Abstract
OBJECTIVE
Examine the association of prepregnancy habitual consumption of fruits and fruit juices and gestational diabetes mellitus (GDM) risk.
RESEARCH DESIGN AND METHODS
A prospective study among women with at least one singleton pregnancy in the Nurses’ Health Study II from 1991 to 2001.
RESULTS
Among 13,475 women, 860 reported a first diagnosis of GDM. The adjusted relative risks (RRs) for GDM from the lowest to highest quintile of whole fruit consumption were 1.00 (referent), 0.80 (95% CI 0.65–0.98), 0.90 (0.73–1.10), 0.80 (0.64–1.00), and 0.93 (0.76–1.16), respectively. The corresponding RRs for fruit juice were 1.00, 0.82 (0.66–1.01), 0.78 (0.63–0.96), 0.84 (0.68–1.04), and 1.00 (0.81–1.23).
CONCLUSIONS
These data suggest that prepregnancy higher consumption of whole fruits is not associated with an increased GDM risk. The association between fruit juices and GDM risk appears to be nonlinear.
Although dietary factors have long been recognized for their roles in the development of impaired glucose tolerance, the association between intakes of fruit and fruit juice and the risk of gestational diabetes mellitus (GDM) has yet to be investigated. The objective of this study was to assess the association of prepregnancy habitual consumption of fruit and fruit juices and their subgroups with GDM risk in a large prospective cohort of U.S. women.
RESEARCH DESIGN AND METHODS
The Nurses’ Health Study II is an ongoing prospective cohort of female U.S. nurses. The cohort was initiated in 1989 and recruited 116,671 women aged 24 to 44. For this analysis, the final sample consisted of 13,475 women who did not have diabetes and major chronic diseases at baseline and were followed until 2001 (after which most women passed the reproductive age).
GDM cases were self-reported and updated every 2 years. A high validity of self-reported diagnosis of GDM in this cohort has been demonstrated (94% of women who reported to have GDM was confirmed by a physician in a validation study) (1). Dietary intake information was collected by a validated 133-item semiquantitative food frequency questionnaire (2) designed to assess food intake during the previous year. For this analysis, we summed up the intake of single items to determine the consumption of fruit (nine items) and 100% fruit juices (four items) (for more information, see Supplementary Data).
All statistical analyses were performed using SAS statistical software (version 8.2; SAS Institute, Cary, NC). In primary analyses, we calculated the cumulative average intakes of dietary variables to reduce within-person variation and to represent long-term dietary intakes. Relative risks (RRs) and 95% CIs of GDM were estimated using Cox proportional hazards models. Tests for nonlinear associations were performed using restricted cubic spline regressions (3).
RESULTS
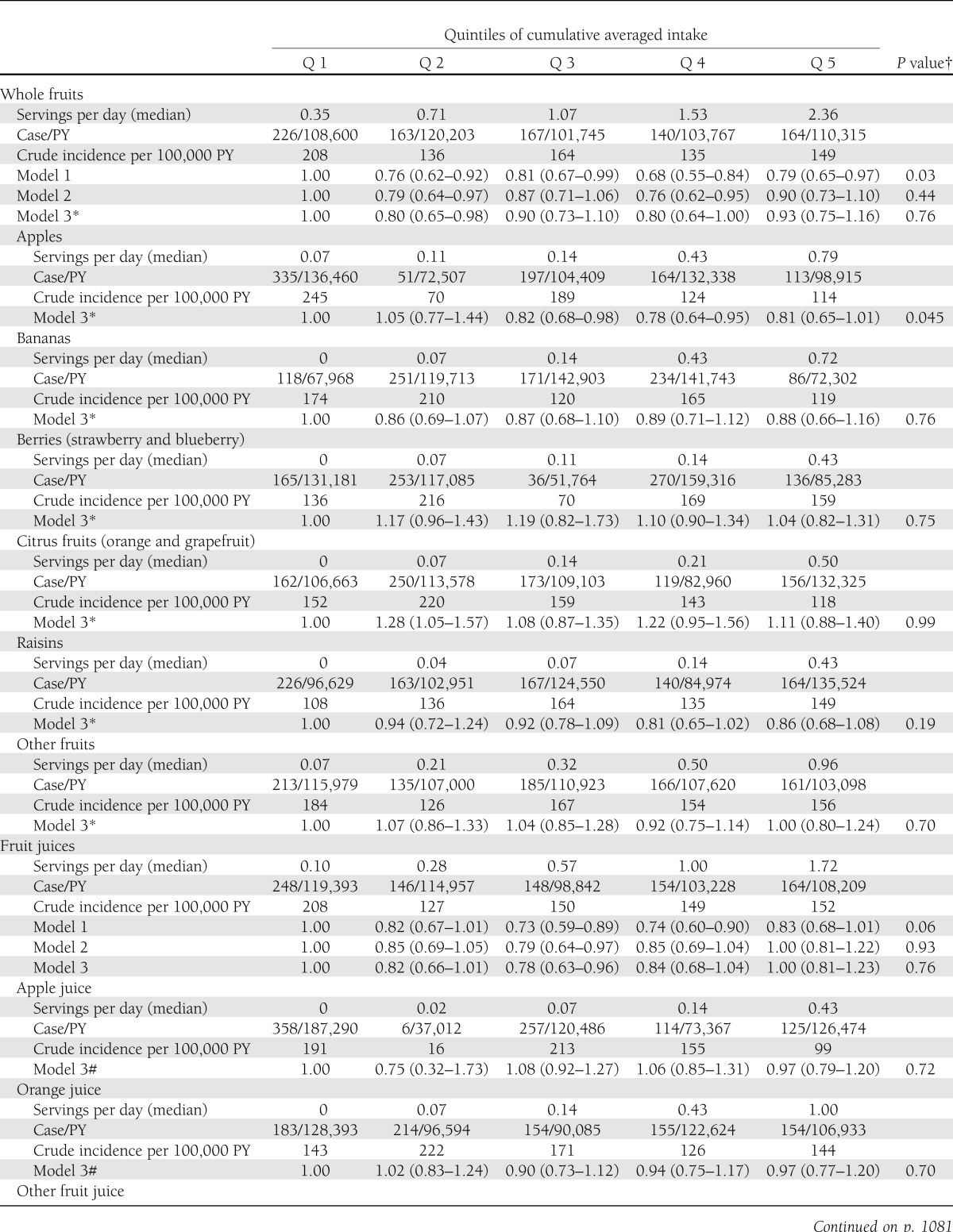
Among 13,475 eligible women, 860 reported a first diagnosis of GDM. At baseline, the median intake was 1.0 serving/day (Supplementary Table 1). After adjustment for age, parity, race, smoking, alcohol intake, physical activity, family history of diabetes, BMI, and other dietary factors (Table 1; model 3), the RRs across the lowest to highest quintiles of fruit consumption were 1.00 (referent), 0.80 (95% CI 0.65–0.98), 0.90 (0.73–1.10), 0.80 (0.64–1.00), and 0.93 (0.76–1.16). In stratified analyses according to participants’ BMI status (<25 or ≥25 kg/m2), family history of diabetes (yes or no), parity (1 or ≥2), or physical activity (low or high), the direction of the association between GDM risk and fruit consumption was consistent in each stratum (data not shown). For subgroups of fruit and the risk of GDM (Table 1), only intake of apple was significantly associated with GDM risk. When apple intake was treated as a continuous variable, each additional serving per day of apple was associated with a 25% lower risk of GDM (95% CI 1–44). The association of 100% fruit juices with GDM risk was nonlinear, with the lowest risk being among women with moderate consumption (Table 1).
Table 1.
RR (95% CI) of GDM in relation to whole fruits and fruit juice consumption among participants in the Nurses’ Health Study II (N = 13,475; GDM case subjects n = 860)
CONCLUSIONS
In this large prospective study, we found that habitual high consumption of fruits before pregnancy was not associated with increased GDM risk. For whole fruit, a slightly lower risk was observed in the 2nd and 4th quintiles as compared with the lowest quintile after controlling for known risk factors of GDM. Among specific fruits, higher apple consumption was associated with a modestly reduced risk of GDM. The association of total fruit juices with GDM risk was nonlinear, with the lowest risk being among women in the 3rd quintile of consumption.
We are unaware of published studies that prospectively examine the association of prepregnancy consumptions of fruit and fruit juices with the risk of GDM. Previous prospective studies on fruit intake and type 2 diabetes risk have yielded mixed results (4–8). Fruits have high antioxidant and fiber content as well as relatively low energy density and low glycemic load. In addition, fruits contain numerous bioactive components, such as vitamins, minerals, carotenoids, folates, flavonoids, and polyphenol, which have been suggested to be beneficial in insulin sensitivity and/or pancreatic β-cell function by relieving oxidative stress (9). However, fruits also contain a relatively high amount of sugar (i.e., fructose), which has been directly linked to impaired pancreatic β-cell function in humans (10). It is highly likely that the overall health effect of whole fruit is a mix of many bioavailable compounds present in whole fruit and is dependent on the individuals’ baseline consumption level.
Our finding of an inverse association between apple intake and GDM risk is consistent with two studies on apples and type 2 diabetes risk (11,12). Apples provide a low glycemic index source of carbohydrate, and are a major source of flavonoids. However, in the current study, flavonoids were not significantly associated with GDM risk, and the association of apple intake with GDM remained significant after the adjustment of flavonoid intakes (data not shown). We speculate that other polyphenolic compounds (i.e., catechins), antioxidants (i.e., vitamin C and β-carotene), or unidentified dietary factors in apples, individually or in combination, may contribute to the potentially protective effects of apples on GDM risk.
The association of total fruit juices with GDM risk was nonlinear. The interpretation of this nonlinear association needs to be cautious. On one hand, vitamins, minerals, and phytochemicals in fruit juices may have beneficial effects for diabetes. On the other hand, fruit juices have lower fiber contents and higher glycemic load than whole fruit. At a moderate level of consumption, the beneficial effects from some components (i.e., vitamins and minerals) may counterbalance the potential adverse effects of the rapidly absorbed sugars. In this study, however, we were unable to completely rule out residual confounding from some unmeasured health behaviors associated with moderate fruit juice consumption.
In conclusion, our data suggest that prepregnancy higher consumption of whole fruits is not associated with increased GDM risk. The association of fruit juices with GDM risk appears to be nonlinear, with the lowest risk being among women with modest consumption. Further studies are warranted to confirm our observations.
Acknowledgments
This study was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health (to L.C., E.Y., and C.Z.), and the School of Public Health, Louisiana State University Health Science Center. The Nurses’ Health Study II was funded by research grants CA-50385 and DK-58845 from the National Institutes of Health.
No potential conflicts of interest relevant to this article were reported.
L.C. contributed to the design and analysis of the study and wrote the manuscript. F.B.H. interpreted the results and reviewed and edited the manuscript. E.Y. conducted the technique review and reviewed and edited the manuscript. D.K.T. reviewed and edited the manuscript. W.C.W. reviewed, edited, and commented on the manuscript. C.Z. contributed to the design and analysis of the study and reviewed and edited the manuscript. L.C. and C.Z. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in abstract form at the 69th Scientific Sessions of the American Diabetes Association, New Orleans, Louisiana, 5–9 June 2009.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-2105/-/DC1.
References
- 1.Solomon CG, Willett WC, Carey VJ, et al. A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA 1997;278:1078–1083 [PubMed] [Google Scholar]
- 2.Feskanich D, Rimm EB, Giovannucci EL, et al. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc 1993;93:790–796 [DOI] [PubMed] [Google Scholar]
- 3.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med 1989;8:551–561 [DOI] [PubMed] [Google Scholar]
- 4.Bazzano LA, Li TY, Joshipura KJ, Hu FB. Intake of fruit, vegetables, and fruit juices and risk of diabetes in women. Diabetes Care 2008;31:1311–1317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montonen J, Järvinen R, Heliövaara M, Reunanen A, Aromaa A, Knekt P. Food consumption and the incidence of type II diabetes mellitus. Eur J Clin Nutr 2005;59:441–448 [DOI] [PubMed] [Google Scholar]
- 6.Villegas R, Shu XO, Gao YT, et al. Vegetable but not fruit consumption reduces the risk of type 2 diabetes in Chinese women. J Nutr 2008;138:574–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ. Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ 2010;341:c4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamer M, Chida Y. Intake of fruit, vegetables, and antioxidants and risk of type 2 diabetes: systematic review and meta-analysis. J Hypertens 2007;25:2361–2369 [DOI] [PubMed] [Google Scholar]
- 9.Ceriello A. Oxidative stress and glycemic regulation. Metabolism 2000;49(Suppl. 1):27–29 [DOI] [PubMed] [Google Scholar]
- 10.Davis JN, Ventura EE, Weigensberg MJ, et al. The relation of sugar intake to beta cell function in overweight Latino children. Am J Clin Nutr 2005;82:1004–1010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knekt P, Kumpulainen J, Järvinen R, et al. Flavonoid intake and risk of chronic diseases. Am J Clin Nutr 2002;76:560–568 [DOI] [PubMed] [Google Scholar]
- 12.Song Y, Manson JE, Buring JE, Sesso HD, Liu S. Associations of dietary flavonoids with risk of type 2 diabetes, and markers of insulin resistance and systemic inflammation in women: a prospective study and cross-sectional analysis. J Am Coll Nutr 2005;24:376–384 [DOI] [PubMed] [Google Scholar]