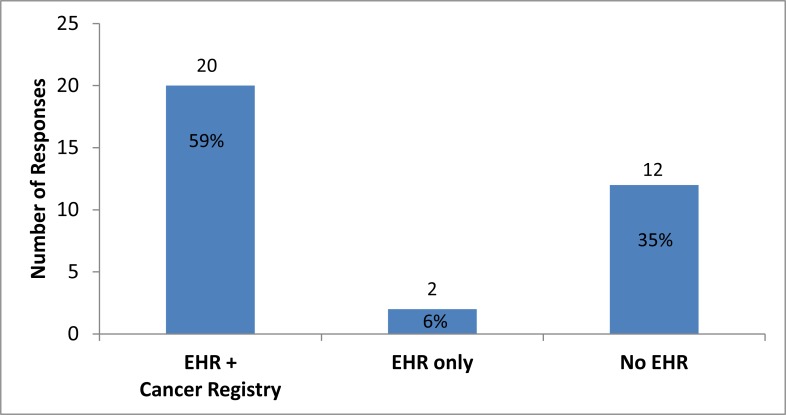
EHR Usage in Cancer Registries
Figure 1 shows the status of EHR implementation in cancer registries within the state of Alabama. Thirty-four respondents were included in this item analysis. Respondents who did not answer or were not working in a cancer registry or other health facility were excluded from this analysis. A total of 20 respondents (59 percent), from seven different counties, reported using EHRs in the cancer registry at their facilities; 2 respondents (6 percent) had implemented EHRs but were not using EHRs in the cancer registry; and the remaining 12 respondents (35 percent) had not completed implementation of EHRs or did not currently have EHRs in their facilities. It should be noted that these data reflect individual participant responses. Due to the lack of identifiers on the survey, data could not be sorted by facility; therefore, multiple respondents could be from the same facility.
Figure 1.
Status of EHR Usage with Cancer Registries
Note: The data in this figure include 34 valid responses. Data were missing or not applicable for 9 of the 43 total respondents.
Table 3 shows respondents’ data pertaining to the wide range of functions for usage of EHRs in cancer registries. More than half of the respondents who are currently using full or partial EHRs reported accessing the EHRs for physician and clinical documentation (56 percent) and patient clinical data and results review (54 percent). Some of the other functions included care plans (28 percent), care coordination (28 percent), clinical and outcomes measurement (28 percent), patient education (23 percent), quality reporting (23 percent), clinical decision support (21 percent), medication reconciliation (18 percent), and regulatory reporting (18 percent). Data indicate that more than 80 percent of these EHR functions are being used by acute care hospitals.
Impact, Benefits, and Challenges of EHRs within Cancer Registries
Table 1 illustrates the mean and standard deviation for each survey item related to impact, benefits, and challenges of EHR usage in cancer registries. On a scale of 1 to 5, the overall mean for each item ranged from 3.71 to 4.33 for impact, 3.86 to 4.28 for benefits, and 3.33 to 3.73 for challenges.
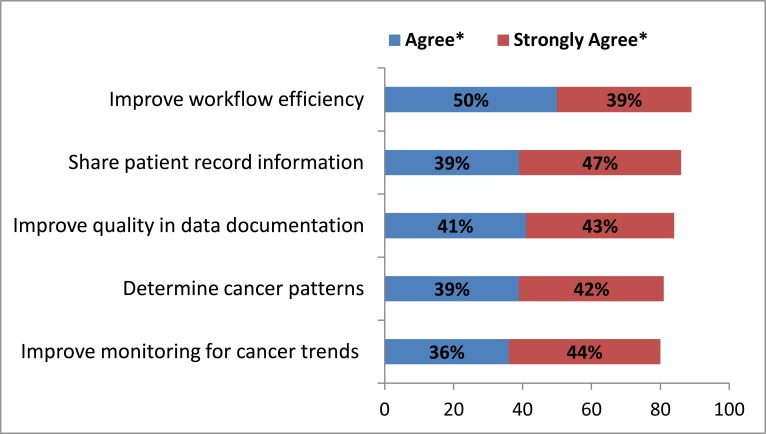
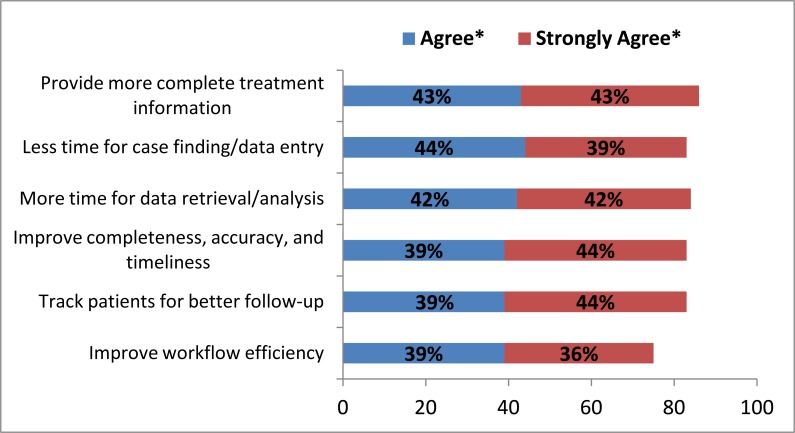
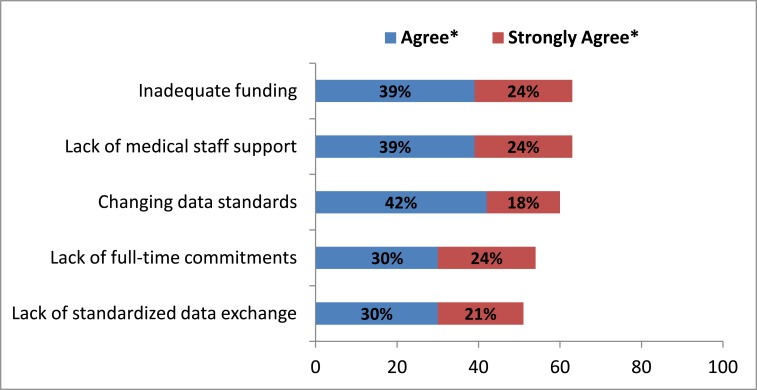
Figure 2 shows respondent data regarding the impact of EHR usage in cancer registries. The highest-ranking responses regarding the impact of EHR usage in a cancer registry were 1) improved workflow efficiency, 2) shared patient record information, 3) improved data quality in data documentation, 4) determination of cancer patterns, and 5) improved monitoring for cancer trends. Figures 3 and 4 identify respondents’ feedback regarding the benefits and challenges of utilizing EHRs in their cancer registry. The top benefits of EHR use in a cancer registry included 1) more complete treatment information, 2) less time for case finding and data entry, 3) more available time for data retrieval and analysis, 4) improved completeness, accuracy, and timeliness, 5) better patient tracking for follow-up, and 6) improved workflow efficiency (see Figure 3). The top challenges to the utilization of EHRs within a cancer registry identified by respondents were 1) lack of adequate funding, 2) lack of medical staff support, 3) changing data standards, 4) lack of full-time commitments, and 5) lack of a standardized data exchange (see Figure 4).
Figure 2.
Impact of EHR Use in Cancer Registry (N = 43)
Note: * The numbers represent percentage of respondents.
Figure 3.
Benefits of EHR Use in Cancer Registry (N = 43)
Note: * The numbers represent percentage of respondents.
Figure 4.
Challenges of EHR Use in Cancer Registry (N = 43)
Note: * The numbers represent percentage of respondents.
Respondents identified the following additional issues related to using EHRs within a cancer registry: 1) data accessibility issues, such as lacking access to a patient's complete health history in physician offices’ medical records and facility treatment records, or lacking access to other health facility records if the patient received care at multiple facilities; 2) documentation and data completeness issues, such as physicians’ documentation and difficulty using existing information with a complete cancer abstract; 3) support and knowledge issues, such as a lack of support from administrators, and lack of clear understanding of the roles and functions of a cancer registry; and 4) the lack of resources, such as lack of funding, lack of sufficient staffing, and limited time to complete tasks.
Discussion
As information technology is increasingly utilized as a bridge between patient clinical records and registry data such as that contained in a cancer registry,12 it is important to understand the impact of this bridging process on the registry field. Survey responses from certified cancer registrars in Alabama address the impact of EHR usage on cancer registries and the benefits and challenges of such usage. Responses from 43 of the potential 60 respondents indicate three primary areas of impact: data sharing, data quality, and workflow. Data showed that respondents believed that EHR usage provided positive benefits such as more time for data retrieval and analysis, more complete patient information for practitioners, and improved tracking of patient follow-up. In addition, the use of EHRs in the cancer registry can also improve the timeliness of information sharing from the point of pathologic diagnosis by sending data electronically to the hospital's cancer registry database and simultaneously reporting the data to the state cancer registry.13 These cited benefits of using EHRs within a cancer registry may also be tied to other public health venues, such as vital records and the national death index, and healthcare claims data.14
Challenges associated with the implementation and utilization of EHRs in the healthcare field are cited throughout the literature.15–16 Data from the voluntary survey of cancer registrars indicated similar challenges in the use of EHRs within a cancer registry, such as lack of resources and lack of clinical staff support (personnel). These comments confirm Fox and Sheridan's assessment that, with the implementation of EHRs, the position of the cancer registrar must evolve to include the role of cancer data manager.17 These authors identified workforce training challenges associated with the transition to EHRs in cancer registries not only for the cancer registrars but also for the physician workforce. New program standards, data collection, and reporting requirements impact the successful transition to and implementation of EHRs within the cancer registry.18
Limitations
Two limitations to this study have been identified: 1) the survey was targeted only to cancer registry professionals at the annual meeting, and therefore a response bias may exist in the data; and 2) survey responses were anonymous, resulting in multiple responses from professionals working at the same facilities.
Conclusion
The utilization of EHRs within cancer registries in Alabama was shown to impact data sharing and data quality as well as workflow processes. The impact of EHRs within the cancer registry on the roles and functions of the cancer registrar are important variables as federal initiatives impact data standards and reporting requirements. Understanding the benefits and challenges underlying these areas of impact within cancer registries has implications for public health data management and data reporting. Data sharing across electronic linkages impacts the timeliness and accuracy of reported data for public health venues. However, the challenges of the lack of resources and clinical support may continue to impact the management of these data for public health uses, such as surveillance and vital statistics. Future research should be conducted to explore potential resources for implementation funding and workforce training to improve EHR utilization within the cancer registry.
Contributor Information
Shannon H Houser, the University of Alabama at Birmingham in Birmingham, AL..
Shannon Colquitt, QuadraMed Corporation in Birmingham, AL..
Kay Clements, the University of Alabama at Birmingham in Birmingham, AL..
Susan Hart-Hester, the University of Mississippi Medical Center in Jackson, MS..
Notes
- 1.Centers for Disease Control and Prevention (CDC). National Program of Cancer Registries (NPCR). Available at http://www.cdc.gov/cancer/npcr (accessed January 18, 2011).
- 2.Centers for Disease Control and Prevention (CDC). National Program of Cancer Registries (NPCR): About the Program. Available at http://www.cdc.gov/cancer/npcr/about.htm (accessed March 14, 2012).
- 3.Centers for Disease Control and Prevention (CDC). National Program of Cancer Registries (NPCR): About the Program. Available at http://www.cdc.gov/cancer/npcr/about.htm (accessed March 14, 2012).
- 4.Centers for Disease Control and Prevention (CDC). National Program of Cancer Registries—Modeling Electronic Reporting Project (NPCR-MERP) Available at http://www.cdc.gov/cancer/npcr/informatics/aerro2/pdf/merp_glossary_1100708.pdf (accessed March 14, 2012).
- 5.Centers for Disease Control and Prevention (CDC). National Program of Cancer Registries—Modeling Electronic Reporting Project (NPCR-MERP) Available at http://www.cdc.gov/cancer/npcr/informatics/aerro2/pdf/merp_glossary_1100708.pdf (accessed March 14, 2012).
- 6.LaTour Kathleen M. “Secondary Records and Healthcare Databases”. In: Shirley Eichenwald Maki., editor. Health Information Management Concepts, Principles, and Practice. 2nd ed. Chicago, IL: AHIMA; 2006. [Google Scholar]
- 7.Jha A, Ferris T, Donelan K, DesRoches C, Shields A, Rosenbaum S, et al. “How Common Are Electronic Health Records in the United States? A Summary of the Evidence”. Health Affairs. 2006;25(no. 6):w496. doi: 10.1377/hlthaff.25.w496. [DOI] [PubMed] [Google Scholar]
- 8.Jha A, DesRoches C, Campbell E, Donelan K, Rao S, Ferris T, et al. “Use of Electronic Health Records in US Hospitals”. New England Journal of Medicine. 2009;360(no. 16):1628. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 9.Alabama Department of Public Health. Alabama State Cancer Registry Available at http://www.adph.org/cancer_registry/ (accessed March 4, 2010).
- 10.Thames, S., W. Scharber, and S. Baral. Interoperability between the EHR and Public Health Disease Surveillance: The Cancer Registry Use Case Centers for Disease Control and Prevention (CDC), Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion. Available at http://www.interoperabilityshowcase.org/himss09/docs/presentations/HIMSS09%20Interop_CDC_NPCR_Presentation.pdf (accessed March 14, 2012).
- 11.Alabama Rural Health Association. “What Is Rural?” Available at http://www.arhaonline.org/what_is_rural.htm (accessed January 14, 2011).
- 12.Fox, L. A., and P. Sheridan. “From Cancer Registrars to Cancer Data Managers: The Dawn of a New Age.” Advance for Health Information Professionals. May 12, 2010. Available at http://health-information.advanceweb.com/Web-Extras/Hands-On-Help/From-Cancer-Registrars-to-Cancer-Data-Managers-The-Dawn-of-a-New-Age.aspx (accessed January 4, 2011).
- 13.Public Health Data Standards Consortium. Building a Roadmap for Health Information Systems Interoperability for Public Health 2008. Available at http://www.docstoc.com/docs/69214957/BUILDING-A-ROADMAP-FOR-HEALTH-INFORMATION-SYSTEMS-INTEROPERABILITY (accessed March 14, 2012).
- 14.Thames, S., W. Scharber, and S. Baral. Interoperability between the EHR and Public Health Disease Surveillance: The Cancer Registry Use Case Centers for Disease Control and Prevention (CDC), Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion. Available at http://www.interoperabilityshowcase.org/himss09/docs/presentations/HIMSS09%20Interop_CDC_NPCR_Presentation.pdf (accessed March 14, 2012).
- 15.Houser S.H, Johnson L. “Perceptions Regarding Electronic Health Record Implementation among Health Information Management Professionals in Alabama: A Statewide Survey and Analysis”. Perspectives in Health Information Management. 2008;5 [PMC free article] [PubMed] [Google Scholar]
- 16.DesRoches C. M, Campbell E. G, Rao S. R, Donelan K, Ferris T. G, Jha A, Kaushal R, Levy D. E, Rosenbaum S, Shields A. E, Blumenthal D. “Electronic Health Records in Ambulatory Care: A National Survey of Physicians”. New England Journal of Medicine. 2008;359(no. 1):50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 17.Fox, L. A., and P. Sheridan. “From Cancer Registrars to Cancer Data Managers: The Dawn of a New Age.”
- 18.Fox, L. A., and P. Sheridan. “From Cancer Registrars to Cancer Data Managers: The Dawn of a New Age.”