Abstract
Context:
Oral verrucous hyperplasia (OVH) is a premalignant lesion that may transform into an oral cancer.
Aims:
The present retrospective study was carried out to analyze the clinico-pathological features of verrucous hyperplasia (VH).
Materials and Methods:
Total 19 diagnosed cases of verrucous hyperplasia were retrospectively analyzed for demographic, clinical and histopathological features including dysplasia.
Results:
Average age of occurrence of lesion was 4 th decade of life, with male predominance (2:1) and common site of occurrence being buccal mucosa. Clinically it present as verrucous exophytic growth with sharp or blunt projections on surface, which corresponds histologically. Tobacco lime quid placement in buccal vestibule was key etiologic factor. Histopathologicaly 68% cases showed dysplasia out of which moderate dysplasia predominates (42%). Moderately dysplastic cases were found to be associated with mixed habit pattern. Maximum cases were treated with excision.
Conclusion:
Biopsy specimen comprising of adjacent normal epithelium is key in distinguishing verrucous hyperplasia from verrucous carcinoma. Clinical behavior and recurrence potential needs to be assessed with long term follow up studies.
Keywords: Premalignant lesions, verrucous hyperplasia, verrucous carcinoma
INTRODUCTION
Verrucous hyperplasia is a histopathological entity, which shows considerable clinical and histological resemblance to verrucous carcinoma. This was first described by Shear and Pindborg (1980)[1] and differentiated from verrucous carcinoma. They separated these entities based on lack of invasive growth in the verrucous hyperplasia that is entirely superficial to adjacent normal epithelium. Verrucous hyperplasia is not only encountered in oral mucosa but also in sinonasal and laryngeal mucosa. Hansen et al. (1985)[2] described proliferative verrucous leukoplakia a type of non-homogeneous leukoplakia which is irreversible, slow growing with highest potential of malignant transformation and resistant to treatment. It is a clinical term and histopathologically it may show simple hyperkeratotic lesion to verrucous hyperplasia, verrucous carcinoma or well differentiated squamous cell carcinoma.
The aim of present study was to retrospectively analyze the clinico-pathological features of oral verrucous hyperplasia in Indian patients. Verrucous hyperplasia is most of the time confused with verrucous carcinoma which needs to be studied retrospectively in order to separate these to entities according to their clinico – pathological behavior.
MATERIALS AND METHODS
Total 19 cases of verrucous hyperplasia were selected from verrucous lesions in archives, over 10 years period. Each patient was retrospectively reviewed for clinical details like age, sex, habits, clinical features like site of lesion, clinical diagnosis, presence of associated lesions, histopathology and recurrence rate.
H and E stained sections were reviewed for verrucous projections, degree and type of keratinization, epithelial dysplasia, thickness of stratum spinosum, the width of rete ridges, the intensity and nature of the inflammatory cell infiltration & associated lesions in adjacent epithelium.
RESULTS
It was observed that the predominant age of occurrence of lesion was found to be in 4th decade of life with mean age of occurrence was 49.89 (± 12.8SD) years. Males (68.42%) outnumbered females (31.58%) (2:1). Buccal mucosa (57.89%) was found to be most commonly involved followed by tongue, gingiva, alveolar mucosa, soft palate in decreasing order. Clinically most cases presented with white, non scrapable, keratotic, exophytic, verruciform lesions ranging from 2 to 4cm not exceeding >6cm. Maximum lesions were diagnosed clinically as verrucous leukoplakia (42.10%) and other were diagnosed as leukoplakia, oral squamous cell carcinoma, verrucous carcinoma, speckled leukoplakia and lichen planus [Figures 1 and 2].
Figure 1.

Verrucous leukoplakia
Figure 2.

Proliferative verrucous leukoplakia
Prevalent habit pattern associated with verrucous hyperplasia was found to be tobacco and lime quid placement in buccal vestibule (36.84%) followed by mixed habit pattern (31.57%). Mixed habits includes simultaneous consumption of different tobacco preparation like pan with or without tobacco, bidi/cigarette smoking, areca chewing, areca and tobacco combinations include kharra, gutkha, mava chewing. Duration of habit range was 4 years to 40 years with mean duration of habit being 21.5 years.
13 cases were treated with surgical excision. Two cases were treated with lasers. Maximum patients were lost to follow up while very few showed evidence of recurrence after excision. Laser operated two cases showed recurrence within one year of follow-up.
Histopathological observations were carried out according to Shear and Pindborg's (1980)[1] criteria-. Main histological distinguishing feature between verrucous carcinoma and verrucous hyperplasia was found to be level of verrucous projections with relation to adjacent epithelium [Figures 3 and 4] Verrucous projections in verrucous hyperplasia were present above the adjacent normal epithelium. These surface projections were classified based on morphology into ‘Sharp’ and ‘Blunt’ types [Figures 5 and 6].
Figure 3.
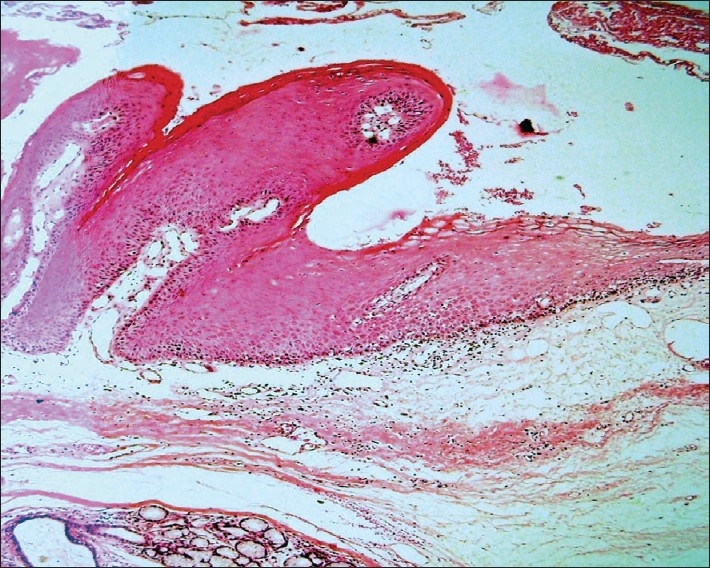
Photomicrograph of verrucous hyperplasia showing superficial proliferation (H and E stain, 4×)
Figure 4.
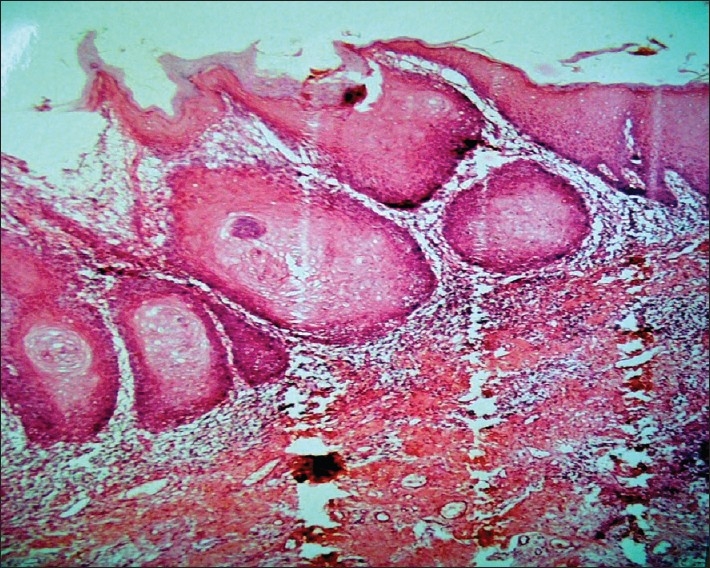
Photomicrograph of verrucous carcinoma showing proliferation in underlying connective tissue (H and E stain, 4×)
Figure 5.
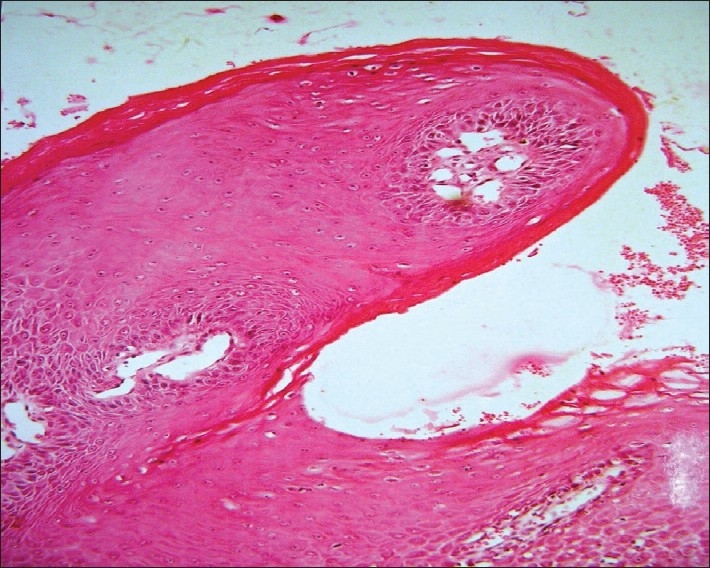
Photomicrograph of verrucous hyperplasia blunt variety(H and E stain, 10×)
Figure 6.
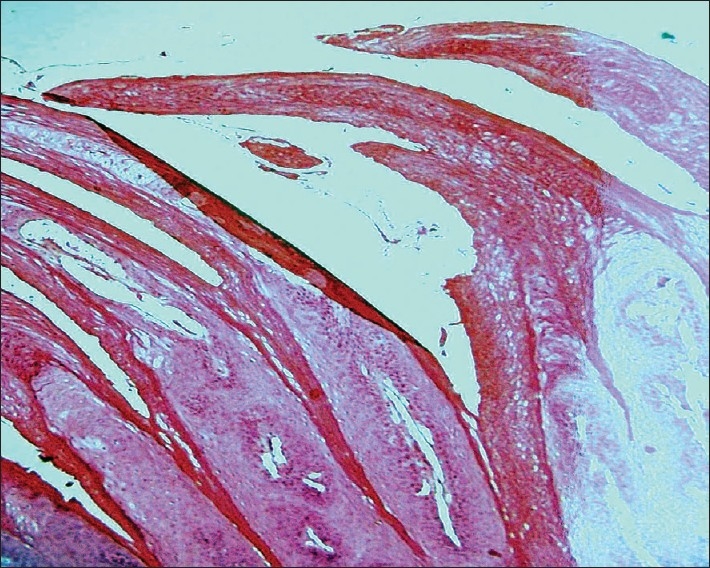
Photomicrograph of verrucous hyperplasia sharp variety(H and E stain, 10×)
Sharp variety (21%) is long, narrow and predominantly orthokeratinized (75%), while blunt variety (79%) show broad, short and mostly parakeratinized epithelium (86.66%). Blunt variety was predominant in our cohort [Graphs 1 and 2]. Blunt variety shows ortho and parakeratinization in 6.66%. Epithelial hyperplasia in the form of increase in the width of stratum spinosum was seen in 99% of cases.
Graph 1.
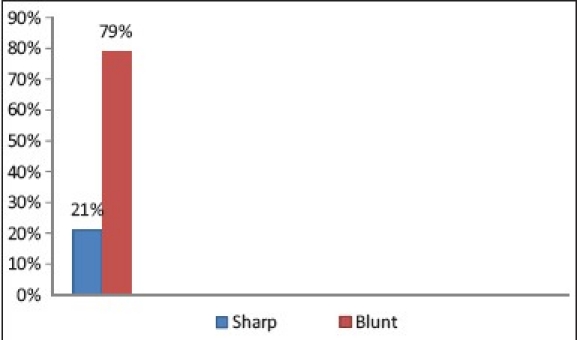
Type of verrucous projections
Graph 2.
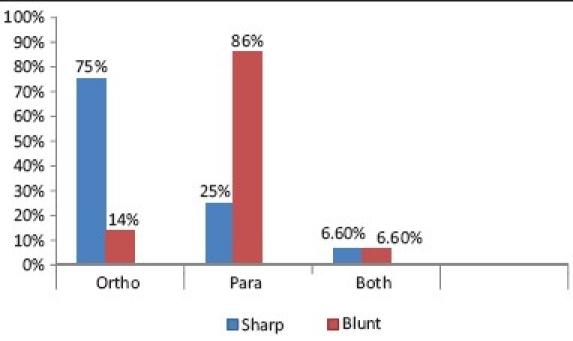
Degree of keratinization
Majority of cases showed broad rete ridges (57%) while only 15% showed narrow rete ridges. Both broad and narrow pattern was observed in 28% of cases.
Inflammatory response in subepithelial connective tissue was observed in 100% of our study cases. Marked inflammatory cells infiltration in the form of lymphocytes, plasma cells and histiocytes was seen in 68% of cases. Many sections showed inflammatory infiltration in clefts associated with necrotic areas.
For grading dysplasia Pindborg photographic standard of epithelial dysplasia was followed. Out of 19 cases, 68.42% showed dysplastic epithelium. Moderate dysplasia (61%) was predominant than mild dysplasia (38%) [Graph 3].
Graph 3.
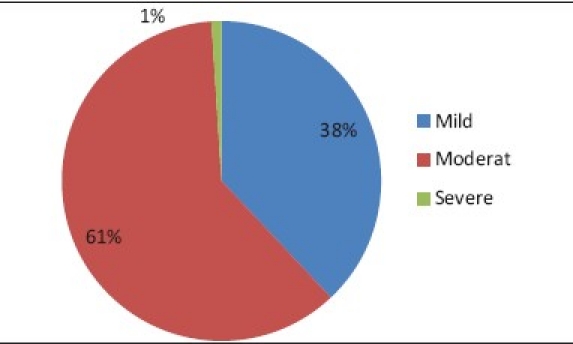
Degree of epithelial dysplasia
Moderate dysplasia was correlated with habit pattern, 87.5% of cases were found to be associated with mixed habit pattern. Adjacent epithelium was assessed it showed 47% of epithelial hyperplasia while other feature found was epithelial hyperplasia with dysplasia (21%). One of our cases showed adjacent atrophic epithelium and juxtaepithelial hyalinization, showing features of OSMF. Normal epithelium was seen in 26% of cases. Verrucous carcinoma and squamous cell carcinoma was not observed in association with any of our study cases [Graph 4].
Graph 4.
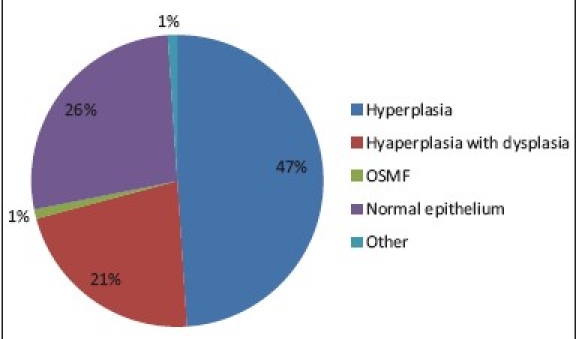
Adjacent epithelial changes
DISCUSSION
Verrucous hyperplasia probably represents a morphological variant of verrucous carcinoma by Slootwage J P and Muller H (1983).[3] Essential features in distinguishing verrucous hyperplasia from verrucous carcinoma is the location of the thickened epithelium with respect to adjacent normal appearing epithelium. In verrucous hyperplasia most of the hyperplastic broadened rete ridges lay above the adjacent normal epithelium while verrucous carcinoma on contrary exhibits a downward growth pattern of otherwise similar rete ridges.
Shear M and Pindborg JJ (1980)[1] stated that verrucous carcinoma often retract normal epithelium down with them into the underlying connective tissue. For that distinction it is very necessary that biopsy should include adjacent normal epithelium. Proliferative verrucous leukoplakia (PVL) is clinically a non-homogeneous leukoplakia which often confused with verrucous hyperplasia.[4] Hansen et al (1985)[2] suggested six histological stages ranging from normal mucosa, hyperkeratosis, verrucous hyperplasia, verrucous carcinoma, papillary squamous cell carcinoma and less well differentiated squamous cell carcinoma. Malignant potential of PVL is more than other types of leukoplakia.
In present study 4th decade was common age of presentation which is early than proposed by Shear M and Pindborg JJ (1980) (6th decade)[1]. Reasons attributed to this may be early acquisition of different habits, frequency and nature of habits and genetic susceptibility. Males predominated females (2:1) which is contradictory to other studies. This again can be correlated to early acquisition of habits which is more in Indian males than females.
The most commone site was buccal vestibular mucosa as opposed to study by Shear M and Pindborg JJ (1980)[1] in which they reported predominant location on gingiva and alveolar mucosa. These sites were in correlation to site of quid placement.
Habit pattern is diverse in Indian population. Most commonly consumed form is smokeless tobacco than the smoked one. We found mixed habit pattern associated with moderate dysplasia than those with exclusively single habit.
Smokeless tobacco habit are tobacco-lime quid placement in buccal vestibule, Pan with or without tobacco, areca nut mixed with tobacco and other ingredient to form kharra, gutkha and mava while smoked form is bidi and cigarette. Frequency and duration of habits also plays an important role in causation of verrucous hyperplasia. Present study showed 4-40 years of duration (mean age 21.5 years).
Histopathologically blunt variety predominates sharp variety as opposed to sharp variety reported by Shear M and Pindborg JJ (1980).[1] This difference may be attributed to lesser sample size in present study. Hyperorthokeratinization was predominant in sharp variety and parakeratinization was predominant in blunt variety. Increase in thickness of stratum spinosum is responsible for verrucous type morphology of lesion. As proposed by Shear and Pindborg considerable acanthosis with broadened rete ridges causes deprivation of distant epithelial cells from blood supply and becomes edematous and swollen. These necrotic cells undergo desquamation, leaving cleft in the surface of the epithelium. Verrucous projections are formed in this way in between clefts. This also explains the presence of the papillary projections of laminapropria, which support the verrucous projections. At a later stage both the verrucous projections and the clefts between them undergo keratinization.
Dysplasia is commonly seen in verrucous hyperplasia which is consistent with finding by Shear and Pindborg (1980)[1] study (66%).
Adjacent epithelium in present study cases showed predominantly epithelial hyperplasia and less frequently epithelial hyperplasia with dysplasia which suggest conversion of long standing simple leukoplakia to verrucous hyperplasia. In present study no other associated lesion like verrucous carcinoma or squamous cell carcinoma was found.
The association of Human papilloma virus (HPV) was found with development of verrucous hyperplasia was found by Greer R D (1990).[5] C-erb B-3 protein expression was an index of malignancy during progression from Verrucous Hyperplasia to Verrucous Carcinoma and Squamous cell carcinoma (Sakurai K, 2000).[6] Expression of P53 and EGFR levels could be use as marker while differentiating verrucous hyperplasia from verrucous carcinoma and squamous cell carcinoma (Wu and Maoxin et al, 2002).[7]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Shear M, Pindborg JJ. Verrucous hyperplasia of the oral mucosa. Cancer. 1980;46:1855–62. doi: 10.1002/1097-0142(19801015)46:8<1855::aid-cncr2820460825>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 2.Hansen LS, Olson JA, Silverman S., Jr Proliferative verrucous leukoplakia: A long-term study of thirty patients. Oral Surg Oral Med Oral Pathol. 1985;60:285–98. doi: 10.1016/0030-4220(85)90313-5. [DOI] [PubMed] [Google Scholar]
- 3.Slootweg PJ, Muller H. Verrucous hyperplasia or verrucous carcinoma: An analysis of 27 patients. J Maxillofac Surg. 1983;11:13–9. doi: 10.1016/s0301-0503(83)80006-x. [DOI] [PubMed] [Google Scholar]
- 4.Murrah VA, Batsakis JG. Proliferative verrucous leukoplakia and verrucous hyperplasia. Ann Otol Rhinol Laryngol. 1994;103:660–663. doi: 10.1177/000348949410300816. [DOI] [PubMed] [Google Scholar]
- 5.Greer RO, Jr, Eversole L R, Crosby L K. Detection of human papillomavirus-genomic DNA in oral epithelial dysplasia, oral smokeless tobacco associated leukoplakia, and epithelial malignancies. J Oral Maxillofac Surg. 1990;48:1201–5. doi: 10.1016/0278-2391(90)90538-d. [DOI] [PubMed] [Google Scholar]
- 6.Sakurai K, Urade M, Takahashi Y, Kishimoto H, Noguchi K, Yasoshima H, et al. Increased expression of C-erbs-3 protein and proliferating cell nuclear antigen during development of verrucous carcinoma of the oral mucosa. Cancer. 2000;89:2597–605. doi: 10.1002/1097-0142(20001215)89:12<2597::aid-cncr12>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 7.Wu M, Putti TC, Bhuiya TA. Comparative study in the expression of p53, EGFR, TFG-[alpha], and cyclin D1 in verrucous carcinoma, verrucous hyperplasia, and squamous cell carcinoma of head and neck region. Appl Immunohistochem Mol Morphol. 2002;10:351–6. doi: 10.1097/00129039-200212000-00011. [DOI] [PubMed] [Google Scholar]


