Abstract
The aim of this retrospective study was to evaluate factors potentially influencing short- and long-term mortality in patients who had a non-traumatic lower limb amputation in a university hospital. A consecutive series of 93 amputations (16% toe/foot, 33% trans-tibial, 9% through knee and 42% trans-femoral) were studied. Their mean age was 75.8 years; 21 (23%) were admitted from a nursing home and 87 (92%) were amputated due to a vascular disease and/or diabetes. Thirty days and 1-year mortality were 30 and 54%, respectively. Cox regression analysis demonstrated that the 30-day mortality was associated with older age (P = 0.01), and the number of co-morbidities (P = 0.04), when adjusted for gender, previous amputations, cause of and amputation level, and residential status. Thus, a patient with 4 or 5 co-morbidities (n = 20) was seven times more likely to die within 30 days, compared with a patient with 1 co-morbidity (n = 16). Further, the risk of not surviving increased with 7% per each additional year the patient got older. Of concern, almost one-third of patients died within 1 month. This may be unavoidable, but a multidisciplinary, optimized, multimodal pre- and postoperative programme should be instituted, trying to improve the outcome.
Keywords: Amputation, Lower limb, Survival, Fatal outcome
INTRODUCTION
Having a lower limb amputation is associated with a somehow high risk of not surviving within the first year from surgery, with perioperative mortality ranging from 9 to 16% [1–5], and 1-year survival rates ranging from 86 to 53% [1–10]. The majority of non-traumatic amputations are most often caused by a vascular disease, followed by diabetes or a combination of both [1, 4, 5, 7–9], whereas worse survival rates have been associated with factors such as older age, diabetes, more than one co-morbidity, above knee amputations (AKAs), type of rehabilitation setting and the post-amputation physical independence grade [1, 3, 6, 8, 11, 12]. Still, other studies found no difference between amputation levels and 1-year mobility [2] or mortality [5], and diabetic amputees seem less likely to die within 1-year than dysvascular amputees [7].
When planning to optimize the treatment and rehabilitation of all patients with lower limb amputations, it seems important to identify whether special attention should be taken into account for subgroups. To this, the ultimate outcome of all patient groups including amputee patients is survival rates.
The aim of this study was to evaluate the factors potentially influencing short- and long-term survival rates of patients with a non-traumatic lower limb amputation.
MATERIALS AND METHODS
All patients who underwent a non-traumatic lower limb amputation in the year 2009 at Hvidovre University Hospital, Copenhagen, Denmark, were identified from the hospitals’ database of surgery.
Medical records were reviewed retrospectively, and data were stratified according to age, gender, residential status (own home or nursing home), previous amputations in the contra-lateral limb, indications for amputation (vascular disease, diabetes, vascular disease and diabetes as well as emboli), number of co-morbidities (0–1, 2–3 and 4–5), American Society of Anesthesiologists (ASA, 0–5) rating [13], amputation level (foot/toe, below knee amputation (BKA), through knee amputation (TKA) and AKA), in-hospital mortality, cause of death (if stated in medical charts) and length of stay in days. Mortality, within 30 and 90 days, in addition to 12 months from surgery were identified from the national civil register. The institutional ethics committee approved the study.
STATISTICAL ANALYSIS
Chi square and ANOVA were used to evaluate the differences between patient characteristics and the level of amputation and mortality within 30 days and 1 year from amputation. Kaplan–Meyer survival graphs were derived for age groups (43–76 versus 77–93 years) and co-morbidity groups. Cox regression analysis (enter method) was used to assess the relationship between the survival and the potentially associated factors. Age was entered as a continuous variable, while reference categories for other variables in the Cox regression were: women, admitted from own home, 0–1 co-morbidities, no previous amputation, amputation related to diabetes and foot/toe amputation. The ASA rating was not included in this analysis due to the possible multicolinearity with the number of co-morbidities.
All analyses were preformed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA). Data are presented as mean (standard deviation), continues data being normally distributed, or as number (percentage) for categorical data, and the level of significance was set at P < 0.05.
RESULTS
Ninety-three of the 95 consecutive lower limb amputations in the study year were caused by a non-traumatic diagnosis. The mean age of the 93 patients was 75.8 (11.4) years, and ranging from 43 to 93 years. Twenty-one (23%) patients were admitted from a nursing home, 20 (22%) were referred from a department of vascular surgery, 5 (5%) from a wound-healing centre, 8 (9%) from other hospital departments and 39 (42%) came from their home. The reason for amputation was gangrene (n = 66), non-healing wounds /infection (n = 18) or other causes n = 9). The distribution of amputation level was, respectively, foot/toe (n = 15), BKA (n = 31), TKA (n = 8) and AKA (n = 39), with a significantly higher proportion of patients admitted from an institution having a TKA or AKA when compared with patients admitted from their own home (P = 0.003). Patients who had a TKA amputation stayed significantly fewer days in the orthopedic ward when compared with patients with other amputations (P = 0.03), otherwise no significant differences were seen between the amputation level and patient characteristics (Table 1). One patient had no co-morbidities, 15 had 1, 57 had 2–3 and 20 had 4–5 co-morbidities. The mortality was 27% in hospital, 30% at 30 days, 44% at 90 days and 54% at 1 year, respectively. Three patients with an ASA of 5 died within 5 days from surgery. Univariate analysis demonstrated that the 30-day mortality was associated with older age, residential status (nursing home), more co-morbidities and the ASA rating (P ≤ 0.04), and except for the number of co-morbidities (P = 0.07), the 1-year mortality was significantly associated with the same variables (Table 2).
Table 1:
Characteristics and outcome of 93 consecutive lower limb amputee patients
| Variable | All (n = 93) | Amputation level |
P-value | |||
|---|---|---|---|---|---|---|
| Foot/toe (n = 15) | BKA (n = 31) | TKA (n = 8) | AKA (n = 39) | |||
| Age | 75.8 (11.4) | 73.8 (14.5) | 73.9 (12.6) | 74.9 (12.5) | 78.2 (8.4) | 0.369 |
| Women | 38 (41) | 3 (8) | 13 (34) | 2 (5) | 20 (53) | 0.151 |
| Men | 55 (59) | 12 (22) | 18 (33) | 6 (11) | 19 (34) | |
| From own home | 72 (77) | 14 (19) | 28 (39) | 3 (4) | 27 (38) | 0.003 |
| From nursery home | 21 (23) | 1 (5) | 3 (14) | 5 (24) | 12 (57) | |
| No previous amputation other limb | 75 (81) | 14 (19) | 25 (33) | 6 (8) | 30 (40) | 0.561 |
| Previous amputation contra lateral limb | 18 (19) | 1 (6) | 6 (33) | 2 (11) | 9 (50) | |
| Amputation due to | ||||||
| Vascular disease | 48 (52) | 7 (15) | 16 (33) | 5 (10) | 20 (42) | 0.955 |
| Diabetes mellitus (DM) | 17 (18) | 4 (24) | 5 (29) | 1 (6) | 7 (41) | |
| Vascular disease + DM | 22 (24) | 4 (18) | 7 (32) | 2 (9) | 9 (41) | |
| Emboli | 6 (6) | 0 | 3 (50) | 0 | 3 (50) | |
| Number of co-morbidities | ||||||
| 0–1 co-morbidities | 16 (17) | 2 (12) | 6 (38) | 1 (6) | 7 (44) | 0.966 |
| 2–3 co-morbidities | 57 (61) | 10 (17) | 20 (35) | 5 (9) | 22 (39) | |
| 4–5 co-morbidities | 20 (22) | 3 (15) | 5 (25) | 2 (10) | 10 (50) | |
| ASA score = 2 | 24 (26) | 5 (21) | 11 (46) | 0 | 8 (33) | 0.446 |
| ASA score = 3 | 58 (62) | 9 (16) | 17 (29) | 7 (12) | 25 (43) | |
| ASA score = 4 | 8 (9) | 0 | 3 (37) | 1 (13) | 4 (50) | |
| ASA score = 5 | 3 (3) | 1 (33) | 0 | 0 | 2 (67) | |
| Length of stay | 28.1 (22.3) | 32.8 (28.4) n = 11 | 35.4 (24.7) n = 24 | 8.5 (2.8) n = 6 | 24 (16.4) n = 27 | 0.032 |
BKA, below knee amputation; TKA, through knee amputation; AKA, above knee amputation; ASA, American Society of Anesthesiologists rating (1–5); 0, none. Categorical variables evaluated with chi square and continuous data with ANOVA. Data are presented as mean (standard deviation) or as number (percentage).
Table 2:
Univariate analysis of factors influencing short- and long-term mortality
| Variable | All, N = 93 | 30-day mortality | P- value | 1-year mortality | P-value |
|---|---|---|---|---|---|
| Age 43–76 years | 47 | 9 (19) | 0.020 | 20 (43) | 0.028 |
| Age 77–93 years | 46 | 19 (41) | 30 (65) | ||
| Women | 38 | 12 (32) | 0.797 | 22 (58) | 0.507 |
| Men | 55 | 16 (29) | 28 (51) | ||
| Admitted from own home | 72 | 17 (24) | 0.011 | 37 (51) | 0.395 |
| Admitted from nursery home | 21 | 11 (52) | 13 (62) | ||
| No previous amputation contra lateral limb | 75 | 22 (29) | 0.740 | 41 (55) | 0.721 |
| Previous amputation contra lateral limb | 18 | 6 (33) | 9 (50) | ||
| Indications for amputation | |||||
| Vascular disease | 48 | 11 (23) | 0.145 | 26 (54) | 0.435 |
| Diabetes mellitus (DM) | 17 | 5 (29) | 9 (53) | ||
| Vascular disease + DM | 22 | 8 (36) | 10 (46) | ||
| Emboli | 6 | 4 (67) | 5 (83) | ||
| 0–1 co-morbidities | 16 | 2 (13) | 0.044 | 5 (31) | 0.067 |
| 2–3 co-morbidities | 57 | 16 (28) | 31 (54) | ||
| 4–5 co-morbidities | 20 | 10 (50) | 14 (70) | ||
| ASA score = 2 | 24 | 8 (21) | 0.006 | 9 (38) | 0.032 |
| ASA score = 3 | 58 | 15 (26) | 31 (53) | ||
| ASA score = 4 | 8 | 5 (63) | 7 (88) | ||
| ASA score = 5 | 3 | 3 (100) | 3 (100) | ||
| Amputation level | |||||
| Foot/toe | 15 | 3 (20) | 0.521 | 6 (40) | 0.655 |
| Trans tibial | 31 | 9 (29) | 18 (58) | ||
| Through the knee | 8 | 4 (50) | 5 (63) | ||
| Trans femoral | 39 | 12 (31) | 21 (54) | ||
Categorical variables evaluated with chi square analysis. Data are presented as number (percentage).
The cause of death for patients who died within 1 month was cardiovascular (n = 14, 50%) and respiratory (n = 6, 21%) problems, while one death was related to an endocrinology disease. The cause of death for three patients who died in-hospital was not stated in the medical chart. In addition, four patients who died after discharge had no cause of death mentioned. Patients admitted from a nursing home were significantly older (mean age 80.6 versus 74.4 years) and discharged after fewer days in the ward (mean 7.4 (2.2) versus 33.9 (22.0) days) (P < 0.03), but with no significant differences regarding ASA ratings and the number of co-morbidities when compared with patients admitted from their own home (P > 0.3). Eleven patients (12%) had a revision (n = 4) or a re-amputation (n = 7) within 30 days from amputation, with six of the re-amputations having a toe/foot amputation as the index operation. None of the 25 patients initially referred from a vascular surgeon or a wound-healing centre were re-amputated, and only one index amputation due to non-healing wounds or infection had a re-amputation. Having a revision or re-amputation was not associated with a higher 30-, 90-day or 1-year mortality (P > 0.2), and there was no significant difference in mortality between patients who were amputated due to a vascular disease or emboli (n = 54) compared with those with diabetes (n = 39), at 30, 90 days or 1 year (P > 0.4).
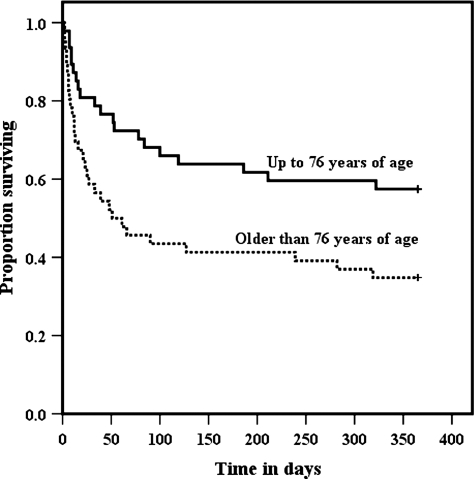
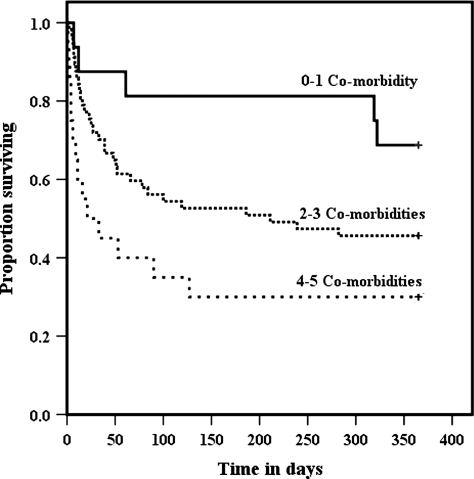
Cox regression analysis demonstrated that the 30-day survival was associated with older age (P = 0.01), and more than three co-morbidities (P = 0.04), when adjusted for gender, residential status, previous amputation, indication for the index amputation and the amputation level (Table 3). A similar result was seen for regression analysis of the 1-year survival (Table 4). One-year Kaplan–Meier survival graphs for age- and co-morbidity groups are presented in Figs. 1 and 2.
Table 3:
Association with 30-day survival
| Variables | Hazard ratio Exp (B) | 95% CI for Exp (B) |
P-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 1.069 | 1.016 | 1.125 | 0.010 |
| Men | 1.255 | 0.529 | 2.975 | 0.607 |
| Admitted from nursery home | 1.560 | 0.654 | 3.674 | 0.331 |
| 0–1 co-morbidities (reference) | ||||
| 2–3 co-morbidities | 2.158 | 0.475 | 9.805 | 0.319 |
| 4–5 co-morbidities | 5.879 | 1.136 | 30.413 | 0.035 |
| Previous amputation contra lateral limb | 1.073 | 0.412 | 2.795 | 0.886 |
| Amputation due to vascular disease or emboli | 0.822 | 0.336 | 2.008 | 0.667 |
| Foot/toe amputation (reference) | ||||
| Trans tibial | 1.598 | 0.421 | 6.069 | 0.491 |
| Through the knee | 2.975 | 0.574 | 15.428 | 0.194 |
| Trans femoral | 1.328 | 0.333 | 5.294 | 0.688 |
Table 4:
Association with 1-year survival
| Variables | Hazard ratio Exp (B) | 95% CI for Exp (B) |
P-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 1.047 | 1.013 | 1.082 | 0.006 |
| Men | 1.086 | 0.586 | 2.011 | 0.793 |
| Admitted from nursery home | 1.083 | 0.533 | 2.203 | 0.825 |
| 0–1 co-morbidities (reference) | ||||
| 2–3 co-morbidities | 2.310 | 0.876 | 6.088 | 0.090 |
| 4–5 co-morbidities | 4.703 | 1.596 | 13.860 | 0.005 |
| Previous amputation contra lateral limb | 0.912 | 0.426 | 1.950 | 0.811 |
| Amputation due to vascular disease or emboli | 1.136 | 0.594 | 2.172 | 0.700 |
| Foot/toe amputation (reference) | ||||
| Trans tibial | 1.887 | 0.733 | 4.857 | 0.188 |
| Through the knee | 2.567 | 0.730 | 9.029 | 0.142 |
| Trans femoral | 1.462 | 0.550 | 3.886 | 0.446 |
Figure 1:
Age groups and survival from the date of amputation.
Figure 2:
Co-morbidities and survival from the date of amputation.
DISCUSSION
The present study of 93 consecutive patients admitted from their own home or a nursing home within the year 2009 shows to our knowledge the lowest short- and long-term survival rates ever reported for lower limb non-traumatic amputations. The 30-days mortality was 30%, and more than half of the patients were dead at 1 year from amputation. The mortality was significantly related to age and pre-amputation morbidity. The regression analysis showed that the risk of not surviving 30 days from amputation was six times higher for a patient with 4–5 co-morbidities when compared with one with 0–1. The risk of not surviving more than 1 month increased with 7% per each additional year the patient got older. The corresponding figures for 1-year survival were five times (comorbidities) and 5% per year (age). None of the patients referred from a vascular surgeon were re-amputated, and only one out of seven initially amputated because of infection was re-amputated. This indicates that being referred from a vascular surgeon to some extent secure the right amputation level, and in infected patients the level of amputation was performed well above the infected area.
Some of these deaths probably are unavoidable due to age and the pre-amputation morbidity, e.g. ASA ratings of 4 and 5 (n = 11), having 4–5 co-morbidities (n = 20), with respectively short-term mortality rates of 73 and 50%, when compared with 21 and 13% in patients with ASA = 2 and 0–1 co-morbidity, respectively. It is considered agreeable that a patient with an ASA rating of 5 (indicating moribund status) should not go through surgery in the future, and that indications and guidelines of other high-risk amputee patients (ASA 4 and having 4–5 co-morbidities) should be carefully reviewed in view of the low survival rates. Still, we cannot exclude that the non-standardized perioperative treatment in the department actually influenced the survival rates negatively, the cause of death being cardiovascular or respiratory in 71% of patients. Thus, we have reason to believe that implementing a multidisciplinary and optimized perioperative regime, including a standardized fluid and transfusion protocol, supplemental oxygen when supine, enforced oral nutrition including supplementary protein drinks, pain management and intensive mobilization out of bed [14], in general, could reduce the high short-term mortality rates seen in these high-risk patients. Furthermore, it may be that the higher 30-day mortality rates (52%) of the 21 patients living in a nursing home pre-amputation could be reduced if not being discharged much sooner than other patients.
The treatment of patients with diabetes was also not standardized, but having diabetes had no significant influence on mortality rates when compared with other patients.
High 1-year mortality rates from 30 to 42% have been reported in previous studies [1, 3–7, 11], while much lower rates from 10 to 22% were reported in other studies [2, 8–10]. These differences may reflect different characteristics of study groups, exemplified by lower mean age in the above-mentioned studies in comparison with patients included in our study. Also, a Finnish study presenting 1-year mortality rates of 38% included trauma patients who lived longer than elderly vascular and diabetic patients undergoing amputation [11].
Still, the extremely high 30-day mortality of 30% seen in the present study is ∼20% higher than that reported in patient groups from the 1990s and up to the year 2005 [1–3, 5], and also much higher than the reports of 13.3% 30-days mortality rates from another consecutive series of even older patients with a hip fracture [15]. Younger age groups (mean 66.7–70.1 years) in these amputee studies when compared with 75.8 years in the present may again explain some of this fatal difference, indicating lengthy attempts to save the limb, possible with a longer period of severe illness. Still, our results regarding 1-year mortality are close to reports from a consecutive series of 174 patients who underwent primary major amputations in a Swedish study (47% mortality) in the late 1990s [4]. Actually these patients were the oldest reported (mean age 79.1 (10.6)), and following a multidisciplinary approach, but with almost half as many (16%) deaths within 30 days from amputation [4], when compared with patients in our series. Thus, it may be possible to reduce the high short-term mortality rates at our hospital.
A limitation of our retrospective analysis of factors influencing short- and long-term survival rates is that we were reliant on factors documented in the medical charts. As others [2], we were unable to include the pre-amputation mobility level of our study group, as this was not consistently reported in charts. Also, the cause of death was not available in 25% of the short-term mortalities. Still data regarding other important factors were complete, with mortality rates verified by the national civil register.
In conclusion, the short-term mortality rates of 30% in this consecutive series of lower limb amputations were the highest ever reported, and significantly influenced by older age and the severity of pre-amputation morbidity. More detailed analysis of the cause of mortality in a larger series, in addition to a multidisciplinary approach, should be instituted to describe and evaluate whether the number of these fatal events could be reduced.
Conflict of interest: none declared.
REFERENCES
- 1.Aulivola B, Hile CN, Hamdan AD, Sheahan MG, Veraldi JR, Skillman JJ, et al. Major lower extremity amputation: outcome of a modern series. Arch Surg. 2004;139:395–9. doi: 10.1001/archsurg.139.4.395. [DOI] [PubMed] [Google Scholar]
- 2.Basu NN, Fassiadis N, McIrvine A. Mobility one year after unilateral lower limb amputation: a modern, UK institutional report. Interact CardioVasc Thorac Surg. 2008;7:1024–6. doi: 10.1510/icvts.2008.180422. [DOI] [PubMed] [Google Scholar]
- 3.Feinglass J, Pearce WH, Martin GJ, Gibbs J, Cowper D, Sorensen M, et al. Postoperative and late survival outcomes after major amputation: findings from the Department of Veterans Affairs National Surgical Quality Improvement Program. Surgery. 2001;130:21–9. doi: 10.1067/msy.2001.115359. [DOI] [PubMed] [Google Scholar]
- 4.Johannesson A, Larsson GU, Oberg T. From major amputation to prosthetic outcome: a prospective study of 190 patients in a defined population. Prosthet Orthot Int. 2004;28:9–21. doi: 10.3109/03093640409167920. [DOI] [PubMed] [Google Scholar]
- 5.Lim TS, Finlayson A, Thorpe JM, Sieunarine K, Mwipatayi BP, Brady A, et al. Outcomes of a contemporary amputation series. ANZ J Surg. 2006;76:300–5. doi: 10.1111/j.1445-2197.2006.03715.x. [DOI] [PubMed] [Google Scholar]
- 6.Dillingham TR, Pezzin LE. Rehabilitation setting and associated mortality and medical stability among persons with amputations. Arch Phys Med Rehabil. 2008;89:1038–45. doi: 10.1016/j.apmr.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 7.Dillingham TR, Pezzin LE, Shore AD. Reamputation, mortality, and health care costs among persons with dysvascular lower-limb amputations. Arch Phys Med Rehabil. 2005;86:480–6. doi: 10.1016/j.apmr.2004.06.072. [DOI] [PubMed] [Google Scholar]
- 8.Kulkarni J, Pande S, Morris J. Survival rates in dysvascular lower limb amputees. Int J Surg. 2006;4:217–21. doi: 10.1016/j.ijsu.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 9.Nehler MR, Coll JR, Hiatt WR, Regensteiner JG, Schnickel GT, Klenke WA, et al. Functional outcome in a contemporary series of major lower extremity amputations. J Vasc Surg. 2003;38:7–14. doi: 10.1016/s0741-5214(03)00092-2. [DOI] [PubMed] [Google Scholar]
- 10.Schoppen T, Boonstra A, Groothoff JW, de VJ, Goeken LN, Eisma WH. Physical, mental, and social predictors of functional outcome in unilateral lower-limb amputees. Arch Phys Med Rehabil. 2003;84:803–11. doi: 10.1016/s0003-9993(02)04952-3. [DOI] [PubMed] [Google Scholar]
- 11.Pohjolainen T, Alaranta H. Ten-year survival of Finnish lower limb amputees. Prosthet Orthot Int. 1998;22:10–6. doi: 10.3109/03093649809164452. [DOI] [PubMed] [Google Scholar]
- 12.Stineman MG, Kurichi JE, Kwong PL, Maislin G, Reker DM, Vogel WB, et al. Survival analysis in amputees based on physical independence grade achievement. Arch Surg. 2009;144:543–51. doi: 10.1001/archsurg.2009.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24:111. [Google Scholar]
- 14.Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248:189–98. doi: 10.1097/SLA.0b013e31817f2c1a. [DOI] [PubMed] [Google Scholar]
- 15.Foss NB, Kehlet H. Mortality analysis in hip fracture patients: implications for design of future outcome trials. Br J Anaesth. 2005;94:24–9. doi: 10.1093/bja/aei010. [DOI] [PubMed] [Google Scholar]