Abstract
OBJECTIVE
Our objective was to determine the secular trend in prevalence of type 2 diabetes in Shanghai, China.
RESEARCH DESIGN AND METHODS
Two consecutive population-based surveys for type 2 diabetes were conducted in randomly selected adults aged 35–74 years in Shanghai in 2002–2003 (n = 12,329) and in 2009 (n = 7,423). Diagnosed type 2 diabetes was determined based on self-report, whereas those undiagnosed were identified by measured fasting and postload glucose according to 2009 American Diabetes Association criteria.
RESULTS
Age-standardized prevalence of diagnosed and undiagnosed type 2 diabetes increased from 5.1 and 4.6% in 2002–2003 to 7.4 and 5.2% in 2009. The prevalence of type 2 diabetes increased with age and was higher among men and in urban residents in both surveys (P < 0.001). Between the two surveys, the increase in the prevalence was more evident in the rural population (P < 0.001) and appeared more rapid in younger birth cohorts (P < 0.05).
CONCLUSIONS
Our results suggest that Shanghai has experienced an increasing burden of type 2 diabetes.
Type 2 diabetes is a major global health problem that affects over 285 million individuals worldwide (1). Over past decades, a continuous increase in prevalence of type 2 diabetes, which parallels a marked lifestyle transition and a worldwide epidemic of obesity, has been observed in both developed and developing countries (2). Unlike the gradual transition in most Western countries, these changes in China have occurred over a very short time (3). This may have led to a more rapidly increasing burden of type 2 diabetes. In this study, we evaluated the trend of type 2 diabetes in Chinese adults using the data derived from two population-based surveys in Shanghai.
RESEARCH DESIGN AND METHODS
In the 2002–2003 survey, representative samples of permanent residents, for at least 5 years, of both urban and rural Shanghai between the ages of 15–74 years were randomly selected through a multistage sampling process (4). Of a total of 17,526 eligible subjects, 14,401 (82.17%) participated the survey.
The 2009 survey adopted a similar sampling process and similar inclusion and exclusion criteria, except that only those aged 35–74 years were eligible. Among 11,844 eligible adults, 7,964 (67.24%) were interviewed.
After excluding subjects younger than age 35 years from the 2002–2003 study and those in both studies with an incomplete questionnaire, the final analysis included 12,329 subjects (5,050 men and 7,279 women; 8,177 urban and 4,152 rural residents) in the 2002–2003 survey and 7,423 subjects (3,461 men and 3,962 women; 5,357 urban and 2,066 rural residents) in the 2009 survey. The urban/rural split in the samples matched those in Shanghai population of the year. The institutional review board at Shanghai Municipal Center of Disease Control and Prevention approved the study. Informed consent was obtained from each participant before data collection.
Data collection
Although the questionnaire used in 2009 included more questions, for the purposes of this article, we only considered the following information: demographic characteristics, a previous diagnosis of type 2 diabetes, and type 2 diabetes among first-degree relatives. Diagnosed diabetes was identified by a positive response to the question: “Have you ever been diagnosed with type 2 diabetes by a doctor?” At the interview, body weight, height, and waist circumference (WC) were obtained using a standardized protocol.
After an overnight fast of at least 10 h, a preload venous blood specimen was collected for each participant. For each subject with no history of type 2 diabetes, a blood sample was drawn at 120 min after an oral glucose tolerance test using a standard 75-g glucose solution. Plasma glucose was measured using the glucose oxidase-peroxidase method. Individuals with undiagnosed type 2 diabetes were identified according to measured glucose levels by 2009 American Diabetes Association criteria (5).
Statistical analysis
Age-standardized prevalence was calculated with the direct method according to the Chinese population data in 2006 (6,7). The χ2 test was used to test the difference in frequency. SAS version 8.2 (SAS Institute, Cary, NC) was used for all statistical analyses.
RESULTS
The participants in the two surveys were comparable in BMI (P > 0.05). Compared with the subjects in the 2002–2003 survey, the participants of the 2009 survey, both men and women, urban and rural residents, were more likely to have more education, higher per capita income, larger WC, and a positive family history of type 2 diabetes (P < 0.001). In both surveys, the rural subjects had less education, lower income, and smaller BMI and WC than urban residents (P < 0.001).
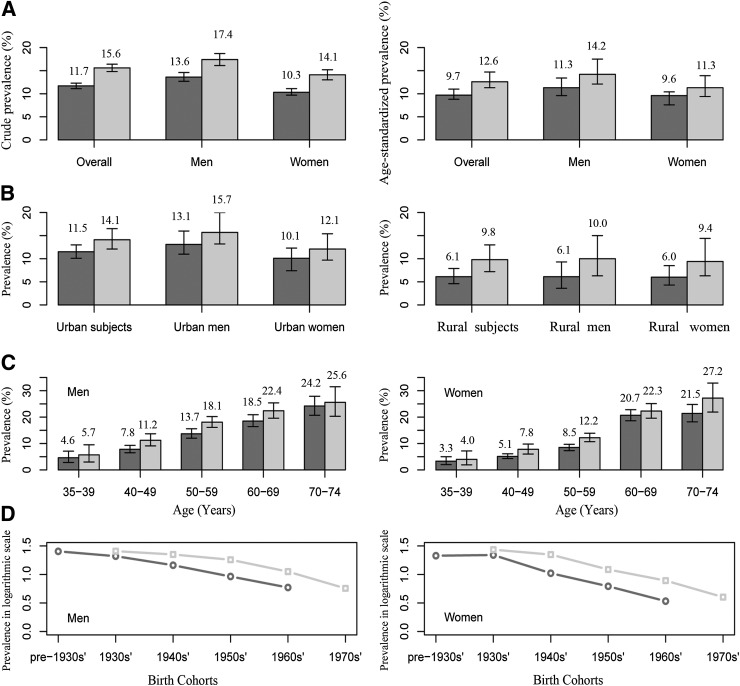
Both crude and age-standardized prevalence of type 2 diabetes were significantly higher in 2009 (15.6 and 12.6%, respectively) than in 2002–2003 (11.7 and 9.7%, respectively) (P < 0.0001) (Fig. 1). The increase came predominantly from diagnosed type 2 diabetes, with age-standardized prevalence of diagnosed and undiagnosed type 2 diabetes increasing from 5.1 and 4.6% in 2002–2003 to 7.4 and 5.2% in 2009. In the 2002–2003 survey, 30.5% of those with undiagnosed diabetes had isolated postload hyperglycemia, and the proportion reached 46.8% in the 2009 survey. The prevalence of type 2 diabetes increased with age and was higher among men and in urban residents in both surveys (P < 0.001). Between the two surveys, the increase was more evident in rural residents (P < 0.001) and was more rapid in younger birth cohorts, with a percentage change of 1.09, 1.21, 1.34, and 1.32% for the men who were born in the 1930s, 1940s, 1950s, and 1960s, and of 1.10, 1.39, 1.34, and 1.43, respectively, for the women (Ptrend < 0.05).
Figure 1.
Comparison of prevalence of type 2 diabetes in the 2002–2003( ) and 2009(
) and 2009( ) surveys. I bars indicate 95% CIs. A: Crude and age-standardized prevalence. B: Age-standardized prevalence in urban and rural areas. C: Age-specific prevalence in men and women. D: Prevalence by birth cohort in men and women (logrithmic scale).
) surveys. I bars indicate 95% CIs. A: Crude and age-standardized prevalence. B: Age-standardized prevalence in urban and rural areas. C: Age-specific prevalence in men and women. D: Prevalence by birth cohort in men and women (logrithmic scale).
CONCLUSIONS
As the largest city and one of the most economically developed areas in China, Shanghai usually has a higher prevalence of type 2 diabetes than other cities in China (6,8). In this study, the overall age-standardized prevalence of type 2 diabetes, combining urban and rural areas, increased from 9.7% in 2002–2003 to 12.6% in 2009 among Chinese adults aged 35–74 years in Shanghai. The age-specific prevalences in 2002–2003 were lower than those in the survey by Yang et al. (6) in several age groups but higher in some others. The prevalence in 2009, on the other hand, was significantly higher in each age-group (P < 0.05). Our results confirm the data in the report by Yang et al. and indicate a heavy and growing burden of type 2 diabetes in China.
Aging of population has been one of the contributors to the rapid increase in diabetes burden in China (9). As one of aging cities in China, Shanghai had 3.0 million adults at ages of 60+ years in 2008, accounting for more than 20% of its residents (10), and the proportion is still increasing.
Although the increase in prevalence of type 2 diabetes between two surveys predominantly came from diagnosed type 2 diabetes, approximately half the cases of type 2 diabetes remained undiagnosed in both surveys. The findings are similar to previous reports (6,11), and can be partly explained by the fact that fasting glucose was usually used alone to screen type 2 diabetes in China (12,13). Isolated postload hyperglycemia has been reported to be more common among Asian type 2 diabetic patients (6,14), thus there may exist more undetected type 2 diabetic subjects in China, representing a major public health problem in the country.
Limitations of this study include low response rate and a difference in sample size between the two surveys. This study, however, has several strengths, including representative samples of adult population in Shanghai, oral glucose tolerance tests for all participants without history of type 2 diabetes, and extensive interpopulation comparison.
Conclusively, the prevalence of type 2 diabetes increased in Shanghai during past years. The experience in Shanghai may predict the situation of the country in near future.
Acknowledgments
This study was funded by the Key Program of Shanghai Municipal Committee of Science and Technology (04 DZ19502), and the Shanghai Medical Development Program (01ZD001).
No potential conflicts of interest relevant to this article were reported.
R.L., W.H.X., and W.J.Z. coordinated the study and contributed to study design, statistical analysis, and draft and revision of the manuscript. W.L. and S.N.Z. contributed to acquisition of funding, study design, and data acquisition. Q.W.J. and G.M.Z. contributed to study design and revision of the manuscript. Y.Y.L., L.S., Q.D.Y., and Y.R. contributed to data acquisition. J.J. contributed to statistical analysis. W.H.X. and W.J.Z. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the study participants of the two cross-sectional surveys and the healthcare workers in each community involved. They also thank Dr. Xinzhi Zhang of the U.S. Centers for Disease Control and Prevention for his constructive comments on the earlier version of the manuscript.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of Fudan University and the Shanghai Center for Disease Control and Prevention.
References
- 1.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4–14 [DOI] [PubMed] [Google Scholar]
- 2.Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care 2011;34:1249–1257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Normile D. Public health. A sense of crisis as China confronts ailments of affluence. Science 2010;328:422–424 [DOI] [PubMed] [Google Scholar]
- 4.Li R, Lu W, Jia J, et al. Relationships between indices of obesity and its cardiovascular comorbidities in a Chinese population. Circ J 2008;72:973–978 [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2009;32(Suppl. 1):S62–S67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang W, Lu J, Weng J, et al. ; China National Diabetes and Metabolic Disorders Study Group Prevalence of diabetes among men and women in China. N Engl J Med 2010;362:1090–1101 [DOI] [PubMed] [Google Scholar]
- 7.National Bureau of Statistics of China. China Statistical Yearbook - 2006 [PDF online], 2006. Beijing, China Statistics Press. Available from http://www.stats.gov.cn/tjsj/ndsj/2007/indexeh.htm Accessed 5 July 2010,
- 8.Pan XR, Yang WY, Li GW, Liu J, National Diabetes Prevention and Control Cooperative Group Prevalence of diabetes and its risk factors in China, 1994. Diabetes Care 1997;20:1664–1669 [DOI] [PubMed] [Google Scholar]
- 9.Yang G, Kong L, Zhao W, et al. Emergence of chronic non-communicable diseases in China. Lancet 2008;372:1697–1705 [DOI] [PubMed] [Google Scholar]
- 10.National Bureau of Statistics of China. Shanghai Statistical Yearbook 2009. Beijing, China Statistics Press, 2009
- 11.Jia WP, Pang C, Chen L, et al. Epidemiological characteristics of diabetes mellitus and impaired glucose regulation in a Chinese adult population: the Shanghai Diabetes Studies, a cross-sectional 3-year follow-up study in Shanghai urban communities. Diabetologia 2007;50:286–292 [DOI] [PubMed] [Google Scholar]
- 12.Liu S, Wang W, Zhang J, et al. Prevalence of diabetes and impaired fasting glucose in Chinese adults, China National Nutrition and Health Survey, 2002. Prev Chronic Dis 2011;8:A13. [PMC free article] [PubMed] [Google Scholar]
- 13.Hu D, Sun L, Fu P, et al. Prevalence and risk factors for type 2 diabetes mellitus in the Chinese adult population: the InterASIA Study. Diabetes Res Clin Pract 2009;84:288–295 [DOI] [PubMed] [Google Scholar]
- 14.Lü Q, Tong N, Liu Y, et al. Community-based population data indicates the significant alterations of insulin resistance, chronic inflammation and urine ACR in IFG combined IGT group among prediabetic population. Diabetes Res Clin Pract 2009;84:319–324 [DOI] [PubMed] [Google Scholar]