Abstract
Purpose
To present a conceptual framework which accounts for the relationship between community violence exposures and youth HIV risk behaviors.
Methods
This article provides an overview of existing research on the links between community violence exposure and HIV risk for youth and offers a conceptual framework for clarifying how community violence exposure might contribute to HIV sexual risk.
Results
Increasing empirical findings substantiate that the links between community violence exposure and HIV risk behaviors among youth are mediated by psychological problem behaviors, low school success and negative peer influences.
Conclusions
Researchers have identified the behaviors that place teens at risk for becoming infected with HIV. However, most scholars have overlooked the potential importance of community violence exposure in influencing such behaviors. This paper presents new directions for adolescent research and HIV interventions based on an integrated conceptual framework.
Keywords: youth, community violence exposure, HIV risk
In the United States, human immunodeficiency virus (HIV) incidence and community violence exposure (CVE) are two major youth concerns that are alarmingly problematic among youth. More HIV infections occurred among young people under 30 (aged 13–29) than any other age group (34%, or 19,200). Among this group, males and racial minorities, are overrepresented1. The high frequency of behavioral risk factors such as early sexual début, incorrect and inconsistent condom use, multiple sexual partners and using alcohol and drugs before sex are among the factors may account for this age disparity in transmission2.
Community violence exposure (CVE) consists of violent incidents (e.g., witnessing or being a victim of robberies, muggings, gang-related deaths, or homicides) taking place outside the home between individuals who are unrelated and who may or may not know each other3. In the U.S., CVE is highest among adolescents and young adults4. Homicides, however, only reflect one narrow aspect of CVE. It is estimated that the frequency of nonfatal injuries in 2008 was at least 120 times that of youth homicides4. Unfortunately, what has been less studied is how CVE may directly and indirectly heighten HIV sexual risk behaviors among youth.
In this article, we provide an overview of the empirical literature which documents associations between CVE and HIV-related sexual risk behaviors among young persons. Next, based on empirical findings and supported by theoretical underpinnings we provide a conceptual model that identifies pathways linking CVE and HIV risk behaviors. We conclude with an agenda for research.
We conducted a review of published literature to identify empirical studies on community violence exposure and HIV-related risk behaviors in the United States. PsychINFO and MEDLINE, two online databases in the social and health sciences arenas, were searched for English-language publications since 1981, the time period when HIV came to national attention. Variations of the following terms were used in the search: community violence, community violence sequelae, HIV risks, STD risks, and sexual behaviors. Additional studies were identified through bibliographic review of acquired articles. Inclusion criteria were: youth as a population focus, quantitative studies with multivariable analyses, and assessment of at least one of the following outcomes: sexual début; sexual activity; multiple sexual partners; inconsistent, improper, or no condom use; and using alcohol or drugs during sex. See Table 1.
Table 1. Community Violence Exposures and HIV-Related Risk Behaviors.
| Reference | Purpose/ design | Sample | Results |
|---|---|---|---|
| Albus et al, 2004 [11] | To examine the link between violence exposure and health risk behaviors Cross-sectional |
N:167 Age:10-19 years Gender: males and females Ethnicity: majority African American Control variables: age, gender, ethnicity |
Knowledge of violence was associated with substance use and sex Victimization was associated with sex. |
| Berenson et al, 2001 [12] | To examine relationship between violence exposure and health-risk Cross-sectional |
N: 517 Age: 9-18 years Gender: girls Ethnicity: 25% White; 42% African American; 30% Hispanic Control variables: race, age, school enrollment, and having repeated a grade |
Girls who witnessed violence were 2-3 times more likely than non-exposed peers to report using drugs before sex, and having intercourse with a partner who had multiple partners. Girls who were victims of community violence only were 2-4 times more likely than their peers not exposed to such violence to report early sexual début, sex with strangers, multiple sex partners, and test positive for a STD. Girls who both witnessed and were victims of community violence were 3-6 times more likely than their peers not exposed to such violence to use drugs before sex |
| Brady, 2006 [13] | To examine the relationship between lifetime community violence exposure and risk behaviors Cross-sectional |
N: 319 Age: 18-20years Gender: males and females Ethnicity: majority white Control variables: gender, ethnic minority status, personality characteristics, aggression, family SES, family support, neighborhood collective efficacy |
Greater lifetime violence exposure was associated with greater lifetime sexual risk-taking (ever had sex, number of sexual partners, number of partners last 3 months) |
| Stiffman et al, 1995 [14] | To examine the relationship between personal and environmental factors and changes in HIV risk behaviors Longitudinal |
N: 602 Age: 16- 21 Gender: males and females Ethnicity: majority African American Control variables: earlier problem behaviors |
Substance use combined with level of community murders predicted increased HIV risk behaviors from adolescence to adulthood Childhood sexual abuse combined with level of community murders predicted increased HIV risk behaviors from adolescence to adulthood |
| Voisin, 2003 [15] | To examine the relationship between violence victimization and sexual risk behaviors Cross-sectional study |
N:120 Age: 14-17 years Gender: males Ethnicity: African American Control variables: SES, household composition, family support, and negative peer influences |
Males who were victims of community violence were more likely than peers not exposed to such violence to engage in HIV sexual risk behaviors |
| Voisin, 2005 [16] | To examine the relationship between community violence and HIV risk behaviors Cross-sectional |
N: 409 Age: 14-18 years Gender: males and females Ethnicity: majority African American and Hispanic Control variables: age, family composition, income, parents' education level, self efficacy |
Youth exposed to community violence were 3 times more likely to report sex without condoms, sex after drug use, and sex with multiple partners than peers not exposed to such violence |
| Voisin et al, 2007 [17] | To examine relationship between witnessing community violence exposure and health risk behaviors Cross-sectional |
N:550 Age: 14-18 years Gender: males and females Ethnicity: 41% White, 39% African American Control variables: gender, free school lunch, religiosity, family social support, community monitoring |
Youth exposed to community violence in the last 12 months prior to being detained, were 1.7 times more likely to have not used a male condom, 1.6 times more likely to be high on alcohol or drugs during sex, and 2.1 times more likely to have sex with a partner who was high on drugs, within the past 2 months prior to being detained |
Rates of Community Violence Exposure (CVE)
A recent national study on community violence found that about 55% of urban adolescents have been exposed to some type of community violence during their lifetime5. Rates of community violence differ greatly depending on how violence exposure is measured (e.g., witnessing, victimization, or both), the population being assessed (e.g., children or adolescents), and geographical location (e.g., rural versus urban)6.
Though CVE is widespread in the U.S., its incidence is higher in large, urban cities and within impoverished enclaves. This partly results in racial minorities being overrepresented in community violence exposure7. Though official crime statistics and homicide rates are only narrow measures of tracking violence exposure rates, they do demonstrate the disparities in CVE with rates being higher for young males and racial minorities. For instance, males ages 15 to 19 are about four times more likely than females to die from homicide8. Additionally, in 2006, the homicide rate for black male teens was 66.4 per 100,000, nearly 20 times higher than the rate for white males (3.4 per 100,000). Rates for other groups were 28.4 per 100,000 for Hispanic males, 16.9 per 100,000 for American Indian males, and 11.5 per 100,000 for Asian and Pacific Islander males.9
Community Violence Exposure and HIV-Related Risk Behaviors
We know from prior research that CSA (not a form of CVE) is associated with risky sexual behaviors among youth10. However, researchers have only recently begun to explore the link between CVE and HIV sexual risk behaviors. Collectively, an increasing number of empirical studies 11-17 across various youth populations show that high rates of CVE (either as witnesses, victims, or both) are positively related to youth HIV-sexual risk behaviors.
For instance, in terms of direct victimization, a study of African American high school males, controlling for income, family composition, and network norms, found that being exposed to community violence was associated with higher rates of sexual risk-taking (e.g., having sex without condoms)15. Similarly, another study of multiethnic youth (aged 14–19), controlling for poverty-related variables, and household composition, found that victims of community violence were almost four times more likely than their nonvictim peers to have had sex without condoms, have sex after drug use, and to have engaged in group sex16.
With regard to witnessing community violence, results controlling for race, gender, and socioeconomic and family factors have documented that among a multiethnic detained youth sample, participants who witnessed violence in the year prior to being detained were twice more likely to report having been high on alcohol or other drugs during sexual intercourse and to have had sex with a partner who was high on alcohol or other drugs than peers not exposed to community violence17.
Researchers have attempted to determine whether there is a differential impact between witnessing or victimization on HIV-related drug and sexual risk behaviors. Results suggest that victimization has a stronger relationship to these risk behaviors than witnessing alone. For instance, in a study of 517 racially-diverse, adolescent girls seeking contraceptive care, results controlling for age, school enrollment, and having repeated a grade indicated that participants who had witnessed violence were two to three times more likely to report drinking alcohol or using other drugs before sex, and having intercourse with a risky sexual partner. Those who experienced violence, however, were two to four times more likely than those who only witnessed violence to report sex with strangers, multiple sexual partners, and testing positive for sexually transmitted diseases12. Longitudinal findings also substantiate results from cross-sectional research documenting that CVE and HIV-related factors co-vary14. Given the above observations, a conceptual formulation of pathways that may account for such relationships is warranted.
Conceptual Model
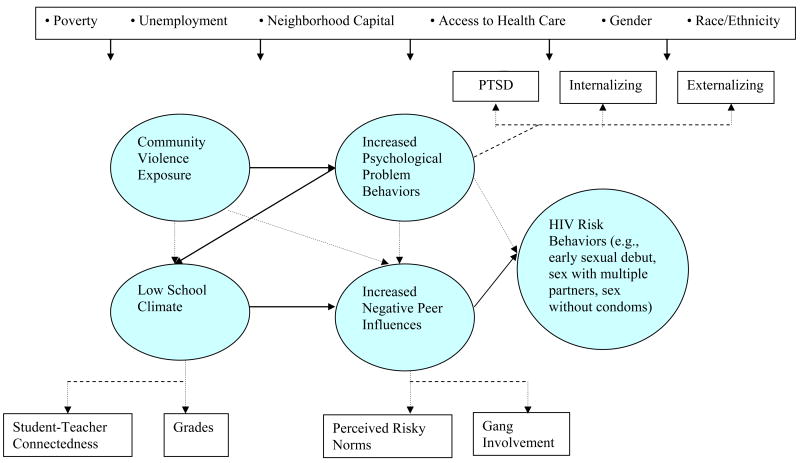
Figure 1 illustrates an integration of ecological spheres (i.e., structural, community, school, peer and individual level factors) that are rarely considered collectively when examining adolescent HIV risk behaviors. This socio-ecological perspective provides important underpinnings for this model. Structural disadvantage with regards to race/ethnicity, poverty, unemployment, lack of neighborhood social capital, access to health care, among others, are important meta variables that influence all domains of this model and predisposes some youth to higher rates of exposure to community violence and its correlates18. There is increasing recognition that ecological factors influence risky sexual behaviors19. Given this, we presume that disparities associated with higher rates of community violence (e.g., psychological problem behaviors, low school success, and negative peer group involvement) result in differential rates of early sexual début, having sex with multiple partners, incorrect and inconsistent condom use, among others. A major innovation of this model is that we conceptually frame what other studies, perhaps because of disciplinary boundaries, have traditionally considered outcome variables (i.e., psychological problem behaviors, low school success, peer influences) as pathways that provide a link from CVE to drug and HIV-related sexual risk behaviors among youth and adolescents.
Figure 1. Conceptual model linking community violence exposure and HIV sexual risk behaviors.
Note: Empirically validated relationships are represented by solid lines; hypothesized relationships are represented by broken lines.
Figure 1 provides a diagrammatic summary of the empirical studies that support this framework. The solid lines represent associations with substantial empirical studies that support the linkages. The dotted lines are hypothesized associations that require further empirical testing. The solid lines, based on existing empirical studies, indicate that CVE is related to low school success by way of psychological distress20-23; and that low school success and HIV-risk behaviors are mediated by peer influences 24. The hypothesized relationships (indicated by broken lines) are based on earlier conceptual work and clinical observations, and need to be tested in future empirical work.
As a means of linking social interaction, institutions, and individual behavior, social control theory25 provides one of many organizing frameworks for this conceptual model. One component of this theory posits that the bond to conventional society is represented by four elements: attachment to others, commitment to conventional institutions, involvement in conventional activities, and belief in conventional values25. It is highly likely that CVE and social disorganization are interrelated and mutually reinforcing weakening the bonds to prosocial “agents.” These agents often are parents and teachers who might also be threatened by loss of safety and consequently less able to adequately monitor and supervise their youth25. Weak social attachment to prosocial figures lessens young people's ability to make sense of the violence around them, which heightens their vulnerability for displaying psychological problem behaviors (e.g., PTSD symptoms, depression, and anxiety). Consequently, youth who display aggressive and other problem behaviors tend to be assessed more negatively by teachers and prosocial peers, placing them at greater risk for low school success25,26 (e.g., poorer grades and low student-teacher connectedness). Accordingly, these youth may feel uncommitted to conventional, societal norms, which may heighten their risk of becoming attached to or being recruited by deviant peers (e.g., gangs especially for boys)28. Such peers, although considered deviant by the larger society, can provide not only a sense of group belonging, status and protection in violent communities, but also sources of income24. Membership in such peer groups results in social learning that may reinforce risky norms, such as unsafe sexual behaviors28. Within this destabilized environment of community norms and authoritative agents, we document that a pathway accounting for the relationship between CVE and HIV drug and sexual risk behavior exists through psychological problem behaviors, low school success, and negative peer influences.
However, there are other potential direct and indirect pathways to sexual risk outcomes as indicated by broken lines. For instance, as shown in Figure 1, CVE may directly impact low school success (e.g., poorer grades and positive engagement with teachers) because youth exposed to such violence may be absent from school due to injury or fear of attending school. Other potential relationships may also exist. Researchers have posited that CVE can lead to desensitization to risk, causing youth in communities plagued by high rates of CVE to become inured to such exposures29 including other risks such as unsafe sexual behaviors and the fear of contracting HIV. Conversely, youth who do not become risk desensitized may develop psychological distress (e.g., PTSD, depression, anxiety). Such symptoms for adolescent girls may lead to less perceived control in sexual relationships, perceiving greater barriers to condom use or adverse consequences such as abandonment, abuse or relationship conflict 30. For some adolescent boys, patterns of externalizing coping may be more consistent with gendered patterns of coping resulting in greater illicit drug use and risky sex to mitigate the psychological trauma associated with CVE31. These various hypothesized pathways should be analyzed further using longitudinal studies to guide researchers to the most promising points for intervention.
Not all youth who are exposed to community violence display psychological problem behaviors, nor does such distress always lead to low school success and so forth. Given that this is an exploratory area of research, and our conceptual framework is the first to account for links between community violence exposure and drug and sexual risk, we present a mediational framework (i.e., linking pathways through which CVE may influence HIV risks). However, we do not discuss the factors that may moderate the relationship among variables. What is necessary is empirical testing of this model, which will then enable researchers to identify empirically-grounded moderators. In the next section, we summarize the literature that provides evidence for the components of the model that have been empirically validated (i.e., the solid lines in the conceptual diagram).
Community Violence Exposure and Psychological Problem Behaviors
Post-Traumatic Stress Disorder and Symptoms
Violence exposure has often been commonly tied to several indicators of psychological problem behaviors, among them is PTSD. PTSD is characterized by three categories of symptoms: re-experiencing the traumatic event, avoidance of stimuli associated with the trauma, and persistent symptoms of increased arousal32. Reviews of the literature indicate that most youth studies report a positive relationship between exposure to community violence and PTSD symptoms, with girls more likely than boys to meet the criteria for PTSD symptoms 6. Research has also documented that effects can persist over time. For instance, a study of youth found that one year after a sniper attack, a significant number of participants reported suffering from moderate to severe PTSD symptoms 33.
Depression and Other Internalizing Behaviors
Reviews of the literature have found associations between CVE, depression, and other internalizing behaviors among adolescents, although the “dose” of the violence seems to matter6. For example, a large study performed on middle-school youth controlling for gender, grade, ethnicity/race, and socioeconomic status found that witnessing community violence predicted depression and anxiety27. However, another study found that community victimization, but not witnessing violence, was positively associated with depression and other internalizing behaviors34. Regarding lingering of negative effects, longitudinal research on inner-city adolescent boys found that exposure to community violence (both witnessing and victimization) controlling for previous status was associated with anxiety and depression over a 1-year period35.
Aggression and Other Externalizing Behavior Problems
Reviews of studies including three longitudinal investigations substantiate that community violence is also associated with aggression among youth6. For instance, longitudinal findings have documented that community violence was predictive of aggressive behaviors in children over a 4-year period after controlling for earlier antisocial behavior35. Similarly, in a sample of African American and Latino boys in grades 5 and 7, exposure to community violence (defined as both witnessing and victimization) was also associated with aggression, controlling for aggression in earlier grades and controlling for previous status35. With regards to the overall effects of CVE, significant gendered patterns persist. Generally, girls tend to report more internalizing psychological problem behaviors whereas boys reported more externalizing behaviors6.
Community Violence Exposure and Low School Success Mediated by Psychological Problem Behaviors
Several researchers have found direct associations between CVE and school success (i.e., student-teacher connections, grades, school behavior, school attendance, or safety)20-23. For instance research has shown that the frequency of witnessing a shooting or stabbing significantly predicted poorer school success, defined as grade retention and child-reported grades, controlling for gender, grade, ethnicity, and socioeconomic status29. Additionally, examination of a national probability sample of middle and high school students showed that students' self-reports of exposure to neighborhood and school danger were related to attendance, school behavior, and grades, controlling for gender, race, socioeconomic status, and urbanicity 37.
Empirical research utilizing a longitudinal design documented that participants who witnessed community violence reported lower school success (i.e., standardized test scores) over a two- year period and that this relationships was mediated by depressive symptoms 21. A more recent study of urban, African American high school students found that for boys, psychological distress variables collectively mediated the relation between CVE and school success (i.e., student-teacher connection and GPAs). Specifically, greater reported violence exposure was associated with lower student-teacher connectedness. For girls, community violence exposure was negatively related to both GPA and student-teacher connectedness via aggressive behavior20.
Low School Success and HIV Risks Behaviors Mediated by Negative Peer Influences
Numerous studies involving diverse youth populations have documented direct inverse relationships between measures of school success and HIV-related sexual risk behaviors38-41. For instance, a national school survey of adolescents in grades 7–12, controlling for sex, race, family structure, and poverty status found that school connectedness was associated with a delay in sexual début41. Similarly, researchers in a study of detained adolescents found that youth who reported low student-teacher connectedness prior to being detained were twice as likely to be sexually active, and engage in risky sexual behaviors relative to their peers who reported high teacher connectedness36.
Findings have also documented associations between school success and HIV-related risk factors. Researchers have shown that for adolescents residing in residential centers, AIDS knowledge, attitude, and behaviors could be predicted by school climate factors such as relationships with teachers and academic achievement40. Finally, findings also provide evidence that among adolescents, increased teacher support was associated with later initiation of first sexual intercourse40.
Recent findings have begun to document that peer influences mediate the relationship between school success and HIV-related risk behaviors with significant gender differences. For instance, among a high school sample of African American youth showed that GPA was negatively associated with both sexual début and risky sex for boys. Additionally, the relationship between student-teacher connectedness and risky sex was mediated by gang involvement. For girls, higher GPAs were associated with fewer norms favoring risky sex, drug use, and earlier sexual début. Moreover, the relationship between GPA, sexual début, and risky sex was mediated by risky peer norms24.
In summary, ample evidence documents that the relationship between community violence exposure and low school success is mediated by psychological distress. Another emerging body of work substantiates links between low school success and HIV-related risk behaviors is mediated by peer influences.
Methodological Considerations
We hope this conceptual model will generate and support future work in this area. In so doing, there are several methodological considerations which need to be addressed based on the limitations of the studies presented in this review. Several studies presented in this review, have controlled for gender and poverty when presenting their findings. However, few have systematically explored how structural disadvantage with regards to race/ethnicity, unemployment, lack of neighborhood social capital, and access to health care, may influence domains presented in this model. This gap represents a major domain for future inquiry.
Another major methodological consideration is that the vast majority of studies on the effects of exposure to community violence have been conducted using cross sectional studies. Few studies have followed participants form preadolescence to adolescence or even adulthood6. This highlights the need for more longitudinal studies to assess the short- and long-term effects of exposure to such violence and many of its related effects.
Conceptualizations of important concepts such as CVE, school success, and peer influences vary in the literature. While an argument can be made for measuring these constructs broadly, it poses significant challenges for comparing findings across studies. For instance, when community violence is combined into a single index comprised of witnessing and victimization, it is difficult to tease out the unique effects from witnessing, victimization or both. On the other hand, a meta-analyses has found minimal variation in the effects of witnessing or being a victim of community violence, which suggests possible, significant overlap between these categories6.
Many studies conducted on the effects of violence exposure and its sequelae have been conducted with racially mixed samples of youth6. Limited by inadequate sample sizes, several studies have differentially controlled for age, race, or gender. Gender in particular is likely to be an important consideration, given that theorists have suggested and empirical findings20,24 have documented that boys and girls negotiate different developmental pathways to risk outcomes. As an important next step, we should examine the relationships among key constructs in this model with large enough samples which would enable us to explore for ethnic and gender differences. Additionally, although several components of the model have been empirically evaluated across different studies, it will need to be tested across a large single population.
As earlier stated, although youth exposed to community violence are at increased risk for developing psychological distress and academic difficulties, not all youth experiences are affected in this way6. Therefore, our proposed conceptual model must first be empirically tested across a single sample, and potential moderators must be identified. It is likely that factors such as personal traits, gender, age, family functioning, and social support may moderate many of the associations in the model.
In summary, this conceptual model integrates several risk domains associated with HIV risk behaviors, and considers how community violence exposures might be related to psychological problem behaviors, low school success, and negative peer influences. Malleable approaches such as locating mental health intervention services in primary systems that's serve youth such as schools, youth centers and churches are important intervention approaches. Another point of intervention is to strengthen bonds to prosocial figures by providing more mentoring and legitimate after-school activities for youth in high violence communities in order to disrupt and reduce connections to risky peer networks. Another, opportunity for intervention is to target specific HIV prevention messages to youth networks (e.g. gangs) that endorse risky norms using peer educators. Such measures call for researchers to work outside of their traditional disciplinary divides in order to conduct more trans-disciplinary research.
Acknowledgments
This research was supported by funding from the National Institutes of Health, 1RO3 HD049283-01 awarded to Dexter Voisin
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dexter R. Voisin, Associate Professor at the School of Social Service Administration, University of Chicago, Chicago, Illinois
Esther J. Jenkins, Professor at Chicago State University, Department of Psychology, Chicago, Illinois
Lois Takahashi, Professor at University of California Los Angeles, School of Public Affairs, Department of Urban Planning
References
- 1.Hall HI, Song R, Rhodes P, et al. Estimation of HIV Incidence in the United States. JAMA. 2008;300:520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CDC. Youth Risk Behavior Surveillance — United States, 2009. MMWR Surveillance Summaries. 2010;59:6. [PubMed] [Google Scholar]
- 3.Krug E, Dahlberg L, Mercy J, Zwi A, Lozano R. World report on violence and health. Geneva: WHO; 2002. [Google Scholar]
- 4.CDC. Web-based Injury Statistics Query and Reporting System (WISQARS): National Center for Injury Prevention and Control, Office of Statistics and Programming. 2010. [Google Scholar]
- 5.Mc Cart M, Smith D, Saunders B, et al. Do urban adolescents become desensitized to community violence? Data from a national study. Am J Orthopsychiatry. 2007;77(3):434–442. doi: 10.1037/0002-9432.77.3.434. [DOI] [PubMed] [Google Scholar]
- 6.Margolin G, Gordis E. The effects of family and community violence on children. Annu Rev Psychol. 2000;51:445–479. doi: 10.1146/annurev.psych.51.1.445. [DOI] [PubMed] [Google Scholar]
- 7.WHO. World report on violence and health. Geneva: World Health Organization (WHO); 2002. [Google Scholar]
- 8.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (producer); 2010. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] Available from: www.cdc.gov/injury/wisqars/fatal.html. [Google Scholar]
- 9.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (producer); 2010. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] Available from: www.cdc.gov/injury/wisqars/fatal.html. [Google Scholar]
- 10.Jones D, Runyan D, Lewis T, Litrownik A, Black M, Wiley T, English D, Proctor L, Jones B, Nagin D. Trajectories of childhood sexual abuse and early adolescent HIV/AIDS risk behaviors: The role of other maltreatment, witnessed violence, and child gender'. J Clin Child Adolesc Psychol. 2010;39(5):667–680. doi: 10.1080/15374416.2010.501286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albus K, Weist M, Perez-Smith A. Associations between youth risk behavior and exposure to violence: implications for the provision of mental health services in urban schools. Behav Modif. 2004;28:548–563. doi: 10.1177/0145445503259512. [DOI] [PubMed] [Google Scholar]
- 12.Berenson A, Wiemann C, McCombs S. Exposure to violence and associated health-risk behaviors among adolescent girls. Arch Pediatr Adolesc Med. 2001;15:1238–1242. doi: 10.1001/archpedi.155.11.1238. [DOI] [PubMed] [Google Scholar]
- 13.Brady S. Lifetime community violence exposure and health risk behavior among young adults in college. J Adolesc Health. 2006;39:610–613. doi: 10.1016/j.jadohealth.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 14.Stiffman A, Dore P, Cunningham R, Earls F. Person and environment in HIV risk behavior change between adolescence and young adulthood. Health Educ Q. 1995;22(2):211–226. doi: 10.1177/109019819502200209. [DOI] [PubMed] [Google Scholar]
- 15.Voisin D. Victims of community violence and HIV sexual risk behaviors among African American adolescent males. J HIV/AIDS Prev Educ Adolesc Child. 2003;5(3/4):87–110. [Google Scholar]
- 16.Voisin D. The relationship between violence exposure and HIV sexual risk behaviors: Does gender matter? Am J Orthopsychiatry. 2005;75(4):497–506. doi: 10.1037/0002-9432.75.4.497. [DOI] [PubMed] [Google Scholar]
- 17.Voisin D, DiClemente R, Salazar L, Crosby R, Yarber W, Staples-Horne M. Community violence exposure and health-risk outcomes among detained adolescents. Am J Orthopsychiatry. 2007;74:506–513. doi: 10.1037/0002-9432.77.4.506. [DOI] [PubMed] [Google Scholar]
- 18.Farmer P. Pathologies of power: rethinking health and human rights. Am J Public Health. 1999;89:1486–96. doi: 10.2105/ajph.89.10.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DiClemente RJ, Salazar LF, Crosby R, Rosenthal S. Prevention and control of sexually transmitted infections among adolescents: The importance of a socio-ecological perspective, a commentary. Public Health. 2004;119(9):825–836. doi: 10.1016/j.puhe.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 20.Voisin D, Neilands T, Hunnicut S. Mechanisms linking violence exposures and school engagement among African American adolescents: Examining the roles of psychological problem behaviors and gender. Am J Orthopsychiatry. doi: 10.1111/j.1939-0025.2010.01072.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henrich CC, Schwab-Stone M, Fanti K, Jones SM, Ruchkin V. The association of community violence exposure with middle-school performance: A prospective study. Appl Dev Psychol. 2004;25:327–348. [Google Scholar]
- 22.Farver J, Natera L, Frosh D. Effects of community violence on inner-city preschoolers and their families. J Appl Dev Psychol. 1999;20:143–158. [Google Scholar]
- 23.Schwartz D, Gorman AH. Community violence exposure and children's school functioning. J Edu Psychol. 2003;95(1):163–173. [Google Scholar]
- 24.Voisin D, Neilands T. Low school engagement and sexual behaviors among African American youth: examining the influences of gender, peer norms, and gang involvement. Children and Youth Services Review. 2010;32(1):51–57. doi: 10.1016/j.childyouth.2009.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hirschi T. Causes of delinquency. Berkeley: University of California Press; 1969. [Google Scholar]
- 26.Kurtz PD, Gaudin JM, Wodarski JS, Howing PT. Maltreatment and the school-aged child: School performance consequences. Child Abuse and Neglect. 1993;51:445–479. doi: 10.1016/0145-2134(93)90080-o. [DOI] [PubMed] [Google Scholar]
- 27.Schwab-Stone M, Ayers T, Kasprow W, Voyce C, Barone C. No safe haven: A study of violence exposure in an urban community. J Am Acad Child Adolesc Psychiatry. 1995;10:1343–1252. doi: 10.1097/00004583-199510000-00020. [DOI] [PubMed] [Google Scholar]
- 28.Petraitis J, Flay B, Miller T. Reviewing theories of adolescent substance use: Organizing pieces in the puzzle. Psychol Bull. 1995;117:167–86. doi: 10.1037/0033-2909.117.1.67. [DOI] [PubMed] [Google Scholar]
- 29.Ng-Mak D, Salzinger S, Feldman R. Pathological adaptation to community violence among inner-city youth. Am J Orthopsychiatry. 2004;74:196–208. doi: 10.1037/0002-9432.74.2.196. [DOI] [PubMed] [Google Scholar]
- 30.DiClemente R, Wingood G, Crosby, et al. A prospective study of psychological distress and sexual risk behaviors among black adolescent females. Pediatrics. 2001;108(5):e5. doi: 10.1542/peds.108.5.e85. [DOI] [PubMed] [Google Scholar]
- 31.Bardy S, Donnenberg G. Mechanisms linking violence exposure and health risk behavior in adolescence: motivation to cope and sensation seeking. J Am Acad of Child Adolesc Psychiatry. 2006;45(6):673–680. doi: 10.1097/01.chi.0000215328.35928.a9. [DOI] [PubMed] [Google Scholar]
- 32.Breslau B, Davis G, Andreski P, Peterson E. Traumatic events and post-traumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry. 1991;74(7):252–261. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- 33.Nader K, Pynoos R, Fairbanks L, Frederick C. Children's PTSD reactions one year after a sniper attack at their school. Am J Psychiatry. 1990;147:1526–1530. doi: 10.1176/ajp.147.11.1526. [DOI] [PubMed] [Google Scholar]
- 34.Fitzpatrick K. Exposure to community violence and presence of depression among low income African American youth. J Consul Clin Psychol. 1993;61:528–531. doi: 10.1037//0022-006x.61.3.528. [DOI] [PubMed] [Google Scholar]
- 35.Gorman-Smith D, Tolan P. The role of exposure to community violence and developmental problems among inner-city youth. Dev Psychopathology. 1998;10:101–116. doi: 10.1017/s0954579498001539. [DOI] [PubMed] [Google Scholar]
- 36.Miller L, Wasserman G, Neugebauer R, Gorman-Smith D, Kamboukos D. Witnessed community violence and antisocial behavior in high-risk-urban boys. J Clin Child Psychol. 1999;28:2–11. doi: 10.1207/s15374424jccp2801_1. [DOI] [PubMed] [Google Scholar]
- 37.Bowen N, Bowen G. Effects of crime and violence in neighborhoods and schools on the school behaviors and performance of adolescents. J Adolesc Res. 1999:319–342. [Google Scholar]
- 38.Voisin D, Salazar L, Crosby R, Ralph D, Yarber W, Staples-Horne M. Teacher connectedness and health-related outcomes among detained adolescents. J Adolesc Health. 2005;37(4):337.e317–337.e323. doi: 10.1016/j.jadohealth.2004.11.137. [DOI] [PubMed] [Google Scholar]
- 39.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 40.McNeely C, Falci C. School connectedness and transition into and out of health risk behavior among adolescents: a comparison of social belonging and teacher support. J Sch Health. 2004;74(7):284–292. doi: 10.1111/j.1746-1561.2004.tb08285.x. [DOI] [PubMed] [Google Scholar]
- 41.Resnick MD, S BP, W BR, Bauman KE, Harris KM, Jones J. Protecting adolescents from harm: Findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278:443–478. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 42.Slonim-Nevo V, Auslander W, Ozawa N. Educational options and AIDS-related behaviors among troubled youth. J Pediatric Psychol. 1995;20(1):41–60. doi: 10.1093/jpepsy/20.1.41. [DOI] [PubMed] [Google Scholar]