Abstract
A chemical genetics approach was taken to identify inhibitors of NS1, a major influenza A virus virulence factor that inhibits host gene expression. A high-throughput screen of 200,000 synthetic compounds identified small molecules that reverted NS1-mediated inhibition of host gene expression. A counter-screen for suppression of influenza virus cytotoxicity identified naphthalimides that inhibited replication of influenza virus and vesicular stomatitis virus. The mechanism of action was through activation of REDD1 expression and concomitant inhibition of mTORC1 via TSC1/TSC2 complex. The antiviral activity of naphthalimides was abolished in REDD1−/− cells. Viruses inhibited REDD1 expression, resulting in activation of the mTORC1 pathway. REDD1−/− cells prematurely up-regulated viral proteins via mTORC1 activation and were permissive to virus replication. In contrast, cells conditionally expressing high levels of REDD1 down-regulated viral protein levels. Thus, REDD1 is a novel host defense factor and chemical activation of REDD1 expression represents a potent antiviral intervention strategy.
Keywords: mRNA export, NS1, influenza virus, S6K, mTORC1, REDD1, DDIT4, Rtp801, VSV
Introduction
Infections by influenza viruses are responsible for ~36,000 deaths annually in the United States 1 and ~500,000 deaths worldwide per year 2. Highly pathogenic strains have been responsible for many deaths worldwide, such as the 1918 pandemic which killed ~30 million people. Currently, there are only two approaches available for preventing or treating epidemic and pandemic influenza, vaccination and inhibitors of virus replication. Vaccination, although highly effective against homologous strains, looses efficacy in the elderly, and it is limited by the highly mutable nature of the virus and the large reservoir of antigenically distinct virus strains. These factors require the annual re-formulation of the vaccine to match the antigenicity of the current influenza virus circulating strains. A number of drugs have been approved for the treatment of influenza. These drugs inhibit virus uncoating (inhibitors of the viral protein M2) or virus spread (inhibitors of the viral protein NA), but the use of these relatively small number of antiviral drugs is limited by the appearance of resistant virus strains. There is a clear need for additional therapeutic modalities for the treatment of influenza virus disease as well as for a better understanding of mechanisms of viral-host interactions leading to the discovery of novel targets for therapeutic intervention.
Many viruses target host mechanisms that are key steps within pathways that regulate antiviral responses. As an example, the NS1 protein of influenza virus is a multifunctional virulence factor that inhibits host gene expression and signal transduction required to induce antiviral responses. NS1 is found both in the nucleus and in the cytoplasm of influenza virus infected cells3,4. The cytoplasmic pool of NS1 inhibits interferon (IFN) gene induction by antagonizing the cytoplasmic signal transduction pathway mediated by RIG-I 5–8. NS1 also prevents IFN action by sequestering double-stranded RNA and/or targeting the function of downstream antiviral effector proteins, such as PKR and the RNase L pathways 9,10. In addition, NS1 has been shown to activate phosphatidylinositol 3-kinase signaling (PI3K), a function that supports virus replication 11.
The nuclear pool of NS1 inhibits host mRNA processing, including splicing12–14, polyadenylation15, and nuclear export16–18, thus preventing proper expression of host antiviral genes but not nuclear export of viral RNAs 15,18. Disruption of NS1 functions by mutations yielded highly attenuated viruses that can only replicate in immunocompromised hosts 19. These findings underscore the key role of NS1 as a pro-viral factor and emphasize the need to identify both inhibitors of this virulence factor as well as novel host antiviral mechanisms that antagonize NS1 functions. Here, we performed a high-throughput screen to identify small molecules that reverted NS1-mediated inhibition of host gene expression. Non-toxic small molecules from the naphthalimide family were identified and these compounds inhibited replication of evolutionarily diverse viruses, including influenza virus and VSV. We show that these small molecules served as probes to identify the mTORC1 inhibitor REDD120,21 as a novel host defense factor. These findings underscore the importance of regulating REDD1 expression as a novel strategy to trigger antiviral response.
Results
Naphthalimides Antagonize NS1 and Influenza Virus
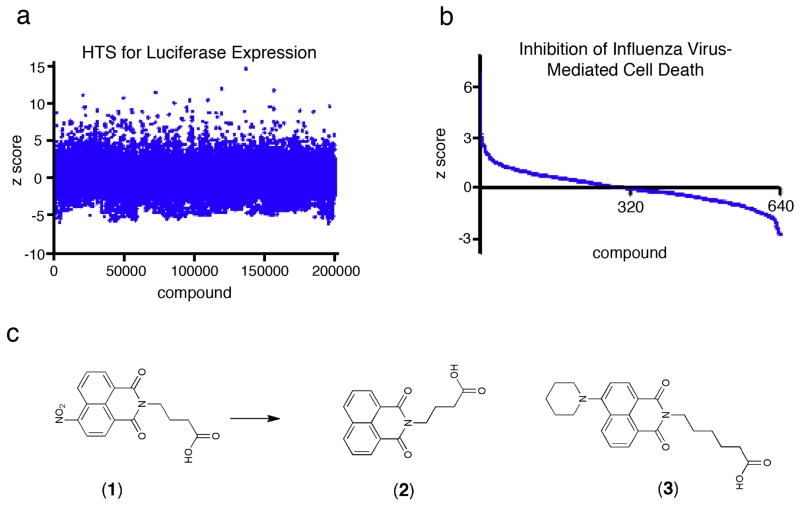
We exploited the potent ability of NS1 to inhibit gene expression by blocking mRNA processing and export15,18, as the basis for a high-throughput assay that measured the effect of NS1 on luciferase expression. Luciferase activity was reduced ~95% in cells transfected with plasmids encoding NS1 when compared to cells expressing luciferase alone, as we previously reported18. We screened 200,000 compounds at 5 μM concentration with this assay and then counter-screened for the ability of these small molecules to suppress cytotoxicity caused by influenza virus infection (Fig.1a,b). Among the most active compounds was 4-[N-4-nitro-(1,8-naphthalimide)]-butanoic acid, compound 1, (Fig. 1c).
Figure 1. Identification of Small Molecules that Revert the Inhibition of Gene Expression Mediated by the Influenza Virus NS1 Protein and that Protect Cells from Virus-Induced Cell Death.
(a) Luciferase expression in 293T cells transfected with NS1 and treated individually with 200,000 synthetic compounds (5 μM) was normalized to on-plate controls treated with 0.3% DMSO. Values are expressed as z scores, using the mean value and standard deviation of the experimental population screened on the same day. Red circle shows compound 1 studied here. (b) The most active 640 compounds were tested at three concentrations for the ability to inhibit the cytopathic effect of A/WSN/1933 influenza virus infection in HBECs. z scores for compounds assayed at 1.7 μM are plotted according to activity. (c) The structure of the most active naphthalimide from the primary screen, compound 1, an inactive analog, 2, and a more potent related compound, 3, are shown.
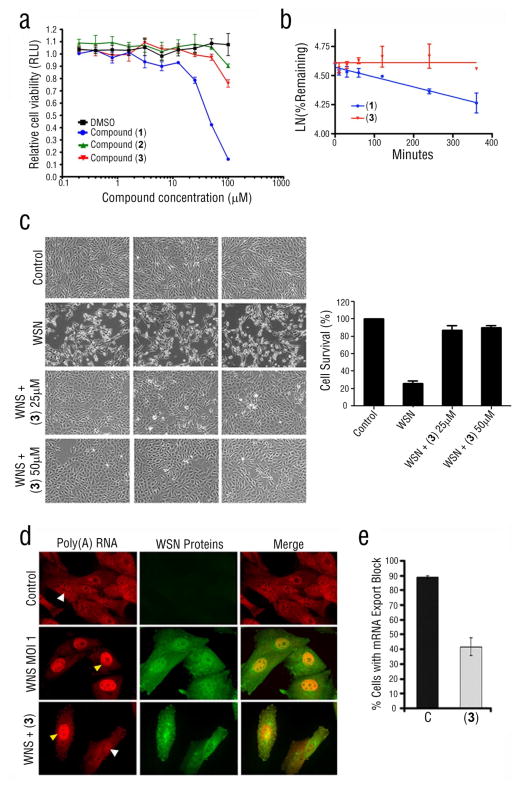
We obtained compounds structurally related to 1 and identified some that had no antiviral activity (2) or more potent activity (3) (Fig. 1c) (Supplementary Results, Fig. S1). Compound 3 was much less cytotoxic than the original 1 (Fig. 2a) and had a much longer half-life than 1 (Fig. 2b). We have also shown that 3 did not alter bulk protein synthesis (Supplementary Results, Fig. S2). To investigate the effect of 3 on virus-mediated cytotoxicity, we infected MDCK cells with influenza A/WSN/1933 virus at m.o.i. 0.001 for 48 h in the presence or absence of 3. Widespread cytopathic effects were observed in MDCK cells in the absence of 3 after 48 h of infection, but 3 largely prevented this effect (Fig. 2c). Since this compound was derived from a screen in which a reversal of NS1-mediated inhibition of gene expression was observed, it would be expected that a significant reversal of the mRNA export block induced by influenza virus would occur in the presence of active compound. Indeed, in cell populations infected with influenza virus in the presence of 3, there was a decrease in the number of cells that retained poly(A) RNA in the nucleus, as compared to infected cells not treated with 3 (Fig. 2d,e). A sub-population of infected cells still presented mRNA export block in the presence of 3; thus, it is possible that these cells are at different phases of the cell cycle, a process known to regulate mRNA export 22. Thus, 3 partially antagonized the mRNA export block in virus-infected cells.
Figure 2. Compound 3 Is Less Cytotoxic, More Stable than 1, and Reverts Influenza Virus-Mediated Cytotoxicity and mRNA Export Block.
(a) MDCK cells were treated for 30 h with compounds 1, 2, and 3 at various depicted concentrations and control cells were treated with the same concentration of DMSO as in the wells containing compound. Cell viability was determined by measuring cell ATP concentrations. (b) The fraction of compound remaining in cells treated with 1 or 3 as a function of incubation time was determined by mass spectrometry. (c) MDCK cells were pre-treated for 17 h with DMSO or with the indicated concentrations of 3 and subsequently mock infected or infected with A/WSN/1933 virus at m.o.i. 0.001 for 48 h. Indicated concentrations of compound were present during infection. DIC imaging was performed in a Zeiss Axiovert 200M. Bar, 90 μM. Cell survival was determined by counting live cells. (d) MDCK cells, mock-infected or infected with A/WSN/1933 in the presence or absence of 25 μM 3, were fixed and subjected to oligo-dT in situ hybridization to detect poly(A) RNA distribution in the nucleus and in the cytoplasm. Influenza proteins were detected by immunofluorescence using antibodies against influenza proteins. Yellow arrowheads point to cells with mRNA export block whereas white arrowheads point to cells that do not show blockage. Bar, 15 μM. (e) Data from triplicate experiments as depicted in (d) were quantified and the percentage of infected cells retaining mRNA in the nucleus is shown. Data represent mean values +/− s.d.
Naphthalimide Inhibits Virus Replication
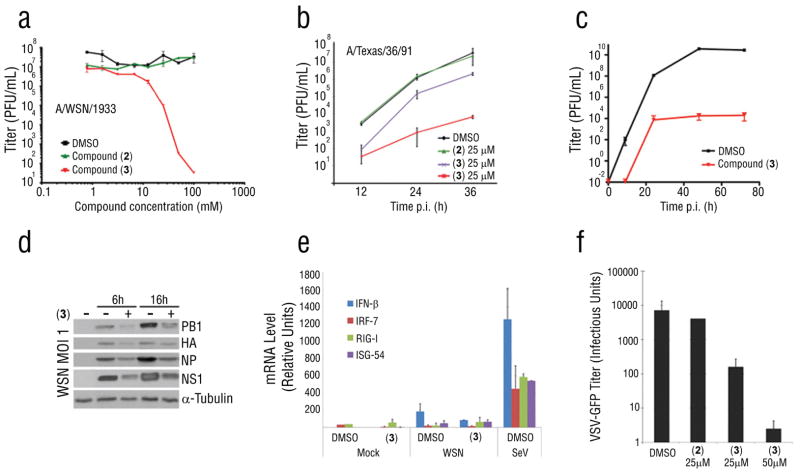
The effect of 3 on virus replication was then assessed using various strains of influenza virus, A/WSN/1933, A/Texas/1991, and the highly virulent A/Brevig/Mission/1/1918 strain that killed ~ 30 million people 23 (Fig. 3a–c). Non-cytotoxic concentrations of 3 reduced viral titers by 103 to 106 between 24 to 36h post-infection, depending on the influenza virus strain. The ratio of the concentration causing half maximum cytotoxicity (CC50) to half virus inhibition (IC50) for 3 was 31 (Fig. 2a, 3a). Similar results were also observed in human A549 cells (Supplementary Results, Fig. S3). As shown in Figure 3d, intracellular influenza virus proteins were also reduced in the presence of 3 (Fig. 3d). Thus, 3 decreased viral protein levels, contributing to the reduction of virus replication.
Figure 3. Compound 3 Inhibits Virus Replication but Does Not Induce Interferon Response.
(a–c) MDCK cells mock infected or infected with the influenza virus strains shown, at m.o.i. 0.001, were untreated or treated with compounds, at the depicted concentrations, and the virus titers of culture supernatants were determined by plaque assay. (d) Levels of intracellular viral proteins were measured by immunoblot analysis with specific antibodies to the indicated proteins. (e) Human A549 cells treated with DMSO or 25 μM 3 were mock infected or infected with A/WSN/1933 at m.o.i. 0.001 and after 36 h, RNA was isolated and the expression of the interferon-responsive genes shown was quantified by real-time RT-PCR. (f) MDCK cells mock infected or infected with VSV-GFP (m.o.i = 0.001) were untreated or treated with the indicated compounds. At 24 h post-infection, virus titers were determined in the supernatants. Data represent mean values +/− s.d.
The antiviral effect of 3 was not IFN-mediated. The mRNA levels of IFN-β and IFN effectors were measured, by qPCR and microarray analysis, revealing that 3 did not induce IFN production or an IFN-mediated response (Fig. 3e; Supplementary Dataset 1). Furthermore, 3 protected cells impaired in interferon response, Vero Cells and Stat1 −/− cells, from influenza virus replication or cell death, respectively (Supplementary Results, Fig. S4). Compound 3 also antagonized expression of high levels of influenza virus proteins in Vero cells (Supplementary Results, Fig. S5). Thus, 3 partially antagonized the block of mRNA export in virus-infected cells, but this effect did not result in the production of interferon. However, the partial release of mRNA export by 3 likely occurred as a consequence of low NS1 levels, resulting in the expression of a significant number of host mRNAs that encode antiviral factors. To investigate whether 3 antagonized NS1 directly or promoted host antiviral functions regulated by NS1 that could also impact replication of other viruses, we infected cells with VSV at 0.001 pfu/cell in the absence or presence of compounds 2 or 3. Compound 3 inhibited VSV replication (Fig. 3f). Thus, 3 targeted host cell function(s) that conferred an antiviral state against diverse viruses.
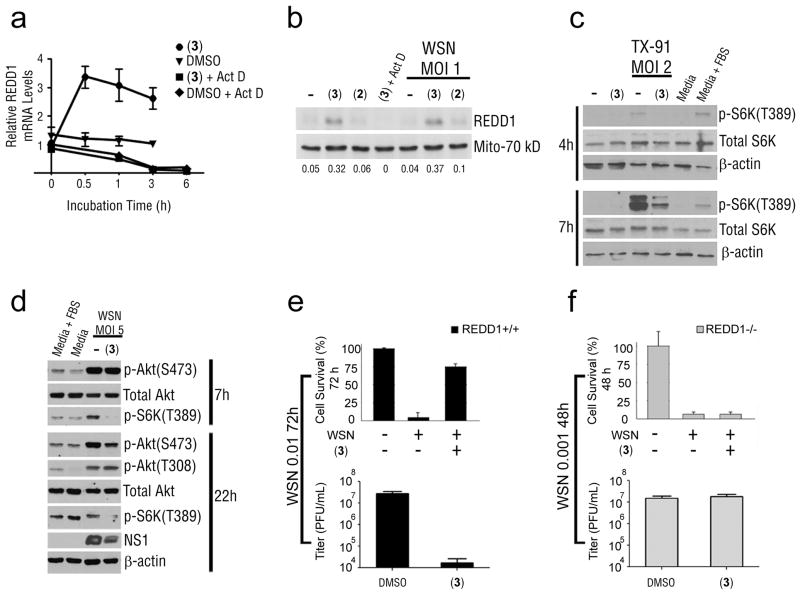
Antiviral Activity of Naphthalimide Requires REDD1
Since 3 targeted the host, we analyzed host pathways by comparing gene expression profiles in human A549 cells in the presence or absence of compound, using Gene Set Enrichment Analysis (Supplementary Results, Fig. S6; Supplementary Dataset 1). In cells treated with 3, the mTORC1 pathway had one of the highest enrichment scores. REDD1, an inhibitor of the mTORC1 pathway 20,21, was up-regulated at the mRNA level (Fig. 4a and Supplementary Dataset 1). The induction of REDD1 mRNA by 3 was abolished in the presence of the transcription inhibitor actinomycin D (Fig. 4a). In addition, REDD1 mRNA similarly decayed over time in the absence or presence of 3 and actinomycin D (Fig. 4a). Thus, these results indicated that induction of REDD1 mRNA by 3 occurred at the transcriptional level. REDD1 protein levels increased ~6–8 fold in the presence of 3 alone or in the presence of both 3 and influenza virus infection (Fig. 4b). Again, this induction of REDD1 protein by 3 was abolished in the presence of actinomycin D (Fig. 4b). We found that influenza virus greatly increased the levels of phosphorylated S6 kinase (p70-S6K) at Thr389 (Fig. 4c), a site phosphorylated by mTORC1, and this effect was greatly reduced in A549 cells treated with 3 (Fig. 4c). The total levels of S6K protein did not change in the presence of 3 (Fig. 4c), demonstrating that the effect of this small molecule occurred at the level of phosphorylation of S6K at Thr389. The mTORC1 inhibitor rapamycin also reduced influenza virus NS1 protein levels (Supplementary Results, Fig. S7).
Figure 4. Influenza Virus Activated the mTORC1 Pathway and Naphthalimide Required the mTORC1 Inhibitor REDD1 for its Antiviral Activity.
(a) A549 cells were untreated or treated with 30 μM 3 for the indicated time periods, in the absence or presence of actinomycin D (0.5 μg/ml). REDD1 mRNA levels were quantified by real time RT-PCR. (b) A549 cells were untreated or treated with 30 μM 3 (in the absence or presence of 0.5 μg/ml actinomycin D as indicated) for 18 h prior to infection and during infection. Cell extracts were obtained at 6 h post-infection and subjected to immunoblot analysis with the indicated antibodies. Densitometry analysis was performed to determine the ratio of REDD1 over loading control (Mito-70 kD) using ImageJ (Supplementary Results, Fig. S18). (c) A549 cells were untreated or treated as in (b) prior to infection and during infection. Cell extracts were subjected to immunoblot analysis with depicted antibodies (Supplementary Results, Fig. S19). (d) Phosphorylation of Akt or S6K was measured by immunoblot analysis in cell extracts of A549 cells infected with influenza virus in the presence or absence of 3. Compound was added prior and during infection as in (b) (Supplementary Results, Fig. S20). (e and f) REDD1+/+ cells were untreated or treated with 3 and mock-infected or infected at m.o.i 0.01 with A/WSN/1933 for 72 h. REDD1−/− MEFs, untreated or treated with 3, were infected with A/WSN/1933 at m.o.i. 0.001 for 48 h. Cell survival was determined by trypan blue exclusion assay and virus titers were measured by plaque assays. Low exp, low exposure; High exp, high exposure.
To investigate whether 3 prevented S6K activation independently of influenza virus, we tested the effect of 3 in H358 cancer cells, which have chronically active S6K. Cells were treated with compounds 3 and inactive 2. Compound 3, but not 2, reduced the activation of S6K in H358 cells (Supplementary Results, Fig. S8a). In two other cancer cell lines that have chronically active AKT, H1993 and LnCAP, 3 also reduced active S6K (Supplementary Results, Fig. S8b). However, 3 did not inhibit phosphorylation of a major active site on AKT at S473 (Fig. 4d), which is a target of mTORC2 24,25. In A549 cells infected with influenza virus for 7h, 3 blocked S6K activation and had no effect on AKT phosphorylation (Fig. 4d). At 22 h post-infection, 3 did not alter pAKT (T308) level but reduced pAKT (S473) level; however, this reduction is probably an indirect effect of 3 on the inhibition of viral replication rather than a direct effect of 3 on AKT. Thus, 3 acts in parallel to, or downstream of AKT.
To determine whether REDD1 was required for the antiviral activity of 3, we tested the antiviral effect of 3 in infected REDD1+/+ or REDD1−/− mouse embryonic fibroblasts. Influenza virus-mediated cell death and replication were inhibited by 3 in REDD1+/+ cells infected at m.o.i. 0.01 for 72 h (Fig. 4e). REDD1+/+ cells were infected at m.o.i. 0.01 for 72 h because this was the best time point in which enough cell death was observed and the protection by 3 could then be determined. Infected REDD1−/− cells, treated in the same conditions as REDD1+/+ cells, were completely dead by 24 h in the presence or absence of compound; therefore, REDD1−/− cells were infected with influenza virus at m.o.i. 0.001 for 48 h, in the absence or presence of 3. Even at this low m.o.i and less infection time, 3 did not protect REDD1−/− cells from virus-mediated cell death or virus replication (Fig. 4f). In addition, REDD1−/− cells infected at m.o.i. 0.001 for 48 h produced approximately as many viral particles as REDD1+/+ cells infected at m.o.i. 0.01 for 72 h (Fig. 4e,f). When REDD1+/+ cells were infected with influenza virus at m.o.i. 0.001, they produced ~200 fold less virus than REDD1−/− cells infected in the same conditions (Supplementary Results, Fig. S9). This effect was also observed in VSV infected REDD1+/+ and REDD1−/− cells (Fig. 5c,d). Treatment of both REDD1+/+ and REDD1−/− cells with 3 alone did not cause cytotoxicity (Supplementary Results, Fig. S10). Thus, REDD1 knockout cells were more permissive to influenza virus replication than wild-type cells. As 3 did not inhibit virus replication in the absence of REDD1 (Fig. 4f), REDD1 is required for the antiviral activity of 3.
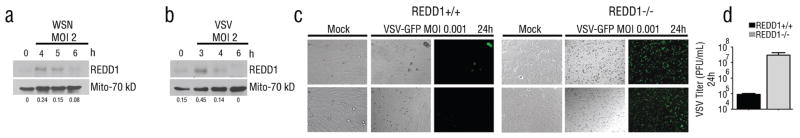
Figure 5. Viruses Activate the mTORC1 pathway via down-regulation of REDD1 expression.
Extracts from cells mock infected or infected with influenza virus (a) or VSV-GFP (b) were subjected to immunoblot analysis with depicted antibodies. Densitometry analysis was performed to determine the ratio of REDD1 over loading control (Mito-70 kD) using ImageJ. (c) Wild-type or REDD1−/− MEFs were infected with VSV-GFP at m.o.i. of 0.001 for 24 h. DIC or fluorescent images of VSV-GFP are shown. Bar, 50 μM. (d) Supernatants of cells from (c) were subjected to plaque assays.
REDD1 is a Host Defense Factor
These data indicated that REDD1 is an important host factor required for antiviral response, raising the possibility that viruses regulate REDD1 expression. During influenza virus and VSV infections, REDD1 expression was initially increased but was then down-regulated (Fig. 5a,b), resulting in activation of S6K (Fig. 4c). The initial up-regulation of REDD1 likely represented a host antiviral response, which was then inhibited by the virus, resulting in activation of mTORC1. Consistent with REDD1 being part of a general host cell antiviral response, REDD1−/− cells were also highly permissive to VSV replication as compared to wild-type cells (Fig. 5c,d), resulting in higher levels of intracellular VSV proteins in REDD1−/− cells than in REDD1+/+ cells (Supplementary Results, Fig. S11). In the absence of REDD1, 3 did not inhibit VSV replication as in REDD1+/+ cells, showing once again that REDD1 is required for its antiviral activity (Supplementary Results, Fig. S12).
By preventing viruses from activating mTORC1, REDD1 might affect two biological functions potentially important for virus replication, autophagy and/or protein translation. By preventing activation of mTORC1, enhanced REDD1 expression would possibly increase autophagy26. However, compound 3 protected ATG5 −/− cells, which lack an autophagic response, against VSV replication (Supplementary Results, Fig. S12). In addition, treatment of cells with chloroquine, an autophagy inhibitor, did not affect viral protein levels in REDD1−/− cells (Supplementary Results, Fig. S13). Together, these results indicated that autophagy was not the mechanism involved in 3-mediated inhibition of viral protein expression. Thus, the requirement for activating mTORC1 for efficient virus replication was likely to be translation.
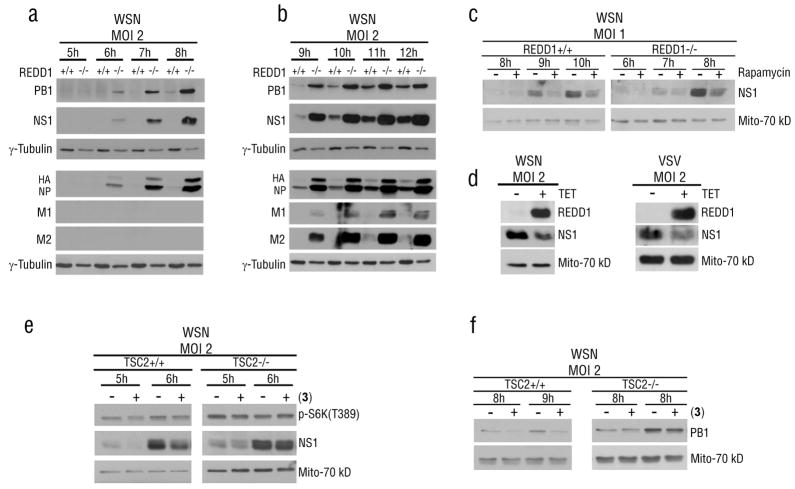
To investigate if the enhanced viral infection in REDD1−/− cells was due to a general increase in translation or an effect on specific viral proteins, expression of several influenza virus proteins was measured as a function of time after infection of both REDD1 wild-type and knockout cells. Lysates from REDD1+/+ and REDD1−/− cells infected with influenza virus were subjected to immunoblot analysis with antibodies against various influenza virus proteins. REDD1−/− cells produced high levels of influenza virus proteins two to three hours earlier than REDD1 +/+ cells (Fig. 6a,b). The enhanced expression of viral proteins led to increased viral RNA levels (Supplementary Results, Fig. S14). Similar results were observed upon VSV infection (Supplementary Results, Fig. S11). To determine if the effect on viral proteins in REDD1 −/− cells was due to mTORC1 activity on translation, REDD1 −/− cells were treated with rapamycin. In fact, rapamycin treatment down-regulated viral protein levels in both REDD1+/+ and REDD1−/− cells (Fig. 6c) (Supplementary Results, Fig. S15) indicating that induction of high viral protein levels in REDD1−/− cells occurred via activation of mTORC1. Furthermore, in cells conditionally expressing high levels of REDD1, viral protein levels were reduced, consistent with the function of REDD1 as a host defense factor (Fig. 6d).
Figure 6. REDD1 regulates viral protein expression in a mTORC1 dependent manner.
(a) REDD1+/+ and REDD1−/− cells were infected with influenza virus WSN at m.o.i. 2 for 1 h at 22 °C and then shifted to 37 °C. Viral protein levels were monitored over time by immunoblot analysis with the depicted antibodies. (b) Viral protein levels were monitored as in (a). (c) WSN-infected REDD1+/+ and REDD1−/− cells were treated with 100nM Rapamycin. Rapamycin was added one 1 h post-infection. NS1 levels were monitored over time by immunoblot analysis. (d) U2OS cells, untreated or treated with tetracycline to induce REDD1 overexpression, were infected as in (a) but with both influenza virus or VSV. NS1 or VSV-M protein levels were monitored by immunoblot analysis. (e and f) TSC2+/+ and TSC2−/− cells were pre-treated with 10 μM 3. Cells were then infected with influenza virus WSN at m.o.i. 2 for 1 h at 22 °C and then shifted to 37 °C in the absence of compound. After 1 hour post-infection, 3 was added back. Cell extracts were obtained at the depicted time points and subjected to immunoblot analysis with the indicated antibodies.
REDD1 prevents the inactivation of the TSC1/TSC2 complex by AKT1, and thus blocks activation of the mTORC1 pathway 20,27. In TSC2 knockout cells, 3 did not induce down-regulation of viral protein expression, as opposed to wild-type cells in which viral protein levels were inhibited by 3 (Fig. 6e,f). In addition, activation of S6K in REDD1−/− infected cells was not inhibited by 3 (Supplementary Results, Fig. S16), indicating that 3 does not act directly on S6K. Thus, 3 requires TSC2 for down-regulating viral protein expression (Fig. 6e,f). Altogether, these findings show that the antiviral activity of 3 occurs through repressing the activity of mTORC1 in a TSC1/TSC2 dependent manner. It is also possible that 3 may act on other pathways.
We have also designed an analog of 3, termed 4, which has similar antiviral properties as 3. Compound 4 prevented virus replication by inducing REDD1, but it is a more potent inhibitor of the highly pathogenic H1N1/1918 influenza virus strain (Supplementary Results, Fig. S17) 23. Altogether, these findings revealed REDD1 as a novel host antiviral factor and showed that the antiviral activity of 3 required REDD1.
Discussion
There are essentially two approaches for identifying novel host processes involved in antiviral functions and that can be exploited therapeutically. One is to learn as much as possible about the host mechanisms required by the virus and then test the effects of inhibiting them. The other is to take an unbiased approach and screen for chemical inhibitors of virus functions, or host genes required by the virus. Taking the chemical genetics version of the second approach, we conducted a screen for compounds that antagonized the inhibition of gene expression by NS1 and identified napthalimides that inhibited replication of influenza viruses and vesicular stomatitis virus. These compounds functioned by increasing expression of REDD1, a major negative regulator of the mTORC1 pathway, and in cells lacking REDD1, the compound lost its antiviral activity.
Many viruses activate AKT through stimulating PI3K 28,29. The NS1 protein of influenza virus directly binds PI3K, resulting in activation of AKT 30–33. This has been interpreted either as functioning to inhibit apoptosis, preventing the cell from dying prematurely during infection, or as necessary in some way to promote virus replication. A recent genome-wide siRNA screen implicated mTORC1 in influenza virus replication34, suggesting that activating that pathway might be one of the functions of elevated AKT1 signaling. Our results imply that an important consequence of AKT signaling for influenza virus replication is activation of the mTORC1 effector S6K through phosphorylation, as the anti-viral napthalimides we identified inhibited phosphorylation of p70 S6K by mTORC1. We showed that the protein up-regulated by our napthalimides, the mTORC1 inhibitor REDD1, is a novel host defense factor. REDD1 was induced by influenza virus or VSV, but was then successfully suppressed by the virus. REDD1 suppression by viruses promoted virus replication as REDD1 knock-out cells were highly permissive to virus replication.
REDD1 is induced by various environmental conditions, including cell confluency, glucocorticoid treatment, hypoxia, and other stress-response pathways, such as ER (endoplasmic reticulum) stress 35. Both ER stress and the hypoxia inducible factor (HIF) play a role in immunity and infection36,37. ER stress was shown to promote plasma cell development, and absence of key components of this pathway results in sensitization to viral infection36. Mouse embryonic fibroblasts deficient in the ER protein kinase PERK/PEK, which is activated by accumulated unfolded proteins in the ER, are more permissive to VSV replication than wild-type cells 38. Up-regulation of REDD1 in response to ER stress39,40 occurs via the transcription factor ATF440. HIF activation by the hypoxia mimetic cobalt chloride promotes cellular resistance to VSV infection, whereas inhibition of HIF activity by RNAi or by a small molecule antagonist showed increased sensitivity to viral infection as measured by enhanced VSV cytotoxicity and replication37; however, the mechanism is not known. During hypoxia, REDD1 was shown to be a direct target of the HIF-1 alpha transcription factor20, which induces REDD1 expression. Thus, activating a stress response pathway or promoting the expression of a stress response protein to a certain extent may induce resistance to pathogens and decrease host cytotoxicity. However, coordination of a stress response to promote cellular resistance without significantly damaging the host upon pathogen invasion remains to be further investigated. We showed that induction of REDD1 by small molecules is an efficient strategy for interfering with the functions of the mTORC1 pathway that are required by viruses.
The effect of the napthalimide on influenza virus was a sharp attenuation of the production of virus proteins early in infection. We found no effect of the napthalimide on global protein synthesis and no induction of an interferon response. In addition, in cells lacking REDD1, in which expression of influenza virus proteins is enhanced, rapamycin inhibited expression of influenza virus proteins at a concentration in which bulk protein synthesis is known to be unaltered. Thus, this indicates selective translational regulation, which has been documented in a number of conditions, including the general amino acid control response41 and other types of processes, such as survival and proliferation42. In addition, during nuclear mRNA processing and export, specific sequences either within the UTRs or in the coding region can dictate differential binding by RNA-binding proteins (hnRNPs), which will regulate processing and export of specific subsets of mRNAs, resulting in differential expression43,44. This raises the possibility that the inhibition of the mTORC1 pathway may alter translation in some way unfavorable to initiation of specific viral mRNAs relative to host messages. In cells infected at a low multiplicity of infection, the first viral messages must compete with the far larger volume of host messages for access to ribosomes. In this respect, the early viral messages would have the same problem as a host cell message of low abundance, such as mRNAs encoding certain transcription factors. However, at the earliest phases of infection, viruses are largely dependent upon normal host processes and it is these processes that are likely to be the most useful therapeutic targets.
Although many viruses can be controlled by vaccination, there is still an important need for antiviral drugs. For viruses, such as influenza virus, that can infect other animals, vaccination will never eradicate the virus. Other viruses, such as small pox or measles can potentially be eradicated by global immunization. However, once the incidence of disease is very low, global vaccination is inevitably discontinued, leaving the human population vulnerable to reemergence of the virus. The long lead times required to produce sufficient vaccine to protect the human population means that appearance of a new or re-occurring highly infectious virus can lead to a pandemic of disease before the vaccine is available. However, antiviral drugs that target viral proteins have the disadvantage that resistance to the drug will arise due to the high rates of mutation inherent in viruses and the large numbers of progeny that they produce. A strategy targeting host processes that are essential for virus replication, such as the one discussed here, would avoid this problem, although it would be limited by the possibility of toxic side effects. Thus, combinations of non-cytotoxic small molecules that target both viral and host proteins are desirable. Recently, influenza A nucleoprotein was identified as an antiviral target45. A small molecule that triggered nucleoprotein aggregation and prevented its import into the nucleus protected against influenza virus replication45. In addition, a chemical compound that inhibited host pyrimidine biosynthesis has been recently shown to reduce influenza virus replication46.
In sum, the strategy of chemically inducing host antiviral activities targeting host pathways without causing significant short-term toxic effects will likely have an important impact in antiviral therapy. One such strategy was identified here with the induction of the mTORC1 inhibitor REDD1 by naphthalimides. Furthermore, small molecules that inhibit the mTORC1 pathway in different ways have the potential for anti-cancer therapy as the mTORC1 pathway is a major regulator of cell proliferation and cancer 47.
Methods
Compound screen
The UT Southwestern Compound Library is composed of 200,000 synthetic drug-like compounds arrayed in DMSO in 384 well plates. 293T cells were transfected with an approximately 10:1 ratio of plasmid pCMV-Luc encoding luciferase and pCAGGS-NS1 encoding NS1, using Lipofectamine2000 (Invitrogen). Cells were transfected with the luciferase plasmid alone as a positive control. After 16 hours, cells were dispensed at 5000 cell/well in 384 well plates. After one hour, compounds from the library were added to a final concentration of 5 μM in 1% DMSO in a one compound/one well format. Experimental samples were limited to columns 3 to 22, with controls treated with 1% DMSO in the first and last two columns of wells. Wells in the first column of each plate contained cells transfected with the luciferase plasmid alone; all other wells received cells transfected with both plasmids. Plates were incubated 22 h at 37°C in 5% CO2, then cooled to room temperature and incubated with Bright-Glo luciferase substrate (Promega) for 4 min and luminescence was recorded. Plates with Z′-scores lower than 0.45 were repeated. Experimental values were normalized to the mean of the luciferase alone control on the same plate. Compounds were ranked by z-score and 640 compounds having the most positive z-scores were selected and re-tested in the assay at 15, 5 and 1.7 μM concentrations. These compounds were also tested for the ability to prevent cell death of immortalized human bronchial epithelial cells (HBEC) that had been infected with A/WS/33 influenza virus by measuring cell ATP levels with ATP-lite (PerkinElmer). A supplementary table describing this screen is added to the end of the Supplementary Information file.
Compound half-life
Compound half-lives were measure in HBECs by LC/MS/MS. Metabolic stability half-life was determined by substrate depletion 48.
Cell survival/Cytotoxicity measurements
MEF, HBEC, or MDCK cells were seeded in white-walled 96 plates at a density of 3×103 cells per well, 16 h prior to compound addition. Compounds dissolved in sterile DMSO (Sigma) at a concentration of 25 mM were diluted to 100 μM in OptiMEM I (Invitrogen) in triplicates. The 100 μM starting dilutions were serially diluted in two-fold steps to a final concentration of 0.2 μM. Control experiments, performed in the absence of compound, had the same final concentration of DMSO as in compound-treated samples. At the time points depicted in the figures, cells were lysed and ATP levels measured by luminescence using the Cell Titre-Glo kit (Promega) following the manufacturer’s instructions. In parallel, cells were also counted at the beginning and at the end of each experiment and cell survival was quantified by trypan blue exclusion assay.
Influenza virus replication
MDCK cells were infected with various strains of influenza virus depicted in the figures at an m.o.i. of 0.001 pfu/cell for 1 hr. Next, cells were washed with PBS and overlaid with OptiMEM containing two-fold compound dilutions ranging from 100 μM to 0.8 μM. Samples containing only the same volume of DMSO as the compounds were included. At 30 h p.i., culture medium was collected, cell debris removed by centrifugation at 1000 ×g for 10 minutes, and frozen at −80 °C. Viral titers were determined by plaque assay. The experiments conducted with the H1N1/1918 strain were performed in a high-containment (BSL3++) facility.
For experiments performed with A549 cells, REDD1+/+ and REDD1−/− cells, and TSC2 cells, the methodology is described in the legends. For experiments performed with U20S cells, cells were plated in 12-well plates in DMEM containing 10% FBS and incubated overnight. Cells were then incubated in media containing tetracycline (1 g/ml) for 2 h to induce REDD1 overexpression. Cells were washed with PBS and infected with A/WSN/1933 or VSV at m.o.i. 2 for 1 h. Tetracycline was added back 1 h post-infection and cell lysates were prepared at various time points post-infection, as indicated in the figure.
VSV Replication Assay
Vesicular stomatitis virus replication: MDCK cells seeded in 35-mm-diameter dishes were infected with VSV-GFP at m.o.i. 0.001 pfu/cell. At 24 h p.i., supernatants were clarified and used for titration on VERO cells. Four-fold serial dilutions of virus containing supernatants were made in PBS containing serum and antibiotics. Fifty microliters of each dilution was mixed with an equal volume of complete growth medium containing 8,000 VERO cells and incubated at 37 °C for 48 h in 96-well plates. Cells were fixed in 4% paraformaldehyde. The number of wells with GFP expression were counted by fluorescence microscopy and subsequently used to calculate relative virus titers. Infection of U2OS cells with VSV was performed in the same manner as influenza virus infection described above.
In situ hybridization
mRNA distribution in MDCK cells infected with influenza virus in the presence or absence of compounds was performed as we previously described 18. Influenza proteins were detected with mouse anti-influenza antibody (Biodesign International) and FITC labeled anti-mouse antibody.
Phospho-S6K analysis
Cells were starved for 18 h and then mock infected or infected as described in the legend of figure 5. Five percent serum was added to induce S6K phosphorylation in control lanes. H358 and H1993 cells were treated with 10 μM 3 and LnCap cells were treated with 30 μM.
All data presented here are representative of at least 3 independent experiments. In the line graphs or histograms, data represent mean values +/− s.d.
Description of real-time RT-PCR, gene expression profiling and analysis, human biochemical network, compound synthesis, details of cells, plasmids and antibodies are described in Supplementary Methods and Supplementary Information.
Supplementary Material
Acknowledgments
We thank R. Sakthivel, L. Melito, and J. Naidoo for technical assistance. We thank S. de Celis, D.E. Levy and B. Levine for reagents. This work was supported by NIH R01 GM07159 to B.M.A.F.; R01 AI079110 and R01AI089539 to B.M.A.F. and M.G.R.; the Diane and Hal Brierley distinguished Chair in Biomedical research to M.G.R and C06-RR15437 from the NCRR; NIH grants R01AI046954, P01AI058113, U54AI057158, U01AI074539 and CRIP, an NIAID funded Center of Excellence for Influenza Research and Surveillance (HHSN266200700010C) to A.G.-S; R01 CA129387 to J.B.; M.M. was supported by the NIH Diversity Supplement R01GM06715908S1.
Abbreviations
- MOI
multiplicity of infection
- NS1
nonstructural 1
- S6K
S6 kinase
- mTORC1
mammalian target of rapamycin
- REDD1, DDIT4, or Rtp801
regulated in development and DNA damage response 1
- VSV
vesicular stomatitis virus
Footnotes
Author contributions: M.M., N.S., G.A.V., D.F., S.P.-L., J.B., C.F., M.A.W., A.G.-S., M.G.R., and B.M.A.F. designed research; M.M., N.S., G.A.V., S.W., N.W., M.S., S.P.-L., and C.F. performed research; D.F. contributed new reagents; M.M., N.S., G. A.V., D.F., N.W., M.S., S. P.-L., J.B., C.F., M.A.W., A.G.-S., M.G.R., and B.M.A.F analyzed data; M.G.R. and B.M.A.F. wrote the paper.
Authors declare no competing financial interest.
References
- 1.Simonsen L, et al. The impact of influenza epidemics on mortality: introducing a severity index. Am J Public Health. 1997;87:1944–1950. doi: 10.2105/ajph.87.12.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith DJ, et al. Mapping the antigenic and genetic evolution of influenza virus. Science. 2004;305:371–376. doi: 10.1126/science.1097211. [DOI] [PubMed] [Google Scholar]
- 3.Krug RM, Etkind PR. Cytoplasmic and nuclear virus-specific proteins in influenza virus-infected MDCK cells. Virology. 1973;56:334–348. doi: 10.1016/0042-6822(73)90310-3. 0042-6822(73)90310-3 [pii] [DOI] [PubMed] [Google Scholar]
- 4.Li Y, Yamakita Y, Krug RM. Regulation of a nuclear export signal by an adjacent inhibitory sequence: the effector domain of the influenza virus NS1 protein. Proceedings of the National Academy of Sciences of the United States of America. 1998;95:4864–4869. doi: 10.1073/pnas.95.9.4864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo Z, et al. NS1 protein of influenza A virus inhibits the function of intracytoplasmic pathogen sensor, RIG-I. Am J Respir Cell Mol Biol. 2007;36:263–269. doi: 10.1165/rcmb.2006-0283RC. 2006-0283RC [pii] [DOI] [PubMed] [Google Scholar]
- 6.Mibayashi M, et al. Inhibition of Retinoic Acid-Inducible Gene-I-Mediated Induction of Interferon-{beta} by the NS1 protein of Influenza A Virus. J Virol. 2007;81:514–524. doi: 10.1128/JVI.01265-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Opitz B, et al. IFNbeta induction by influenza A virus is mediated by RIG-I which is regulated by the viral NS1 protein. Cell Microbiol. 2007;9:930–938. doi: 10.1111/j.1462-5822.2006.00841.x. CMI841 [pii] [DOI] [PubMed] [Google Scholar]
- 8.Pichlmair A, et al. RIG-I-Mediated Antiviral Responses to Single-Stranded RNA Bearing 5′-Phosphates. Science. 2006;314:997–1001. doi: 10.1126/science.1132998. [DOI] [PubMed] [Google Scholar]
- 9.Li S, Min JY, Krug RM, Sen GC. Binding of the influenza A virus NS1 protein to PKR mediates the inhibition of its activation by either PACT or double-stranded RNA. Virology. 2006;349:13–21. doi: 10.1016/j.virol.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Min JY, Krug RM. The primary function of RNA binding by the influenza A virus NS1 protein in infected cells: Inhibiting the 2′-5′ oligo (A) synthetase/RNase L pathway. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:7100–7105. doi: 10.1073/pnas.0602184103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hale BG, Jackson D, Chen YH, Lamb RA, Randall RE. Influenza A virus NS1 protein binds p85beta and activates phosphatidylinositol-3-kinase signaling. Proc Natl Acad Sci U S A. 2006;103:14194–14199. doi: 10.1073/pnas.0606109103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fortes P, Beloso A, Ortin J. Influenza virus NS1 protein inhibits pre-mRNA splicing and blocks mRNA nucleocytoplasmic transport. EMBO J. 1994;13:704–712. doi: 10.1002/j.1460-2075.1994.tb06310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qiu Y, Nemeroff M, Krug RM. The influenza virus NS1 protein binds to a specific region in human U6 snRNA and inhibits U6-U2 and U6-U4 snRNA interactions during splicing. Rna. 1995;1:304–316. [PMC free article] [PubMed] [Google Scholar]
- 14.Woff T, O’Neil RE, Palese P. NS1-Binding protein (NS1-BP): a novel human protein that interacts with the influenza A virus nonstructural NS1 protein is relocalized in the nuclei of infected cells. J Virol. 1998;72:7170–7180. doi: 10.1128/jvi.72.9.7170-7180.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nemeroff ME, Barabino SM, Li Y, Keller W, Krug RM. Influenza virus NS1 protein interacts with the cellular 30 kDa subunit of CPSF and inhibits 3' end formation of cellular pre-mRNAs. Mol Cell. 1998;1:991–1000. doi: 10.1016/s1097-2765(00)80099-4. [DOI] [PubMed] [Google Scholar]
- 16.Qian XY, Alonso-Caplen F, Krug RM. Two functional domains of influenza virus NS1 protein are required for regulation of nuclear export of mRNa. J Virol. 1994;68:2433–2441. doi: 10.1128/jvi.68.4.2433-2441.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiu Y, Krug RM. The influenza virus NS1 protein is a poly(A)-binding protein that inhibits nuclear export of mRNAs containing poly(A) Journal of virology. 1994;68:2425–2432. doi: 10.1128/jvi.68.4.2425-2432.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Satterly N, et al. Influenza virus targets the mRNA export machinery and the nuclear pore complex. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:1853–1858. doi: 10.1073/pnas.0610977104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcia-Sastre A, et al. Influenza A virus lacking the NS1 gene replicates in interferon-deficient systems. Virology. 1998;252:324–330. doi: 10.1006/viro.1998.9508. [DOI] [PubMed] [Google Scholar]
- 20.Brugarolas J, et al. Regulation of mTOR function in response to hypoxia by REDD1 and the TSC1/TSC2 tumor suppressor complex. Genes Dev. 2004;18:2893–2904. doi: 10.1101/gad.1256804. gad.1256804 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma XM, Blenis J. Molecular mechanisms of mTOR-mediated translational control. Nat Rev Mol Cell Biol. 2009;10:307–318. doi: 10.1038/nrm2672. nrm2672 [pii] [DOI] [PubMed] [Google Scholar]
- 22.Chakraborty P, et al. Nucleoporin levels regulate cell cycle progression and phase-specific gene expression. Developmental cell. 2008;15:657–667. doi: 10.1016/j.devcel.2008.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tumpey TM, et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;310:77–80. doi: 10.1126/science.1119392. 310/5745/77 [pii] [DOI] [PubMed] [Google Scholar]
- 24.Hresko RC, Mueckler M. mTOR.RICTOR is the Ser473 kinase for Akt/protein kinase B in 3T3-L1 adipocytes. The Journal of biological chemistry. 2005;280:40406–40416. doi: 10.1074/jbc.M508361200. M508361200 [pii] [DOI] [PubMed] [Google Scholar]
- 25.Sarbassov DD, Guertin DA, Ali SM, Sabatini DM. Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science. 2005;307:1098–1101. doi: 10.1126/science.1106148. 307/5712/1098 [pii] [DOI] [PubMed] [Google Scholar]
- 26.Rubinsztein DC, Gestwicki JE, Murphy LO, Klionsky DJ. Potential therapeutic applications of autophagy. Nat Rev Drug Discov. 2007;6:304–312. doi: 10.1038/nrd2272. nrd2272 [pii] [DOI] [PubMed] [Google Scholar]
- 27.Vega-Rubin-de-Celis S, et al. Structural analysis and functional implications of the negative mTORC1 regulator REDD1. Biochemistry. 2010;49:2491–2501. doi: 10.1021/bi902135e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buchkovich NJ, Yu Y, Zampieri CA, Alwine JC. The TORrid affairs of viruses: effects of mammalian DNA viruses on the PI3K-Akt-mTOR signalling pathway. Nat Rev Microbiol. 2008;6:266–275. doi: 10.1038/nrmicro1855. nrmicro1855 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cooray S. The pivotal role of phosphatidylinositol 3-kinase-Akt signal transduction in virus survival. The Journal of general virology. 2004;85:1065–1076. doi: 10.1099/vir.0.19771-0. [DOI] [PubMed] [Google Scholar]
- 30.Ehrhardt C, et al. Influenza A virus NS1 protein activates the PI3K/Akt pathway to mediate antiapoptotic signaling responses. Journal of virology. 2007;81:3058–3067. doi: 10.1128/JVI.02082-06. JVI.02082-06 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hale BG, Jackson D, Chen YH, Lamb RA, Randall RE. Influenza A virus NS1 protein binds p85beta and activates phosphatidylinositol-3-kinase signaling. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:14194–14199. doi: 10.1073/pnas.0606109103. 0606109103 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shin YK, Liu Q, Tikoo SK, Babiuk LA, Zhou Y. Influenza A virus NS1 protein activates the phosphatidylinositol 3-kinase (PI3K)/Akt pathway by direct interaction with the p85 subunit of PI3K. The Journal of general virology. 2007;88:13–18. doi: 10.1099/vir.0.82419-0. 88/1/13 [pii] [DOI] [PubMed] [Google Scholar]
- 33.Zhirnov OP, Klenk HD. Control of apoptosis in influenza virus-infected cells by up-regulation of Akt and p53 signaling. Apoptosis. 2007;12:1419–1432. doi: 10.1007/s10495-007-0071-y. [DOI] [PubMed] [Google Scholar]
- 34.Konig R, et al. Human host factors required for influenza virus replication. Nature. 2010;463:813–817. doi: 10.1038/nature08699. nature08699 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brugarolas J. mTORC1 signaling and hypoxia. In: Polunovsky V, Houghton PJ, editors. mTOR pathway and mTOR inhibitors in cancer therapy. Humana Press; 2010. in press. [Google Scholar]
- 36.Todd DJ, Lee AH, Glimcher LH. The endoplasmic reticulum stress response in immunity and autoimmunity. Nat Rev Immunol. 2008;8:663–674. doi: 10.1038/nri2359. nri2359 [pii] [DOI] [PubMed] [Google Scholar]
- 37.Zinkernagel AS, Johnson RS, Nizet V. Hypoxia inducible factor (HIF) function in innate immunity and infection. J Mol Med. 2007;85:1339–1346. doi: 10.1007/s00109-007-0282-2. [DOI] [PubMed] [Google Scholar]
- 38.Krishnamoorthy J, Mounir Z, Raven JF, Koromilas AE. The eIF2alpha kinases inhibit vesicular stomatitis virus replication independently of eIF2alpha phosphorylation. Cell Cycle. 2008;7:2346–2351. doi: 10.4161/cc.6323. 6323 [pii] [DOI] [PubMed] [Google Scholar]
- 39.Jin H-O, et al. Activating transcription factor 4 and CCAAT/enhancer-binding protein-β negatively regulate the mammalian target of rapamycin via Redd1 expression in response to oxidative and endoplasmic reticulum stress. Free Radical Biology & Medicine. 2009;46:1158–1167. doi: 10.1016/j.freeradbiomed.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 40.Whitney ML, Jefferson LS, Kimball SR. ATF4 is necessary and sufficient for ER stress-induced upregulation of REDD1 expression. Biochem Biophys Res Commun. 2009;379:451–455. doi: 10.1016/j.bbrc.2008.12.079. S0006-291X(08)02494-7 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Costa-Mattioli M, Sossin WS, Klann E, Sonenberg N. Translational control of long-lasting synaptic plasticity and memory. Neuron. 2009;61:10–26. doi: 10.1016/j.neuron.2008.10.055. S0896-6273(08)01089-1 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shahbazian D, et al. Control of cell survival and proliferation by mammalian eukaryotic initiation factor 4B. Molecular and cellular biology. 2010;30:1478–1485. doi: 10.1128/MCB.01218-09. MCB.01218-09 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Farny NG, Hurt JA, Silver PA. Definition of global and transcript-specific mRNA export pathways in metazoans. Genes Dev. 2008;22:66–78. doi: 10.1101/gad.1616008. gad.1616008 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Keene JD. RNA regulons: coordination of post-transcriptional events. Nat Rev Genet. 2007;8:533–543. doi: 10.1038/nrg2111. nrg2111 [pii] [DOI] [PubMed] [Google Scholar]
- 45.Kao RY, et al. Identification of influenza A nucleoprotein as an antiviral target. Nat Biotechnol. 2010;28:600–605. doi: 10.1038/nbt.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hoffmann HH, Kunz A, Simon VA, Palese P, Shaw ML. Broad-spectrum antiviral that interferes with de novo pyrimidine biosynthesis. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:5777–5782. doi: 10.1073/pnas.1101143108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Choo AY, Blenis J. Not all substrates are treated equally: implications for mTOR, rapamycin-resistance and cancer therapy. Cell Cycle. 2009;8:567–572. doi: 10.4161/cc.8.4.7659. 7659 [pii] [DOI] [PubMed] [Google Scholar]
- 48.McNaney CA, et al. An automated liquid chromatography-mass spectrometry process to determine metabolic stability half-life and intrinsic clearance of drug candidates by substrate depletion. Assay Drug Dev Technol. 2008;6:121–129. doi: 10.1089/adt.2007.103. [DOI] [PubMed] [Google Scholar]
- 49.Yuen T, Wurmbach E, Pfeffer RL, Ebersole BJ, Sealfon SC. Accuracy and calibration of commercial oligonucleotide and custom cDNA microarrays. Nucleic Acids Res. 2002;30:e48. doi: 10.1093/nar/30.10.e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kanehisa M, et al. KEGG for linking genomes to life and the environment. Nucleic Acids Res. 2008;36:D480–484. doi: 10.1093/nar/gkm882. gkm882 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.