Abstract
Objectives. We assessed whether a 2-phase labeling and choice architecture intervention would increase sales of healthy food and beverages in a large hospital cafeteria.
Methods. Phase 1 was a 3-month color-coded labeling intervention (red = unhealthy, yellow = less healthy, green = healthy). Phase 2 added a 3-month choice architecture intervention that increased the visibility and convenience of some green items. We compared relative changes in 3-month sales from baseline to phase 1 and from phase 1 to phase 2.
Results. At baseline (977 793 items, including 199 513 beverages), 24.9% of sales were red and 42.2% were green. Sales of red items decreased in both phases (P < .001), and green items increased in phase 1 (P < .001). The largest changes occurred among beverages. Red beverages decreased 16.5% during phase 1 (P < .001) and further decreased 11.4% in phase 2 (P < .001). Green beverages increased 9.6% in phase 1 (P < .001) and further increased 4.0% in phase 2 (P < .001). Bottled water increased 25.8% during phase 2 (P < .001) but did not increase at 2 on-site comparison cafeterias (P < .001).
Conclusions. A color-coded labeling intervention improved sales of healthy items and was enhanced by a choice architecture intervention.
New public health strategies are needed to combat the rising prevalence of obesity. A major contributor to obesity is the consumption of energy-dense food purchased outside the home.1,2 Interventions targeting the point of purchase have the potential to reduce obesity at the population level.3–5
Menu labeling with calories is a policy that has been gaining public and legislative support since 2006 and will soon be mandated as part of the Patient Protection and Affordable Health Care Act for restaurants and food vendors with more than 20 locations.3,6–9 However, listing calorie information is effective only if consumers understand how to interpret it.10 Previous research has demonstrated that the ability to correctly interpret nutrition information requires not only high literacy but also high numeracy skills.11 Evidence for the effectiveness of calorie labeling has been equivocal,12–18 and one study of a low-income, minority population in New York City found no effect of calorie labeling on food purchases.17
Information-based labeling policies were created with the assumption that, given calorie information, consumers will make a rational choice by choosing lower calorie options.19,20 However, behavioral economists and psychologists have identified decision biases that explain why individuals often make choices, such as overeating, leading to poor health outcomes.19,21 Patterns of behavior that may play a role in poor nutrition choices include individuals’ tendency to stay with the usual or default option, to be motivated by actions with immediate benefit, and to be less motivated by actions with long-term benefit as well as limitations of self-control.19,20 “Choice architecture” refers to the framing or presentation of choice options.21 Strategies to change choice architecture by setting specific default choices have been successful in increasing individuals’ retirement savings and organ donations.22,23 One study demonstrated that changing the location of healthy sandwiches to the front page of a menu was more effective than was providing calories.16
We conducted a 2-phase food-labeling intervention that addressed low nutritional literacy and decision biases during 6 months in a large hospital cafeteria. Phase 1 was a simple color-coded labeling intervention of food and beverages. Phase 2 was a choice architecture intervention to increase visibility and convenience of healthy items in the cafeteria. We compared the change in sales of healthy and unhealthy items from baseline to phase 1 and from phase 1 to phase 2.
METHODS
The setting for this study was the main cafeteria at Massachusetts General Hospital in Boston between December 1, 2009 and September 1, 2010. The hospital has 1 main cafeteria and 4 smaller on-site cafeterias. The Massachusetts General Hospital Nutrition and Food Services operates all cafeterias. The main cafeteria is open 7 days a week from 6:30 a.m. to 8:00 p.m. The average number of transactions during each weekday is 6534, and the average sales during each weekday are $31 404. During the 2 years before we started the study, overall cafeteria sales did not vary by season (winter, spring, summer, or fall).
Intervention
After collecting baseline data for 3 months, we conducted a 2-phase intervention for 6 months. Phase 1 was a labeling intervention designed to inform cafeteria patrons about the relative healthiness of cafeteria items with a simple color-coded scheme. Phase 2 maintained the labeling and added a choice architecture intervention to increase the visibility and convenience of some healthy items.
Phase 1: labeling intervention. We designed a color-coded scheme to label all items red, yellow, or green on the basis of the United States Department of Agriculture's 2005 My Pyramid healthy eating recommendations.24 The Massachusetts General Hospital staff nutritionists developed the food rating system in this study. We rated packaged items on the basis of the nutrition information provided on the product label. We rated food prepared in the cafeteria on the basis of the individual ingredients for each of the recipes. We calculated the fat and calorie contents for the average portion size served to each individual. Before beginning the study, all the cafeteria cooks and servers were required to participate in an in-service seminar to reinforce the importance of consistency in measuring recipe ingredients and serving specified portion sizes to customers.
We categorized all food and beverages into 4 groups (food entree, food item, food condiment, or beverage) and rated them on 3 positive and 2 negative criteria. The 3 possible positive criteria for a food or beverage were (1) being a fruit or vegetable, (2) being a whole grain, or (3) having lean protein or low-fat dairy as the main component (defined as 1 of the first 3 ingredients by weight) of the item. Negative criteria were related to the saturated fat and caloric content of a food or beverage assuming a 2000-calorie per day diet with less than 10% of calories from saturated fat. We set an upper limit of 5 grams of saturated fat per food entree and 2 grams of saturated fat per food item, condiment, or beverage to account for 3 meals per day (each with ≤ 5 g of saturated fat) plus 5 grams of saturated fat for discretionary calories in snacks. For calories, we assumed 3 meals per day at 500 calories each and 500 discretionary calories. Therefore, the 2 possible negative criteria for a food or beverage were a (1) saturated fat content of 5 or more grams per entree or 2 or more grams per item, condiment, or beverage; and (2) caloric content of 500 or more kilocalories per entree, 200 or more kilocalories per item, or 100 or more kilocalories per condiment or beverage. For beverages, we considered each additional 100 kilocalories an additional negative criterion.
We categorized food and beverages that had more positive criteria than negative criteria as green. We categorized food and beverages that had positive criteria equal to negative criteria or that possessed only 1 negative criterion as yellow. We categorized food and beverages that had 2 negative criteria and no positive criteria as red. We rated items with no positive or negative criteria as yellow, except for diet beverages with zero calories, which we rated green. Red beverages included sugar-sweetened beverages with 200 or more kilocalories per container and whole milk dairy products with 100 or more kilocalories and 5 or more grams of saturated fat per container. Yellow beverages included sugar-sweetened beverages with less than 200 kilocalories per container. Fountain soda was not available in the cafeteria during the study, and therefore all cold beverages were sold in prepackaged cans, cartons, or bottles.
The labeling intervention began in March 2010. During 1 weekend, all food and beverages were labeled red, yellow, or green on the menu board located either directly over the individual food station, directly over the shelf where the food was located, or directly on the packaging. The labeling intervention was advertised as the Massachusetts General Hospital Choose Well, Eat Well program, and the message to cafeteria patrons focused on making a better choice. We posted new signage to describe the labeling on a wall in the cafeteria as well as on 2 large columns in the middle of the cafeteria. This signage highlighted that green meant “consume often,” yellow meant “consume less often,” and red meant “there is a better choice in green or yellow.” Rather than tell patrons to stop for red items, we used a positive yet clear message to redirect patrons toward a better choice. During the first 2 weeks, a dietician was available in the cafeteria to answer questions about the labels. Throughout both phases 1 and 2, we supplied the cafeteria with pocket-sized pamphlets containing information about the labeling as well as the specific amount of calories and fat in all items.
Phase 2: Choice architecture intervention. In June 2010, we began the choice architecture intervention. We made the changes for this phase over a weekend and did not advertise them. The main target items for phase 2 were cold beverages, premade sandwiches, and chips. We chose cold beverages because they represented a large portion of cafeteria sales (20% of overall sales), and we hypothesized that location and convenience would influence beverage purchases. We also hypothesized that location and convenience would influence the sales of chips and premade sandwiches because cafeteria patrons who do not have a lot of time to spend in the cafeteria are likely to purchase these items.
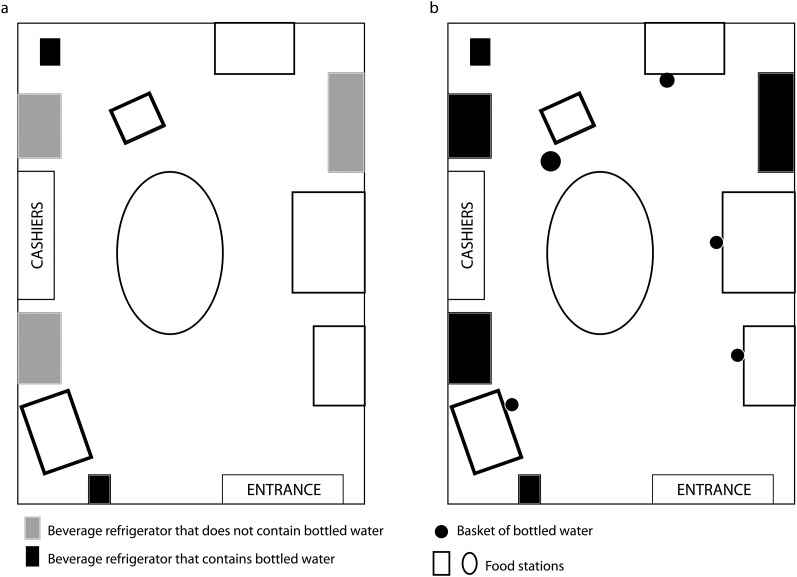
We rearranged all 5 beverage refrigerators so that the green beverages (including water, diet beverages, and low-fat dairy products) were located at eye level and yellow and red beverages were located below eye level. We defined eye level as a height between 5 and 6 feet. During baseline and phase 1, bottled water was available in 2 refrigerators that were not centrally located in the cafeteria, similar to the cafeteria layout before the study started (Figure 1). During phase 2, we added bottled water to the other 3 beverage refrigerators and added 5 baskets of bottled water throughout the cafeteria near the food stations (Figure 1). We rearranged the premade sandwich refrigerator so that the green sandwiches were located at eye level and the yellow and red sandwiches were below or above eye level. Chips were located on 2 adjacent racks, and we placed the yellow chips on the higher eye level racks and the red chips on the bottom (no chips were rated green).
FIGURE 1—
Location of bottled water for sale in the cafeteria during (a) baseline and phase 1, and (b) phase 2: a 2-phase labeling and choice architecture intervention; Massachusetts General Hospital, Boston; December 1, 2009–September 1, 2010.
Data Collection and Measures
Before collecting any data, all 9 cafeteria cash registers were programmed to capture the information needed to identify an item as red, yellow, or green. Throughout the study, register data were exported daily. The 14 cashiers who worked in the cafeteria during the study were trained to enter the specific names of food and beverages (e.g., diet soda or regular soda rather than just “soda”), and then we categorized the item as red, yellow, or green once it was in the database. During the baseline phase, 10 anonymous shoppers made purchases in the cafeteria over the course of 9 weeks to validate the accuracy of data entry. The cashiers knew that they were being tested during this period but did not know when the testing would occur. Overall, during 9 weeks, the cashiers entered 847 out of 901 (94%) items correctly, and accuracy increased from 89% to 96% during the 9 weeks.
The primary outcome was change in sales of red and green items from baseline to phase 1 and from phase 1 to phase 2. Secondary outcomes were change in sales of cold beverages, premade sandwiches, and chips. For the primary outcome, we compared the proportion of total sales that were labeled red or green across all phases. As a secondary outcome, we compared the proportion of cold beverages sold that were labeled red, yellow, or green as well as the proportion that were diet soda, regular soda, and bottled water. We analyzed the proportions of premade sandwiches that were labeled red or green as well as the proportion of chips that were labeled red.
Analysis
We excluded data from weekends and holidays, including the week from December 24, 2009 to January 3, 2010. We also excluded data from May 1, 2010 to May 5, 2010 because of a “boil water” emergency in the city of Boston that affected cafeteria sales. The salad bar items were sold by weight. We assigned all salad bar purchases as green because the majority of the daily salad bar options were green (60%–67% green and 33%–36% yellow). We were unable to include 2.7% of items sold in the cafeteria in the analysis because we could not definitively identify them as red, yellow, or green through the cash registers. We calculated the statistical significance of changes from one phase to the next using logistic regression to model the likelihood that an item was of a given type (e.g., green), controlling for day of the week and adjusting for clustering within phase.
Comparison Site Analysis
We compared sales of bottled water, premade sandwiches, and chips in the main cafeteria to 2 on-site cafeterias that did not have the labeling or choice architecture interventions. There were 1482 daily weekday transactions for the comparison sites. We were unable to compare other items because the comparison site cash registers were not programmed to collect these data. For these analyses, we used a difference-in-differences approach to calculate changes in purchases between subsequent phases at the intervention site after controlling for changes observed in the control sites. For example, the framework for the difference-in-differences analysis for bottled water during phase 2 was as follows: (the proportion of bottled water purchased in the cafeteria during phase 2 − the proportion of bottled water purchased in the cafeteria during phase 1) − (the proportion of bottled water purchased in the comparison sites during phase 2 − the proportion of bottled water purchased in the comparison sites during phase 1). We used logistic regression to calculate these quantities and the statistical significance of the changes using indicators for phase, an indicator for site, and phase by site interaction terms, all controlling for day of the week. A statistically significant interaction term indicated the change was associated with the intervention rather than existing trends in purchasing.
RESULTS
During the baseline period, there were 977 793 items sold in the cafeteria; 24.9% of sales were red, 32.9% were yellow, and 42.2% were green (Table 1). There were 199 513 cold beverages sold; 26.1% were red, 21.6% were yellow, and 51.7% were green.
TABLE 1—
Relative Change in Sales of Red, Yellow, and Green Cafeteria Items During the 2-Phase Intervention: A 2-Phase Labeling and Choice Architecture Intervention; Massachusetts General Hospital, Boston; December 1, 2009–September 1, 2010
| Sale Item | Baseline,a % | Phase 1: Labeling,b Relative % Change in Sales From Baseline | Phase 2: Labeling + Choice Architecture,c Relative % Change in Sales From Phase 1 |
| Total sales | |||
| All red items | 24.9 | −9.2 | −4.9 |
| All yellow items | 32.9 | 1.2 | 3.9 |
| All green items | 42.2 | 4.5 | −0.5 |
| Beverage sales | |||
| All red beverages | 26.1 | −16.5 | −11.4 |
| All yellow beverages | 21.6 | −0.2 | 1.1 |
| All green beverages | 51.7 | 9.6 | 4.0 |
| Diet soda | 19.6 | 9.2 | −0.8 |
| Regular soda | 19.5 | −23.1 | −5.9 |
| Bottled water | 13.6 | −2.4 | 25.8 |
Note. P < .001 for all.
For all items sold, n = 977 793; for all beverages sold n = 199 513.
For all items sold, n = 988 734; for all beverages sold n = 202 098.
For all items sold, n = 958 197; for all beverages sold n = 198 557.
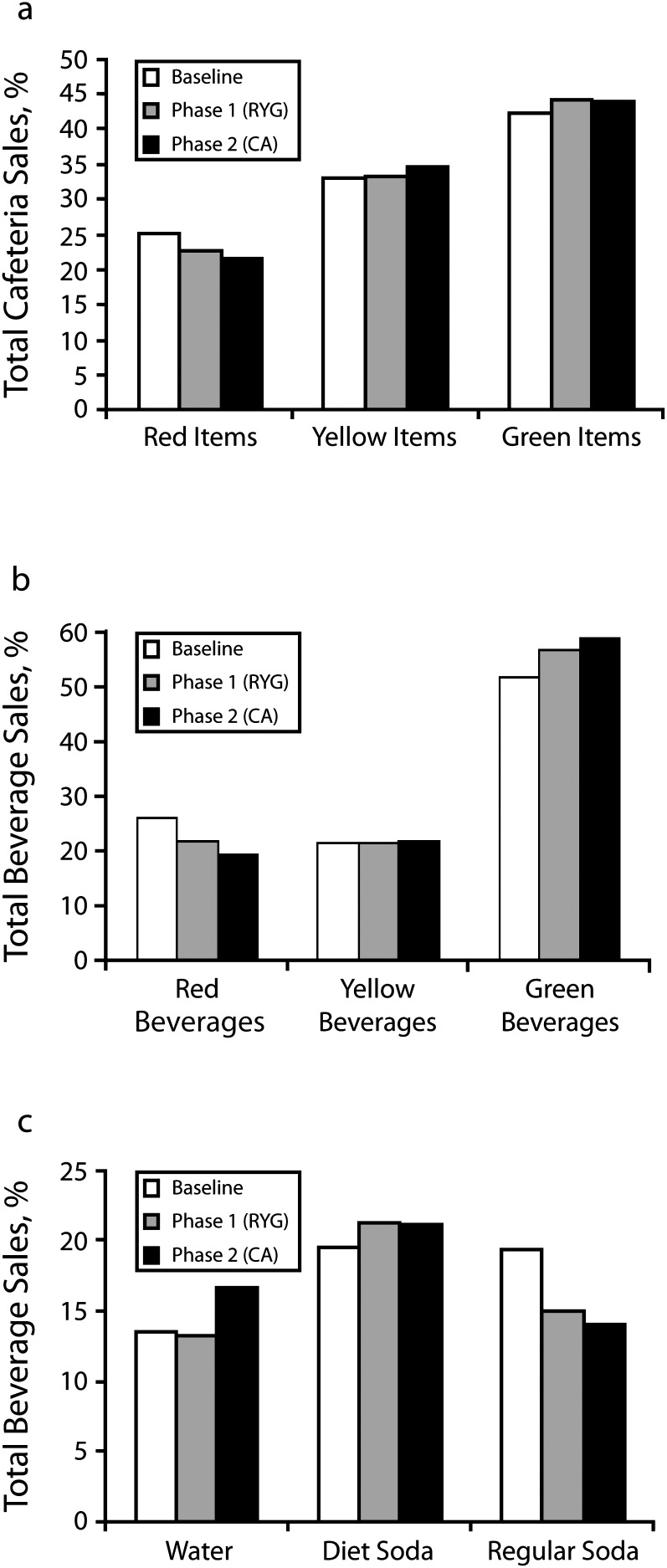
Figure 2 shows the proportion of sales of items that were red, yellow, and green during the baseline period, phase 1 (labeling), and phase 2 (labeling + choice architecture). From baseline to phase 2, the sales of red items decreased and the sales of green items increased (for both, P < .001). Sales of bottled water and diet soda increased, and sales of regular soda decreased (for both, P < .001). Table 1 shows the relative changes in sales of red, yellow, and green items during the 2 intervention phases. During phase 1, sales of all red items decreased 9.2% (P < .001), and all red beverages decreased 16.5% (P < .001). During phase 2, sales of red items further decreased 4.9% (P < .001), and red beverages decreased 11.4% (P < .001). All green items increased 4.5% (P < .001) during phase 1, and green beverages increased 9.6% (P < .001). During phase 2, sales of all green items decreased 0.8% (P < .001) relative to phase 1, but green beverages further increased 4.0% (P < .001).
FIGURE 2—
Proportion of red, yellow, and green items sold during baseline, phase 1 (labeling), and phase 2 (labeling + choice architecture): a 2-phase labeling and choice architecture intervention; Massachusetts General Hospital, Boston; December 1, 2009–September 1, 2010.
Note. CA = choice architecture; RYG = red, yellow, green.
To better understand beverage sales, we looked specifically at diet soda, regular soda, and bottled water. Diet soda sales increased 9.2% (P < .001) during phase 1 and then decreased 0.8% (P < .001) during phase 2 relative to phase 1 (Table 1). Regular soda sales decreased 23.1% (P < .001) during phase 1 and then decreased an additional 5.9% (P < .001) in phase 2. Although bottled water sales decreased 2.4% (P < .001) during phase 1, there was a large increase in sales of 25.8% (P < .001) during phase 2. Compared with baseline, the mean number of red beverages sold daily in phase 2 decreased by 238, and the mean number of green beverages increased by 199 (Table 2).
TABLE 2—
Change in Mean Number of Cold Beverages Sold in the Cafeteria Daily During the Intervention Compared With Baseline: A 2-Phase Labeling and Choice Architecture Intervention; Massachusetts General Hospital, Boston; December 1, 2009–September 1, 2010
| Sale Item | Number Sold Daily During Baseline, Mean (SD) | Number Sold Daily During Phase 2, Mean (SD) | Change From Baseline to Phase 2 |
| All beverages | 3303 (180) | 3255 (158) | −48 |
| Red beverages | 866 (85) | 628 (56) | −238 |
| Yellow beverages | 718 (84) | 709 (49) | −9 |
| Green beverages | 1719 (148) | 1918 (105) | 199 |
| Diet soda | 651 (54) | 691 (48) | 40 |
| Regular soda | 649 (103) | 459 (46) | −190 |
| Bottled water | 452 (40) | 544 (45) | 92 |
Table 3 shows the comparison of the sales of specific items targeted in the phase 2 intervention between the main cafeteria (intervention site) and 2 on-site comparison cafeterias. Bottled water, prepackaged sandwiches, and chips were sold at both the intervention and comparison cafeterias and were identifiable with available cash register data. Sales of bottled water increased significantly more in the intervention site than in the comparison sites during phase 2 (between-group absolute difference was 3.2%; P < .001). The sales of red sandwiches decreased more and the sales of green sandwiches increased more in the intervention site compared with the comparison sites, and the sales of chips labeled red decreased significantly more in the intervention site than in the comparison sites.
TABLE 3—
Change in Sales of Items Targeted During the Choice Architecture Intervention at the Intervention Site and Comparison Sites: A 2-Phase Labeling and Choice Architecture Intervention; Massachusetts General Hospital, Boston; December 1, 2009–September 1, 2010
| Phase 1: Labeling |
Phase 2: Labeling + Choice Architecture |
||||
| Sale Item | Baseline Proportion of Sales,a % | Absolute Change in Sales From Baseline,% | Between-Group Difference, % | Absolute Change in Sales From Phase 1, % | Between-Group Difference |
| Bottled water | |||||
| Intervention site | 13.6 | −0.3 | −1.1 | 3.4 | 3.2 |
| Comparison sites | 18.6 | 0.8 | 0.3 | ||
| Red sandwiches | |||||
| Intervention site | 14.6 | 2.5 | −0.3 | −2.7 | −0.7 |
| Comparison sites | 10.3 | 2.8 | −2.0 | ||
| Green sandwiches | |||||
| Intervention site | 24.0 | 0.5 | 1.9 | 7.5 | 4.3 |
| Comparison sites | 20.2 | −1.4 | 3.2 | ||
| Red chips | |||||
| Intervention site | 36.7 | −0.8 | −3.9 | −5.2 | −11.2 |
| Comparison sites | 77.4 | 3.1 | 6.1 | ||
Note. P < .001 for all.
Proportion of baseline sales for each type of item at the intervention or the control site (i.e., water is a proportion of all beverage sales, sandwiches are a proportion of all premade sandwich sales, and chips are a proportion of all chips sales).
DISCUSSION
Our results demonstrate that a simple color-coded labeling intervention increased sales of healthy items and decreased sales of unhealthy items in a large hospital cafeteria. A choice architecture intervention that improved the visibility and convenience of healthy items further improved the effectiveness of labeling. By addressing low nutrition literacy and decision biases with our intervention, we saw significant improvements in food and beverage choices of cafeteria patrons over the 6-month period.
Menu labeling with calories is a public health policy that has already been implemented in some US cities and will soon be required by federal law.8,9 The evidence for the effectiveness of this policy is unclear. Some studies suggest that consumers purchase slightly fewer calories with calorie labeling,12–15 whereas others have shown no change in calories purchased.12,16–18 Most studies rely on cross-sectional designs and register receipts, self-report, or direct observation.
Reading and understanding nutrition labels is a complex task.10,11 Even highly literate consumers may have difficulty interpreting labels because of low numeracy skills.11 Interpreting the meaning of caloric information on a menu requires an understanding of one's total caloric needs, an accurate estimation of a serving size, and adequate time at the point of purchase to consider and act on the information. Phase 1 of our intervention tested a simplified labeling scheme. Although this scheme provided the consumer with less precise information than does calorie labeling, it conveyed complex information in a way that could be easily understood and acted on immediately. The effectiveness of this system was most striking for beverage sales, with red beverages decreasing 16.5% and green beverages increasing 9.6%.
Any information-based labeling intervention, however, does not account for decision biases inherent in many individuals’ health behaviors.19,20 Phase 2 of our study tested whether changing the choice architecture by rearranging the presentation of the food or beverage options would increase healthier choices. The strongest example of the effectiveness of this intervention was the increase in bottled water purchases. During phase 1, bottled water remained in 2 refrigerators that were not centrally located in the cafeteria (Figure 1), and despite the green label, there was a slight decrease in sales. During phase 2, bottles of water were placed in every refrigerator in the cafeteria at eye level as well as in baskets near several of the food stations (Figure 1), and water sales increased 25.8%. By making water the default choice, the choice architecture reduced the likelihood that patrons would be tempted by sugared beverages that were less prominently displayed but still available for purchase.
The consumption of sugar-sweetened beverages in the United States has increased dramatically in recent decades, and there is strong epidemiologic evidence for the association between sugared beverages and poor health outcomes, including obesity, diabetes, and heart disease.25–28 By phase 2, the cafeteria sold 238 fewer red beverages per day and 190 fewer regular sodas. Although our study does not examine individual-level data, significant changes in the beverage habits of employees who visit the cafeteria regularly could translate into health benefits over time.
A limitation of this study is that there was no control cafeteria. However, we were able to compare sales data for some items at 2 on-site cafeterias that had no intervention, and the changes in the intervention cafeteria were significantly different from those of the comparison cafeterias. We were not able to create a washout period after phase 2 to assess the effectiveness of a choice architecture–only intervention because the changes to the menu boards and displays in the cafeteria for the Choose Well, Eat Well program were designed as permanent changes to the cafeteria. Another limitation to this study is that we could not assess longitudinal change for individuals over time.
This study demonstrated the effectiveness of a labeling and choice architecture intervention in promoting healthy food and beverage choices in a large hospital cafeteria. Without changing the price or selection, we saw significant increases in healthy choices that were sustained over a 6-month period. Our results suggest that a simple information-based nutrition intervention is effective and is enhanced by an additional intervention that takes decision biases into account. In the future, these types of interventions could be integrated with menu calorie labeling to improve the reach and effectiveness of this policy.
Acknowledgments
Harvard Clinical and Translational Science Center, National Center for Research Resources (grant 1 UL1 RR025758-03) and the National Heart, Lung, and Blood Institute (grant 1 K23HL93221 to A. N. T.) supported this project.
We thank Emily Gelsomin, RD, LDN, for her contribution to the design and implementation of the food-labeling system. We also thank the entire staff of the Massachusetts General Hospital Eat Street Café for their hard work, cooperation, and enthusiasm during the study.
The results of the article were presented at the American Heart Association Nutrition, Physical Activity, and Metabolism and Cardiovascular Epidemiology and Prevention 2011 Scientific Sessions in Atlanta, Georgia, March 24, 2011.
Note. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Human Participant Protection
The Partners Human Research Committee deemed this study exempt from institutional review board review per the regulations found at 45 CFR 46.101(b) (2), including observation of public behavior.
References
- 1.Center for Science in the Public Interest Anyone's Guess: The Need for Nutrition Labeling at Fast-Food and Other Chain Restaurants. Washington, DC; November 2003. Available at: http://www.cspinet.org/restaurantreport.pdf. Accessed December 14, 2010 [Google Scholar]
- 2.Pereira MA, Kartashov AI, Ebbeling CBet al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365(9453):36–42 [DOI] [PubMed] [Google Scholar]
- 3.Berman M, Lavizzo-Mourey R. Obesity prevention in the information age: caloric information at the point of purchase. JAMA. 2008;300(4):433–435 [DOI] [PubMed] [Google Scholar]
- 4.Kumanyika SK, Obarzanek E, Stettler Net al. American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation. 2008;118(4):428–464 [DOI] [PubMed] [Google Scholar]
- 5.Kuo T, Jarosz CJ, Simon P, Fielding JE. Menu labeling as a potential strategy for combating the obesity epidemic: a health impact assessment. Am J Public Health. 2009;99(9):1680–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pomeranz JL, Brownell KD. Legal and public health considerations affecting the success, reach, and impact of menu-labeling laws. Am J Public Health. 2008;98(9):1578–1583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ludwig DS, Brownell KD. Public health action amid scientific uncertainty: the case of restaurant calorie labeling regulations. JAMA. 2009;302(4):434–435 [DOI] [PubMed] [Google Scholar]
- 8.Stein K. A national approach to restaurant menu labeling: the Patient Protection and Affordable Health Care Act, section 4205. J Am Diet Assoc. 2010;110(9):1280–1286 [DOI] [PubMed] [Google Scholar]
- 9.Nestle M. Health care reform in action—calorie labeling goes national. N Engl J Med. 2010;362(25):2343–2345 [DOI] [PubMed] [Google Scholar]
- 10.Krukowski RA, Harvey-Berino J, Kolodinsky J, Narsana RT, Desisto TP. Consumers may not use or understand calorie labeling in restaurants. J Am Diet Assoc. 2006;106(6):917–920 [DOI] [PubMed] [Google Scholar]
- 11.Rothman RL, Housam R, Weiss Het al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31(5):391–398 [DOI] [PubMed] [Google Scholar]
- 12.Harnack LJ, French SA. Effect of point of purchase calorie labeling on restaurant and cafeteria food choices: a review of the literature. Int J Behav Nutr Phys Act. 2008;551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bassett MT, Dumanovsky T, Huang Cet al. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am J Public Health. 2008;98(8):1457–1459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pulos E, Leng K. Evaluation of a voluntary menu-labeling program in full-service restaurants. Am J Public Health. 2010;100(6):1035–1039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. Am J Public Health. 2010;100(2):312–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Downs JS, Loewenstein G, Wisdom J. Strategies for promoting healthier food choices. American Economic Review: Papers & Proceedings. 2009;99(2):159–164 [DOI] [PubMed] [Google Scholar]
- 17.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: a first look at the effects on low-income people in New York City. Health Aff (Millwood). 2009;28(6):w1110–w1121 [DOI] [PubMed] [Google Scholar]
- 18.Finkelstein EA, Strombotne KL, Chan NL, Krieger J. Mandatory menu labeling in one fast-food chain in King County, Washington. Am J Prev Med. 2011;40(2):122–127 [DOI] [PubMed] [Google Scholar]
- 19.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298(20):2415–2417 [DOI] [PubMed] [Google Scholar]
- 20.Blumenthal K, Volpp KG. Enhancing the effectiveness of food labeling in restaurants. JAMA. 2010;303(6):553–554 [DOI] [PubMed] [Google Scholar]
- 21.Thaler RH, Sunstein CR. Nudge: Improving Decisions About Health, Wealth, and Happiness. New York: Penguin Group; 2009 [Google Scholar]
- 22.Thaler RH, Benartzi S. Save More Tomorrow: Using behavioral economics to increase employee saving. J Polit Econ. 2004;112(1):S164–S187 [Google Scholar]
- 23.Johnson EJ, Goldstein D. Medicine. Do defaults save lives? Science. 2003;302(5649):1338–1339 [DOI] [PubMed] [Google Scholar]
- 24.United States Department of Agriculture Dietary Guidelines for Americans; 2005Available at: http://www.choosemyplate.gov. Accessed June 11, 2009
- 25.Brownell KD, Farley T, Willett WCet al. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med. 2009;361(16):1599–1605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among US adults: 1988–1994 to 1999–2004. Am J Clin Nutr. 2009;89(1):372–381 [DOI] [PubMed] [Google Scholar]
- 27.Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121(11):1356–1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33(11):2477–2483 [DOI] [PMC free article] [PubMed] [Google Scholar]