Abstract
Objective
We sought to examine trends in the race-specific incidence of acute respiratory failure in the United States.
Design
Retrospective cohort study.
Setting
We used the National Hospital Discharge Survey (NHDS) database (1992-2007), an annual survey of approximately 500 hospitals weighted to provide national hospitalization estimates.
Patients
All incident cases of noncardiogenic acute respiratory failure hospitalized in the United States.
Interventions
None
Measurements and Main Results
We identified noncardiogenic acute respiratory failure by the presence of ICD–9 codes for respiratory failure or pulmonary edema (518.4, 518.5, 518.81, 518.82) and mechanical ventilation (96.7x), excluding congestive heart failure. Incidence rates were calculated using yearly census estimates standardized to the age and sex distribution of the 2000 census population. Annual cases of noncardiogenic acute respiratory failure increased from 86,755 in 1992 to 323,474 in 2007. Noncardiogenic acute respiratory failure among black Americans increased from 56.4 (95% CI 39.7 – 73.1) to 143.8 (95% CI 123.8 – 163.8) cases per 100,000 in 1992 and 2007, respectively. Among white Americans, the incidence of noncardiogenic acute respiratory failure increased from 31.2 (95% CI 26.2-36.5) to 94.0 (95% CI 86.7 – 101.2) cases per 100,000 in 1992 and 2007, respectively. The average annual incidence of noncardiogenic acute respiratory failure over the entire study period was 95.1 (95% CI 93.9 – 96.4) cases per 100,000 for black Americans compared to 66.5 (95% CI 65.8 – 67.2) cases per 100,000 for white Americans (rate ratio = 1.43, 95% CI 1.42-1.44). Overall in–hospital mortality was greater for other-race Americans, but only among patients with ≥ 2 organ failures (57% [95% CI 56-59%] for other-race, 51% [95% CI, 50-52%] for white, 50% [95% CI, 49-51%] for black).
Conclusions
The incidence of noncardiogenic acute respiratory failure in the United States increased between 1992 and 2007. Black and other-race Americans are at greater risk of developing noncardiogenic acute respiratory failure compared to white Americans.
Keywords: Respiratory failure, health status disparities, epidemiology, National Hospital Discharge Survey, international classification of diseases, acute lung injury
Introduction
The literature documenting racial and ethnic disparities in health and healthcare is extensive.(1) Recently, there has been an increasing recognition of racial and ethnic differences in the incidence and outcomes of critical illnesses(2-4). Although the incidence of sepsis among black patients is greater than white patients(3), the influence of race on the incidence of acute respiratory failure has not been well investigated(5). One population-based epidemiologic study found that black men had the highest annual age-adjusted mortality rate from acute respiratory distress syndrome (ARDS), the most severe form acute respiratory failure, compared with other racial/ethnic and gender subgroups (12.8 per 100,000 compared to 9.1 per 100,000 for white men)(6); however, several other reports in have found no association between race and acute lung injury (ALI)(7, 8). Whether this higher number of deaths reflects a higher incidence of acute respiratory failure among black patients, a higher case-fatality from acute respiratory failure, or both, remains unknown.
Obtaining prospective national epidemiologic estimates of acute respiratory failure among racial and ethnic minorities would be difficult and impractical, and data from a limited population or a short time period may be inaccurate. Prior population-based studies of patients with acute respiratory failure were conducted in regions of the country with racial distributions that are significantly different than the US population as a whole and did not discuss the contribution of race. Specifically, these studies derived from regions of the US with small proportions of black Americans(9, 10), or were conducted in Europe(11). Using a data set that can provide national estimates is therefore necessary for better estimation of the incidence of acute respiratory failure among non-white Americans.
We sought to determine the incidence of acute respiratory failure among Americans stratified by race using nationally collected data from 1992 through 2007. Specifically, we wanted to evaluate whether there were racial differences in the incidence and outcomes of acute respiratory failure over time.
Materials and Methods
Data source
The National Center for Health Statistics has conducted the National Hospital Discharge Survey (NHDS) continuously since 1965. The NHDS is composed of a sample of all nonfederal acute care hospitals in the United States, including approximately 500 hospitals, with equal representation of all geographic regions(12). The database is constructed through the surveying of discharge records for inpatients from each participating hospital, representing approximately 1 percent of all hospitalizations, or 350,000 discharges annually in the United States. Discharge records are abstracted for demographic information (age, sex, race, ethnicity, geographic location, and marital status), seven diagnostic codes and four procedural codes from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), dates of hospital admission and discharge, sources of payment, and disposition at discharge.
Definitions
Cases were identified from discharge records in the NHDS from 1992-2007. We defined noncardiogenic acute respiratory failure as the presence the following codes among any of the seven collected ICD-9-CM diagnosis fields: 518.4 (acute edema of lung), 518.5 (pulmonary insufficiency following trauma and surgery), 518.81 (acute respiratory failure), and 518.82 (other pulmonary insufficiency, not elsewhere classified). We excluded patients with a cardiogenic cause (428.0-428.9) as these patients have a distinct pathophysiology of respiratory failure that differs from other causes. Patients needed to be mechanically ventilated as indicated by the procedural codes 96.7x (mechanical ventilation) to further increase the specificity for acuity of the respiratory failure(13). The procedural code for mechanical ventilation was introduced in the fourth quarter of 1991, thus we chose 1992, the first complete calendar year in which this code was used, as the start date for our study. To identify the underlying risk for acute respiratory failure in each patient we identified severe sepsis(14) (Box E1, Supplementary Digital Content), pneumonia (480-487), aspiration (507.0), acute pancreatitis (577.0) or trauma (E800-929). We identified organ failures using a previously defined combination of ICD-9 diagnosis and procedure codes as presented in Table E1 (Supplemental Digital Content)(14). With the exception of hypertension (ICD-9 401-405.9, 437.2), all chronic co-morbid medical conditions were identified from ICD-9 codes using an established co-morbidity index (Charlson-Deyo score)(15, 16). We defined case-fatality as the proportion of patients with acute respiratory failure who were dead at hospital discharge.
Race definitions and missing data
The NHDS race designation is limited to the mutually exclusive groups of white, black, Asian/Pacific Islander, American Indian/Alaskan Native, or other based upon administrative claims. Hispanic ethnicity is not collected in the database. However, NHDS only provides relative standard errors for three race groups: white, black, and other as these three groups are the most reliably coded(17). As such, we collapsed patients with Asian/Pacific Islander and American Indian/Alaskan Native into other race. Approximately 20% of discharges in the sample of the NHDS did not have race collected(18). This is largely because many hospitals in the NHDS report race for less than 3% of discharges. The hospitals that under report data on race tend to have a higher proportion of white discharges than hospitals that report race(18). Thus, excluding patients with missing race data may under estimate incidence rates for all race groups and bias comparisons between racial groups.
To overcome this potential for bias, we performed multiple imputation to determine the race for the 20% of discharges for whom race was not collected thereby including all observed cases of acute respiratory failure(19, 20). This technique involves an iterative process of multiple regression switching (multiple imputation by chained equations) to estimate the race for those in whom race is not collected, conditional on the observed data for patients with and without race(21, 22). We generated 40 imputed datasets and combined them using traditional methods(20, 23, 24). Additional details of the imputation procedure are presented in the online methods (Supplemental Digital Content, Methods).
Statistical analysis
Incidence rates were calculated using the population age, racial, and gender distribution for each year provided by the US Census, and were standardized to the 2000 US census distribution using direct standardization(25). All estimates are presented according to accepted guidelines for the accuracy of NHDS data. Specifically, only absolute, unweighted samples of more than 60 patients with relative standard error (RSE) measures of less than 30 percent were included in data analyses. The RSE was calculated as a first-order Taylor-series approximation as outlined in the RSE tables of the NHDS documentation(26). The standard error for each estimate was calculated by first multiplying the RSE by the estimated incidence or proportion within each imputation, and then combining standard errors for each imputation using Rubin’s rules to get a single estimate of each standard error(24). Then, 95 percent confidence intervals were calculated from these standard errors. We plotted incidence rates over time and examined the proportion of patients with ≥ 2 organ failures over time to characterize severity of illness. Data for continuous variables were compared with t-tests and data for categorical variables were compared with the chi-square test, as appropriate for the variable. Analyses were performed with SAS version 9.2 (SAS Institute, Cary, NC) and Stata 11 (Statacorp, College Station, TX). The study was exempt from IRB review because the data was previously collected, deidentified, and publicly available.
Sensitivity analysis
We performed several sensitivity analyses to assess the impact of our methods and the underlying patient diagnoses on our results. Although multiple imputation should produce a less biased estimate of acute respiratory failure incidence than complete case analysis(19), there is a possibility that any difference in the disease incidence across race groups may be attributable to the misclassification of race among patients with missing data during the imputation process. While our calculated standard errors account for uncertainty in the imputed race estimate, we further assessed the robustness of our results to how patients with missing race were handled by performing an additional “worst case” analysis. In this analysis we assigned all patients who were missing race to the white race group. We then repeated our incidence calculations for black and “white” (white + missing race) patients. This analysis is “worst case” because provides the most conservative estimate of the effect the missing data had on black vs. white differences in acute respiratory failure incidence and case-fatality.
We also calculated the incidence rate ratio between black and white patients for each year for complete cases and compared it to that generated from the multiple imputation analysis. Finally, in two separate analyses, we calculated the yearly incidence rate ratios between black and white patients after excluding patients with the ICD-9 code 518.4 – acute edema of the lung and patients with a history of chronic renal disease (using Charlson-Deyo) or hypertension. By excluding these patients we reduce the likelihood that any observed differences in acute respiratory failure across race is attributed to differing distributions of volume associated pulmonary edema or risk factors for volume associated pulmonary edema.
Results
From 1992 through 2007, there were approximately 3.2 million discharges with noncardiogenic acute respiratory failure in the US Of these patients, 652,452 (20.0%) were missing data for race. The demographic and clinical characteristics for patients in the cohort are summarized in Table 1. White patients were older on average and more likely to be female compared with non-white patients. Black patients had greater organ failures than white patients, more comorbid conditions than other race groups and were more likely to have hypertension, diabetes, end stage renal disease, and HIV/AIDS.
Table 1.
Characteristics of patients with noncardiogenic acute respiratory failure, 1992-2007, by race
| Characteristic* | White (N=1,987,431) |
Black (N=458,624) |
Other (N=160,499) |
Missing (N=652,452) |
|---|---|---|---|---|
| Age, years | 59 (23) | 52 (23) | 53(26) | 57 (23) |
| Male (%) | 52 | 55 | 54 | 55 |
| Primary expected source of payment (%) |
||||
| Medicare | 51 | 40 | 37 | 46 |
| Private | 27 | 21 | 21 | 26 |
| Medicaid | 12 | 26 | 26 | 17 |
| Self-pay / none | 5 | 7 | 9 | 7 |
| Other | 5 | 6 | 7 | 4 |
| Number of comorbidities (%) |
||||
| 0 | 36 | 33 | 38 | 38 |
| 1 | 35 | 37 | 38 | 36 |
| 2 | 21 | 22 | 19 | 19 |
| ≥3 | 7 | 8 | 5 | 7 |
| Comorbid conditions (%) |
||||
| COPD | 31 | 24 | 22 | 29 |
| Hypertension | 17 | 25 | 15 | 16 |
| Diabetes | 9 | 11 | 10 | 8 |
| Cancer | 8 | 7 | 8 | 6 |
| Cirrhosis | 1.4 | 1 | 4 | 2 |
| End stage renal disease |
3 | 5 | 3 | 3 |
| HIV/AIDS | 0.8 | 5 | 4 | 1 |
| Number of organ failures (%) |
||||
| 1 | 71 | 69 | 70 | 71 |
| 2 | 23 | 25 | 24 | 23 |
| 3+ | 5 | 6 | 6 | 7 |
| Length of hospital stay, days, median (IQR) |
9 (4-16) | 9 (4-18) | 10 (4-17) | 8 (3-16) |
Data presented as mean (SD) unless otherwise noted. Percentages may not add to 100 due to rounding.
Incidence
During the 16-year study period, the number of patients meeting our definition of noncardiogenic acute respiratory failure increased from 86,755 in 1992 to 323,474 in 2007. The overall age, sex, and race-adjusted mean annual incidence after imputation was 74.1 (95% CI 73.2 – 74.9) cases per 100,000 population, increasing from 36.1 (95% CI 30.8 – 41.4) per 100,000 population in 1992 to 106.1 (95% CI 99.3 – 112.9) per 100,000 population in 2007. The incidence of acute respiratory failure among black Americans was greater in each year over the study period, compared to white Americans (Figure 1). Acute respiratory failure among black Americans increased from 56.4 (95% CI 39.7 – 73.1) to 143.8 (95% CI 123.8 – 163.8) cases per 100,000 in 1992 and 2007, respectively. Among white Americans, the incidence of acute respiratory failure increased from 31.2 (95% CI 26.2-36.5) to 94.0 (95% CI 86.7 – 101.2) cases per 100,000 over the same time period. Incidence rates for other-race increased from 70.2 (95% CI 43.5 - 97.8) to 106.5 (95% CI 80.3-132.8) cases per 100,000 in 1992 and 2007, respectively. However, incidence rates for other-race Americans were highly unstable, showing a large drop from 159 to 97 cases per 100,000 persons between 1999 and 2000. This was attributable to a 31% increase in the population (denominator) of other-race Americans measured by the 2000 census (17,684,298) compared to that estimated for 1999 by the US census (13,450,403). Between 2000 and 2007, incidence rates for other-race Americans were relatively flat.
Figure 1.
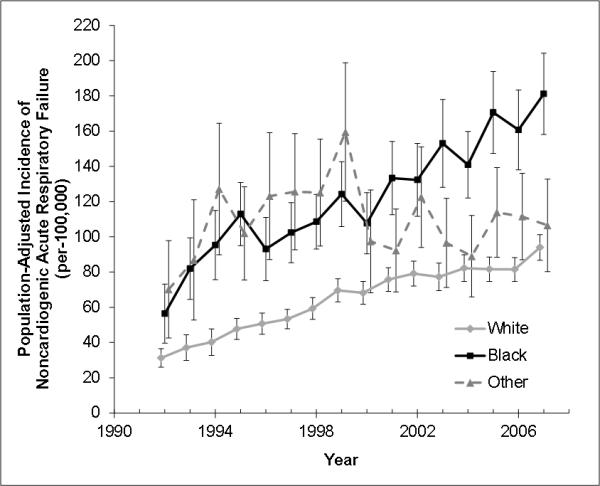
Incidence of noncardiogenic acute respiratory failure in the United States by race (1992-2007). Incidence rates are calculated using the age and sex distribution for each year as estimated by the US Census and standardized to the age and sex distribution of the 2000 US Census. Error bars represent 95% confidence intervals incorporating uncertainty of the multiple imputation process and the complex survey design of the National Hospital Discharge Survey.
The mean annual incidence of noncardiogenic acute respiratory failure (cases per 100,000 population ) over the entire study period was 65.0 (95% CI 64.3 – 65.6) for white Americans, 123.6 (95% CI 122.0 –125.3) for black Americans, and 108.8 (95% CI 106.2 – 111.3) for other Americans (rate ratio for black = 1.90, 95% CI 1.88 -1.92, other = 1.63, 95% CI 1.60-1.67, vs, white). Age and race-adjusted incidence rates for acute respiratory failure among men were consistently greater than women over the entire study period (Figure 2).
Figure 2.
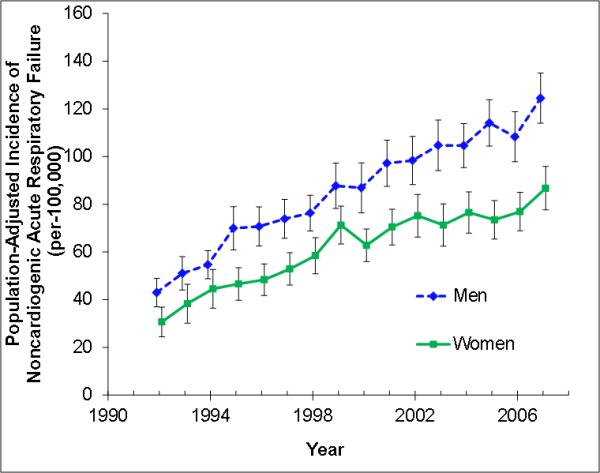
Incidence of noncardiogenic acute respiratory failure in the United States by sex (1992-2007). Incidence rates are calculated using the age and race distribution for each year as estimated by the US Census and standardized to the age and sex distribution of the 2000 US Census. Error bars represent 95% confidence intervals incorporating uncertainty of the multiple imputation process and the complex survey design of the National Hospital Discharge Survey.
Outcomes
Although incidence was greatest for black Americans, severity of illness and hospital mortality were similar across race groups. The proportion of patients with two or more organ failures increased over time from 23% (95% CI 17-29%) in 1992 to 44% (95% CI 41-47%) in 2007 as shown in Figure E1 (Supplemental Digital Content). There was a steady decline in case-fatality for all Americans between 1992 and 2007 (Figure 3). Case-fatality was greater among patients with two or more organ failures (n=953,188) and fluctuated widely over time for this smaller group, but declined between 1992 and 2007 for all race groups regardless of the number of organ failures. Aggregate case fatality [95% CI] over the 16 year period did not vary appreciably by race in patients with < 2 organ failures (25% [24.7-25.3], 23% [22.8-23.4%], 25% [24.2-25.5%] for white, black, other race, respectively; p=0.07), but among patients with ≥ 2 organ failures mortality was greatest among the other-race group (51% [50-52%], 50% [49-51%] and 57% [56-59%] for white, black, other-race, respectively; p<0.001). Although statistically significant, case-fatality for the entire study period among patients with acute respiratory failure did not vary meaningfully by sex (32.0% [31.9-32.1%] for men vs. 32.9% [32.8-33.0%] for women).
Figure 3.
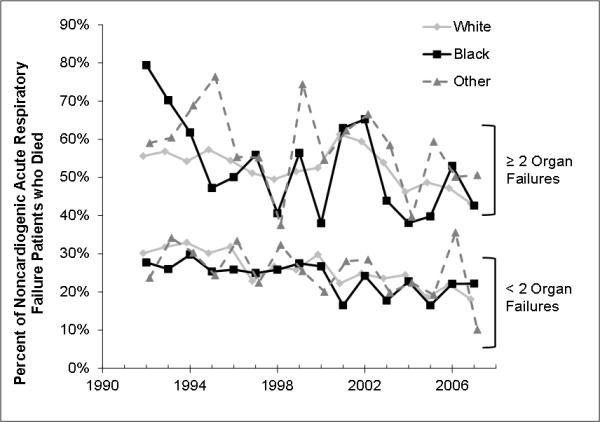
Percent of noncardiogenic acute respiratory failure patients who died during their hospital stay in the United States by race (1992-2007), by the number of organ failures. Estimates are based upon the mean of the multiply imputed data and the complex survey design of the National Hospital Discharge Survey. Organ failures calculated using standard definitions.(14) Error bars have been removed to improve clarity of interpretation.
Among patients with observed race, black patients had minimally greater differences in the rate of severe sepsis compared to white patients (Table 2). This relationship persisted after multiple imputation of race. For example, the age and gender adjusted rate (95% CI) of sepsis among white, black, and other-race patients with acute respiratory failure was 41.7 % (41.3-42.2), 42.5% (41.8-43.0%), and 42.5 (41.5-43.6), respectively. The rate of severe sepsis among patients with acute respiratory failure increased over the study period for all race groups while rates of pneumonia remained relatively constant. (Figure E2, Supplemental Digital Content). White patients were the least likely to be discharged home and more likely to be transferred to a long-term or short-term care facility compared to all other race groups (Table 3).
Table 2.
At-risk conditions for patients with noncardiogenic acute respiratory failure, 1992-2007, by race
| At-risk condition (%)*† | White (N=1,987,431) |
Black (N=458,624) |
Other (N=160,499) |
|---|---|---|---|
| Severe sepsis | 42 | 43 | 43 |
| Pneumonia | 29 | 27 | 29 |
| Aspiration | 15 | 13 | 14 |
| Trauma | 7 | 5 | 10 |
| Overdose/ poisoning |
6 | 3 | 3 |
| Pancreatitis | 2 | 3 | 3 |
| None / other | 38 | 41 | 37 |
Includes only patients with recorded race. Numbers to not add to 100% because categories are not mutually exclusive
P<0.01 for all comparisons across race
Table 3.
Discharge disposition of patients with ALI, 1992-2007, by race
| Discharge Disposition (%)*† | White (N=1,987,431) |
Black (N=458,624) |
Other (N=160,499) |
|---|---|---|---|
| Died | 34 | 33 | 35 |
| Home | 34 | 39 | 39 |
| Long-term care facility | 14 | 12 | 12 |
| Short-term care facility | 9 | 7 | 7 |
| Discharged against medical advice |
0.9 | 1.4 | 0.8 |
| Unknown | 8 | 7 | 6 |
Includes only patients with observed race. Percentages may not add to 100% due to rounding
P<0.01 for all comparisons across race
Sensitivity analysis
On the “worst-case” analysis, when all patients with missing race data were assumed to be white, the incidence of acute respiratory failure across the 16 year study period was still significantly greater among black (100.1 [95% CI 98.8 – 101.5] cases / 100,000 population) compared to white Americans (69.0 [95% CI 68.3-69.7] cases / 100,000 population). These rates resulted in an incidence rate ratio of respiratory failure (95% CI) for black Americans of 1.45 (1.42-1.47). Complete case analysis yielded black versus white incidence rate ratios that were almost identical to the multiple imputation analysis (Table E2, Supplemental Digital Content). Yearly age and gender-adjusted incidence estimates by race for this sensitivity analysis are presented in Figure E3 (Supplemental Digital Content). Excluding patients with ICD-9 code of 518.4 and those with chronic renal failures or hypertension resulted in no to minimal changes in the incidence rate ratios for black versus white patients (Table E2, Supplemental Digital Content).
Discussion
Using a nationally representative sample of hospital discharges in the United State, we determined that there were significant racial differences in the incidence of noncardiogenic acute respiratory failure from 1992-2007. Black Americans had approximately 1.9 times the incidence and other-race patients had 1.6 times the incidence of acute respiratory failure of white Americans. There was no clinically important difference in case-fatality between black and white patients with acute respiratory failure, but other-race patients with ≥ 2 organ failures experienced greater case-fatality than white patients. Men had a higher annual incidence of acute respiratory failure compared to women. Overall, there was a substantial increase in the incidence of acute respiratory failure between 1992 and 2007 with an increasing number of total deaths despite a decline in overall case-fatality.
Our data estimate the incidence of acute respiratory failure in the US at 74.1 cases per 100,000 person-years. Although our estimate is somewhat lower than those previously published, by excluding patients with a cardiogenic cause for respiratory failure we reduced incidence estimates relative to these publications (5, 11, 27-29). For example, several investigators estimated the incidence of acute respiratory failure in a single state or the US as a whole to be between 137 to 270 per 100,000(5, 27, 29). Outside of the US, estimates of acute respiratory failure range from to 78 per 100,000 in Sweden, Denmark and Iceland to 217 per 100,000 in Ontario, Canada(11, 28). These prior studies examined all patients receiving mechanical ventilation, regardless indication, or examined mechanically ventilated patients with an acute respiratory failure diagnosis code. All included patients with congestive heart failure. Our results are therefore consistent with prior estimates of the incidence of respiratory failure.
Although the causes for respiratory failure among our cohort are heterogeneous, acute lung injury is likely a major contributor. This is supported by evidence suggesting that our definition includes many patients with ALI. No study has rigorously validated the use of ICD-9 coding for the diagnosis of ALI, though several studies that examined various administrative definitions of ALI exist(9, 13, 30, 31). Using ICD-9 codes similar to those employed in our analysis, these studies suggest that the specificity of ICD-9 codes for ALI or ARDS is excellent (>90%) while the sensitivity is low (48-88%). Notably, the addition of mechanical ventilation codes and the exclusion of heart failure codes, the approach employed in our analysis, increases the specificity of the codes for ALI(31). In addition, more than 60% of patients in our analysis have risk factors consistent with traditional risk factors for acute lung injury. Nevertheless, because we were unable to determine if patients met the American European Consensus Conference definition for ALI, we recognize that a sizeable proportion of cases in our analysis represent patients with other causes of respiratory failure. These include diagnoses such as unilateral pneumonia, COPD or asthma, or pulmonary edema secondary to non-cardiac volume overload, such as that which may occur in the setting of renal failure,
Our data also indicate that black Americans have a greater incidence of acute respiratory failure compared to white patients, but a similar case-fatality. Our results suggest that the greater population-based rates of death for black patients with acute respiratory failure secondary to ALI described by Moss and colleagues(6) may result from differences in ALI incidence rather than in ALI case fatality. There are several possible explanations for this finding. First, black Americans are at higher risk for developing at-risk conditions for acute respiratory failure such as sepsis and potentially other conditions that increase the risk of pulmonary edema such as acute renal disease(2, 3). The underlying mechanism behind racial differences in sepsis and other predisposing conditions for acute respiratory failure among black Americans are multifactorial, but likely include a combination of differences in chronic disease burden, social and environmental differences, or potentially genetic susceptibility to infection. Second, black Americans also have greater severity of illness at the time of ICU admission which may reflect a greater delay in presentation or perhaps a delay in diagnosis of an at risk condition(32). The greater organ dysfunction seen among black patients in our cohort supports this prior work. Third, care delivered to critically ill black patients may be different than care delivered to white patients(32) which may result from black patients receiving care in lower quality hospitals(3, 33-35). These are just several of the potential mechanisms underlying the greater rates of acute respiratory failure among black Americans that warrant further study.
We found no clinically significant difference in case-fatality between black and white patients, while other-race patients were at greater risk of death. We caution over interpretation of this result as prior work suggests that black patients are at greater risk of death once acquiring acute respiratory failure and our study was not powered to detect equivalence in case-fatality across race groups(4, 36). Although nationally representative, estimates for case-fatality for black and other-race patients were based upon relatively small numbers and, when combined with the variability that results from the NHDS sampling design, were quite unstable. Nevertheless, further examination of differences in case-fatality across race groups is warranted.
Beyond racial differences, our data corroborate several, but not all, studies suggesting that the incidence of acute respiratory failure among all races is increasing(29, 36, 37). There are several possible explanations for this trend. First, as discussed above, rates of conditions that predispose patients to respiratory failure, such as sepsis or acute renal failure, are increasing over time(2, 38, 39). Second, since the publication of the landmark low tidal volume study by the ARDSnet in 2000(40), there has been much greater focus on identification and appropriately treating patients with ALI(4, 41-44), and in identifying those patients at risk for ALI(45). The greater incidence we observed may partially reflect better documentation of a patient’s risk for ALI or better documentation of ALI itself in the medical and administrative record. Providers may also be more likely to identify ALI among black patients given the expansion in the literature identifying worse outcomes among this group(3, 4, 35). However, we observed no change in the rate of increase in acute respiratory failure over the study period making this explanation less likely. Third, changes to reimbursement practice may have led to greater incentives to use the codes for respiratory failure. This possibility is also less likely given the rising severity of illness for our cohort over time. Even if coding for borderline patients has increased this more likely reflects appropriate coding among previously unidentified patients rather than fraudulent coding among those without disease.
There are several limitations that should be considered when interpreting our study results. First, we used ICD-9 codes to identify acute respiratory failure and its underlying causes. As a result, the large increase in the incidence of acute respiratory failure from 1992-2007 while consistent with other national trends in mechanical ventilation and sepsis(2, 28, 29, 39), may be a result of change in procedural or diagnostic coding. For example, the procedural code for mechanical ventilation was required for our definition of respiratory failure, and because this code was introduced in 1991, it may not have been readily coded into medical records in the early years of the study. This limitation, while potentially artificially lowering incidence rates during the early years of our study, should in no way differentially impact different race groups. Second, The ICD-9 codes that we used to identify respiratory failure also identify a heterogeneous group of illnesses that may include non-cardiogenic causes of pulmonary edema such as ALI, but also respiratory failure from volume overload states such as chronic renal failure. When excluding such patients from our analyses, black patients remained at greater risk of respiratory failure, but the relationship was slightly attenuated. Subsequent research should formally test the validity of each administrative definition of respiratory failure. Third, race categorization was based upon race as assigned in the medical record rather than the more preferred self-reported race(46). Moreover, race was missing in 20% of patients. Although we used multiple imputation and a “worse case” sensitivity analysis to overcome this limitation, incidence rates incorporating missing data are suboptimal. We were also unable to characterize the contribution of ethnicity to the incidence and outcomes of respiratory failure.
Conclusion
We determined that the incidence of noncardiogenic acute respiratory failure in the United States is increasing at the same time that it’s associated case-fatality is declining. Black and other-race Americans are at significantly greater risk of developing acute respiratory failure than white Americans, but only other-race Americans are at greater risk of death. Although race-based differences in acute respiratory failure incidence may in part be driven by greater incidence of at risk conditions such as sepsis among black Americans, sepsis is not solely responsible. Further research should validate administrative definitions of non-cardiogenic respiratory failure and focus on the mechanisms underlying race-based differences in respiratory failure incidence.
Supplementary Material
Acknowledgements
Dr. Cooke had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This work was performed at the University of Michigan and Emory University.
Financial support: This work was possible due to the support of the Robert Wood Johnson Foundation Clinical Scholars program (Dr. Cooke), Atlanta Clinical and Translational Science Institute KL2 RR-025009 (Dr. Erickson), and NIH FD R01-003440 (Dr. Martin).
Footnotes
Dr. Eisner is a full-time employee of Genentech, Inc. Dr. Cooke has not disclosed any potential conflicts of interest.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Smedley BD, Stith AY, Nelson AR, et al. Unequal treatment : confronting racial and ethnic disparities in health care. National Academy Press; Washington, D.C.: 2003. [PubMed] [Google Scholar]
- 2.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 3.Barnato AE, Alexander SL, Linde-Zwirble WT, et al. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med. 2008;177(3):279–284. doi: 10.1164/rccm.200703-480OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erickson SE, Shlipak MG, Martin GS, et al. Racial and ethnic disparities in mortality from acute lung injury. Crit Care Med. 2009;37(1):1–6. doi: 10.1097/CCM.0b013e31819292ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wunsch H, Linde-Zwirble WT, Angus DC, et al. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38(10):1947–1953. doi: 10.1097/CCM.0b013e3181ef4460. [DOI] [PubMed] [Google Scholar]
- 6.Moss M, Mannino DM. Race and gender differences in acute respiratory distress syndrome deaths in the United States: an analysis of multiple-cause mortality data (1979-1996) Crit Care Med. 2002;30(8):1679–1685. doi: 10.1097/00003246-200208000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Ryb GE, Cooper C. Race/ethnicity and acute respiratory distress syndrome: a National Trauma Data Bank study. J Natl Med Assoc. 2010;102(10):865–869. doi: 10.1016/s0027-9684(15)30700-8. [DOI] [PubMed] [Google Scholar]
- 8.Brown LM, Kallet RH, Matthay MA, et al. The influence of race on the development of acute lung injury in trauma patients. Am J Surg. 2011;201(4):486–491. doi: 10.1016/j.amjsurg.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomsen GE, Morris AH. Incidence of the adult respiratory distress syndrome in the state of Utah. Am J Respir Crit Care Med. 1995;152(3):965–971. doi: 10.1164/ajrccm.152.3.7663811. [DOI] [PubMed] [Google Scholar]
- 10.Rubenfeld GD, Caldwell E, Peabody E, et al. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353(16):1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- 11.Luhr OR, Antonsen K, Karlsson M, et al. Incidence and mortality after acute respiratory failure and acute respiratory distress syndrome in Sweden, Denmark, and Iceland. The ARF Study Group. Am J Respir Crit Care Med. 1999;159(6):1849–1861. doi: 10.1164/ajrccm.159.6.9808136. [DOI] [PubMed] [Google Scholar]
- 12.US Department of Health and Human Services. Public Health Service [Last accessed Dec 20, 2010];National Center for Health Statistics National Hospital Discharge Survey 1979-2005. Multi-year Public-Use Data File Documentation. Available at: http://www.cdc.gov/nchs/about/major/hdasd/nhdsdes.htm.
- 13.Howard AE, Courtney-Shapiro C, Kelso LA, et al. Comparison of 3 methods of detecting acute respiratory distress syndrome: clinical screening, chart review, and diagnostic coding. Am J Crit Care. 2004;13(1):59–64. [PubMed] [Google Scholar]
- 14.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 17.Blustein J. The reliability of racial classifications in hospital discharge abstract data. Am J Public Health. 1994;84(6):1018–1021. doi: 10.2105/ajph.84.6.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kozak LJ. Underreporting of race in the National Hospital Discharge Survey. Adv Data. 1995;265:1–12. [PubMed] [Google Scholar]
- 19.Donders AR, van der Heijden GJ, Stijnen T, et al. Review: a gentle introduction to imputation of missing values. J Clin Epidemiol. 2006;59(10):1087–1091. doi: 10.1016/j.jclinepi.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 20.Janssen KJ, Donders AR, Harrell FE, Jr., et al. Missing covariate data in medical research: to impute is better than to ignore. J Clin Epidemiol. 2010;63(7):721–727. doi: 10.1016/j.jclinepi.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 21.van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18(6):681–694. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 22.Carlin JB, Galati JC, Royston P. A new framework for managing and analyzing multiply imputed data in Stata. Stata J. 2008;8(1):49–67. [Google Scholar]
- 23.Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10(4):585–598. doi: 10.1002/sim.4780100410. [DOI] [PubMed] [Google Scholar]
- 24.Marshall A, Altman DG, Holder RL, et al. Combining estimates of interest in prognostic modelling studies after multiple imputation: current practice and guidelines. BMC Med Res Methodol. 2009;9:57. doi: 10.1186/1471-2288-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rothman KJ, Greenland S. Modern epidemiology. 2nd ed Lippincott-Raven; Philadelphia: 1998. [Google Scholar]
- 26.Dennison C, Pokras R. Design and operation of the National Hospital Discharge Survey: 1988 redesign. Vital Health Stat 1. 2000;(39):1–42. [PubMed] [Google Scholar]
- 27.Behrendt CE. Acute respiratory failure in the United States: incidence and 31-day survival. Chest. 2000;118(4):1100–1105. doi: 10.1378/chest.118.4.1100. [DOI] [PubMed] [Google Scholar]
- 28.Needham DM, Bronskill SE, Sibbald WJ, et al. Mechanical ventilation in Ontario, 1992-2000: incidence, survival, and hospital bed utilization of noncardiac surgery adult patients. Crit Care Med. 2004;32(7):1504–1509. doi: 10.1097/01.ccm.0000129972.31533.37. [DOI] [PubMed] [Google Scholar]
- 29.Carson SS, Cox CE, Holmes GM, et al. The changing epidemiology of mechanical ventilation: a population-based study. J Intensive Care Med. 2006;21(3):173–182. doi: 10.1177/0885066605282784. [DOI] [PubMed] [Google Scholar]
- 30.Rubenfeld GD, Caldwell E, Steinberg KP, et al. ICD-9 codes do not accurately identify patients with the acute respiratory distress syndrome (ARDS) [abstract] Am J Respir Crit Care Med. 1998;157:A680. [Google Scholar]
- 31.Poulose JT, Cartin-Ceba R, Shoja A, et al. Comparison of International Classification of Disease-Ninth Revision (ICD-9) Coding with Retrospective Case Review for the Diagnosis of Acute Respiratory Distress Syndrome [abstract] Am J Respir Crit Care Med. 2009;179:A4660. [Google Scholar]
- 32.Williams JF, Zimmerman JE, Wagner DP, et al. African-American and white patients admitted to the intensive care unit: is there a difference in therapy and outcome? Crit Care Med. 1995;23(4):626–636. doi: 10.1097/00003246-199504000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Jha AK, Orav EJ, Li Z, et al. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167(11):1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 34.Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. Jama. 2008;299(18):2180–2187. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- 35.Mayr FB, Yende S, D’Angelo G, et al. Do hospitals provide lower quality of care to black patients for pneumonia? Crit Care Med. 2010;38(3):759–765. doi: 10.1097/CCM.0b013e3181c8fd58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mayr FB, Yende S, Linde-Zwirble WT, et al. Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. Jama. 2010;303(24):2495–2503. doi: 10.1001/jama.2010.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li G, Malinchoc M, Cartin-Ceba R, et al. Eight-year trend of acute respiratory distress syndrome: a population-based study in Olmsted County, Minnesota. Am J Respir Crit Care Med. 2011;183(1):59–66. doi: 10.1164/rccm.201003-0436OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lameire N, Van Biesen W, Vanholder R. The changing epidemiology of acute renal failure. Nat Clin Pract Nephrol. 2006;2(7):364–377. doi: 10.1038/ncpneph0218. [DOI] [PubMed] [Google Scholar]
- 39.Dombrovskiy VY, Martin AA, Sunderram J, et al. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007;35(5):1244–1250. doi: 10.1097/01.CCM.0000261890.41311.E9. [DOI] [PubMed] [Google Scholar]
- 40.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 41.Treggiari MM, Martin DP, Yanez ND, et al. Effect of intensive care unit organizational model and structure on outcomes in patients with acute lung injury. Am J Respir Crit Care Med. 2007;176(7):685–690. doi: 10.1164/rccm.200701-165OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wolthuis EK, Kesecioglu J, Hassink LH, et al. Adoption of lower tidal volume ventilation improves with feedback and education. Respir Care. 2007;52(12):1761–1766. [PubMed] [Google Scholar]
- 43.Cooke CR, Kahn JM, Watkins TR, et al. Cost-effectiveness of implementing low-tidal volume ventilation in patients with acute lung injury. Chest. 2009;136(1):79–88. doi: 10.1378/chest.08-2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cooke CR, Shah CV, Gallop R, et al. A simple clinical predictive index for objective estimates of mortality in acute lung injury. Crit Care Med. 2009;37(6):1913–1920. doi: 10.1097/CCM.0b013e3181a009b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gajic O, Dabbagh O, Park PK, et al. Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2011;183(4):462–470. doi: 10.1164/rccm.201004-0549OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaplan JB, Bennett T. Use of race and ethnicity in biomedical publication. Jama. 2003;289(20):2709–2716. doi: 10.1001/jama.289.20.2709. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


