Abstract
Long-term care (LTC) is an important sector in the healthcare industry; however, the adoption of electronic health record (EHR) systems in LTC facilities lags behind that in other sectors of healthcare. This study examines the adoption and utilization of EHRs in LTC facilities in Texas and identifies the barriers preventing implementation of EHRs.
A survey instrument was mailed to all Texas LTC facilities between October 2010 and March 2011. The survey found that in Texas, 39.5 percent of LTC facilities have fully or partially implemented EHR systems and 15 percent of LTC facilities have no plans to adopt EHRs yet. There is significant variation in the use of EHR functionalities across the LTC facilities in Texas. In the LTC facilities, the administrative functions of EHRs have been more widely adopted and are more widely utilized than the clinical functions of EHRs. Among the clinical functions adopted, the resident assessment, physician orders, care management plan, and census management are the leading functions used by the LTC facilities in Texas. Lack of capital resources is still the greatest barrier to EHR adoption and implementation. Policy makers, vendors, LTC administrators, educators, and researchers should make more effort to improve EHR adoption in LTC facilities.
Key words: electronic health record, long-term care, health information technology, survey, utilization, technology adoption
Background
The aging of the US population and the projected growth of the oldest age bracket (85 years and older) will have a major effect on the demand for and supply of long-term care (LTC) services and on the resources needed to provide those services.1 Seniors themselves consume more than 50 percent of total healthcare services and dollars in this country.2 LTC providers care for the fastest-growing segment of the population and account for a high proportion of the healthcare dollars spent. The patients in LTC experience frequent transitions, which may create gaps in quality and opportunities for errors.3, 4
An electronic health record (EHR) system has the potential to reduce errors, improve quality of care, and deliver healthcare more efficiently.5, 6 LTC providers can “achieve an increase of 37 percent in administrative productivity” by using EHR systems over time.7 Although health information technology (HIT) applications that positively affect both quality of care and patient safety currently exist, they are not widely used in current LTC settings.8 LTC facilities lag in EHR adoption, compared to the other sectors of healthcare.9 Part of the reason for this is that current HIT agendas and strategies focus more on acute and ambulatory care, and LTC suffers from relative inattention.10 Chaudhry et al. summarized the impact of EHRs on the quality, efficiency, and cost of medical care from 74 journal articles at four benchmark institutes; however, none of the studies included a LTC setting.11 Furthermore, most EHRs are intended primarily for acute care facilities, so LTC facilities face unique challenges in using EHRs, such as different documentation needs for facilitating preventive measures, different starting doses of medications, and special reporting needs. Utilization of EHRs in LTC facilities does not initially save time for clinicians.12 LTC settings are often intensely interdisciplinary and holistic in their approach to their patients and residents. Therefore, the challenges and opportunities for promoting EHR adoption and utilization in LTC facilities are greater than ever.13
Policy makers need reliable and valid data on EHR adoption rates in LTC facilities to assess movement toward the goal of promoting EHR adoption.14 If national cross-sectional data were available, we could have a “big picture” of national EHR adoption and utilization status in LTC facilities. If time-series data in a state were available, we could analyze the trend of EHR adoption and utilization status in LTC facilities in that state. However, information on EHR adoption in LTC facilities is relatively scarce.15 In January 2010, the US Department of Health and Human Services (HHS) developed two survey instruments on EHR adoption and use in nursing homes. Unfortunately, no further report was published. Consequently, no national cross-sectional data are available. Several regional surveys, including a 2008 report from Minnesota and a 2007 report from California, are the only EHR adoption and utilization data sources related to LTCs.16, 17 No regional survey has been conducted more than one time to provide time-series data. On the positive side, each of the state surveys contributed a piece of puzzle to the “big picture” of national EHR adoption and utilization status, and set a baseline for these states. Because EHR adoption and utilization has been proposed for decades, no state has the first-mover advantage in EHR adoption. Therefore, we have reasons to assume that EHR adoption status would be homogeneous across the United States, unless a state has special policies impacting EHR adoption.
The purpose of this study is to assess EHR adoption and utilization status in LTC facilities in Texas, identify the barriers to EHR adoption, and help policy makers assess movement toward the goal of promoting EHR adoption. The findings of the study can set a baseline for Texas EHR adoption and utilization in LTC facilities and contribute to the “big picture” of national EHR adoption and utilization status. By comparing the statewide surveys, the authors attempt to identify the similarities, rather than the discrepancies, in EHR adoption in different states and at different times.
Methods
The sources for the literature review came from the university library databases and Internet searches, including specific website searches, electronically published periodicals, government reports, and other relevant organizational information. Searches were made for peer-reviewed and non-peer-reviewed publications within the past 10 years, using various keywords and keyword combinations, such as EHR, HIT, nursing homes, and LTC. Titles and abstracts were reviewed first, and relevant articles were read, including mining of each paper's reference list for any additional relevant work. Significantly more literature was reviewed regarding HIT in general and, more specifically, HIT within hospital and ambulatory settings. Internet searches were conducted using keywords and key organizations to narrow the requested information track. Federal websites were also searched and regularly researched to keep abreast of current proceedings.
Previous literature revealed that HIT applications in LTC facilities had many similar functions as those in hospitals, such as billing, drug ordering, and inventory management.18 The administrative functions were more widely adopted and utilized than the clinical functions.19 Both regional surveys and scholars identified that lack of capital resources was the leading barrier to EHR adoption.20, 21, 22, 23 Other significant barriers included insufficient time, lack of technical infrastructure, lack of technical support staff, inability to easily input historical data, and lack of technical knowledge.24, 25, 26, 27, 28
Based on the literature review, a questionnaire was developed. Besides the questions in the HHS 2010 survey, including the minimum data set (MDS), the clinical functions, and the barriers to HIT adoption and use, the questionnaire also collected information about LTC facility characteristics, EHR implementation status, the administrative functions, and LTC administrators’ perspectives on EHR adoption and utilization. A pilot survey instrument was mailed in October 2010 to nearby LTC facilities to assess the validity and reliability of the questionnaire. Per the responses from the pilot survey, a few survey questions were edited. In January 2011, a final survey instrument was mailed to a total of 1,177 LTC facilities in Texas, whose addresses were generated from the database on the official Medicare Web site (http://www.medicare.gov/NHCompare). Because of invalid mailing addresses, 264 survey questionnaires were returned to the authors. Therefore, the valid population size in this survey is 913. By the end of March 2011, completed surveys were received from 137 LTC facilities for a 15 percent response rate.
Results and Observations
Demographic Characteristics
Table 1 displays the demographic characteristics of survey respondents, including facility ownership status, location, affiliation types, and number of beds.
Table 1.
Demographic Characteristics of Survey Respondents
| Characteristics | Survey Respondents | All Texas LTCsc | Comparison | |||
|---|---|---|---|---|---|---|
| % | n | % | n | Z | p-value | |
| Ownership status | ||||||
| For-profit | 73.0% | 100 | 85.3% | 1,004 | –3.72 | .00 |
| Not-for-profit | 20.4% | 28 | 12.0% | 141 | 2.79 | .99 |
| Local government | 5.8% | 8 | 2.3% | 27 | 2.43 | .99 |
| State government | 0.7% | 1 | 0.4% | 5 | 0.50 | .69 |
| Veterans affairs | 0.0% | 0 | 0.0% | 0 | ||
| Location | ||||||
| Rural | 54.7% | 75 | 59.8% | 704 | –1.14 | .13 |
| Suburbana | 16.1% | 22 | ||||
| Urban | 24.8% | 34 | 40.2% | 473 | 1.14 | .87 |
| Metropolitan statistical area | ||||||
| (MSA)b | 4.4% | 6 | ||||
| Affiliation type | ||||||
| Hospital based | 6.6% | 9 | n/a | n/a | ||
| Part of a regional multicenter chain | 48.2% | 66 | n/a | n/a | ||
| Part of a national multicenter chain | 11.7% | 16 | n/a | n/a | ||
| Freestanding | 33.6% | 46 | n/a | n/a | ||
| Number of beds | ||||||
| 0–49 | 5.8% | 8 | 6.8% | 80 | −0.42 | .34 |
| 50–99 | 35.8% | 49 | 31.9% | 375 | 0.92 | .82 |
| 100–149 | 41.6% | 57 | 47.7% | 562 | –1.36 | .09 |
| 150 or more | 16.8% | 23 | 13.6% | 160 | 1.02 | .85 |
aA suburban area refers either to an outlying residential area of a city or town or to a separate municipality, borough, or unincorporated area outside a town or city. Source: David Rusk. Cities without Suburbs. 3rd ed. Washington, DC: Woodrow Wilson Center Press, 2003.
bA metropolitan statistical area (MSA) is a single urbanized area with a population of at least 2.5 million. An urbanized area is defined as a central city and any densely populated area adjacent to that central city. An urbanized area is required to have more than 50,000 inhabitants and be closely settled. Source: Office of Management and Budget. Federal Register 75, no. 123, June 28, 2010. Available at http://www.whitehouse.gov/sites/default/files/omb/assets/fedreg_2010/06282010_metro_standards-Complete.pdf (accessed October 8, 2011).
cInformation about ownership status and number of beds of all Texas LTCs was retrieved from http://www.medicare.gov. Information about location was retrieved from, Rural Assistance Center web site at http://ims2.missouri.edu/rac/amirural/ where only “rural” and “urban” information is available. In the proportion comparison, “urban” in the sample includes suburban, urban, and MSA.
Considering the low response rate, the authors considered whether the survey sample is representative of the population of the LTC facilities in Texas. The authors compared the proportions of demographic characteristics between the survey sample and the entire population of LTCs in Texas (see Table 1). We found that except the for-profit proportion, all other proportions of the respondent characteristics are not significantly different from those of the entire population of LTCs in the state. Therefore, the survey sample is representative of the population of LTC facilities in Texas.
EHR Implementation
EHR implementation status by demographic characteristics is outlined in Table 2. Responses showed little difference in the rate of EHR implementation among for-profit (34.0 percent), not-for-profit (42.9 percent), and local government (50.0 percent) facilities, with a p-value of .5. Only one state-government-owned LTC facility completed the survey, and this facility had partially implemented an EHR system.
Table 2.
EHR Implementation Status by Demographic Characteristics
| EHRs Fully or Partially Implemented | ||
|---|---|---|
| Characteristics | % | n |
| Ownership status | ||
| For-profit | 34.0% | (34/100) |
| Not-for-profit | 42.9% | (12/28) |
| Local government | 50.0% | (4/8) |
| State government | 100% | (1/1) |
| Location | ||
| Rural | 26.7% | (20/75) |
| Suburban | 59.1% | (13/22) |
| Urbana | 45.0% | (18/40) |
| Affiliation type | ||
| Hospital based | 55.6% | (5/9) |
| Part of a regional multicenter | (23/66) | |
| chain | 34.8% | |
| Part of a national multicenter | 50.0% | (8/16) |
| chain | ||
| Freestanding | 32.6% | (15/46) |
| Number of beds | ||
| 0–49 | 50.0% | (4/8) |
| 50–99 | 30.6% | (15/49) |
| 100–149 | 40.4% | (23/57) |
| 150 or more | 39.1% | (9/23) |
aIn this table, “urban” includes both urban and metropolitan statistical area (MSA) responses.
Rural facilities had a lower EHR implementation rate (26.7 percent) than suburban (59.1 percent) and urban (45.0 percent) facilities. The differences were statistically significant, with p-values of .002 and .023, respectively. Suburban and urban facilities’ EHR implementation rates were not significantly different, with a p-value of .85.
Table 2 displays that the EHR implementation rates varied in facilities with different affiliation types and sizes (number of beds). However, the differences were not significant, with p-values of .4 and .6, respectively; therefore, LTC facilities of different affiliation types and sizes have comparable EHR implementation rates in Texas.
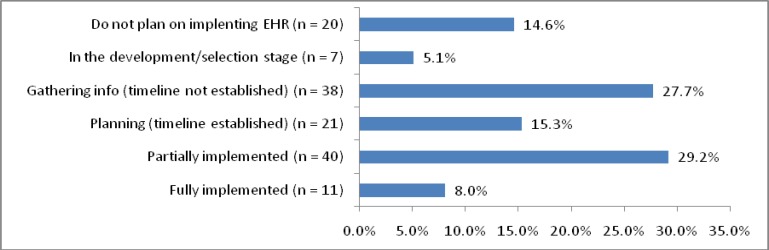
Figure 1 shows that almost one-third of the respondents have already implemented EHRs at least partially; however, almost as many (27.7 percent) have not yet established a timeline, and some (5.1 percent) are still in the selection stage. The percentage of facilities that do not plan on implementing an EHR system is 14.6 percent.
Figure 1.
EHR Implementation Status of Texas Long-Term Care Facilities
We compared EHR implementation status of LTC facilities in the 2007 California, 2008 Minnesota, and 2010–2011 Texas survey data (see Table 3) and found that except for the “not planning” proportion, the differences among other proportions of EHR implementation status in the three surveys are not statistically significant; that is, EHR implementation status across the states in the past several years is comparable.
Table 3.
Comparison of EHR Implementation in Long-Term Care Facilities
| Texas 2010–2011 | Minnesota 2008 | California2007 | ||||||
|---|---|---|---|---|---|---|---|---|
| % | n | % | n | % | n | χ2 | p-value | |
| Fully or partially implemented | 37.2% | 51 | 22.3% | 66 | 8.2% | 8 | 3.22 | .2 |
| Development or selection stage | 43.1% | 59 | 38.7% | 115 | 40.8% | 40 | 2.18 | .4 |
| Planning or information gathering | ||||||||
| stage | 5.1% | 7 | 7.4% | 22 | 10.2% | 10 | 0.75 | .7 |
| Not started or no plans | 14.6% | 20 | 31.6% | 94 | 40.8% | 40 | 11.21 | <.01 |
| Total | 137 | 297 | 98 | |||||
Functionalities
Respondents reported using 26 different software applications for EHRs in LTC facilities, with 25.5 percent of respondents having implemented American Healthtech.
The survey collected information about the utilization of technology to support administrative and clinical functions in LTC facilities (see Table 4 and Table 5). The survey results show significant variation in the use of these functions across LTC facilities. Because of federal and state regulations, it is not surprising that the finance functions, including billing, claim submission, payroll, and accounting, have the highest utilization status. The other administrative functions vary from a low adoption rate (13.9 percent for appointment reminders) to a high one (57.7 percent for admission). One surprising observation is that only 44.5 percent of LTC facilities have a Web site, and 48.2 percent of LTC facilities contact clients and staff via official e-mail. In the current information age, the website and e-mail utilization rate is quite low and will impede the communication and marketing efforts of the LTC facilities.
Table 4.
EHR Administrative Functionalities
| Administrative Functions | Survey Respondents | |
|---|---|---|
| % | n | |
| Communication and information distribution | ||
| Website | 44.5% | 61 |
| E-mail with clients | 48.2% | 66 |
| E-mail not with clients | 48.2% | 66 |
| Finance | ||
| Billing | 77.4% | 106 |
| Claim submission | 75.2% | 103 |
| Payroll | 62.8% | 86 |
| Accounting | 65.0% | 89 |
| Other | ||
| Human resources information management | 37.2% | 51 |
| Inventory management | 18.2% | 25 |
| Scheduling | 20.4% | 28 |
| Appointment reminder | 13.9% | 19 |
| Eligibility information | 23.4% | 32 |
| Prior authorization | 17.5% | 24 |
| Admission | 57.7% | 79 |
| Discharge | 50.4% | 69 |
| Transfer | 43.8% | 60 |
| Summary of services provided | 30.7% | 42 |
Notes:
Website refers to the utilization of an official website.
E-mail with clients refers to the utilization of official e-mail for contacting clients, including existing and prospective residents.
E-mail not with clients refers to the utilization of official e-mail for internal communication only.
Billing refers to the process of claim preparation, including coding.
Claim submission refers to the process in which claims are submitted to clearinghouses or insurers.
Payroll refers to the process of distribution of paychecks to employees each payday.
Accounting refers to the other accounting functionalities besides billing, claim submission, and payroll.
Human resources information management refers to the processes at the intersection of human resources management and information technology, such as online recruitment, hiring, training, and so forth.
Inventory management refers to the processes involved in the stocked goods management, such as ordering, shipping, handling, stocking, and so forth.
Scheduling refers to making arrangements for clients and internal staff.
Appointment reminder refers to the applications that automatically check physicians’ schedules and notify patients of upcoming appointments.
Eligibility information refers to an online system that provides timely and accurate information regarding a recipient's eligibility for services.
Prior authorization refers to the functionality that can submit preauthorization requests to insurers.
Admission refers to the applications applied in resident check-in processing.
Discharge refers to the applications applied in resident check-out processing.
Transfer refers to the applications applied in the resident transferring process.
Summary of services provided refers to the applications applied in summarizing services provided.
Table 5.
EHR Clinical Functionalities
| Clinical Functions | Survey Respondents | |
|---|---|---|
| % | n | |
| Resident assessment | ||
| Minimum data set (MDS) | 84.7% | 116 |
| Resident assessment protocols (RAPs) | 72.3% | 99 |
| Triggers | 61.3% | 84 |
| Computerized provider order entry (CPOE) | ||
| Physician orders | 56.9% | 78 |
| E-prescribing between practitioner and pharmacy | 10.2% | 14 |
| Medication orders and drug dispensing | 32.8% | 45 |
| Laboratory/procedures information | 34.3% | 47 |
| Care management | ||
| Individual care management plan | 59.1% | 81 |
| Clinical charting applications, including assessment and progress notes | 24.1% | 33 |
| Receiving external clinical documents | 14.6% | 20 |
| Treatment administration information | 29.2% | 40 |
| Electronic access to an assigned care manager | 16.1% | 22 |
| Dietary | 35.0% | 48 |
| Clinical decision support tools | 20.4% | 28 |
| Census management | 50.4% | 69 |
Notes:
Minimum data set (MDS) refers to the utilization of MDS.
Resident assessment protocols (RAPs) refers to the utilization of RAPs.
Triggers refer to the utilization of Triggers.
Physician orders refer to the processes of electronic entry of medical practitioner instructions for the treatment of residents under the practitioner's care.
E-prescribing refers to the electronic transmission of prescription information from the prescriber's computer to a pharmacy computer.
Medication orders and drug dispensing refers to the processes during the preparation, packaging, labeling, record keeping, and transfer of a prescription drug to a resident.
Laboratory/procedures information refers to a class of applications that receives, processes, and stores information generated by medical laboratory processes.
Individual care management plan refers to a collaborative process of assessment, planning, facilitation, and advocacy for options and services to meet a resident's needs.
Clinical charting applications refers to the applications in clinical charting, including assessment and progress notes.
Receiving external clinical documents refers to the ability to receive external clinical documents about the residents, including provider notes, lab data, radiology data, medical devices, patient history, and so forth.
Treatment administration information refers to the ability to manage the residents' treatment information.
Electronic access to an assigned care manger allows an existing or perspective resident to access an assigned care manager online.
Dietary refers to the IT application to manage residents' dietary needs.
Clinical decision support tools provide best-practice suggestions for care plans and interventions based on clinical problems or diagnoses.
Census management refers to patient demographics.
Except for the resident assessment functions, including the minimum data set (MDS), the resident assessment protocols (RAPs), and the Triggers, which have been required by federal regulations since the 1990s, the other clinical functions are used less than the administrative ones.29 That finding is the same as the observations in previous studies, which found that the administrative functions are more widely adopted and utilized than the clinical functions.30, 31 Physician orders, the most frequently discussed clinical function to reduce potential errors in healthcare, have a 56.9 percent utilization rate. The other two functions with utilization rates greater than 50 percent are the individual care management plan (59.1 percent) and census management (50.4 percent) functions. This result is also similar to the findings in previous reports.32, 33 In this survey, e-prescribing between practitioner and pharmacy is the clinical function with the lowest adoption rate (10.2 percent).
Barriers
Survey respondents rated four groups of barriers that may have slowed or prevented them from implementing EHRs in their facilities. The four groups of barriers include capital factors, human resource factors, EHR product factors, and management factors. Results are reported in Table 6.
Table 6.
Barriers Slowing or Preventing EHR Implementation
| Barriers | Survey Respondents | |
|---|---|---|
| % | n | |
| Capital factors | ||
| Lack of capital resources to invest | 46.0% | 63 |
| Lack of proven benefit | 15.3% | 21 |
| Lack of technical infrastructure (servers, etc.) | 35.0% | 48 |
| Human resource factors | ||
| Insufficient time to select, contract, install software/technology | 29.2% | 40 |
| Lack of health information technology (HIT) knowledge | 12.4% | 17 |
| Fear of technology | 8.0% | 11 |
| Lack of technical support staff | 21.2% | 29 |
| EHR product factors | ||
| Difficulty finding HIT products that meet needs | 20.4% | 28 |
| Too complex | 7.3% | 10 |
| User interfaces are not user friendly | 16.1% | 22 |
| Inability to easily input historic medical record data into software/technology | ||
| system | 27.0% | 37 |
| Management factors | ||
| Risk of new state/federal requirements | 18.2% | 25 |
| Not part of the strategic planning | 15.3% | 21 |
| Unclear benefits of EHR in improving quality | 15.3% | 21 |
| Unclear needs for change management | 11.7% | 16 |
“Lack of capital resources to invest” is the number one barrier to EHR implementation in all three surveys (46.0 percent in Texas in 2010–2011, 72.1 percent in Minnesota in 2008, and 60.0 percent in California in 2007). “Lack of technical infrastructure” is the second most frequently reported barrier in this survey (35 percent). “Insufficient time” (29.2 percent) and “inability to easily input historic medical record data” (27 percent) are the next two reported barriers, which were also the barriers found in the Minnesota and California reports. This finding indicates that these problems have not been solved yet. “Lack of technical support staff” (21.2 percent) is another barrier cited by more than 20 percent of respondents in this survey. Other barriers were cited by fewer than 20 percent of respondents, but the long list of barriers shows that the LTC EHR market is complicated; therefore, a “one size fits all” strategy does not work. “Risk of new state/federal requirements” (18.2 percent) leads in the management barrier category. This result shows that the rapid development of federal and state regulations recently is a concern to the LTC administrators.
Discussion
This research study is an assessment of EHR adoption and utilization status in Texas LTC facilities. This study establishes a baseline and offers a cross-sectional view of EHR adoption and utilization status in Texas LTC facilities. It summarizes EHR adoption and utilization status, the functionalities of EHRs in use, and the barriers to EHR implementation. Given the rapid rate of change in the EHR industry and the evolution of LTC facilities in Texas, future studies are necessary to understand the trends in adoption and utilization of EHRs.
This survey identified important factors for policy makers, EHR vendors, LTC administrators, educators, and researchers to consider in promoting EHR adoption and utilization. First, for policy makers, this survey reiterates the barriers to EHR adoption in LTC facilities. Of those, the top barrier is still the lack of capital resources. This finding shows that the significant capital costs of implementing EHRs are still a burden for LTC facilities, particularly those operating close to their financial margins. State and private organizations should work with LTC facilities to address this barrier, and the government has to continue seeking better incentives to solve this challenging issue in EHR adoption. Based on this survey, lack of technical infrastructure is another serious barrier in Texas. This finding may show that the development of IT infrastructure in LTC facilities in Texas deserves more attention. Another barrier, the risk of new state or federal requirements, shows that policy makers should accelerate the establishment of a long-term agenda for EHR regulations to provide a clearer guideline in EHR adoption and utilization.
Although a LTC facility may have the opportunity to use an EHR system adopted by hospitals, the EHR system may not meet the specific complex and diverse needs of the LTC facility and may therefore be only partially used. Development of an EHR system in a collaborative fashion for LTC facilities should be supported. It is unclear how EHR vendors are prepared to meet the needs of LTC clients. This question should be explored. Although EHR systems have been in existence for decades, the inability to input historical data is still a big barrier to EHR adoption and utilization. Better communication between vendors and LTC facilities is indispensable for more effective EHR system design and development for LTC facilities.
Finally, as shown in this survey, lack of proven benefits of EHR use is a barrier to EHR adoption and utilization. Researchers should conduct research examining the relationship of EHR utilization to the financial outcomes and quality of care in LTC facilities.
We believe that education and training are the solution to some issues related to EHR adoption and utilization in LTC facilities. First, training more EHR-related professionals is helpful to alleviate the problem of lack of technical support staff. Secondly, even in the current information age, more than 10 percent of LTC administrators have no plans to adopt EHRs and do not know the needs and benefits of EHRs. LTC administrators should attend EHR training programs to keep abreast of compliance and technology requirements. Finally, education programs are also necessary for policy makers, who may underestimate the importance of EHRs.
Limitation
One limitation of the study is that 15 percent of LTC facilities completed the survey. Nonresponse bias could be a concern. In future research, the authors will include a tracking design in the questionnaire to follow up with nonrespondents and improve the response rate. On the other hand, the whole population was surveyed. Inspection of the distribution of responses suggests that the survey sample is representative of the population of Texas LTC facilities. Therefore, although the response rate is low, the conclusions drawn in the study can be inferred to apply to the whole population of Texas LTC facilities.
Conclusion
Although the Health Information Technology for Economic and Clinical Health Act of 2009 produced a great deal of attention to and knowledge of the benefits of EHR systems, the status of EHR adoption and utilization in Texas in 2010–2011 is similar to that found in Minnesota in 2008 and California in 2007. Lack of capital resources is still the leading barrier in EHR adoption and utilization, and the other barriers remain unsolved. More challenges and opportunities for adopting EHRs in LTC facilities are faced by LTC administrators, vendors, policy makers, educators, and researchers.
Support
Funding for this study was provided by the Texas Long Term Care Institute.
Contributor Information
Tiankai Wang, the Health Information Management Department of Texas State University–San Marcos in San Marcos, TX..
Sue Biedermann, the Health Information Management Department of Texas State University–San Marcos in San Marcos, TX..
Notes
- 1.Institute of Medicine (IOM) Improving the Quality of Long-Term Care. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 2.LTC HIT Summit. A Road Map for Health IT in Long Term Care 2008.
- 3.MedPAC (Medicare Payment Advisory Commission) Report to the Congress: Issues in a Modernized Medicare Program. Washington, DC: MedPAC; 2005. [Google Scholar]
- 4.Coleman E. “Falling through the Cracks: Challenges and Opportunities for Improving Transitional Care for Persons with Continuous Complex Care Needs”. Journal of the American Geriatric Society. 2003;51(2):549–55. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 5.Hamilton, B. A. Evaluation Design of the Business Case of Health Information Technology in Long-Term Care (Final Report) US Department of Health and Human Services, 2006.
- 6.Congressional Budget Office (CBO). Evidence on the Costs and Benefits of Health Information Technology 2008.
- 7.WinterGreen Research, Inc. Nursing Home and Long-Term Care Information Systems: Market Opportunities, Strategies, and Forecasts, 2006 to 2012 2006.
- 8.Menachemi N, Burke B, Brooks R. “Adoption Factors Associated with Patient Safety-related Information Technology”. Journal of Healthcare Quality. 2004;26(no. 6):39–44. doi: 10.1111/j.1945-1474.2004.tb00535.x. [DOI] [PubMed] [Google Scholar]
- 9.Kaushal R, Bates D. W, Poon E. G, Jha A. K, Bluementhal D, the Harvard Interfaculty Program for Health Systems Improvement NHIN Working Group “Functional Gaps in Attaining a National Health Information Network”. Health Affairs. 2005;24(no. 5):1281–89. doi: 10.1377/hlthaff.24.5.1281. [DOI] [PubMed] [Google Scholar]
- 10.LTC HIT Summit. A Road Map for Health IT in Long Term Care
- 11.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton S, Shekelle P. “Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Cost of Medical Care”. Annals of Internal Medicine. 2006;144(no. 10):E12–W18. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 12.Rochon P.A, Field T. S, Bates D. W, Lee M, Gavendo L, Errramuspe-Mainard J, Judge J, Gurwitz J. H. “Computerized Physician Order Entry with Clinical Decision Support in the Long-Term Care Setting: Insights from the Baycrest Centre for Geriatric Care”. Journal of American Geriatrics Society. 2005;53(no. 10):1780–89. doi: 10.1111/j.1532-5415.2005.53515.x. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine (IOM). Improving the Quality of Long-Term Care
- 14.US Department of Health and Human Services. Survey Questions for EHR Adoption and Use in Nursing Homes: Final Report 2010.
- 15.US Department of Health and Human Services. Survey Questions for EHR Adoption and Use in Nursing Homes: Final Report 2010.
- 16.Stratis Health. Minnesota Nursing Home Health Information Technology Survey Results Minnesota Department of Health, Minnesota e-Health Initiative, 2008.
- 17.Hudak, S., and S. Sharkey. Health Information Technology: Are Long Term Care Providers Ready? California HealthCare Foundation, 2007.
- 18.West D, Szeinbach S, Harp S. “Information Technology and System Integration in Long-Term Care”. The Consultant Pharmacist. 1997;12(no. 9):976–86. [Google Scholar]
- 19.Kaushal R, Bates D. W, Poon E. G, Jha A. K, Bluementhal D, the Harvard Interfaculty Program for Health Systems Improvement NHIN Working Group “Functional Gaps in Attaining a National Health Information Network”. Health Affairs. 2005;24(no. 5):1281–89. doi: 10.1377/hlthaff.24.5.1281. [DOI] [PubMed] [Google Scholar]
- 20.Stratis Health. Minnesota Nursing Home Health Information Technology Survey Results
- 21.Hudak, S., and S. Sharkey. Health Information Technology: Are Long Term Care Providers Ready? [PMC free article] [PubMed]
- 22.Kaushal R, Bates D. W, Poon E. G, Jha A. K, Bluementhal D, the Harvard Interfaculty Program for Health Systems Improvement NHIN Working Group “Functional Gaps in Attaining a National Health Information Network”. Health Affairs. 2005;24(no. 5):1281–89. doi: 10.1377/hlthaff.24.5.1281. [DOI] [PubMed] [Google Scholar]
- 23.Ward M, Jaana M, Bahensky J, Vartak S, Wakefield D. “Clinical Information System Availability and Use in Urban and Rural Hospitals”. Journal of Medical Systems. 2006;30:429–38. doi: 10.1007/s10916-006-9014-3. [DOI] [PubMed] [Google Scholar]
- 24.Stratis Health. Minnesota Nursing Home Health Information Technology Survey Results
- 25.Hudak, S., and S. Sharkey. Health Information Technology: Are Long Term Care Providers Ready? [PMC free article] [PubMed]
- 26.Ash J, Berg A, Cohera E. “Some Unintended Consequences of Information Technology in Health Care: The Nature of Patient Care Information System-related Errors”. Journal of the American Medical Informatics Association. 2004;11:104–12. doi: 10.1197/jamia.M1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O'Connell R. C. Cho, Shah N, Brown K, R. Shiffman. “Take Note(s): Differential EHR Satisfaction with Two Implementations under One Roof”. Journal of the American Medical Informatics Association. 2004;11(no. 1):43–49. doi: 10.1197/jamia.M1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jaana M, Ward M, Pare G, Sicotte C. “Antecedents of Clinical Information Technology Sophistication in Hospitals”. Health Care Management Review. 2006;31(no. 4):289–99. doi: 10.1097/00004010-200610000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Resnick H.E, Manard B. B, Stone R. I, Alwan M. “Use of Electronic Information Systems in Nursing Homes: United States, 2004”. Journal of the American Medical Informatics Association. 2009;16(no. 2):179–86. doi: 10.1197/jamia.M2955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaushal R, Bates D. W, Poon E. G, Jha A. K, Bluementhal D, the Harvard Interfaculty Program for Health Systems Improvement NHIN Working Group “Functional Gaps in Attaining a National Health Information Network”. Health Affairs. 2005;24(no. 5):1281–89. doi: 10.1377/hlthaff.24.5.1281. [DOI] [PubMed] [Google Scholar]
- 31.Flex Monitoring Team. The Current Status of Health Information Technology Use in CAHs Flex Monitoring Team Brief Paper No. 11. 2006.
- 32.Stratis Health. Minnesota Nursing Home Health Information Technology Survey Results
- 33.Hudak, S., and S. Sharkey. Health Information Technology: Are Long Term Care Providers Ready? [PMC free article] [PubMed]