Abstract
Objective:
To identify the cross-national prevalence of psychotic symptoms in the general population and to analyze their impact on health status.
Method:
The sample was composed of 256 445 subjects (55.9% women), from nationally representative samples of 52 countries worldwide participating in the World Health Organization's World Health Survey. Standardized and weighted prevalence of psychotic symptoms were calculated in addition to the impact on health status as assessed by functioning in multiple domains.
Results:
Overall prevalences for specific symptoms ranged from 4.80% (SE = 0.14) for delusions of control to 8.37% (SE = 0.20) for delusions of reference and persecution. Prevalence figures varied greatly across countries. All symptoms of psychosis produced a significant decline in health status after controlling for potential confounders. There was a clear change in health impact between subjects not reporting any symptom and those reporting at least one symptom (effect size of 0.55).
Conclusions:
The prevalence of the presence of at least one psychotic symptom has a wide range worldwide varying as much as from 0.8% to 31.4%. Psychotic symptoms signal a problem of potential public health concern, independent of the presence of a full diagnosis of psychosis, as they are common and are related to a significant decrement in health status. The presence of at least one psychotic symptom is related to a significant poorer health status, with a regular linear decrement in health depending on the number of symptoms.
Keywords: World Health Survey, extended phenotype, schizophrenia
Introduction
In the last few years, the traditional view of psychosis as a categorical entity (involving a qualitative change from normality to illness), an assumption of the main diagnostic systems such as the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) or the International Classification of Diseases, 10th edition (ICD-10),1 has been challenged for epidemiological, experimental, and theoretical reasons supporting the idea that psychotic symptoms may in fact be distributed along a continuum (eg, Johns and Van Os2; or for a recent systematic review of this topic, see van Os et al3).
This would imply that psychotic symptoms are present in the community population without diagnosable disorders, and these symptoms could potentially impact daily functioning even when the symptoms do not reach the clinical threshold for a disorder. Although different subtypes of schizophrenia have been proposed (eg, type I and II; positive, negative, or mixed4; deficit syndrome5), the different positive symptoms remain a central feature of the diagnosis.
The prevalence of psychotic symptoms in studies in community populations ranges from 4%6 to as much as 28.4%7 in the National Comorbidity Study, in which the clinically reappraised diagnosis of nonaffective psychotic disorder was only 0.7%. A replication using 6 psychosis screen items of the Composite International Diagnostic Interview (CIDI) found that 9.1% reported at least 1 symptom (with visual hallucinations being the most frequent: 6.3%). Likewise, the NEMESIS study in the Netherlands showed that 17.5% of subjects in the general population reported at least one psychotic symptom.8 The accumulated evidence indicates that these symptoms are distributed along a continuum, but the debate about dimensional and categorical representations of psychosis remains open and the most useful approach seems to be a combination of the 2.9
Thus, psychotic symptoms seem to be continuously distributed with their clinical relevance depending on several psychosocial factors that have been insufficiently studied (eg, the relationship to life events or belonging to an immigrant or minority group of the population).10 Most studies on the distribution and impact of psychotic symptoms have been conducted in a single country with comparisons of interregional national samples.3,11
Clear cross-national differences also exist in the frequency of specific psychotic symptoms. For example, in the International Pilot Study of Schizophrenia (IPSS12,13), which involved evaluation and follow-up of 1202 patients from 9 countries representing all regions of the world, there were no relevant differences in the prevalence of any type of psychosis but marked differences in the percentage of subjects reporting particular symptoms, eg, 9% of subjects reporting auditory hallucinations in Washington, DC, 28% in Agra (India), and 46% in Cali (Colombia); and 11% reporting delusions in Moscow vs 24% in Taipei. The IPSS employed trained clinical interviewers, but similar results have been found in studies using highly structured interviews such as the CIDI carried out by lay trained interviews as in our study detailed later. Thus, in the DOSMeD study,14 including 10 countries in all regions of the world, respondents from developed countries scored higher in affective symptoms while those from developing countries scored higher in visual hallucinations, with no differences in delusions. Likewise, in the EMPIRIC study in the general population of England, a relevant difference in specific symptoms was found according to ethnicity: 4.7% of Bangladeshi subjects in the sample reported at least 1 of 4 psychotic symptoms, whereas this was true of 9.9% of Pakistani and 12.1% of Black Caribbean subjects.15 There were no intergroup differences in the impact of symptoms on social functioning, and there was a linear increase in the impact with an increase in the number of symptoms from none to 3.
With regard to the distribution of psychotic symptoms in the general population, there are 2 issues that have not been sufficiently addressed in the past: (1) their impact on health status as assessed by capacities of functioning in multiple domains16 and (2) comparisons across countries of their distribution and impact.
The present study, using the World Health Organization World Health Survey (WHS) data, aimed to:
Identify the cross-national prevalence of psychotic symptoms assessed in the WHS.
Analyze the impact of psychotic symptoms on a composite measure of health and functioning.
Methods
Sample
Countries from the WHS were included in the analysis if the survey sample was nationally representative. Countries were drawn from all regions of the world and different levels of epidemiological and economic development, with 20 countries from the African region, 13 countries from the European region, 7 countries from the Americas region, and 12 countries from the Asian region, for a total of 52 countries. Fifteen countries were classified in the high or upper-mid economic levels according to the World Bank category,17 and 37 in the lower-mid or low level. All samples were drawn from a current national frame using a multistage cluster design so as to allow each household and individual respondent to be assigned a known nonzero probability of selection. The sampling guidelines and summary descriptions of the sampling procedures for each site are available from the WHS website (http://www.who.int/healthinfo/survey/en/index.html). For example, in 27 of the countries Global Positioning System devices were used to obtain the coordinates of the households drawn into the sample and mapped to national boundaries and population distributions to examine the representativeness of the sample. The individual global response rate was 98.5%. All data were weighted to account for sampling design in each country. Poststratification corrections were made to the weights to adjust for the population distribution obtained from the UN Statistical Division and for nonresponse.18 In order to make valid comparisons across countries, age and sex were standardized based on the WHO World Standard Population and data from the UN Statistical Division.19
Informed consent was obtained from all respondents, and the study was cleared by the ethical review committees at each site. The final sample was composed of 256 445 subjects.
All interviews were conducted by specially trained interviewers. A standard procedure for the training and quality control was implemented at all sites and supervised periodically as per a specified quality assurance protocol.20
Measures
All respondents were interviewed using the WHS instrument, an extensive interview about health status, that, among other things, collected data on sociodemographic characteristics, daily consumption of alcohol in the week before the interview, household economic status based on a list of indicators, questions about functioning, health status and quality of life, depressive symptoms, lifetime diagnosis of schizophrenia, lifetime and current treatment for schizophrenia, and psychotic symptoms during the last 12 months (see http://www.who.int/healthinfo/survey/en/index.html for the survey instrument).
Assessment of Psychotic Symptoms
Individual questions based on the CIDI version 3.021 were included to assess the presence of psychotic symptoms. The questions included assessed delusional mood (A feeling that something strange and unexplainable was going on that other people would find hard to believe?), delusions of reference and persecution (A feeling that people were too interested in you or there was a plot to harm you?), delusions of control (feeling that your thoughts were being directly interfered or controlled by another person, or your mind was being taken over by strange forces?), and hallucinations (An experience of seeing visions or hearing voices that others could not see or hear when you were not half asleep, dreaming or under the influence of alcohol or drugs?), over the past 12 months The response format was dichotomous (ie, “Yes” or “No”). The psychosis module of the CIDI has demonstrated high concordance with clinician ratings with a kappa agreement coefficient of .82 for DSM-IV diagnosis of schizophrenia and as high as .87 for hallucinations and .85 for delusions among the specific positive symptoms.22 Likewise, the CIDI psychosis module had adequate agreement with lifetime diagnosis of psychosis in other diagnostic interview, the Mini International Neuropsychiatric Interview for delusions (kappa = .82) and hallucinations (kappa = .72).23 Hanssen et al24 report that psychotic experiences reported in the CIDI were a good screening tool for subsequent confirmation of a diagnosis of psychosis by clinical interviewers using the Structured Clinical Interview for DSM-III-R25 in users of mental health services. The CIDI has also been extensively used in the WHO World Mental Health surveys in 28 countries and has been translated into a range of languages using a specified protocol. A point of note, however, is that the goal of our study was not to detect clinical psychosis among respondents, but specific psychotic symptoms present in the general population.
Health State and Health-Related Domains Measures
The measure of health state was based on 16 health-related questions that were grouped into 8 health domains, namely, vision, mobility, self-care, cognition, interpersonal activities, pain and discomfort, sleep and energy, and affect. Composition of this measure is explained elsewhere.26 A composite health status score was derived using a partial credit model.27 Using Winsteps,28 the rating scale model was fitted for the 16 health variables, and the raw scores were transformed through Rasch modeling into a continuous cardinal scale where a score of 0 represents worst health and a maximum score of 100 represents best health.
Statistical Analysis
Weighted and age–sex adjusted prevalence estimates were calculated for the 4 psychotic symptoms included in the survey. Likewise, the weighted and standardized estimates for the percentage of subjects reporting between 1, 2, 3 and 4 symptoms were calculated as well as the percentage of subjects reporting at least one symptom. Primary sampling units and poststratification weights accounting for age and gender differences were used. These analyses were separately performed for each country included in the study.
Thirteen percent of the sample data were missing in the main variables. Multiple imputation of missing values was performed using the ICE program29 implemented in the Stata software. This is based on a multivariate distribution, such that information from all other variables in the imputation model is used in imputing individual missing values.30 For all continuous variables, a predictive mean matching algorithm was used; for dichotomous variables, a logistic regression model was used. Five complete data files were imputed. Additionally, we checked the relationship between missingness of individual items after imputation with the percentage of people endorsing each symptom in overall sample and separately by country in order to confirm that the missing data for the main variables of the study were missing completely at random. The correlations in the overall sample were very low, suggesting lack of relation: 0.079 for delusions of mood, 0.049 for delusions of reference and persecution, 0.054 delusions of control, and 0.058 for hallucinations. The same patterns were found in each country separately (results not shown—available on request from the authors).
With the goal of analyzing the presence of a continuum in the impact on health and functioning as the number of psychotic symptoms increases, the whole sample was divided into 5 categories (0–4) as a simple addition of the number of psychotic symptoms in each subject. A linear regression analysis was performed with the composite health score generated from the Rasch model as the dependent variable. The number of psychotic symptoms was introduced as a dummy variable with the absence of symptoms as a reference. Age, gender, marital status, employment status, years of formal education, alcohol consumption, depression, and income status (quintile) were included in the equation in order to control for their effect as potential confounders. The presence of depression was established according to the responses to the CIDI items about depressive symptoms and their duration over the past 12 months according to the criteria specified in the International Classification of Diseases, 10th Edition.1,26
Finally, we tested for potential differences in the impact of psychotic symptoms among different domains of health and functioning. Each domain is composed by 2 items, and total scores were calculated through factor analyses using polychoric correlations and weighting individual items to obtain a factor score converted to individual domains scores ranging from 0 to 100 as in the case of the composite health score. Then several, regression analyses were performed with the total score for each domain as dependent variables and number of psychotic symptoms as the independent variable.
All analyses were done with the statistical package STATA, version 10.0.31
Results
Prevalence of Symptoms
In the final samples, 55.9% were women, the mean age was 45.0 years (SD = 11.9), and the mean number of years of formal education was 7.5 (SD = 0.1); 66.0% of the subjects were married, 19.6% single, and 8.9% widowed; 4.9% were unemployed (and looking for a job) (see table 1). Age- and gender-adjusted and weighted estimates for the presence of each psychotic symptom in each country are shown in table 1.
Table 1.
Weighted and Sex-Age Standardized Prevalence Estimates (SE) for Types of Psychotic Symptom in Each Country
| Country | N | Strange Things | People Too Interested | Thoughts Controlled | Hallucinations | Diagnosis |
| World Bank category: high/upper-mid | ||||||
| Croatia | 993 | 5.11 (0.98) | 4.46 (0.73) | 1.72 (0.45) | 1.73 (0.46) | 1.97 (0.50) |
| Czech Republic | 949 | 3.84 (0.71) | 5.57 (1.11) | 1.23 (0.36) | 0.58 (0.23) | 0.37 (0.18) |
| Estonia | 1021 | 7.88 (1.16) | 6.79 (0.99) | 2.69 (0.57) | 2.14 (0.45) | 1.50 (0.42) |
| Hungary | 1411 | 3.23 (0.56) | 3.72 (0.57) | 1.38 (0.43) | 1.13 (0.31) | 2.56 (0.54) |
| Latvia | 929 | 7.44 (1.11) | 7.07 (1.25) | 2.13 (0.67) | 3.45 (0.81) | 0.93 (0.50) |
| Malaysia | 6145 | 4.38 (0.28) | 3.42 (0.25) | 2.05 (0.19) | 2.80 (0.22) | 0.24 (0.06) |
| Mauritius | 3968 | 3.98 (0.54) | 6.34 (0.90) | 2.43 (0.43) | 2.28 (0.36) | 0.67 (0.16) |
| Mexico | 38 746 | 6.09 (0.30) | 4.69 (0.25) | 2.39 (0.16) | 3.54 (0.22) | 0.36 (0.04) |
| Russian Federation | 4427 | 4.23 (0.70) | 4.55 (0.63) | 1.34 (0.30) | 1.17 (0.41) | 0.41 (0.12) |
| Slovakia | 2535 | 4.15 (0.80) | 6.45 (1.09) | 0.48 (0.13) | 2.13 (0.71) | 0.25 (0.14) |
| Slovenia | 687 | 3.61 (0.81) | 7.98 (1.14) | 2.67 (0.69) | 0.87 (0.40) | 1.08 (0.45) |
| South Africa | 2629 | 9.51 (1.20) | 6.45 (0.87) | 5.98 (0.89) | 8.19 (1.28) | 1.21 (0.29) |
| Spain | 6373 | 2.50 (0.26) | 1.70 (0.21) | 0.64 (0.12) | 0.51 (0.11) | 0.49 (0.13) |
| United Arab Emirates | 1183 | 5.16 (0.92) | 4.01 (0.74) | 1.94 (0.58) | 3.47 (1.03) | 1.51 (0.66) |
| Uruguay | 2996 | 4.04 (1.04) | 2.90 (0.55) | 1.18 (0.28) | 1.17 (0.39) | 0.75 (0.11) |
| Total | 74 992 | 5.05 (0.23) | 4.86 (0.23) | 1.92 (0.13) | 2.39 (0.17) | 1.00 (0.10) |
| World Bank category: lower-mid/low | ||||||
| Bangladesh | 5942 | 3.97 (0.56) | 8.82 (0.89) | 3.57 (0.41) | 4.69 (0.57) | 0.78 (0.20) |
| Bosnia and Herzegovina | 1031 | 0.90 (0.29) | 1.04 (0.37) | 0.82 (0.30) | 0.49 (0.21) | 0.10 (0.06) |
| Brazil | 5000 | 16.13 (0.62) | 21.73 (0.76) | 9.98 (0.54) | 13.67 (0.61) | 1.67 (0.22) |
| Burkina Faso | 4948 | 17.05 (1.6) | 16.31 (1.7) | 8.77 (1.02) | 7.37 (0.98) | 1.30 (0.27) |
| Chad | 4875 | 11.36 (1.2) | 8.11 (1.03) | 10.48 (1.4) | 8.28 (1.17) | 3.15 (0.41) |
| China | 3994 | 4.22 (1.77) | 1.70 (0.57) | 0.65 (0.23) | 0.88 (0.25) | 0.27 (0.08) |
| Comoros | 1836 | 8.55 (0.92) | 5.96 (0.85) | 7.66 (0.92) | 5.19 (0.76) | 0.80 (0.28) |
| Congo | 3077 | 13.72 (1.7) | 12.27 (1.9) | 10.06 (1.7) | 6.96 (1.53) | 3.91 (1.10) |
| Cote d'Ivoire | 3251 | 12.42 (1.1) | 13.99 (1.1) | 8.56 (0.86) | 7.72 (0.84) | 1.17 (0.29) |
| Dominican Republic | 5027 | 11.82 (0.48) | 10.82 (0.46) | 6.85 (0.38) | 11.82 (0.48) | 1.23 (0.16) |
| Ecuador | 5677 | 5.90 (0.72) | 4.78 (0.66) | 2.98 (0.42) | 3.76 (0.45) | 0.94 (0.21) |
| Ethiopia | 5090 | 5.90 (0.54) | 11.46 (0.90) | 6.35 (0.56) | 4.75 (0.43) | 1.45 (0.22) |
| Georgia | 2950 | 1.55 (0.35) | 0.88 (0.22) | 0.52 (0.13) | 0.63 (0.19) | 0.51 (0.17) |
| Ghana | 4165 | 2.17 (0.28) | 2.96 (0.35) | 2.01 (0.28) | 2.69 (0.32) | 0.64 (0.14) |
| Guatemala | 4890 | 9.61 (0.45) | 8.45 (0.42) | 5.43 (0.35) | 7.41 (0.40) | 0.38 (0.09) |
| India | 10 692 | 13.54 (0.77) | 14.46 (0.80) | 11.28 (0.71) | 12.29 (0.77) | 2.51 (0.30) |
| Kazakhstan | 4499 | 1.73 (0.30) | 2.05 (0.52) | 0.52 (0.15) | 0.48 (0.15) | 0.45 (0.13) |
| Kenya | 4640 | 10.52 (0.87) | 8.45 (0.72) | 8.45 (1.05) | 11.01 (1.1) | 0.73 (0.21) |
| Lao People's Democratic Republic | 4989 | 4.49 (0.41) | 1.05 (0.17) | 1.01 (0.17) | 1.66 (0.23) | 0.32 (0.09) |
| Malawi | 5551 | 2.99 (0.41) | 3.53 (0.48) | 2.77 (0.47) | 3.24 (0.40) | 1.24 (0.24) |
| Mali | 5209 | 10.89 (0.85) | 9.27 (0.74) | 8.36 (0.72) | 6.95 (0.62) | 2.25 (0.42) |
| Mauritania | 3907 | 7.41 (0.91) | 5.85 (0.85) | 4.45 (0.72) | 5.01 (0.82) | 2.72 (0.54) |
| Morocco | 5000 | 7.73 (0.67) | 11.87 (1.1) | 6.93 (0.67) | 7.87 (0.77) | 0.66 (0.22) |
| Myanmar | 6045 | 1.48 (0.39) | 1.16 (0.33) | 0.87 (0.27) | 1.47 (0.44) | 0.33 (0.12) |
| Namibia | 4379 | 6.76 (0.67) | 5.75 (0.59) | 4.31 (0.53) | 5.51 (0.59) | 2.99 (0.48) |
| Nepal | 8822 | 17.70 (0.72) | 22.71 (0.71) | 14.1 (0.49) | 32.03 (0.93) | 2.54 (0.31) |
| Pakistan | 6502 | 0.80 (0.13) | 1.18 (0.24) | 0.82 (0.15) | 0.92 (0.18) | 1.12 (0.19) |
| Paraguay | 5288 | 4.61 (0.34) | 5.62 (0.42) | 2.26 (0.24) | 3.01 (0.28) | 0.46 (0.10) |
| Philippines | 10 083 | 6.22 (0.59) | 3.75 (0.39) | 1.79 (0.22) | 2.64 (0.28) | 0.43 (0.08) |
| Senegal | 3465 | 13.24 (1.2) | 10.98 (1.0) | 8.90 (0.95) | 8.13 (0.88) | 1.48 (0.35) |
| Sri Lanka | 6805 | 1.54 (0.26) | 1.26 (0.25) | 0.83 (0.25) | 0.72 (0.18) | 0.65 (0.16) |
| Swaziland | 3121 | 10.90 (1.1) | 9.96 (0.89) | 8.68 (1.00) | 10.18 (1.1) | 5.70 (0.73) |
| Tunisia | 5203 | 7.98 (0.75) | 11.19 (0.99) | 5.74 (0.56) | 6.02 (0.62) | 1.84 (0.25) |
| Ukraine | 2860 | 4.41 (0.59) | 5.20 (0.85) | 1.17 (0.26) | 0.86 (0.19) | 0.60 (0.15) |
| Vietnam | 4174 | 0.37 (0.11) | 0.40 (0.13) | 0.20 (0.07) | 0.21 (0.10) | 0.07 (0.04) |
| Zambia | 4166 | 7.78 (0.48) | 7.19 (0.47) | 6.18 (0.43) | 3.05 (0.35) | 0.72 (0.15) |
| Zimbabwe | 4292 | 4.62 (0.60) | 5.51 (0.67) | 3.95 (0.53) | 3.08 (0.40) | 1.07 (0.23) |
| Total mid low/low | 181 445 | 7.04 (0.14) | 7.25 (0.14) | 4.91 (0.12) | 5.49 (0.11) | 1.38 (0.06) |
| Total sample | 256 437 | 6.49 (0.12) | 6.59 (0.12) | 4.09 (0.09) | 4.64 (0.09) | 1.11 (0.05) |
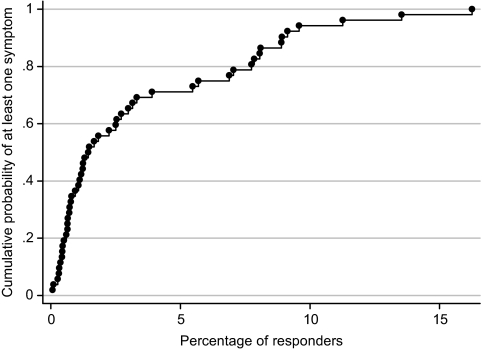
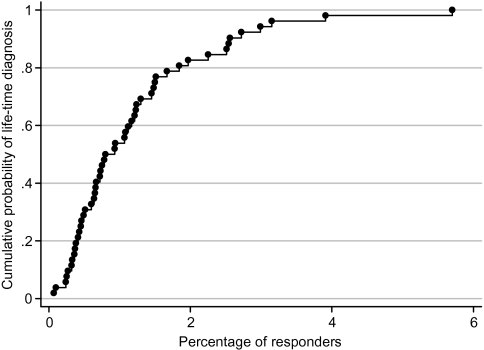
The overall prevalence was 7.08% (SE = 0.17) for delusional mood, 8.37 (SE = 0.20) for delusions of reference and persecution, 4.80% (SE = 0.14) for delusions of control, and 5.81% (SE = 0.16) for hallucinations. Prevalence figures varied highly across countries (eg, from 0.8% in Vietnam to 31.4% in Nepal in estimates for hallucinations). A 12.52% of the total sample responded positively to at least one symptom. The percentage of subjects reporting a previous lifetime diagnosis of schizophrenia was 1.04% (95% CI: 1.00–1.08). This percentage also varied across countries although in not as wide a range as found in specific symptoms, from 0.07% in Vietnam to 5.70% in Swaziland. Figures 1 and 2 show the cumulative distribution by country of percentage of people reporting, respectively, at least one symptom and lifetime diagnosis. For at least one symptom, the median was 1.47% (95% CI: 0.99–2.88) and the interquartile range (IQR) was 0.66%–6.30%. For lifetime diagnosis, the median was 0.87% (95% CI: 0.65–1.22) and the IQR was 0.46%–1.51%. Respondents with a previous diagnosis had significantly (t(240337) = 74.6, P < .001; g = 1.51) higher mean number of symptoms (mean = 1.24, SD = 1.46) than those without a diagnosis (mean = 0.21; SD = 0.67). Among the subjects without a previous diagnosis of schizophrenia, 88.6% did not report any symptom in the 12 months before the interview, 5.8% reported one symptom, 2.9% 2 symptoms, 1.7% 3 symptoms, and 1.1% 4 symptoms. In subjects with a diagnosis, 47.5% reported no symptoms, 17.4% one symptom, 11.0% 2 symptoms, 11.5% 3 symptoms, and 12.6% 4 symptoms in the 12 months before the interview.
Fig. 1.
Cumulative Distribution of Persons Reporting At Least One Psychotic Symptom, by Country.
Fig. 2.
Cumulative Distribution of Lifetime Diagnosis of Schizophrenia, by Country.
Number of Psychotic Symptoms
The estimates by country of the percentage of subjects reporting between 1 and 4 symptoms or at least 1 symptom are shown in table 2. Descriptive data and comparisons across groups of number of symptoms are presented in table 3. All comparisons were significant with P < .001, but the effect sizes in general indicate nonmeaningful differences. Thus, the Cramer's V coefficient of association between ordinal (number of symptoms) and the different categorical variables, which ranges from 0 (no association) to 1 (perfect association), had a highest value of 0.047. Likewise, effect size (Hedge's g) for quantitative variables indicated very low values for differences in age (maximum g of 0.012) or alcohol unit consumption per day (maximum g of 0.07). There was a relevant effect, however, for years of formal education with a clear linear trend to a higher number of symptoms related to less education (maximum effect size, between 0 and 4 symptoms, of −0.56).
Table 2.
Weighted and Sex-Age Standardized Prevalence Estimates (SE) for Number of Psychotic Symptom in Each Country
| Country |
Number of symptoms |
||||
| 1 | 2 | 3 | 4 | At Least 1 | |
| World Bank category: high/upper-mid | |||||
| Croatia | 5.06 (0.94) | 1.54 (0.42) | 1.21 (0.41) | 0.30 (0.17) | 8.10 (1.12) |
| Czech Republic | 6.96 (1.19) | 1.67 (0.41) | 0.27 (0.13) | 0 (—) | 8.90 (1.29) |
| Estonia | 6.89 (1.05) | 2.48 (0.48) | 1.27 (0.43) | 0.61 (0.26) | 11.26 (1.45) |
| Hungary | 5.22 (0.63) | 1.32 (0.36) | 0.37 (0.20) | 0.14 (0.09) | 7.05 (0.75) |
| Latvia | 9.13 (1.24) | 3.30 (0.78) | 0.63 (0.30) | 0.48 (0.34) | 13.54 (1.62) |
| Malaysia | 4.73 (0.29) | 1.87 (0.18) | 0.82 (0.12) | 0.43 (0.09) | 7.85 (0.36) |
| Mauritius | 4.01 (0.59) | 1.48 (0.26) | 1.55 (0.30) | 0.70 (0.17) | 7.74 (1.01) |
| Mexico | 4.40 (0.21) | 2.31 (0.17) | 1.14 (0.10) | 1.06 (0.11) | 8.92 (0.36) |
| Russian Federation | 4.18 (0.59) | 1.67 (0.27) | 0.66 (0.38) | 0.39 (0.18) | 6.89 (0.80) |
| Slovakia | 5.94 (0.94) | 2.88 (0.88) | 0.25 (0.11) | 0.06 (0.04) | 9.13 (1.28) |
| Slovenia | 5.50 (0.95) | 3.00 (0.71) | 0.70 (0.36) | 0.38 (0.28) | 9.58 (1.24) |
| South Africa | 7.94 (0.85) | 3.91 (0.62) | 3.16 (0.62) | 1.24 (0.45) | 16.25 (1.70) |
| Spain | 2.17 (0.24) | 0.72 (0.13) | 0.22 (0.07) | 0.21 (0.06) | 3.32 (0.30) |
| United Arab Emirates | 4.39 (0.73) | 1.61 (0.58) | 1.39 (0.56) | 0.67 (0.33) | 8.06 (1.16) |
| Uruguay | 3.49 (0.66) | 1.29 (0.39) | 0.67 (0.21) | 0.29 (0.08) | 5.47 (1.28) |
| Total high/med-high | 5.37 (0.23) | 2.01 (0.14) | 0.98 (0.10) | 0.47 (0.06) | 8.83 (0.32) |
| World Bank category: lower-mid/low | |||||
| Bangladesh | 8.51 (0.85) | 3.07 (0.39) | 1.28 (0.18) | 0.64 (0.17) | 13.49 (1.21) |
| Bosnia and Herzegovina | 0.77 (0.30) | 0.38 (0.17) | 0.01 (0.01) | 0.38 (0.20) | 1.54 (0.42) |
| Brazil | 14.69 (0.61) | 8.69 (0.43) | 5.66 (0.41) | 2.92 (0.28) | 31.96 (0.90) |
| Burkina Faso | 9.33 (0.87) | 7.03 (0.85) | 3.83 (0.60) | 3.36 (0.61) | 23.55 (1.83) |
| Chad | 7.11 (0.74) | 4.97 (0.73) | 1.88 (0.35) | 3.85 (0.85) | 17.82 (1.70) |
| China | 3.30 (1.37) | 1.09 (0.51) | 0.24 (0.10) | 0.11 (0.06) | 4.74 (1.87) |
| Comoros | 8.84 (1.21) | 4.32 (0.70) | 1.87 (0.36) | 0.98 (0.26) | 16.01 (1.63) |
| Congo | 6.09 (0.96) | 3.67 (0.59) | 2.60 (0.67) | 4.91 (1.30) | 17.27 (1.80) |
| Cote d'Ivoire | 9.37 (0.80) | 6.95 (0.80) | 3.38 (0.45) | 1.99 (0.44) | 21.69 (1.46) |
| Dominican Republic | 9.96 (0.45) | 4.21 (0.32) | 3.52 (0.28) | 2.74 (0.24) | 21.13 (0.61) |
| Ecuador | 4.63 (0.51) | 2.61 (0.45) | 1.16 (0.23) | 1.05 (0.21) | 9.45 (0.96) |
| Ethiopia | 10.49 (0.68) | 4.70 (0.48) | 1.70 (0.28) | 0.65 (0.24) | 17.54 (0.84) |
| Georgia | 1.16 (0.32) | 0.40 (0.11) | 0.23 (0.09) | 0.23 (0.08) | 2.01 (0.43) |
| Ghana | 2.44 (0.33) | 1.06 (0.20) | 0.93 (0.18) | 0.60 (0.14) | 5.03 (0.46) |
| Guatemala | 6.58 (0.38) | 3.20 (0.27) | 2.78 (0.25) | 2.39 (0.24) | 14.95 (0.54) |
| India | 11.71 (0.66) | 6.46 (0.44) | 4.85 (0.44) | 3.05 (0.40) | 26.08 (1.15) |
| Kazakhstan | 1.91 (0.46) | 0.49 (0.14) | 0.16 (0.08) | 0.24 (0.11) | 2.80 (0.60) |
| Kenya | 8.03 (0.84) | 4.20 (0.64) | 3.86 (0.88) | 2.64 (0.39) | 18.73 (1.32) |
| Lao People's Democratic Republic | 3.97 (0.40) | 1.30 (0.18) | 0.34 (0.09) | 0.03 (0.03) | 5.65 (0.49) |
| Malawi | 2.07 (0.33) | 1.44 (0.27) | 1.04 (0.23) | 1.11 (0.26) | 5.66 (0.67) |
| Mali | 4.55 (0.57) | 3.31 (0.38) | 3.44 (0.45) | 3.15 (0.42) | 14.46 (0.93) |
| Mauritania | 5.38 (0.80) | 2.82 (0.55) | 1.44 (0.29) | 1.59 (0.36) | 11.23 (1.29) |
| Morocco | 8.04 (0.71) | 5.38 (0.69) | 2.67 (0.39) | 1.81 (0.36) | 17.90 (1.28) |
| Myanmar | 1.49 (0.32) | 0.71 (0.22) | 0.37 (0.11) | 0.23 (0.11) | 2.80 (0.69) |
| Namibia | 6.06 (0.59) | 2.70 (0.38) | 1.85 (0.36) | 1.30 (0.30) | 11.91 (0.91) |
| Nepal | 22.77 (0.67) | 11.26 (0.49) | 6.82 (0.35) | 4.98 (0.35) | 45.84 (0.95) |
| Pakistan | 1.38 (0.25) | 0.31 (0.08) | 0.20 (0.07) | 0.25 (0.06) | 2.14 (0.33) |
| Paraguay | 4.95 (0.38) | 2.39 (0.24) | 1.29 (0.18) | 0.44 (0.10) | 9.07 (0.52) |
| Philippines | 5.71 (0.56) | 2.18 (0.25) | 0.86 (0.12) | 0.41 (0.08) | 9.15 (0.77) |
| Senegal | 6.54 (0.66) | 5.36 (0.75) | 3.47 (0.50) | 3.31 (0.51) | 18.68 (1.46) |
| Sri Lanka | 1.34 (0.26) | 0.73 (0.16) | 0.26 (0.08) | 0.10 (0.04) | 2.43 (0.42) |
| Swaziland | 8.67 (0.92) | 5.28 (0.71) | 2.64 (0.53) | 2.92 (0.52) | 19.50 (1.49) |
| Tunisia | 6.38 (0.66) | 4.39 (0.47) | 2.82 (0.34) | 1.70 (0.25) | 15.30 (1.24) |
| Ukraine | 4.29 (0.65) | 1.72 (0.42) | 0.73 (0.20) | 0.19 (0.09) | 6.93 (0.94) |
| Vietnam | 0.37 (0.17) | 0.16 (0.06) | 0.09 (0.05) | 0.03 (0.02) | 0.66 (0.20) |
| Zambia | 4.23 (0.39) | 2.50 (0.29) | 4.35 (0.37) | 0.48 (0.11) | 11.56 (0.59) |
| Zimbabwe | 4.74 (0.67) | 2.58 (0.38) | 1.00 (0.21) | 1.08 (0.27) | 9.40 (0.96) |
| Total low-mid/low | 6.09 (0.12) | 3.36 (0.08) | 1.91 (0.06) | 1.54 (0.07) | 12.90 (0.19) |
| Total all sample | 5.89 (0.11) | 2.99 (0.07) | 1.65 (0.05) | 1.24 (0.05) | 11.78 (0.16) |
Table 3.
Descriptive Data for Subjects according to the Number of Psychotic Symptoms
| Predictors |
Number of psychotic symptoms |
|||||
| 0 | 1 | 2 | 3 | 4 | g or Va | |
| Gender (% of women) | 55.1 | 57.9 | 57.4 | 59.7 | 59.9 | 0.022 |
| Age in years (mean [SD]) | 40.7 (16.5) | 40.2 (16.3) | 39.8 (16.2) | 39.7 (15.8) | 41.7 (16.7) | 0.012 |
| Marital status (%) | 0.022 | |||||
| Married | 61.8 | 60.6 | 58.4 | 58.3 | 56.9 | |
| Never married | 19.5 | 18.6 | 18.9 | 16.8 | 16.6 | |
| Separated | 2.3 | 2.9 | 3.2 | 4.0 | 4.4 | |
| Divorced | 2.7 | 2.7 | 3.0 | 2.7 | 2.8 | |
| Widowed | 8.8 | 9.2 | 9.9 | 10.2 | 11.5 | |
| Cohabiting | 4.8 | 6.0 | 6.5 | 8.0 | 7.9 | |
| Years of formal education | 7.2 (5.2) | 6.3 (5.2) | 5.9 (5.1) | 5.3 (4.9) | 4.3 (4.6) | 0.56 |
| Income quintiles | 0.042 | |||||
| Lowest quintile | 24.5 | 27.5 | 28.0 | 33.1 | 33.6 | |
| 2nd quintile | 24.9 | 29.0 | 31.2 | 30.7 | 36.0 | |
| 3rd quintile | 23.1 | 21.4 | 21.7 | 21.2 | 19.2 | |
| 4th quintile | 18.3 | 15.3 | 14.2 | 11.3 | 9.2 | |
| Highest quintile | 9.2 | 6.8 | 4.9 | 3.7 | 2.1 | |
| Employment (% unemployed) | 5.5 | 5.9 | 7.4 | 6.9 | 7.0 | 0.019 |
| Alcohol units per day | 0.22 (1.0) | 0.27 (1.3) | 0.31 (1.3) | 0.27 (1.2) | 0.30 (1.2) | 0.07 |
| Depression (%) | 7.2 | 8.6 | 9.1 | 9.2 | 10.0 | 0.023 |
Note: All contrasts were significant with P < .001.
g, highest Hedge's g effect size for paired post hoc comparisons; V, Cramer's V.
Difference in Health Status according to Number of Symptoms
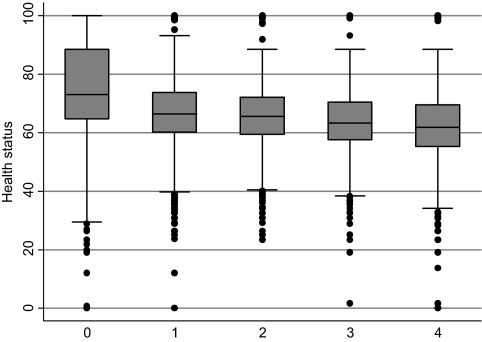
There were significant differences between the number of symptoms with regard to their impact on health. Post hoc comparisons indicate a progressive decrease in health status (P < .001 in all cases) with the increase in number of symptoms. The mean health score for subjects not reporting any psychotic symptoms was 76.2 (SD = 15.0), 68.5 (SD = 12.7) for subjects reporting one symptom, 66.8 (SD = 11.9) for the 2 symptom group, 64.8 (SD = 11.6) for the 3 symptom group, and 63.0 (SD = 12.5) for subjects reporting 4 symptoms. Hedge's g effect size was moderate to high in comparisons of subjects without symptoms vs subjects with one or more symptom. Thus, when compared with subjects with one symptom, g was 0.55, with subjects with 2 symptoms it was 0.69, 0.85 with subjects with 3 symptoms, and 0.96 with subjects with 4 symptoms. Comparisons between subjects reporting one symptom or more indicated a pattern of a regular linear decrease in health with a higher number of symptoms but with more moderate effect sizes for differences: 1 vs 4, g = 0.44; 1 vs 3, g = 0.30; 1 vs 2, g = 0.14; 2 vs 3, g = 0.17; 2 vs 4, g = 0.31; 3 vs 4, g = 0.15. All effect sizes were significant and had 95% CIs excluding zero, as expected given the large sample sizes. The gradient on impact with the increase of symptoms is graphically represented at figure 3.
Fig. 3.
Box-plot of Mean Health Status Scores according to the Number of Psychotic Symptoms.
Impact on Health
The regression analysis on the impact of the number of symptoms, controlling for confounders, clearly pointed to a gap between the absence of symptoms and the presence of at least one symptom and then a linear increase in the impact on health as the number of symptoms increased. The mean Variance Inflation Factor = 4.27 suggests that multicollinearity is not a substantive problem in the data, allowing for meaningful interpretation of the results. Results of the regression analysis are shown in table 4. The adjusted R2 was .26. The results indicate that women report worse health status than men. Increased age is associated with decreasing health status, as is being in lower income quintiles and having less education. An unmarried status is associated with better health compared with being divorced or widowed and with worse health compared with being married. Alcohol consumption is also significantly related to poorer health status, although the size of the coefficient (−0.01) suggests that this is not a relevant effect. A diagnosis of major depression is also related to poorer health status. Potential effects due to differential distribution of symptoms across countries were controlled for introducing dummy variables for nationality in the regression analysis. Despite that, we performed regressions separately for each country in order to check that the main effect of interest (the continuum on the impact according to the number of symptoms) was demonstrated in every country. Mostly, those analyses did confirm that idea, particularly for the step between zero and one symptom. All analyses were also performed without the inclusion of outlier countries with regard to the prevalence of symptoms (Nepal at the high end and Vietnam at the low end). These analyses showed very similar results (details not shown; available upon request from the authors).
Table 4.
Final Equation for the Linear Regression Analysis: Impact of Number of Psychotic Symptoms Over Health Status, Controlling for Demographics
| Independent Variables | Coefficient (SE) | P | 95% CI |
| Gender (reference = men) | −3.77 (0.02) | <.001 | −3.82 to −3.73 |
| Age in years | −0.32 (0.00) | <.001 | −0.32 to −0.31 |
| Marital status (reference category = married) | |||
| Never married | −0.23 (0.03) | <.001 | −0.30 to −0.17 |
| Separated | −0.99 (0.07) | <.001 | −1.13 to −0.84 |
| Divorced | −0.35 (0.07) | <.001 | −0.49 to −0.21 |
| Widowed | −1.75 (0.04) | <.001 | −1.83 to −1.66 |
| Cohabiting | −0.04 (0.06) | .535 | −0.15 to 0.08 |
| Years of formal education | 0.14 (0.00) | <.001 | 0.13 to 0.14 |
| Income quintiles (reference category = highest) | |||
| 1st quintile | −3.42 (0.07) | <.001 | −3.55 to −3.29 |
| 2nd quintile | −2.69 (0.06) | <.001 | −2.81 to −2.57 |
| 3rd quintile | −1.91 (0.06) | <.001 | −2.02 to −1.81 |
| 4th quintile | −1.04 (0.05) | <.001 | −1.14 to −0.94 |
| Employment (reference = employed) | −0.30 (0.05) | <.001 | −0.40 to −0.20 |
| Alcohol consumption | −0.01 (0.00) | .001 | −0.01 to −0.002 |
| Number of psychotic symptoms (reference = no symptoms) | |||
| One symptom | −6.88 (0.05) | <.001 | −6.97 to −6.79 |
| Two symptoms | −8.68 (0.06) | <.001 | −8.81 to −8.55 |
| Three symptoms | −10.59 (0.08) | <.001 | −10.75 to −10.43 |
| Four symptoms | −11.78 (0.10) | <.001 | −11.97 to −11.59 |
| Depression (reference = not depression) | −1.11 (0.04) | <.001 | −1.20 to −1.03 |
| Country (67 dummy variables, results not reported) | — | — | — |
| Constant | 90.94 (0.17) | <.001 | 90.6–91.3 |
In the analyses reported above, the diagnosis of depressive episode was included as a potential confounder as an independent variable. In order to test if the self-reported psychotic symptoms reflect general severity of psychopathology, depression and the number of psychotic symptoms were included as independent variables in a linear regression analysis with health status as the dependent variable. The regression coefficient for the number of symptoms (4.12; SE = 0.02) was almost equal to and not significantly different from that for depression diagnosis (4.03; SE = 0.05).
Impact on Specific Domains of Health and Functioning
The results of the regression analyses comparing individual domains of functioning show that all the regression coefficients were significant, with clear differences between different domains. In order of size, the regression coefficients were 7.85 (SE = 0.07) for mood state, 6.01 (0.06) for sleep and energy, 5.90 (0.07) for pain and discomfort, 5.24 (0.06) for cognition, 4.21 (0.07) for mobility, 3.61 (0.05) for social activities, 2.21 (0.05) for self-care, and 2.13 (0.06) for vision.
Discussion
The results show that, in this large cross-national sample, prevalence rates of psychotic symptoms are in general smaller than those previously reported in the literature for the United States32 and for Europe8,15,33, but there is a very wide range in the prevalence, with several countries with an extremely high percentage of subjects reporting at least one symptom (eg, 45.8% in Nepal). Most previous studies, however, have not compared different countries, and, when that has been done, marked differences have been found in specific symptoms but not as widely in the prevalence of disorders.13,34 In a recent meta-analysis, differences in prevalence rates were found between 46 countries according to the economic level, in the opposite direction found here: higher rates in developed countries.35 Also, when comparing ethnic groups within the same area, clear differences in specific symptoms can be observed.15 Here, we have also found differences between countries in the lifetime prevalence of schizophrenia, but the range is clearly smaller than for specific symptoms. Differences between countries, perhaps due to cultural differences, may be a potential cause for concern regarding the robustness of the results. However, those differences are in the proportion of subjects reporting the symptoms, and, in the linear regression, dummies for countries were introduced to control for this potential bias. Furthermore, we found that the impact of symptoms remained the same in separate analyses for each country. Moreover, we also performed the analyses removing the outlier countries, and the results remained essentially the same. Thus, it seems that the variations in the reporting rates across countries do not detract from the relationship between the presence of psychotic symptoms and decreases in functioning.
The results of this study indicate that psychotic symptoms are clearly related with worse functioning even among those who do not meet the diagnostic criteria for a disorder. The relationship is continuous with a significant change in the impact between the absence of symptoms and the presence of at least one symptom. That is, the impact adopts the form of a linear relationship when at least one symptom is present: the more symptoms present, the more the impact on health. There is a clear separation in impact in the threshold between subjects without symptoms and all groups of subjects with symptoms. Subsequently, a linear and small progressive decrease in health status occurs as the number of symptoms increases. This effect is present even when controlling for a lifetime diagnosis of schizophrenia, current treatment of schizophrenia symptoms, presence of comorbid depression, alcohol consumption, socioeconomic status, and other potential confounders.
The results suggest a similar impact of the different psychotic symptoms. These results seem to provide support to the idea of a continuum in psychotic symptoms when at least one symptom is present, with a clear discontinuity from no symptoms to at least one symptom and then a small increase in the impact on health as the number of symptoms increases. Our results point to 2 categorical groups in the general population, one without symptoms and the other with a continuous distribution of psychotic symptoms. Nevertheless, in the current discussion regarding the developments of DSM-V and ICD-11, different authors have warned about the risks of taking dimensional approaches or extending excessively the number of diagnostic categories.36,37 The finding of the marked effect on health status of reporting even one psychotic symptom seems to point out to a categorical change, but that by itself does not imply the threshold of a natural category. Given that not all persons who report a psychotic symptom have a diagnosis of a psychotic disorder, while they are accompanied by significant decrements in health, the identification of such psychotic symptoms should signal the need for further assessment. This would be particularly true in clinical settings and could lead to an exploration of the need for early intervention in a high-risk population.
It is also interesting to see that, in several countries, the prevalence of, for instance, hallucinations (in the last 12 months) is lower than the expected prevalence of schizophrenia (lifetime) for those countries. This probably reflects that since only noninstitutionalized subjects were included in the sample, the more extreme symptom presentations are excluded. In any case, the high percentage of subjects with a self-reported lifetime diagnosis of schizophrenia who report at least one symptom and the clear difference in the number of symptoms reported for subjects with and without a previous diagnosis indirectly support the validity of the symptoms reported.
Limitations of our study include the lack of data on potential determinants of severity or disability associated with psychotic symptoms, such as the number and frequency of episodes, episode length, age at onset, and episode severity as defined by more extensive ratings of individual additional symptoms. Longitudinal studies are needed in order to analyze the natural history of these syndromes in the general population. The cross-sectional nature of the study also does not allow an inference with regard to the causal link between psychotic symptoms and health status to be addressed. Particularly, the main limitation of this work is in the lack of measurement of negative and cognitive symptoms that may better predict course and outcome in psychotic disorders.38 Besides, the study did not collect information about substance use such as cannabis, which could be a relevant mediator of the relationship between psychotic symptoms and health status. Likewise, there are other factors such as stress or trauma that could be related with psychotic symptoms and poor functioning and were not included in the survey.
As commented above, this study has implications for current approaches to the classification of psychotic disorders. In the context of the debate on the feasibility of addressing dimensions in addition to categorical diagnosis in the review of the current diagnostic systems, this study suggests that, within the dimension of reality distortion or positive symptoms, the more symptoms the subject has, the worse functioning and health. That provides support for the whole set of symptoms for that dimension in order to better characterize the outcome. It also indicates that minimal presentations of psychotic symptoms, although strongly varying across countries, have potential clinical relevance everywhere, and it could be important to detect subjects with these symptoms early, with the goal of further thorough screening of those at higher risk, bearing in mind the danger of stigmatization this could involve and the potential negative effects of treatments in persons with minor presentations of symptoms.39 Within the framework of the current debate about the inclusion of a psychosis risk syndrome in the DSM-V,40–43 it is not clear if the presence of one symptom is indicative or not of an incipient clinical disorder, but it does signal the need for a more detailed evaluation.
Funding
Instituto de Salud Carlos III; Centro de Investigación Biomédica en Red de Salud Mental; CIBERSAM Spain (www.cibersam.es); World Health Organization.
Acknowledgments
The views expressed in this paper are those of the authors and do not necessarily represent the views or policies of the World Health Organization. The sponsors played no role in study design or conduct of the study, the collection, management, analysis, or interpretation of data, the preparation, review, and approval of the manuscript, or the decision to submit the manuscript for publication. The Authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1.World Health Organization. Geneva, Switzerland: World Health Organization; 1993. The International Classification of Diseases (10th edition, ICD-10) [Google Scholar]
- 2.Johns LC, Van Os J. The continuity of psychotic experiences in the general population. Clin Psychol Rev. 2001;21:1125–1141. doi: 10.1016/s0272-7358(01)00103-9. [DOI] [PubMed] [Google Scholar]
- 3.Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179–195. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- 4.Andreasen NC, Olsen S. Negative vs. positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39:789–794. doi: 10.1001/archpsyc.1982.04290070025006. [DOI] [PubMed] [Google Scholar]
- 5.Carpenter WT, Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145:578–583. doi: 10.1176/ajp.145.5.578. [DOI] [PubMed] [Google Scholar]
- 6.Eaton WW, Romanoski A, Anthony JC, Nestadt G. Screening for psychosis in the general population with a self-report interview. J Nerv Ment Dis. 1991;179:689–693. doi: 10.1097/00005053-199111000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:1022–1031. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- 8.Van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: a psychosis continuum in the general population? Schizophr Res. 2000;45(1–2):11–20. doi: 10.1016/s0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- 9.Allardyce J, Gaebel W, Zielasek J, Van OJ. Deconstructing psychosis conference February 2006: the validity of schizophrenia and alternative approaches to the classification of psychosis. Schizophr Bull. 2007;33:863–867. doi: 10.1093/schbul/sbm051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim C, Chong SA, Keefe RS. Psychosocial factors in the neurobiology of schizophrenia: a selective review. Ann Acad Med Singap. 2009;38:402–406. [PubMed] [Google Scholar]
- 11.Perala J, Suvisaari J, Saarni SI, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007;64(1):19–28. doi: 10.1001/archpsyc.64.1.19. [DOI] [PubMed] [Google Scholar]
- 12.Sartorius N, Shapiro R, Kimura M, Barrett K. WHO international pilot study of schizophrenia. Psychol Med. 1972;2:422–425. doi: 10.1017/s0033291700045244. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Report of the International Pilot Study of Schizophrenia. Geneva, Switzerland: World Health Organization; 1973. Report No. WHO Offset publication No 2. [Google Scholar]
- 14.Sartorius N, Jablensky A, Korten A, et al. Early manifestations and first-contact incidence of schizophrenia in different cultures. A preliminary report on the initial evaluation phase of the WHO Collaborative Study on determinants of outcome of severe mental disorders. Psychol Med. 1986;16:909–928. doi: 10.1017/s0033291700011910. [DOI] [PubMed] [Google Scholar]
- 15.King M, Nazroo J, Weich S, et al. Psychotic symptoms in the general population of England—a comparison of ethnic groups (The EMPIRIC study) Soc Psychiatry Psychiatr Epidemiol. 2005;40:375–381. doi: 10.1007/s00127-005-0900-7. [DOI] [PubMed] [Google Scholar]
- 16.Salomon JA, Mathers CD, Chatterji S, Sadana R, Ustun TB, Murray CJL. Quantifying individual levels of health: definitions, concepts and measurement issues. In: Murray CJL, Evas DB, editors. Health Systems Performance Assessment: Debates, Methods and Empiricism. Geneva, Switzerland: World Health Organization; 2003. pp. 301–318. [Google Scholar]
- 17.World Bank. World Bank List of Economies. 2010; http://data.worldbank.org/about/country-classifications/country-and-lending-groups. Accessed July 27, 2010. [Google Scholar]
- 18.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 19.Ahmad OB, Boschi-Pint C, López AD, Murray CJL, Inoue M. Age Standardization of Rates: A New WHO Standard. 2001. Geneva, Switzerland: World Health Organization. GPE Discussion Paper Series. [Google Scholar]
- 20.Ustun TB, Chatterji S, Mechbal A, Murray CJL WHS Collaborating Groups. Quality assurance in surveys: standards, guidelines and procedures. In: Household Sample Surveys in Developing and Transition Countries. New York: United Nations Statistics Division, Department for Economic and Social Affairs; 2005:199–230. [Google Scholar]
- 21.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cooper L, Peters L, Andrews G. Validity of the Composite International Diagnostic Interview (CIDI) psychosis module in a psychiatric setting. J Psychiatr Res. 1998;32:361–368. doi: 10.1016/s0022-3956(98)00021-1. [DOI] [PubMed] [Google Scholar]
- 23.Amorim P, Lecrubier Y, Weiller E, Hergueta T, Sheehan D. DSM-IH-R Psychotic Disorders: procedural validity of the Mini International Neuropsychiatric Interview (MINI). Concordance and causes for discordance with the CIDI. Eur Psychiatry. 1998;13(1):26–34. doi: 10.1016/S0924-9338(97)86748-X. [DOI] [PubMed] [Google Scholar]
- 24.Hanssen MS, Bijl RV, Vollebergh W, Van OJ. Self-reported psychotic experiences in the general population: a valid screening tool for DSM-III-R psychotic disorders? Acta Psychiatr Scand. 2003;107:369–377. doi: 10.1034/j.1600-0447.2003.00058.x. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: history, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 26.Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: the relevance of thresholds. Br J Psychiatry. 2010;196:365–371. doi: 10.1192/bjp.bp.109.071191. [DOI] [PubMed] [Google Scholar]
- 27.Wilson M, Allen DD, Li JC. Improving measurement in health education and health behavior research using item response modeling: comparison with the classical test theory approach. Health Educ Res. 2006;21(Suppl 1):i19–i32. doi: 10.1093/her/cyl053. [DOI] [PubMed] [Google Scholar]
- 28.Linacre JM. A User's Guide to Winsteps Ministeps Rasch-Model Computer Programs, Program Manual. Chicago, IL: Winsteps.com; 2005. [Google Scholar]
- 29.Royston P. Multiple imputation of missing values. Stata J. 2004;4:227–241. [Google Scholar]
- 30.van Buuren S, Oudshoorn CGM. Multivariate Imputation by Chained equations. MICE V 1.0 User's Manual. Leiden, The Netherlands: TNO Preventie en Gezondheid; 2009. [Google Scholar]
- 31.Stata Statistical Software: Release 10 [computer program] College Station, TX: StataCorp LP; 2007. StataCorp. [Google Scholar]
- 32.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rossler W, Riecher-Rossler A, Angst J, et al. Psychotic experiences in the general population: a twenty-year prospective community study. Schizophr Res. 2007;92(1–3):1–14. doi: 10.1016/j.schres.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 34.Jablensky A, Sartorius N, Ernberg G, et al. Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychol Med Monogr Suppl. 1992;20:1–97. doi: 10.1017/s0264180100000904. [DOI] [PubMed] [Google Scholar]
- 35.Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frances A. Whither DSM-V? Br J Psychiatry. 2009;195(5):391–392. doi: 10.1192/bjp.bp.109.073932. [DOI] [PubMed] [Google Scholar]
- 37.Jablensky A. Towards ICD-11 and DSM-V: issues beyond ‘harmonisation’. Br J Psychiatry. 2009;195:379–381. doi: 10.1192/bjp.bp.109.071241. [DOI] [PubMed] [Google Scholar]
- 38.Van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635–645. doi: 10.1016/S0140-6736(09)60995-8. [DOI] [PubMed] [Google Scholar]
- 39.Carpenter WT. Anticipating DSM-V: should psychosis risk become a diagnostic class? Schizophr Bull. 2009;35:841–843. doi: 10.1093/schbul/sbp071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corcoran CM, First MB, Cornblatt B. The psychosis risk syndrome and its proposed inclusion in the DSM-V: a risk-benefit analysis. Schizophr Res. 2010;120(1–3):16–22. doi: 10.1016/j.schres.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang LH, Wonpat-Borja AJ, Opler MG, Corcoran CM. Potential stigma associated with inclusion of the psychosis risk syndrome in the DSM-V: an empirical question. Schizophr Res. 2010;120(1–3):42–48. doi: 10.1016/j.schres.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yung AR, Nelson B, Thompson AD, Wood SJ. Should a “Risk Syndrome for Psychosis” be included in the DSMV? Schizophr Res. 2010;120(1–3):7–15. doi: 10.1016/j.schres.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 43.Arango C. Risk syndrome for schizophrenia/psychosis or attenuated psychotic symptoms syndrome. How they may affect child and adolescent psychiatry? Eur Child Adolesc Psychiatry. 2010 doi: 10.1007/s00787-010-0144-2. In press. [DOI] [PubMed] [Google Scholar]