Abstract
Recently, we reported a case of gastric mucosa-associated lymphoid tissue (MALT) lymphoma presenting with unique vascular features. In the report, we defined the tree-like appearance (TLA) on the images of abnormal blood vessels which resembled branches from the trunk of a tree in the shiny mucosa, in which the glandular structure was lost. The 67-year-old female was diagnosed with gastric MALT lymphoma. The patient received eradication therapy for H. pylori. Conventional endoscopy revealed multiple ill-delineated brownish depressions in the stomach and cobblestone-like mucosa was observed at the greater curvature to the posterior wall of the upper gastric body 7 mo after successful eradication. Unsuccessful treatment of gastric MALT lymphoma was suspected on conventional endoscopy. Conventional endoscopic observations found focal depressions and cobblestone-like appearance, and these lesions were subsequently observed using magnified endoscopy combined with narrow band imaging to identify abnormal vessels presenting with a TLA within the lesions. Ten biopsies were taken from the area where abnormal vessels were present within these lesions. Ten biopsies were also taken from the lesions without abnormal vessels as a control. A total of 20 biopsy samples were evaluated to determine whether the diagnosis of MALT lymphoma could be obtained histologically from each sample. A positive diagnosis was obtained in 8/10 TLA (+) sites and in 2/10 TLA(-) sites. Target biopsies of the site with abnormal blood vessels can potentially improve diagnostic accuracy of gastric MALT lymphoma.
Keywords: Mucosa associated-lymphoid tissue, Magnified endoscopy, Narrow band imaging, Tree-like appearance
INTRODUCTION
Gastric lymphoma arising from mucosa-associated lymphoid tissue (MALT) was first reported as a low-grade gastric lymphoma in 1983 by Isaacso[1]. MALT has distinct histological and clinical characteristics compared with nodal B-cell lymphoma[1-4]. MALT lymphoma arising in the stomach grossly presents as a flat, superficial[5], or even invasive lesion with erosions and ulcerations, and develops from chronic active gastritis. Gastric MALT lymphoma is often misdiagnosed endoscopically as gastric ulcer, gastritis, or gastric cancer, and it is necessary to establish the diagnosis of gastric MALT lymphoma from these diseases. It is important to initially suspect gastric MALT lymphoma because the endoscopic features of gastric MALT lymphoma are variable. The definitive diagnosis is made by histopathologic examination of the biopsy material, and the presence of a lymphoepithelial lesion in which tumor cells invade and destroy mucosal epithelial glands is one of the most important findings. However, biopsy specimens are often small or crushed, making the diagnosis difficult. In addition, gastric MALT lymphoma lesions are often located close to the lamina muscularis mucosae, and this makes the histopathologic diagnosis from endoscopic biopsy difficult. Therefore, it is often found that the definitive diagnosis of MALT lymphoma can not be obtained after multiple biopsies even in cases where gastric MALT lymphoma is suspected based on endoscopic features of conventional endoscopy. The usefulness of magnified endoscopy (ME) combined with narrow band imaging (NBI) is well recognized in the diagnosis of gastritis and gastric cancer[6-9]. Recently, the characteristic features of gastric MALT lymphoma, based on magnified endoscopic imaging without NBI, were reported by Ono et al[10]. We took advantage of ME combined with NBI and recently reported a case of gastric MALT lymphoma presenting with unique vascular features[11]. In this case report, we defined the tree-like appearance (TLA) on the images of abnormal blood vessels resembling branches from the trunk of a tree in the shiny mucosa, in which the glandular structure was lost.
Following the first case report, we addressed whether target biopsies from the lesion with vascular abnormalities detected by ME combined with NBI can contribute to the histological diagnosis of gastric MALT lymphoma. We carried out ME combined with NBI in one patient with MALT lymphoma. After obtaining both oral and written informed consent from the patient, target biopsy samples were taken from the sites with and without abnormal blood vessels under the guidance of ME combined with NBI, and the relationship between the presence of abnormal blood vessels and the diagnosis of MALT lymphoma from biopsy histology was investigated.
This case study was approved by the Medical Ethics Committee of Saitama Medical University International Medical Center.
CASE REPORT
A 67-year-old female was diagnosed with gastric MALT lymphoma. The initial diagnosis in this patient made using ME combined NBI has been reported elsewhere[11]. She had undergone eradication therapy for H. pylori with clarithromycin, amoxicillin, and a proton pump inhibitor. The gastric lesion was carefully observed using ME combined with NBI 7 mo after successful eradication therapy. The endoscopic system was composed of an image processor (CV-260SL, Olympus Medical Systems, Tokyo, Japan), a light source (CLV-260SL), and a zoom endoscope (GIF-Q240Z). Conventional endoscopy revealed multiple ill-delineated brownish depressions in the stomach (Figure 1A and C), while cobblestone-like mucosa was recognized at the greater curvature to the posterior wall of the upper gastric body (Figure 2A). Unsuccessful treatment of gastric MALT lymphoma was suspected on conventional endoscopy. Magnified endoscopy combined with the NBI system was then carried out. When the cobblestone-like mucosa at the greater curvature to the posterior wall of the upper gastric body was examined by ME combined with NBI, branching TLAs were observed (Figure 2C), and three target biopsy samples were taken from the sites with TLAs. When multiple brownish depressions in the stomach were examined by ME combined with NBI (Figure 1A), TLAs were observed at the same site (Figure 1B). Seven target biopsy samples were then taken from seven depressions with TLAs. For comparison, a total of 10 target biopsies were taken from the following sites under the guidance of ME combined with NBI: 3 from the site without TLAs adjacent to the cobblestone-like lesion at the upper body, 7 from another seven brownish depressions without TLAs (Figures 1D and 2B). The assistant doctor recorded the presence or absence of TLA during the procedure to ensure objectivity of the examination.
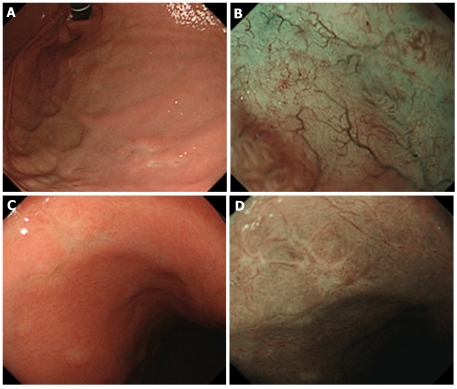
Figure 1.
Routine observation revealed multiple ill-delineated brownish depressions in the stomach. A: A brownish depression in the anterior wall of the upper gastric corpus; B: Narrow band imaging (NBI) findings of Figure 1A (TLA+); C: A brownish depression in the anterior wall of the middle portion of the gastric corpus; D: NBI findings of Figure 1C (TLA-). TLA: Tree-like appearance.
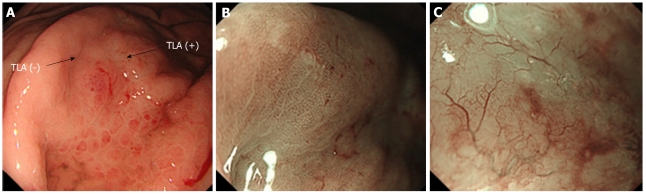
Figure 2.
Routine observation revealed cobblestone-like mucosa at the greater curvature to the posterior wall of the upper gastric body. A: Biopsy site of the cobblestone-like mucosa; B: Narrow band imaging (NBI) findings of the sites adjacent to the cobblestone-like mucosa at the upper gastric body (Figure 2A) TLA(-); C: Observation of cobblestone-like mucosa at the greater curvature to the posterior wall of the upper gastric body. Magnified endoscopy combined with NBI revealed disappearance of gland structure and branching abnormal blood vessels (Figure 2A) TLA(+). TLA: Tree-like appearance.
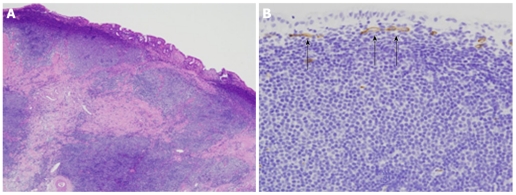
Histological sections were examined by a gastrointestinal pathologist experienced in the diagnosis of lymphoma, and Wotherspoon grade 4 or 5 tumors which were immunohistochemically positive for CD20 and negative for CD3, CD10, and Cyclin D1 were diagnosed as MALT lymphoma. Eight of the 10 biopsies taken from the site with TLAs suggested a lymphoepithelial lesion, and the atypical lymphocytes were immunohistochemically CD20+, CD10-, and CD5-. These findings were consistent with MALT lymphoma (Figure 3A and B). On the other hand, 8 of the 10 biopsies from the site without TLAs showed only infiltration of inflammatory cells such as lymphocytes, plasma cells, and eosinophils in the gastric mucosa exhibiting gastric foveolar hyperplasia (Figure 4), without findings suggestive of MALT lymphoma (Table 1).
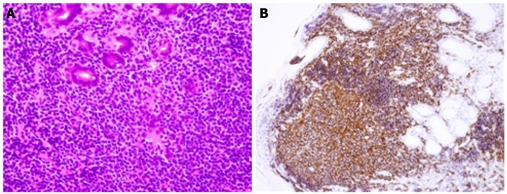
Figure 3.
Histology of biopsy samples. A: Histopathologic findings revealed hyperplasia of atypical centrocyte-like cells with small to medium-sized, ovoid nuclei and clear cytoplasm in the lamina propria mucosae and their infiltration among glandular epithelial cells, suggesting a lymphoepithelial lesion (hematoxylin and eosin stain, × 600); B: Immunohistochemistry. The lesion was positive for CD20 (× 200).
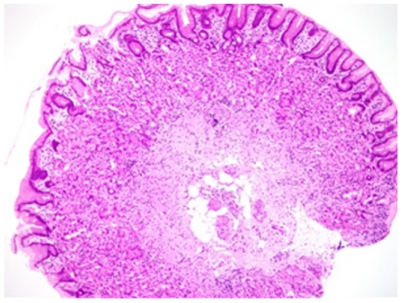
Figure 4.
Histology of biopsy samples revealed only infiltration of inflammatory cells such as lymphocytes, plasma cells, and eosinophils in the gastric mucosa with foveolar hyperplasia (hematoxylin and eosin stain, ×100 ).
Table 1.
Biopsy results in the presence or absence of abnormal blood vessels
| Diagnosis | ||||
| MALT lymphoma | Others | Total | ||
| Abnormal blood vessels | Present | 8 | 2 | 10 |
| Absent | 2 | 8 | 10 | |
MALT: Mucosa-associated lymphoid tissue.
DISCUSSION
In this case study, we have clearly shown that target biopsies from a suspected MALT lymphoma based on ME with NBI are useful in the histological diagnosis of gastric MALT lymphoma. Gastric MALT lymphoma is often misdiagnosed as gastric ulcer, gastritis, and early gastric cancer by endoscopy and the diagnostic accuracy of the initial endoscopy has been shown to range from 11% to 22%, and from 50%-75% with biopsy histology[12-14]. The potential reasons for this are that MALT lymphoma accounts for only 1% to 7% of gastric malignant tumors[1,3-4], MALT lymphoma is not taken into account at examination, multiple occurrence and a large variety of endoscopic findings[2] and difficulty in diagnosis with small biopsy samples.
In addition, MALT lymphoma cells are present near the lamina muscularis mucosae in many cases, and this makes pathological diagnosis by biopsy difficult.
In this case report, we have shown that the tree-like appearance of the abnormal blood vessels, clearly observed by ME with NBI, could be one of the unique features suggestive of gastric MALT lymphoma. This finding could be helpful as superficial depressed-type lesions potentially include circumscribed atrophic gastritis and poorly-differentiated adenocarcinoma. Nakamura et al[15-16] studied mouse gastric MALT lymphoma and reported that VEGF activity in the gastric MALT lymphoma area can potentially induce angiogenesis, and therefore, a rich vascular system is observed in this area compared with normal areas. Further study is necessary to determine whether VEGF also contributes to the generation of abnormal blood vessels observed in human gastric MALT lymphoma. Our study was focused on the abnormal vascular pattern in gastric MALT lymphoma, in agreement with a previous report on abnormal vessels on ME[10]. Of note, these vascular findings are relatively easy to detect using NBI, because NBI can show clearly defined vascular images. Therefore, our report also suggests the importance of NBI for the endoscopic evaluation of gastric MALT lymphoma.
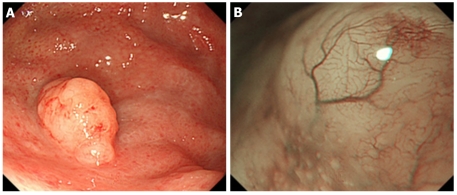
To further characterize these NBI findings of MALT lymphoma, the resected specimen from another patient with gastric MALT lymphoma (different from the patient in this case report) was compared with our patient’s NBI findings. As shown in Figure 5A, a 10-mm elevated lesion was observed in the greater curvature of the gastric fornix. On NBI, the mucosa which had lost its glandular structure and appeared shiny showed a TLA (Figure 5B). Histological examination of the EMR specimen revealed that the gastric mucosa was infiltrated by medium-sized atypical lymphocytes, and the glandular structure was destroyed or had disappeared (Figure 6A). These findings were consistent with loss of the glandular structure. Immunostaining was positive for CD20 and Bcl-2, and negative for CD3, CD10, and Cyclin D1, leading to a diagnosis of gastric MALT lymphoma. CD34 staining showed unusual microvessels running transversely immediately under the superficial layer of the mucosa, which may correspond to the TLA, as visualized by NBI (Figure 6B). These findings suggest that the mucosa showing the TLA on NBI reflects marked lymphoma cell infiltration and the associated angiogenesis, thereby providing very useful information for the selection of optimal biopsy sites.
Figure 5.
Endoscopic findings of gastric mucosa-associated lymphoid tissue lymphoma. A: An elevated lesion, 10 mm in diameter, was observed in the greater curvature of the gastric fornix; B: Narrow band imaging findings. The mucosa that had lost its glandular structure, appeared shiny and had a tree-like appearance.
Figure 6.
Histopathological examination of endoscopic mucosal resection specimen. A: The mucosa was infiltrated by medium-sized atypical lymphocytes forming follicle-like structures. (hematoxylin and eosin stain, × 100 ); B: CD34. Unusual microvessels were observed running transversely immediately under the superficial layer of the mucosa (× 200).
Since this report only included one patient and further studies involving more patients are needed, our study suggests that the TLA, observed by ME with NBI, is a good indicator of the infiltration of MALT lymphoma. Because endoscopic features of gastric MALT lymphoma are diverse and the diagnosis often depends on biopsy, ME with NBI would be very helpful in identifying possible multifocal distribution from the mixture of normal and abnormal appearing gastric mucosa. The combination of ME with NBI may also reduce the number of biopsies before and even after the treatment of gastric MALT lymphoma because it can provide precise information about the distribution of MALT lymphoma in the stomach.
In general, if the lesion disappeared after eradication therapy and changed into atrophic-like mucosa under conventional endoscopy, it is considered a complete remission[17]. However, in some patients, lesions, such as ill-delineated, brownish depressions, do not change into clear, atrophic-like mucosa even after remission. Even in such cases, we consider it useful to evaluate the presence or absence of the TLA by ME with NBI. There are no clear guidelines for the recommended interval and duration of follow-up endoscopy. However, since some patients reportedly show recurrence after complete remission, long-term follow-up is required[18-20]. We regularly perform follow-up ME with NBI every 2-3 mo during the first year.
Footnotes
Peer reviewer: Marmo Riccardo, Postgraduate Specialist, Gastroenterology Unit, Azienda Sanitaria Locale Salerno, Presidio Ospedaliero Polla, Via Luigi Curto Polla 84037, Italy
S- Editor Yang XC L- Editor Webster JR E- Editor Yang XC
References
- 1.Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 1983;52:1410–1416. doi: 10.1002/1097-0142(19831015)52:8<1410::aid-cncr2820520813>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 2.Wotherspoon AC, Doglioni C, Isaacson PG. Low-grade gastric B-cell lymphoma of mucosa-associated lymphoid tissue (MALT): a multifocal disease. Histopathology. 1992;20:29–34. doi: 10.1111/j.1365-2559.1992.tb00912.x. [DOI] [PubMed] [Google Scholar]
- 3.Wotherspoon AC, Finn TM, Isaacson PG. Trisomy 3 in low-grade B-cell lymphomas of mucosa-associated lymphoid tissue. Blood. 1995;85:2000–2004. [PubMed] [Google Scholar]
- 4.Kita H. EUS to predict cure of gastric mucosa-associated lymphoma after Helicobacter pylori eradication. Gastrointest Endosc. 2007;65:97–98. doi: 10.1016/j.gie.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 5.The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc. 2003;58:S3–43. doi: 10.1016/s0016-5107(03)02159-x. [DOI] [PubMed] [Google Scholar]
- 6.Yao K, Oishi T, Matsui T, Yao T, Iwashita A. Novel magnified endoscopic findings of microvascular architecture in intramucosal gastric cancer. Gastrointest Endosc. 2002;56:279–284. doi: 10.1016/s0016-5107(02)70194-6. [DOI] [PubMed] [Google Scholar]
- 7.Nakagawa S, Kato M, Shimizu Y, Nakagawa M, Yamamoto J, Luis PA, Kodaira J, Kawarasaki M, Takeda H, Sugiyama T, et al. Relationship between histopathologic gastritis and mucosal microvascularity: observations with magnifying endoscopy. Gastrointest Endosc. 2003;58:71–75. doi: 10.1067/mge.2003.316. [DOI] [PubMed] [Google Scholar]
- 8.Otsuka Y, Niwa Y, Ohmiya N, Ando N, Ohashi A, Hirooka Y, Goto H. Usefulness of magnifying endoscopy in the diagnosis of early gastric cancer. Endoscopy. 2004;36:165–169. doi: 10.1055/s-2004-814184. [DOI] [PubMed] [Google Scholar]
- 9.Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video) Endoscopy. 2004;36:1080–1084. doi: 10.1055/s-2004-825961. [DOI] [PubMed] [Google Scholar]
- 10.Ono S, Kato M, Ono Y, Itoh T, Kubota K, Nakagawa M, Shimizu Y, Asaka M. Characteristics of magnified endoscopic images of gastric extranodal marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue, including changes after treatment. Gastrointest Endosc. 2008;68:624–631. doi: 10.1016/j.gie.2008.02.066. [DOI] [PubMed] [Google Scholar]
- 11.Nonaka K, Ishikawa K, Shimizu M, Sakurai T, Nakai Y, Nakao M, Yoshino K, Arai S, Kita H. Education and Imaging. Gastrointestinal: gastric mucosa-associated lymphoma presented with unique vascular features on magnified endoscopy combined with narrow-band imaging. J Gastroenterol Hepatol. 2009;24:1697. doi: 10.1111/j.1440-1746.2009.06030.x. [DOI] [PubMed] [Google Scholar]
- 12.Yokoi T, Nakamura T, Nakamura S. Differential diagnosis of gastric MALT lymphomas. Stomach and Intestine. 2001;36:13–20. [Google Scholar]
- 13.Sugino Y, Imai Y, Huse S, Suzuki K, Kuribayashi Y, Mukai M, Ishiki S, Oya Y, Kubota T, Kitajima M, et al. Radiological diagnosis on superficial-type malignant lymphoma in the stomach -Differential diagnosis from early gastric cancer. Stomach and Intestine. 2001;36:29–39. [Google Scholar]
- 14.Taal BG, Boot H, van Heerde P, de Jong D, Hart AA, Burgers JM. Primary non-Hodgkin lymphoma of the stomach: endoscopic pattern and prognosis in low versus high grade malignancy in relation to the MALT concept. Gut. 1996;39:556–561. doi: 10.1136/gut.39.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakamura M, Matsui H, Murayama SY, Matsumoto T, Yamada H, Takahashi S, Tsuchimoto K. Interaction of VEGF to gastric low grade MALT lymphoma by Helicobacter heilmannii infection in C57/BL/6 mice. Inflammopharmacology. 2007;15:115–118. doi: 10.1007/s10787-007-1549-5. [DOI] [PubMed] [Google Scholar]
- 16.Nakamura M, Takahashi S, Matsui H, Murayama SY, Aikawa C, Sekiya Y, Nishikawa K, Matsumoto T, Yamada H, Tsuchimoto K. Microcirculatory alteration in low-grade gastric mucosa-associated lymphoma by Helicobacter heilmannii infection: its relation to vascular endothelial growth factor and cyclooxygenase-2. J Gastroenterol Hepatol. 2008;23 Suppl 2:S157–160. doi: 10.1111/j.1440-1746.2008.05554.x. [DOI] [PubMed] [Google Scholar]
- 17.Ono S, Kato M, Ono Y, Nakagawa M, Shimizu Y, Asaka M. Magnified endoscopic images of gastric MALT lymphoma before and after treatment. Endoscopy. 2007;39 Suppl 1:E328. doi: 10.1055/s-2007-966826. [DOI] [PubMed] [Google Scholar]
- 18.Zucca E, Dreyling M. Gastric marginal zone lymphoma of MALT type: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 Suppl 5:v175–v176. doi: 10.1093/annonc/mdq182. [DOI] [PubMed] [Google Scholar]
- 19.Ono S, Kato M, Takagi K, Kodaira J, Kubota K, Matsuno Y, Komatsu Y, Asaka M. Long-term treatment of localized gastric marginal zone B-cell mucosa associated lymphoid tissue lymphoma including incidence of metachronous gastric cancer. J Gastroenterol Hepatol. 2010;25:804–809. doi: 10.1111/j.1440-1746.2009.06204.x. [DOI] [PubMed] [Google Scholar]
- 20.Zullo A, Hassan C, Cristofari F, Perri F, Morini S. Gastric low-grade mucosal-associated lymphoid tissue-lymphoma: Helicobacter pylori and beyond. World J Gastrointest Oncol. 2010;2:181–186. doi: 10.4251/wjgo.v2.i4.181. [DOI] [PMC free article] [PubMed] [Google Scholar]