Abstract
Recent ESC/EACTS revascularization guidelines advocate a ‘Heart Team’ (HT) approach in the decision-making process when managing patients with coronary disease. We prospectively assessed HT decision-making in 150 patients analysing personnel attendance, data presented, the ‘actioning’ of the HT decision and, if not completed, then the reasons why. Additionally, 50 patients were specifically re-discussed after 1 year in order to assess consistency in decision-making. We have two HT meetings each week. At least one surgeon, interventional cardiologist and non-interventional cardiologist were present at all meetings. Data presented included patient demographics, symptoms, co-morbidities, coronary angiography, left ventricular function and other relevant investigations, e.g. echocardiograms. HT decisions included continued medical treatment (22%), percutaneous coronary intervention (PCI; 22%), coronary-artery bypass grafting (CABG; 34%) or further investigations such as pressure wire studies, dobutamine stress echo or cardiac magnetic resonance imaging (22%). These decisions were fully undertaken in 86% of patients. Reasons for aberration in the remaining 21 patients included patient refusal (CABG 29%, PCI 10%) and further co-morbidities (28%). On re-discussion of the same patient data (n = 50) a year later, 24% of decisions differed from the original HT recommendations reflecting the fact that, for certain coronary artery disease pattern, either CABG or PCI could be appropriate.
Keywords: Heart team meeting, Transparent decision-making
INTRODUCTION
Coronary artery disease (CAD) is the most common cause of death in Europe, accounting for 1.92 million deaths each year. Overall, CAD is estimated to cost the EU economy 49 billion euros per year [1]. This represents a significant workload to clinicians specializing in coronary revascularization. At the start of this century, there was a significant increase in percutaneous coronary intervention (PCI) while the rate of coronary-artery bypass grafting (CABG) was declining, a practice which was not entirely evidence-based. This probably reflected the fact that the cardiologists were the gate-keepers and that there was no multi-disciplinary team (MDT; cardiologist, surgeon, patient) discussion for the patient's best management. However, the landmark Syntax trial [2] and the recent ESC/EACTS guidelines on coronary revascularization [3] have provided some evidence and guidance for better decision-making and improved patient's treatment.
ESC/EACTS guidelines published in 2010 have recommended for the first time a ‘Heart Team’ (HT) approach for making decisions regarding myocardial revascularization [3]. The MDT approach to decision-making has widely been adopted for the management of not only cancers but also a number of benign and medical chronic diseases [4–6]. The suggested benefits of these meetings include increased patient continuity of care, good communication between teams and a valuable opportunity for teaching. Unfortunately, there are no data on MDTs for patients with CAD.
AIM
An HT approach to the management of patients with CAD has been adopted for over 5 years in our unit. Our aim in this study was to evaluate our practice by analysing the decision-making process, patient outcome and the reproducibility of the decisions taken.
METHODS
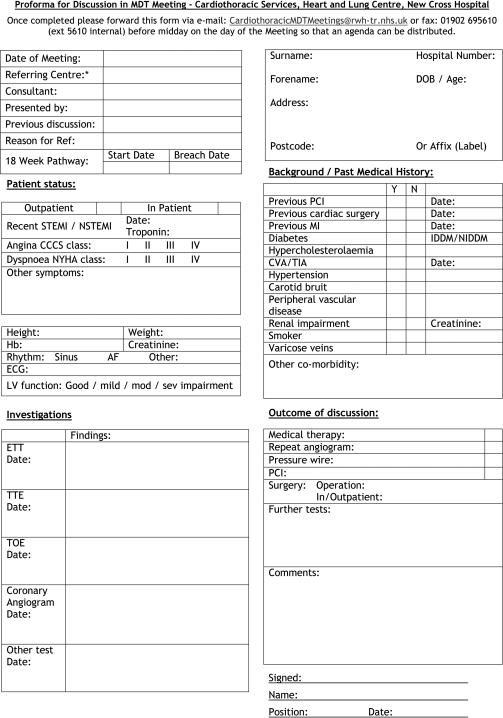
Two HT meetings are held weekly at our tertiary referral coronary/cardiac surgery unit. At least one cardiac surgeon, one interventional cardiologist and one non-interventional cardiologist are present at each meeting. The meeting is chaired by a consultant (cardiac surgeon or cardiologist) and the decisions are documented by the MDT co-ordinator. Meetings are also attended by junior medical and surgical staff and other related health professionals such as interventional radiologists and cardiac anaesthetists. There is an MDT proforma which is filled-in prior to the meeting, so that the relevant data are at hand during the meeting (Fig. 1).
Figure 1:
MDT proforma for patient's data presentation.
All patients with CAD potentially requiring coronary revascularization by PCI or CABG and discussed at MDT meeting at our centre between February 2010 and May 2010 (n = 150) were included. Their prospectively gathered data were analysed as was the implementation of the decisions. Fifty of these patients were randomly selected to be re-presented with the same data 1 year after first being discussed; data regarding decisions were again prospectively collected.
Data are expressed as median (range) and percentages.
RESULTS
There are 700 elective cardiac catheterizations, 1650 PCI and 800 CABGs performed at our unit annually.
In 2010, 848 patients were discussed at the HT meeting, a mean of nine patients per meeting. Of the 150 patients included during the study period, 22% were females. The median numbers of surgeons and cardiologists present at each meeting were 2 (1 to 4) and 4 (1 to 8), respectively. A surgeon was the chair of the meeting for 47% of patients' discussions, while a cardiologist did so for the remaining 53% HT meetings.
Decisions taken included medical management (22%), PCI (22%), CABG (34%) or further investigations such as review of symptoms at a post myocardial infarct clinic, pressure wire studies (PWSs), dobutamine stress echo (DSE) or cardiac magnetic resonance imaging (MRI) in 22%.
For those who required further investigations, three patients underwent DSE and thereafter further HT discussion, they were managed medically. Another three patients underwent cardiac MRI with two of them being referred for CABG while the third died during his hospital stay. Twelve patients underwent PWS and were thereafter treated medically (n = 3), with PCI (n = 7) or CABG (n = 2).
HT decisions were carried out in 86% of patients. Reasons for aberration in the remaining 21 patients included patient refusal (CABG 29%, PCI 10%), further initially unrecognized co-morbidities (28%), different vessels revascularized (9%) or other reasons (24%) that were not clear from the medical records.
Of the 50 patients re-discussed at a later date, 24% of decisions (n = 12) differed from the original HT recommendations. This apparent aberration in the decision-making reflects the fact that the evidence to treat some CAD pattern with PCI, medical therapy or CABG was not very strong (level 2b evidence). One such example (Patient 2, Table 1) was a 58-year old with isolated blocked proximal LAD disease (retrograde filling) where at the initial HT meeting the decision was for LIMA to LAD but on re-presenting his data a year later the HT felt that PCI to LAD would be equally effective (Table 1).
Table 1:
Data of patients who had a different decision at re-presentation
| Patient | Coronary pathology | LV function | Initial HT decision | Re-discussion HT decision |
|---|---|---|---|---|
| 1 | Blocked RCA, proximal LAD >50% | Good | CABG | PCI |
| 2 | Blocked, retrograde filling LAD | Good | CABG | PCI |
| 3 | Mid LAD disease | Moderate | DSE | Medical Rx |
| 4 | RCA and LAD disease, ?50% Cx | Good | PWS | CABG |
| 5 | LAD in-stent stenosis, ?40% | Good | PWS | PCI |
| 6 | ?50% OM disease | Good | PWS | Medical Rx |
| 7 | Blocked RCA, ?50% Cx and LAD disease | Good | PWS | CABG |
| 8 | Significant RCA disease, LAD ?50% | Good | PWS | PCI |
| 9 | Blocked RCA, LAD ?50% | Good | PWS | Medical Rx |
| 10 | ?50% LAD | Good | Medical Rx | PWS |
| 11 | Blocked RCA, Diffuse LAD and OM disease | Good | PCI | Medical Rx |
| 12 | Dominant Cx, Diffuse OM disease, small LAD | Good | PCI | Medical Rx |
RCA: right coronary artery; LAD: left anterior descending artery; Cx: circumflex artery; OM: obtuse marginal artery; CABG: coronary artery bypass grafting; PCI: percutaneous coronary intervention; DSE: dobutamine stress echo; PWS: pressure wire study; Medical Rx: medical treatment; ?: possibly/approximately.
DISCUSSION
There was a recent report concerning a patient who had 67 stents within his coronary tree [7]. Although this is not the norm, but no doubt feasible, it raises some concern about the appropriateness of this management approach. It could well be that an HT approach for this patient would have been better.
The EACTS/ESC guidelines provide with evidence-based decision-making process for various types of coronary pathology in terms of their optimal treatment and also recommend the HT approach to making decisions regarding coronary revascularization [3].
The HT approach is the equivalent of a medical MDT meeting that is extensively used in the management of cancer patients. Its remit has now been extended to the management of patients with diabetes, stoke and chronic obstructive pulmonary disease [4]. Although there are no randomised control trials to confirm the benefit of MDTs, these meetings provide an evidence-based approach to decision-making. They also ensure a better team working, co-ordinated patient care and provide a great platform for education and training [4].
The necessity for a cardiac MDT or an HT approach is further consolidated by (a) the recent publication by Hannan et al. [8] and (b) the report by Lee et al. [9]. The latter conducted a survey of patient's perception about why PCI was carried out. One-third of the patients thought that their treatment was an emergency despite the PCI being carried out as an elective procedure. Two-thirds thought that the PCI would prolong their life with just under half thinking that it has saved their lives. These attitudes certainly reflect a misinformation for the patients. Hannan et al. [8] showed that if a cardiologist felt that the patient would benefit from PCI, then in 94% of patients a PCI was carried. On the other hand, if a cardiologist (interventional no doubt) felt that the patient would benefit from CABG, then only 53% of patients actually underwent CABG.
Although the HT is a relatively new concept, we have been practising this approach for over 5 years. Our assessment has shown that this approach is reproducible and offers transparency in the decision-making process for revascularizing patients with CAD. This transparency in showing how a management plan has been reached is the key benefit of the multi-disciplinary process, and is arguably more important than the actual decision itself, whether it be PCI, CABG or medical management.
A multi-disciplinary approach to patient management has been a key part in the management of patients with oncological problems for several years. We have set up our HT meetings from the experience gained from these cancer MDTs. Hence, the meetings are held at set times during the week and in a dedicated room. Patients' data are gathered prior to the meeting on a set proforma sheet so that time is not wasted during the meeting to look through patient records. All relevant investigations are also brought to the meeting and uploaded on the system prior to the start. All relevant specialists dedicate time to attend and a coordinator ensures that all the paper works and investigations are in order, as well as documenting the decision taken during the meeting.
Although the HT approach has been successfully adopted in our practice, we presume that it is still sporadic in the UK and possibly, non-existent in Europe and North America as there has been no previous report relating to an HT approach in the literature. The success of the implementation of an HT meeting resides in the (a) willingness of both cardiologist and cardiac surgeons to offer the best possible (evidence-based) treatment to patients with CAD, (b) dedicated time within the schedule of work to hold these meetings regularly and (c) the personnel and other support back-up to ensure smooth running of the meetings.
Although there was a different decision reached at the re-discussion of 24% of the 50 patients re-discussed after a year, this merely reflects the fact that there is variable strength of the evidence (level 1a to level 3) [3] available for the treatment of various CAD pattern. Moreover, it may also have reflected the increased level of experience that would have been acquired a year later and this is exemplified by ‘Patient 2’ in Table 1.
We are hoping to make our HT process even more robust with the introduction of an electronic MDT database. This is currently being evaluated and will provide an improved way to record the relevant information for discussion at the meeting, the decisions made and the carrying out of these decisions. The Syntax score [10] and EuroSCORE [11] could also be incorporated within the e-HT meetings, thus improving the decision-making process. The inclusion of the Syntax score may provide a guide as to which patients are more likely to benefit from CABG, i.e. Syntax score >33. Likewise, if the EuroSCORE is prohibitively high, then a PCI option might be favoured. An e-system will also allow for easier prospective assessment of the practice and constant monitoring of outcomes.
Last but not the least, a further step could be considered where the patients attend their own discussion at the MDT meeting; their wishes directly communicated with interaction in the decision-making process of their illness. However, this will require a different set up and an enormous amount of coordination between surgeons, cardiologists and patients.
CONCLUSION
An HT approach to decision-making provides transparency for decision-making in the treatment of patients with CAD. It is a robust and usually reproducible process. Decision could be strengthened with the inclusion of Syntax score and EuroSCORE.
ACKNOWLEDGEMENT
We would like to acknowledge the contribution of all the cardiac surgeons and cardiologists (local and visiting) who work at the Heart & Lung Centre, Wolverhampton as well as our Heart Team coordinator (Emma Morris).
Conflict of interest: none declared.
APPENDIX. Conference Discussion
Dr S. Head (Rotterdam, Netherlands): I'm a big fan of the Heart Team, I would say. But how do you consider patients in whom the cardiologist performs an angiography and then, for instance, sees that the lesions would be perfect for stenting? Do you “take the patients off the table”, put them before the Heart Team, and then re-discuss them, or do you also sometimes stent them straight away?
Dr Long (Wolverhampton, UK): No, all those patients are discussed by the Heart Team. And even if a cardiologist believes that a lesion should be treated with a PCI, we bring the patient to the Heart Team for discussion with the group, with the surgeons, so that the case is discussed by all colleagues. Data was presented at the Postgraduate Meeting yesterday, from Hannan and the survey of cardiologists published in Circulation, that showed that if a cardiologist believed a lesion should be treated with a PCI and the patient didn't go through the Heart Team, over 95% of those patients would get PCI. If, after the angiography, the cardiologist thought the patient potentially should be referred for surgery, only 50% of those patients ended up being referred for surgery. So I think this is where the Heart Team is very important.
Dr Head: I do have a second question about reproducibility of the Heart Team. You re-evaluated 50 patients. Have you also considered sending these 50 patients to another centre to see what the reproducibility would be between centres, or do you only look at it within your own centre?
Dr Long: I think that's a good idea. Not many other centres have a Heart Team set up with recognized scheduled time each week, with it being a formal part of the cardiologists' and the cardiac surgeons' week. But potentially that's something that we could do in the future.
Dr G. Wimmer-Greinecker (Bad Bevensen, Germany): May I ask you two questions. First of all, how do you deal with patients that come from other referring cardiologists? Do you discuss them in your Heart Team, or do you have an external Heart Team for them?
Dr Long: We discuss them at our Heart Team meeting. We have visiting cardiologists from other units.
Dr Wimmer-Greinecker: And that is accepted by the referring cardiologists?
Dr Long: Absolutely.
Dr Wimmer-Greinecker: And the second thing is, can you tell us something about the size of your Cardiology group? I mean, you said you have two discussion rounds every week.
Dr Long: Yes.
Dr Wimmer-Greinecker: So when are they scheduled, e.g. Monday and Thursday?
Dr Long: Wednesday and Friday, two hours.
Dr Wimmer-Greinecker: Wednesday and Friday. So if a patient comes in on Friday, his case would be discussed on Wednesday of the next week. So all those patients are discharged again, and there is no problem from the reimbursement point of view if you readmit them to the hospital? Are you planning in the future that you might have a Heart Team discussion every day with a slightly smaller team?
Dr H. Luckraz (Wolverhampton, United Kingdom): I am one of the authors of the paper. I'll probably answer this question for you. In the UK, obviously, reimbursement doesn't really come into it in terms of admission and discharge and readmission. For most of these patients who come in after the MDT discussion on a Friday, i.e., Friday afternoon until Wednesday morning, if they come in with an NSTEMI, their culprit lesion is dealt with by the cardiologist, and then the patient is stabilized in the cardiology ward, so then we have the time to discuss those patients at the Wednesday meeting. On the other hand, if a patient just came in with unstable angina and had an angiogram, he'd get discharged home, we'd discuss his case, and then he would come to the outpatient clinic to be reviewed by the speciality with which the final decision lay.
Dr T. Kieser (Calgary, AB, Canada): I was just curious how you managed the logistics of getting surgeons there, because they're always operating. How many surgeons do you have and what time of day?
Dr Long: There are six cardiac surgeons in our unit. And on each of the days, three of the surgeons are operating. But the referrals from the cardiologists are to a group of surgeons, they work together, and so even if they're unable to attend every meeting, they will attend during the week.
Dr Kieser: That's good. I think, too, this Heart Team takes the stress off the individual team member. Nobody makes the final decision, it's sort of “spread the blame”, but, you know, it's what we all should be doing for the patient.
REFERENCES
- 1.Allender S, Scarborough P, O'Flaherty M, Capewell S. Patterns of coronary heart disease mortality over the 20th century in England and Wales: possible plateaus in the rate of decline. BMC Public Health. 2008;8:148. doi: 10.1186/1471-2458-8-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kappetein AP, Feldman TE, Mack MJ, Morice MC, Holmes DR, Ståhle E, et al. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J. 2011;32:2125–34. doi: 10.1093/eurheartj/ehr213. [DOI] [PubMed] [Google Scholar]
- 3.Taggart DP, Boyle R, de Belder MA, Fox KA. The 2010 ESC/EACTS guidelines on myocardial revascularisation. Heart. 2011;97:445–6. doi: 10.1136/hrt.2010.216135. [DOI] [PubMed] [Google Scholar]
- 4.Taylor C, Munro A, Glynne-Jones R, Griffith C, Trevatt P, Richards M, et al. Multidisciplinary team working in cancer: what is the evidence? Br Med J. 2010;340:c951. doi: 10.1136/bmj.c951. [DOI] [PubMed] [Google Scholar]
- 5.Lamb BW, Brown KF, Nagpal K, Vincent C, Green JS, Sevdalis N. Quality of care management decisions by multidisciplinary cancer teams: a systematic review. Ann Surg Oncol. 2011;18:2016–25. doi: 10.1245/s10434-011-1675-6. [DOI] [PubMed] [Google Scholar]
- 6.Langhorne P, Pollock A. What are the components of effective stroke unit care? Age Ageing. 2002;31:365–71. doi: 10.1093/ageing/31.5.365. [DOI] [PubMed] [Google Scholar]
- 7.Khouzam RN, Dahiya R, Schwartz R. A heart with 67 stents. J Am Coll Cardiol. 2010;56:1605. doi: 10.1016/j.jacc.2010.02.077. [DOI] [PubMed] [Google Scholar]
- 8.Hannan E, Racz MJ, Gold J, Cozzens K, Stamato NJ, Powell T, et al. Adherence of catheterization laboratory cardiologists to American College of Cardiology/American Heart Association Guidelines for percutaneous coronary interventions and coronary artery bypass graft surgery: what happens in actual practice? Circulation. 2010;121:267–75. doi: 10.1161/CIRCULATIONAHA.109.887539. [DOI] [PubMed] [Google Scholar]
- 9.Lee JH, Chuu K, Spertus J, O'Keefe JH. Widespread patient misconceptions regarding the benefits of elective percutaneous corornary intervention. Circulation. 2008;118:S1161. [Google Scholar]
- 10.Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, et al. The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroInterv. 2005;1:219–27. [PubMed] [Google Scholar]
- 11.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16:9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]