Abstract
High LDL-cholesterol (LDL-C) characterizes familial hypercholesterolemia (FH) and familial combined hyperlipidemia (FCH). LDL-apheresis, used in these patients to reduce LDL-C levels, has been shown to also affect HDL levels and composition. We studied LDL-apheresis effects on six FH and nine FCH subjects’ serum capacity to modulate cellular cholesterol efflux, an index of HDL functionality, and to load macrophages with cholesterol. Serum cholesterol efflux capacity (CEC) and macrophage cholesterol loading capacity (CLC) were measured before, immediately after, and two days after LDL-apheresis. The procedure reduced total cholesterol (TC), LDL-C, and apoB plasma levels (−69%, −80% and −74%, respectively), parameters only partially restored two days later. HDL-C and apoA-I plasma levels, reduced after LDL-apheresis (−27% and −16%, respectively), were restored to almost normal levels two days later. LDL-apheresis reduced serum aqueous diffusion (AD) CEC, SR-BI-CEC, and ABCA1-CEC. AD and SR-BI were fully restored whereas ABCA1-CEC remained low two days later. Sera immediately and two days after LDL-apheresis had a lower CLC than pre-LDL-apheresis sera. In conclusion, LDL-apheresis transiently reduces HDL-C levels and serum CEC, but it also reduces also serum capacity to deliver cholesterol to macrophages. Despite a potentially negative effect on HDL levels and composition, LDL-apheresis may counteract foam cells formation.
Keywords: low density lipoprotein, familial hypercholesterolemia, familial combined hyperlipidemia, cholesterol efflux capacity, cholesterol loading capacity
Familial hypercholesterolemia (FH) and familial combined hyperlipidemia (FCH) are common inherited disorders associated with increased circulating LDL-cholesterol (LDL-C) and severe atherosclerosis (1). FH is a genetic autosomal disorder caused by a number of mutations in the LDL receptor gene (2). The clinical picture, characterized by accelerated atherosclerosis and tendon xanthomas, can vary from mild to severe forms, according to the degree of LDL receptor deficiency or dysfunction and the resulting defective hepatic clearance of LDL-C from the circulation. FCH is a polygenic disorder, in which complex mechanisms lead to increased serum levels of LDL-C and apoB and hypertriglyceridemia. Together with total cholesterol (TC) and LDL-C, HDL-cholesterol (HDL-C) levels are considered to be among the relevant factors determining cardiovascular risk in the general population and in patients affected by these two disorders (3, 4).
At present, HDL quality is believed to be one of the major determinants of HDL-related atheroprotection, especially with respect to the ability of individual sera to promote cellular cholesterol efflux, the first rate-limiting step of the reverse cholesterol transport (RCT) process, considered an important antiatherosclerotic mechanism and a marker inversely correlated with cardiovascular risk (5). The different HDL subfractions play a specific role in the diverse cholesterol efflux mechanisms, and modifications in their composition may affect their actual functions. In particular, pre-β (lipid free/poor apoA-I) HDL particles are acceptors for the ATP-binding cassette A1 (ABCA1)-mediated cholesterol unidirectional efflux (6, 7), whereas mature HDL are involved in aqueous diffusion (AD) and scavenger receptor BI (SR-BI)-mediated efflux, a bidirectional facilitated transport of cholesterol that, like AD, depends on the cholesterol concentration gradient (8). Both pre-β HDL and mature HDL may drive ATP-binding cassette G1 (ABCG1)-mediated unidirectional efflux (6, 9).
LDL-apheresis is used in patients with severe dyslipidemia refractory to diet and pharmacologic therapy to reduce circulating LDL-cholesterol through apoB-directed removal systems (10). This procedure has also been shown to remove variable amounts of HDL particles and to modify HDL subfraction distribution and composition (11). However, little is known on the effect of LDL-apheresis on serum ability to promote cellular cholesterol efflux and delivery.
In this work, we measured serum capacity to promote cholesterol efflux (CEC) through the SR-BI, ABCG1, ABCA1, and AD pathways before, immediately after, and two days after LDL-apheresis. We also studied the modifications induced by the apheretic treatment on serum macrophage cholesterol loading capacity (CLC).
METHODS
Study participants
Fifteen patients (mean age 62 ± 7; 3 females, 12 males) affected by FH (n = 6) or FCH (n = 9) were enrolled for the study. Patients were from a cohort chronically treated with LDL-apheresis at the Reference Center for Hereditary Dyslipidaemias in Pisa because of refractory hypercholesterolemia in presence of severe forms of cardiovascular complications; two patients of the FCH group, despite a good control of plasma lipids by statin therapy, underwent apheretic treatment because of very high levels of plasma lipoprotein(a) and severe polidistrectual arteriopathy. Experimental protocol was applied two times for each patient. The study was performed in accordance with the ethical principles set in the Declaration of Helsinki. Study participants gave their written informed consent, and the study protocol received approval from the local ethical committee.
LDL-apheresis
LDL-apheresis was performed using two techniques: one based on specific absorption of apoB-containing lipoproteins on dextran sulfate cellulose columns (Liposorber LA-15 columns and MA-03 apparatus; Kaneka Co., Japan), and the other based on apoB-containing lipoprotein extracorporeal precipitation induced by heparin in acid pH (HELP system; B. Braun Avitum, Melsungen, Germany).
In both procedures, an extracorporeal venous-venous circulation provided a blood flow of 90 to 120 ml/min; the initial heparin bolus was 1,500 IU, followed by continuous infusion of 1,000 IU/h. Plasma was separated by a polysulfone hollow-fiber filter (Sulflux FS-05).
Patients were assigned to one of the two techniques in considerations of clinical/pharmacological biocompatibility with the LDL-apheresis procedures, idiosyncrasy, and/or interference between ACE inhibitor drugs or ARB therapy and liposorber columns (12).
Laboratory measurements
TC, HDL-C, and triglycerides (TG) were measured by standard enzymatic techniques (Synchron CX9 Pro; Beckman Coulter Inc., Fullerton, CA). LDL-C was calculated according to the Friedewald formula (13). ApoA-I, apoB, and lipoprotein(a) were measured by rate nephelometry (BN-ProSpec; Siemens Healthcare Diagnostics, Italy).
Measurement of serum CEC
Efflux studies were performed as previously described (9, 14) using J774 macrophages, Fu5AH rat hepatoma cells, or CHO cells expressing human ABCG1 (CHO-GI cells) (15, 16). J774 cells were cultured in 10% FCS-RPMI, Fu5AH cells in 10% FCS-DMEM, and CHO-GI cells in 10% FCS-DMEM. For efflux studies, cells were labeled with [1,2-3H] cholesterol in the presence of an ACAT inhibitor (2 µg/ml, Sandoz 58035; Sigma-Aldrich, Milano, Italy). J774 cells were treated with or without 0.3 mM c-AMP (cpt-AMP; Sigma-Aldrich) in 0.2% BSA for 18 h to upregulate ABCA1 (9, 17, 18). The efflux medium was prepared using 2% (v/v) whole serum and incubated with cells for 4–6 h (see supplemental methods). CEC was expressed as a percentage of radiolabeled cholesterol released to the medium over the total radioactivity incorporated by cells. To minimize the intra-assay variability, every serum sample was run in triplicate and for each, the percentage of efflux was obtained and the average and standard deviation were calculated. A pool of human normolipidemic sera was tested in each assay as reference standard 1 (St1), and its CEC was used to normalize the patient samples values from different experiments to correct for the inter-assay variability. A second pool of human normolipidemic sera as reference standard 2 (St2) was tested in each assay, and its CEC, after normalization, was the index of the inter-assay variability (14).
Measurement of serum macrophage CLC
THP-1 monocytes were cultured in RPMI 1640 medium supplemented with 10% FBS at 37°C in 5% CO2. To perform the experiments, cells were seeded in 12-well plates at the density of 106 cells/well in the presence of 100 ng/ml PMA for 72 h to allow differentiation into macrophages. THP-1 cells were exposed for 8 h to 5% (v/v) whole serum from one control subject and from six patients before, immediately after, and two days after LDL-apheresis.
Cellular cholesterol content before and after serum exposure was measured as previously described (19). Briefly, at the end of the experiment, cell monolayers were washed with PBS and lysed in 0.5 ml of a 1% sodium cholate solution in water supplemented with 10 U/ml DNase. Cholesterol was then measured fluorimetrically using the Amplex Red Cholesterol Assay Kit (Molecular Probes, Eugene, OR) as described by the manufacturer. The amount of cholesterol in each well was measured by comparison with a cholesterol standard curve included in each experiment. An aliquot of the cell lysates was also taken to measure cell protein by a modified Lowry method (20). CLC was defined as macrophage cholesterol content after exposure of cells to serum and expressed as micrograms of cholesterol per milligram of protein.
Statistical analyses
Statistical analyses were performed using Prism (version 5.0) (GraphPad Inc., San Diego, CA). Data were expressed as mean ± SEM or mean ± SD. Treatment groups were compared using a paired or unpaired two tailed Student t-test, and significant differences were defined as P < 0.05. Variables showing no normal distribution, checked by Chi-squared test, were logarithmically transformed when appropriate. The Pearson correlation coefficient (r) was used to test the relationship between cholesterol efflux capacity of sera and plasma lipids.
RESULTS
Effect of LDL-apheresis on plasma lipids
Data on patient circulating lipid levels before and after LDL-apheresis are shown in Table 1. Levels of TC, LDL-C, and apoB, as expected and consistently with earlier reports (11), were markedly reduced immediately after LDL-apheresis [−80% (P < 0.001) and −74% (P < 0.001), respectively]. Two days after the procedure, TC, LDL-C, and apoB plasma levels were increased to values corresponding to about 50% of those before apheresis. HDL-C and apoA-I plasma levels were also reduced by LDL-apheresis [−27% (P < 0.001) and −16% (P < 0.01), respectively]; however, two days later, plasma HDL-C and apoA-I levels had returned to concentrations similar to those detected before the procedure [−11% and −1%, respectively; not significant (NS)]. TG levels were also markedly reduced after LDL-apheresis (−63%; P < 0.01); two days later, the TG plasma levels increased to about 80% of preprocedure values (NS). The variations in plasma lipids before and after LDL-apheresis were found to be similar in FH and FCH patients, and they were independent of the apheretic technique applied (data not shown).
TABLE 1.
Effect of LDL-apheresis on plasma lipids, lipoproteins, and apolipoproteins in FH and FCH patients
| Lipid | Before LDL-apheresis | After LDL-apheresis | Two days after LDL-apheresis |
| mg/dl | mg/dl | mg/dl | |
| TC | 250.0 ± 21.60 | 77.4 ± 5.30(−69%) | 144.6 ± 8.40 (−42%) |
| TG | 171.6 ± 32.60 | 64.2 ± 11.40(−63%) | 138.5 ± 17.30 (−19%) |
| LDL-C | 172.4 ± 20.3 | 33.4 ± 4.9(−80%) | 77.6 ± 7.3 (−55%) |
| ApoB | 134.5 ± 10.10 | 34.5 ± 3.50(−74%) | 72.7 ± 3.90 (−46%) |
| HDL-C | 44.0 ± 2.70 | 31.9 ± 1.80(−27%) | 39.3 ± 2.20 (−11%) |
| ApoA-I | 144.0 ± 5.70 | 120.3 ± 4.00(−16%) | 142.6 ± 6.10 (−1%) |
| Lipoprote in(a) | 95.4 (2.4–222.0) | 15.2 (2.4–48.9) | 39.2 (2.4–94.1) |
Values are expressed as mean ± SEM (n = 15). Percentage change of lipid values immediately after and two days after LDL-apheresis are in parentheses. Lipoprotein(a) levels are expressed as median (minimum-maximum) because of its asymmetric distribution.
Patient serum CEC before, immediately after, and two days after LDL-apheresis
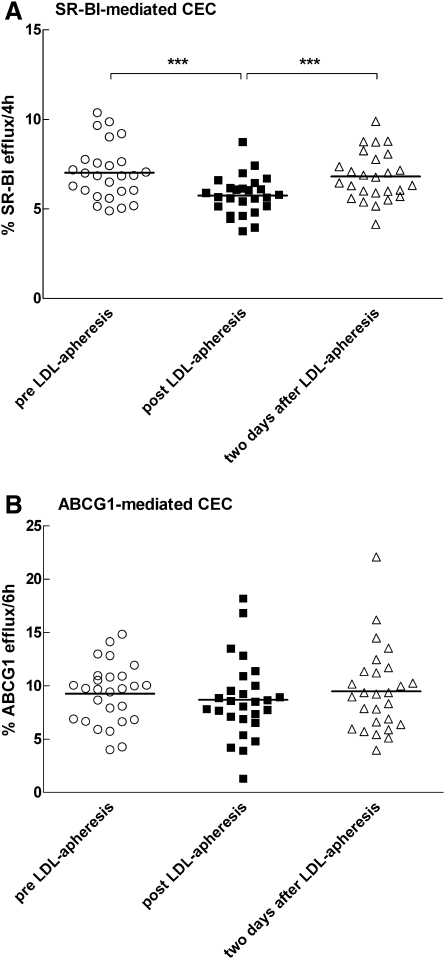
SR-BI-mediated CEC.
Preprocedure serum SR-BI-mediated CEC was lower than that of a normolipidemic serum added as a control (mean ± SD 7.03% ± 1.54% and 9.09% ± 0.18%, respectively; P < 0.05). SR-BI-mediated CEC of sera immediately after LDL-apheresis was significantly reduced (−18%; P < 0.001) compared with pretreatment values (Fig. 1A). Sera harvested two days after the procedure showed a complete recovery of the SR-BI-mediated CEC (mean ± SD 6.81% ± 1.35% two days after LDL-apheresis and 7.03% ± 1.54% before LDL-apheresis; NS). The variations of SR-BI-mediated CEC of sera before and after LDL-apheresis at both visits were correlated with the variations observed in HDL-C (r = 0.6828; P < 0.0001) and apoA-I plasma levels (r = 0.5474; P < 0.001).
Fig. 1.
CEC of sera from subjects before, immediately after, and two days after LDL-apheresis. SR-BI-mediated CEC (A) and ABCG1-mediated CEC (B). Efflux of radiolabeled cholesterol to 2% (v/v) serum was measured as described in Methods. Specifically, SR-BI-mediated CEC was measured in Fu5AH hepatoma cells (A) and ABCG1-mediated CEC was the difference in efflux between hABCG1 overexpressing CHO and control CHO cells (B). Each point represents the average efflux to serum from single patients harvested before LDL-apheresis (open circles), immediately after LDL-apheresis (filled squares), and two days after LDL-apheresis (open triangles) (n = 26). Statistical significance was estimated by paired, two-tailed t-tests; ***P < 0.001.
ABCG1-mediated CEC.
Preprocedure ABCG1-mediated CEC was lower than that of normolipidemic serum added as a control (mean ± SD 9.26% ± 2.81% and 14.01% ± 0.26%, respectively; P < 0.001). No differences were detected in ABCG1-mediated CEC of sera collected before, immediately after, or two days after LDL-apheresis (mean ± SD 9.26% ± 2.81%, 8.69% ± 3.67%, and 9.49% ± 3.94%, respectively; NS) (Fig. 1B). The ABCG1-mediated CEC of sera before and after LDL-apheresis at both visits were not correlated with either HDL-C level (r = 0.2024; NS) or apoA-I plasma level (r = 0.1179; NS).
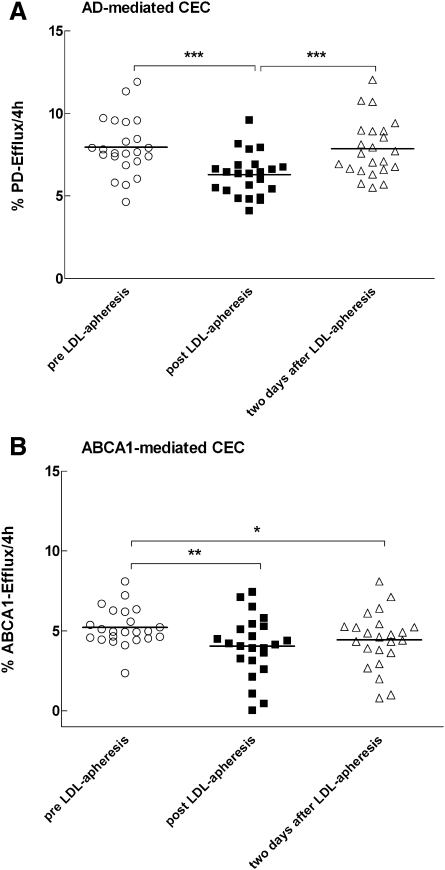
AD- and ABCA1-mediated CEC.
Serum AD- and ABCA1-mediated CEC were measured using J774 macrophages. When these cells are in basal conditions, serum-induced cholesterol efflux mainly occurs by AD because no specific transporters are expressed on the plasma membrane (14, 21). When cells are treated with cAMP, expression of ABCA1 is induced, and the resulting measured cholesterol efflux upon exposure to patient serum is the result of both AD- and ABCA1-mediated CEC (22).
Preprocedure serum AD-mediated CEC was significantly lower compared with normolipidemic serum efflux values (mean ± SD 7.97% ± 1.69% and 10.24% ± 0.33%, respectively; P < 0.05). Similar to that observed for the SR-BI pathway, serum CEC by AD immediately after LDL-apheresis was significantly reduced (−21%; P < 0.001), but it was completely restored two days after LDL-apheresis (mean ± SD 7.81% ± 1.71% two days after LDL-apheresis and 7.97% ± 1.69% before the procedure; NS) (Fig. 2A). The variations of AD-mediated CEC of sera before and after LDL-apheresis at both visits were correlated with the variations observed in HDL-C level (r = 0.7086; P < 0.0001) and apoA-I plasma level (r = 0.5179; P < 0.001).
Fig. 2.
CEC of sera from subjects before, immediately after, and two days after LDL-apheresis. AD-mediated CEC (A) and ABCA1-mediated CEC (B). Efflux of radiolabeled cholesterol to 2% (v/v) serum was measured as described in Methods. Specifically, AD-mediated CEC was measured in J774 macrophages in basal conditions (A), and ABCA1-mediated CEC was the difference in efflux between cAMP-treated J774 and J774 in basal conditions (B). Each point represents the average efflux to serum from single patients harvested before LDL-apheresis (open circles), immediately after LDL-apheresis (filled squares), and two days after LDL-apheresis (open triangles) (n = 23). Statistical significance was estimated by paired, two-tailed t-tests; *P < 0.05; **P < 0.01; ***P < 0.001.
Preprocedure serum ABCA1-mediated CEC was not significantly different from normolipidemic serum efflux values (mean ± SD 5.25% ± 1.18% and 5.62% ± 0.40%, respectively; NS). The ABCA1-mediated CEC of sera immediately after LDL-apheresis was reduced by about 20% with respect to pretreatment values (P < 0.01) and remained substantially unchanged two days after LDL-apheresis (4.17% ± 1.97% immediately after LDL-apheresis and 4.66% ± 2.05% after two days; NS; Fig. 2B). The ABCA1-mediated CEC of sera before and after LDL-apheresis at both visits were not correlated with either HDL-C level (r = 0.09357; NS) or apoA-I plasma level (r = 0.04224; NS).
No differences were found when comparing results obtained separately with serum from patients with FH and FCH for all the CEC pathways studied. The results were also largely independent of the apheretic technique applied (data not shown).
Patient serum macrophage CLC before, immediately after, and two days after LDL-apheresis
Serum macrophage CLC was evaluated measuring the capacity of patient sera obtained before, immediately after, and two days after LDL-apheresis to deliver cholesterol to human macrophages THP-1. THP-1 initial cholesterol content prior the exposure with serum was 25.07 ± 2.20 µg/mg of protein. The macrophage CLC of the pre-LDL-apheresis serum was significantly higher compared with that of normolipidemic serum added as a control (mean ± SD 34.99 ± 1.60 µg/mg protein and 29.13 ± 2.20 µg/mg of protein, respectively; P < 0.001). Immediately after LDL-apheresis, serum macrophage CLC was markedly lower than that relative to preapheresis sera (mean ± SD 21.91 ± 2.20 µg/mg protein). A similar value of serum macrophage CLC was found in serum drawn two days after apheresis (mean ± SD 23.52 ± 2.40 µg/mg of protein), with no statistically significant difference with the immediate postapheretic values (Fig. 3).
Fig. 3.
Macrophage CLC of sera from subjects before, immediately after, and two days after LDL-apheresis. Cellular cholesterol content of THP-1 cells incubated in the absence or presence of 5% (v/v) serum was measured as described in Methods. Each bar represents the average ± SD cholesterol content of cells exposed to patient serum harvested before LDL-apheresis (filled bar), immediately after LDL-apheresis (horizontal lines bar), and two days after LDL-apheresis (vertical lines bar) (n = 6). Intracellular cholesterol content is expressed as micrograms of cholesterol per milligrams of protein. Statistical analysis was estimated by unpaired two tailed t-test; ***P < 0.001.
DISCUSSION
Subjects with FH and FCH have increased circulating LDL-C and severe atherosclerosis (1). The present work shows that LDL-apheresis in these patients induces, consistent with previous reports (11), modifications of both circulating LDL-C and HDL-C levels, and it demonstrates that post-LDL-apheresis patient serum has a transiently lower CEC through SR-BI and AD processes and a less efficient ABCA1-mediated CEC lasting for at least two days after treatment. However, post-LDL-apheresis sera show a reduced macrophage serum CLC, still present two days after the procedure.
We found that AD-, SR-BI- and ABCG1-mediated CEC of preapheresis sera, from either FH or FCH patients, were significantly lower than that of normolipidaemic serum. ABCA1-mediated CEC of patient sera before LDL-apheresis did not differ significantly from that of control serum. Our data are consistent with previous observations obtained in FH patients of an impaired capacity of isolated HDL particles to mediate cellular free cholesterol efflux via both SR-BI and ABCG1 pathways and a normal capacity of serum to mediate cellular cholesterol efflux via the ABCA1 pathway (23). In addition, we extended, for the first time, the same observation to FCH patients.
LDL-apheresis, consistent with previous reports, induced a reduction of circulating TC, LDL-C, apoB, HDL-C, and apoA-I (11, 24). Two days after the procedure, all lipid parameters but HDL-C and apoA-I were still low; SR-BI- and AD-mediated CEC were significantly reduced immediately after LDL-apheresis and, in parallel with HDL-C and apoA-I plasma levels, returned to pretreatment values after two days (Figs. 1A and 2A). These results indicate that both AD- and SR-BI-mediated CEC are driven by plasma HDL-C/apoA-I, as indicated by the good correlations found between these two serum CEC parameters and HDL-C/apoAI plasma levels.
The reduction of serum SR-BI-mediated CEC after LDL-apheresis could be determined by the specific depletion of HDL-apoE induced by this procedure (11), as lipid-bound apoE is particularly efficient in promoting SR-BI-mediated cholesterol efflux (25). ApoE-rich mature HDL is also reported to promote cholesterol efflux through the ABCG1 pathway (26). However, after LDL-apheresis, we did not observe any variation of serum ABCG1-mediated CEC in our subjects (Fig. 1B). We may speculate that the apheretic procedure may promote a remodeling of HDL with the formation of mature HDL or pre-β HDL acting as ABCG1 acceptors and resulting in an overall unchanged serum ABCG1-mediated CEC. Indeed, we recently demonstrated that pre-β reconstituted HDL of 7.8 nm promotes ABCG1-mediated cholesterol efflux (9). The lack of correlation observed between ABCG1-mediated CEC and HDL-C levels indicates that, in addition to ABCA1-mediated CEC (27), ABCG1-mediated CEC may also be independent of HDL quantity.
ABCA1-mediated CEC was significantly reduced to the same extent immediately and two days after the apheretic procedure (Fig. 2B). The discrepancy between the low ABCA1-mediated CEC two days after apheresis and the almost complete restoration of total HDL-C serum levels at the same time point can be explained by considering that HDL quality and not quantity is important for ABCA1-mediated CEC. Indeed, it has been reported that LDL-apheresis induces a reduction of more than 50% of serum pre-β1 HDL (11), which is the HDL fraction that we previously demonstrated to correlate specifically with ABCA1-mediated cholesterol efflux (6).
As cellular cholesterol accumulation is the result of efflux-influx processes, to evaluate the net effect of LDL-apheresis on overall serum atherogenic properties, we measured serum macrophages CLC of patient sera obtained before and after apheretic treatment. The significant reduction in serum macrophage CLC after LDL-apheresis is an important new observation, possibly contributing to explain the antiatherosclerotic effect of the apheretic procedure. In particular, the reduced CLC of sera obtained immediately after apheresis most probably reflects the marked reduction in circulating LDL-C and apoB observed soon after LDL-apheresis. Two days after LDL-apheresis, LDL-C was increased, but the restored AD- and SR-BI-mediated CEC may contribute toward maintaining a low serum macrophage CLC.
In conclusion, our results demonstrate that LDL-apheresis can modify HDL level, composition, and functionality, thus affecting serum CEC, and at the same time reduce serum capacity to deliver cholesterol to macrophages, thus counteracting foam-cell formation. Our findings may contribute to clarifying the mechanisms of the antiatherosclerotic action of LDL-apheresis.
Supplementary Material
Footnotes
Abbreviations:
- AD
- aqueous diffusion
- CEC
- cholesterol efflux capacity
- CLC
- cholesterol loading capacity
- FCH
- familial combined hyperlipidemia
- FH
- familial hypercholesterolemia
- HDL-C
- HDL-cholesterol
- LDL-C
- LDL-cholesterol
- NS
- not significant
- RCT
- reverse cholesterol transport
- SR-BI
- scavenger receptor class B type I
- TC
- total cholesterol
- TG
- triglyceride
This work was supported by Istituto Nazionale per le Ricerche Cardiovascolari (INRC) and Consortium TEFARCO Innova.
The online version of this article (available at http://www.jlr.org) contains supplementary data in the form of methods.
REFERENCES
- 1.Masoura C., Pitsavos C., Aznaouridis K., Skoumas I., Vlachopoulos C., Stefanadis C. 2011. Arterial endothelial function and wall thickness in familial hypercholesterolemia and familial combined hyperlipidemia and the effect of statins. A systematic review and meta-analysis. Atherosclerosis. 214: 129–138 [DOI] [PubMed] [Google Scholar]
- 2.Austin M. A., Hutter C. M., Zimmern R. L., Humphries S. E. 2004. Genetic causes of monogenic heterozygous familial hypercholesterolemia: a HuGE prevalence review. Am. J. Epidemiol. 160: 407–420 [DOI] [PubMed] [Google Scholar]
- 3.Real J. T., Chaves F. J., Martinez-Uso I., Garcia-Garcia A. B., Ascaso J. F., Carmena R. 2001. Importance of HDL cholesterol levels and the total/ HDL cholesterol ratio as a risk factor for coronary heart disease in molecularly defined heterozygous familial hypercholesterolaemia. Eur. Heart J. 22: 465–471 [DOI] [PubMed] [Google Scholar]
- 4.Goldstein J. L., Hazzard W. R., Schrott H. G., Bierman E. L., Motulsky A. G. 1973. Hyperlipidemia in coronary heart disease. I. Lipid levels in 500 survivors of myocardial infarction. J. Clin. Invest. 52: 1533–1543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rader D. J., Alexander E. T., Weibel G. L., Billheimer J., Rothblat G. H. 2009. The role of reverse cholesterol transport in animals and humans and relationship to atherosclerosis. J. Lipid Res. 50(Suppl.): S189–S194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Favari E., Lee M., Calabresi L., Franceschini G., Zimetti F., Bernini F., Kovanen P. T. 2004. Depletion of pre-beta-high density lipoprotein by human chymase impairs ATP-binding cassette transporter A1- but not scavenger receptor class B type I-mediated lipid efflux to high density lipoprotein. J. Biol. Chem. 279: 9930–9936 [DOI] [PubMed] [Google Scholar]
- 7.Dean M., Hamon Y., Chimini G. 2001. The human ATP-binding cassette (ABC) transporter superfamily. J. Lipid Res. 42: 1007–1017 [PubMed] [Google Scholar]
- 8.de la Llera-Moya M., Connelly M. A., Drazul D., Klein S. M., Favari E., Yancey P. G., Williams D. L., Rothblat G. H. 2001. Scavenger receptor class B type I affects cholesterol homeostasis by magnifying cholesterol flux between cells and HDL. J. Lipid Res. 42: 1969–1978 [PubMed] [Google Scholar]
- 9.Favari E., Calabresi L., Adorni M. P., Jessup W., Simonelli S., Franceschini G., Bernini F. 2009. Small discoidal pre-beta1 HDL particles are efficient acceptors of cell cholesterol via ABCA1 and ABCG1. Biochemistry. 48: 11067–11074 [DOI] [PubMed] [Google Scholar]
- 10.Szczepiorkowski Z. M., Winters J. L., Bandarenko N., Kim H. C., Linenberger M. L., Marques M. B., Sarode R., Schwartz J., Weinstein R., Shaz B. H. 2010. Guidelines on the use of therapeutic apheresis in clinical practice--evidence-based approach from the Apheresis Applications Committee of the American Society for Apheresis. J. Clin. Apher. 25: 83–177 [DOI] [PubMed] [Google Scholar]
- 11.Orsoni A., Saheb S., Levels J. H., Dallinga-Thie G., Atassi M., Bittar R., Robillard P., Bruckert E., Kontush A., Carrie A., et al. 2011. LDL-apheresis depletes apoE-HDL and pre-beta1-HDL in familial hypercholesterolemia: relevance to atheroprotection. J. Lipid Res. 52: 2304–2313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kojima S., Shida M., Takano H., Inami S., Yodogawa K., Yokoyama H., Kuramochi M. 2001. Effects of losartan on blood pressure and humoral factors in a patient who suffered from anaphylactoid reactions when treated with ACE inhibitors during LDL apheresis. Hypertens. Res. 24: 595–598 [DOI] [PubMed] [Google Scholar]
- 13.Friedewald W. T., Levy R. I., Fredrickson D. S. 1972. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 18: 499–502 [PubMed] [Google Scholar]
- 14.Zanotti I., Favari E., Bernini F. 2012. Cellular cholesterol efflux pathways: impact on intracellular lipid trafficking and methodological considerations. Curr. Pharm. Biotechnol. 13: 292–302 [DOI] [PubMed] [Google Scholar]
- 15.Jessup W., Gelissen I. C., Gaus K., Kritharides L. 2006. Roles of ATP binding cassette transporters A1 and G1, scavenger receptor BI and membrane lipid domains in cholesterol export from macrophages. Curr. Opin. Lipidol. 17: 247–257 [DOI] [PubMed] [Google Scholar]
- 16.Calabresi L., Favari E., Moleri E., Adorni M. P., Pedrelli M., Costa S., Jessup W., Gelissen I. C., Kovanen P. T., Bernini F., et al. 2009. Functional LCAT is not required for macrophage cholesterol efflux to human serum. Atherosclerosis. 204: 141–146 [DOI] [PubMed] [Google Scholar]
- 17.Favari E., Zanotti I., Zimetti F., Ronda N., Bernini F., Rothblat G. H. 2004. Probucol inhibits ABCA1-mediated cellular lipid efflux. Arterioscler. Thromb. Vasc. Biol. 24: 2345–2350 [DOI] [PubMed] [Google Scholar]
- 18.Yancey P. G., Bortnick A. E., Kellner-Weibel G., de la Llera-Moya M., Phillips M. C., Rothblat G. H. 2003. Importance of different pathways of cellular cholesterol efflux. Arterioscler. Thromb. Vasc. Biol. 23: 712–719 [DOI] [PubMed] [Google Scholar]
- 19.Zimetti F., Weibel G. K., Duong M., Rothblat G. H. 2006. Measurement of cholesterol bidirectional flux between cells and lipoproteins. J. Lipid Res. 47: 605–613 [DOI] [PubMed] [Google Scholar]
- 20.Markwell M. A., Haas S. M., Bieber L. L., Tolbert N. E. 1978. A modification of the Lowry procedure to simplify protein determination in membrane and lipoprotein samples. Anal. Biochem. 87: 206–210 [DOI] [PubMed] [Google Scholar]
- 21.Rothblat G. H., de la Llera-Moya M., Favari E., Yancey P. G., Kellner-Weibel G. 2002. Cellular cholesterol flux studies: methodological considerations. Atherosclerosis. 163: 1–8 [DOI] [PubMed] [Google Scholar]
- 22.Khera A. V., Cuchel M., de la Llera-Moya M., Rodrigues A., Burke M. F., Jafri K., French B. C., Phillips J. A., Mucksavage M. L., Wilensky R. L., et al. 2011. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N. Engl. J. Med. 364: 127–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bellanger N., Orsoni A., Julia Z., Fournier N., Frisdal E., Duchene E., Bruckert E., Carrie A., Bonnefont-Rousselot D., Pirault J., et al. 2011. Atheroprotective reverse cholesterol transport pathway is defective in familial hypercholesterolemia. Arterioscler. Thromb. Vasc. Biol. 31: 1675–1681 [DOI] [PubMed] [Google Scholar]
- 24.Sampietro T., Tuoni M., Ferdeghini M., Ciardi A., Marraccini P., Prontera C., Sassi G., Taddei M., Bionda A. 1997. Plasma cholesterol regulates soluble cell adhesion molecule expression in familial hypercholesterolemia. Circulation. 96: 1381–1385 [DOI] [PubMed] [Google Scholar]
- 25.Chroni A., Nieland T. J., Kypreos K. E., Krieger M., Zannis V. I. 2005. SR-BI mediates cholesterol efflux via its interactions with lipid-bound ApoE. Structural mutations in SR-BI diminish cholesterol efflux. Biochemistry. 44: 13132–13143 [DOI] [PubMed] [Google Scholar]
- 26.Matsuura F., Wang N., Chen W., Jiang X. C., Tall A. R. 2006. HDL from CETP-deficient subjects shows enhanced ability to promote cholesterol efflux from macrophages in an apoE- and ABCG1-dependent pathway. J. Clin. Invest. 116: 1435–1442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de la Llera-Moya M., Drazul-Schrader D., Asztalos B. F., Cuchel M., Rader D. J., Rothblat G. H. 2010. The ability to promote efflux via ABCA1 determines the capacity of serum specimens with similar high-density lipoprotein cholesterol to remove cholesterol from macrophages. Arterioscler. Thromb. Vasc. Biol. 30: 796–801 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.