Abstract
In this article, a data-driven approach was adopted to demonstrate how real-life diary techniques [ie, the experience sampling method (ESM)] could be deployed for assessment purposes in patients with psychotic disorder, delivering individualized and clinically relevant information. The dataset included patients in an acute phase of psychosis and the focus was on paranoia as one of the main psychotic symptoms (30 patients with high levels of paranoia and 34 with low levels of paranoia). Based on individual cases, it was demonstrated how (1) symptom and mood patterns, (2) patterns of social interactions or activities, (3) contextual risk profiles (eg, is being among strangers, as opposed to family, associated with higher paranoia severity?), and (4) temporal dynamics between mood states and paranoia (eg, does anxiety precipitate or follow the onset of increased paranoia severity?) substantially differ within individual patients and across the high vs low paranoid patient group. Most striking, it was shown that individual findings are different from what is found on overall group levels. Some people stay anxious after a paranoid thought came to mind. For others, paranoia is followed by a state of relaxation. It is discussed how ESM, surfacing the patient’s implicit knowledge about symptom patterns, may provide an excellent starting point for person-tailored psychoeducation and for choosing the most applicable therapeutic intervention.
Keywords: experience sampling method, mobile assessment, psychosis, affect/schizophrenia
Introduction
To find out what people do in general, we must first discover what each person does in particular, then determine what, if anything, these particulars have in common …
Thorngate, 1986, In: Valsiner (ed), The Individual Subject and Scientific Psychology, pp 75-76.1
Real-life diary techniques such as the experience sampling method (ESM)2,3 or ecological momentary assessment (EMA)4 have fundamentally increased our knowledge of the phenomenology and etiology of psychotic disorders. It has been shown that positive symptoms, such as hallucinations and delusions fluctuate over periods of minutes or hours, and both internal and external contextual features may influence the frequency and intensity of these symptoms as they unfold in daily life.5 Increases in paranoia, for example, were found to be precipitated by a decrease in self-esteem,5 an increase in anxiety,5,6 and increased feelings of subjective stress.7 Similarly, anxiety and depression have been shown to precipitate the onset of hallucinations.8 External factors have also been implicated in the onset of positive symptoms including day-to-day urban exposure,9 social context,10 and cannabis use.11 All these studies investigated and compared groups and showed that self-monitoring of psychotic symptoms (1) is feasible, (2) provides a much more detailed and fine-grained picture of symptoms, and (3) reveals patterns that may be relevant for treatment.12
Assessing individual risk profiles and symptom patterns in daily life rather than group comparisons based on retrospective reports would offer important information for clinical practice. For decades, clinicians have sought for possibilities to extend regular (psycho)therapy into patients’ everyday life.13 As a result, homework assignments are considered as a core and crucial component of psychotherapy.14,15 Recently, several authors have emphasized a possible role for momentary assessment using mobile technology (eg, palmtop computer, mobile phone) in clinical practice, referred to as “mobile intervention”.12,13,16–18 Mobile interventions have several advantages over regular homework assignments and daily diaries, such as the possibility to tailor the content of the intervention based on person characteristics or current mental state and to provide basic exercises and tasks.13 As described by Granholm and colleagues (2008),19 mobile phones have been used to give individualized, in-the-moment feedback based on information about symptoms that was gathered during previous face-to-face clinical therapy sessions (eg, for hallucinations “Did you ever not comply with what the voices were asking of you? Do you remember what happened?”). Another recently published study protocol aims at enrolling people with psychotic disorder in a 5 km running program.17 Mobile technology is elegantly used in this project to count running steps and to play an individualized music playlist. These are all very promising studies because they move the therapy outside the doctor’s office into patient’s real life.
ESM, however, may be equally relevant in earlier stages of the clinical process, during the assessment and diagnostic phase. During this phase, the clinician and the patient have to create a mutual dialectic about the nature and causes of the patient’s problems. Momentary assessment may substantially contribute to this process because it provides real-life data about the particular patient improving both the patient’s and the therapist’s insight into symptom patterns as well as into the specific internal and contextual triggers (eg, does cannabis increase or decrease symptom intensity in this person? Are hallucinations more present when alone vs with others?), thus creating an opportunity for tailoring treatment to the specific needs and problems of the patient. Making patients active partners in this assessment process, resulting in a greater sense of ownership and empowerment, may improve compliance during the therapeutic phase. In an ongoing research project by Wichers and colleagues,18 first positive results have been found in a sample of patients with depression, who were given weekly feedback on their symptoms based on their personal ESM reports over a period of 6 weeks.
In the current article, we used a data-driven approach to demonstrate how the ESM could be deployed for assessment purposes in individual patients with psychotic disorder, delivering individualized and clinically relevant information. We will focus on paranoia as one of the main psychotic symptoms, but similar approaches could be adopted for other symptoms. First, we will demonstrate how ESM can improve insight into symptom and mood patterns, by showing individual moment-to-moment and daily variation in paranoia intensity, positive affect (PA), and negative affect (NA). Second, we will illustrate how ESM can contribute to a better understanding of day patterns of social interactions or activities that someone is involved in. People are often poor judges of these patterns and this may be particularly true for patients with unstructured day patterns who often experience cognitive problems. Third, ESM data will be used to disentangle individual contextual risk patterns, associating contextual features such as social company with paranoia severity. Fourth, internal mood states such as anxiety may precipitate the onset of increased paranoia severity but could equally result from increased paranoia. In this article, it is illustrated how the temporal dynamic association between mood states and paranoia could be disentangled for individual patients.
The dataset5 includes patients in an acute phase of psychosis, 1 group with high levels of paranoia (30 patients), and another group with low levels of paranoia (34 patients). Based on individual cases, we will examine how these patterns differ within individual patients and across the 2 patient groups.
Methods
Sample
A previously collected ESM dataset designed to study paranoia was selected.5 This dataset included 2 patient groups: 30 patients diagnosed with a psychotic disorder who currently present paranoid psychotic symptoms (“paranoid patients”) (defined as having a score of >3 on item P6 [suspiciousness] of the Positive and Negative Syndrome Scale [PANSS]) and 34 patients diagnosed with a psychotic disorder who currently have other psychotic symptoms (“nonparanoid patients”) (defined as having a score of <4 on the PANSS items P6 [suspiciousness] and having a score of >3 on at least one of the PANSS items P1 [delusions], P3 [hallucinatory behavior], P5 [grandiosity], and G9 [unusual thought content]) (for a full description of the sample see ref.5). Information regarding number of valid reports, sociodemographic, and clinical characteristics of the 2 patient groups are summarized in table 1.
Table 1.
Demographics and Sample Characteristics
| Paranoid Patients (n = 30) | Nonparanoid Patients (n = 34) | |
| Sex, % male/female | 87/13 | 76/24 |
| Age, mean (SD) | 38.1 (10.7) | 36.0 (11.6) |
| Diagnosis | ||
| Schizophrenia/psychotic disorder (n) | 28 | 28 |
| Schizoaffective disorder (n) | 2 | 6 |
| PANSS total, mean (SD) | 71.4 (13.7) | 60.5 (9.7) |
| PANSS suspiciousness, mean (SD) | 5.3 (1.1) | 2.3 (0.9) |
| Number valid beeps, mean (range) | 37 (20–59) | 38 (21–58) |
| Negative affect, mean (SD) | 2.3 (1.3) | 1.9 (1.2) |
| Positive affect, mean (SD) | 4.2 (1.5) | 4.5 (1.5) |
| Paranoia, mean (SD) | 3.1 (1.6) | 2.1 (1.1) |
| Anxiety, mean (SD) | 2.3 (1.7) | 1.8 (1.3) |
| Irritation, mean (SD) | 2.4 (1.8) | 2.1 (1.6) |
| Relaxation, mean (SD) | 4.3 (1.7) | 4.5 (1.8) |
Note: PANSS, Positive and Negative Syndrome Scale.
Inclusion criteria for all participants were (1) signed informed consent, (2) age 18–65 years, and (3) sufficient command of the Dutch language to understand and fill out the questionnaires. Patients were recruited from clinical and ambulatory mental health facilities in the south of the Netherlands. Interview data and, when necessary, clinical record data were used to yield International Classification of Diseases and Related Health Problems-10 diagnosis by the OPCRIT computer program.20
ESM Procedure
Data on daily life experience were collected using the ESM, a structured self-assessment technique, collecting data in the natural flow of daily life.2,3 Previous studies have demonstrated the feasibility, validity, and reliability of ESM in general and patient populations.3,21 Participants received a pre-programmed digital wristwatch and 10 pocket size assessment forms collated in a booklet for each day. Ten times a day on 6 consecutive days, the watch emitted a signal at unpredictable moments between 7.30 am and 10.30 pm. After each “beep”, participants were asked to fill out the ESM self-assessment forms, collecting reports of mood, psychopathology, and context on 7-point Likert scales and open-ended questions.
The ESM procedure was explained in a briefing session, and all participants completed a practice form in order to confirm that they did understand the procedure. Participants were instructed to complete their reports immediately after the beep and to register the time at which they completed the questionnaire. During the sampling period, research staff contacted participants frequently by phone or visited them to assess whether they were complying with the instructions. During a debriefing session, participants were interviewed to be sure that they had complied with the instructions. Reports were assumed valid when subjects responded to the beep within 15 minutes. Participants were only included in the analyses when they responded validly to at least one-third of the emitted beeps.22
ESM Measures
The following variables were derived from the ESM questionnaires:
Paranoid Ideation.
This was measured using participants’ mean score on the items “I feel that others dislike me,” “I feel that others might hurt me,” “I feel suspicious,” and “I feel safe,” rated on a 7-point Likert scale, ranging from 1 not at all to 7 very (Cronbach’s alpha 0.76).
Mood.
Participants’ mean score on 5 emotion adjectives (insecure, lonely, anxious, sad, irritated, and guilty) constituted NA (Cronbach’s alpha 0.83). PA was defined as the mean score on 3 emotion adjectives (cheerful, relaxed, and satisfied; Cronbach’s alpha 0.80). All emotion items were rated on 7-point Likert scales (1 not at all to 7 very).
Social company.
At each beep, participants indicated whether they were alone or in social company. Responses were coded as (0) alone, (1) family, (2) friends, (3) health care professional, (4) acquaintances, and (5) strangers/others.
Activity.
At each beep, participants indicated what they were doing. Responses were coded as (0) nothing, (1) work/school, (2) household chores/(self)care, (3) leisure/watching television, (4) transport, (5) social interaction, (6) eating/drinking, and (7) something else.
Results
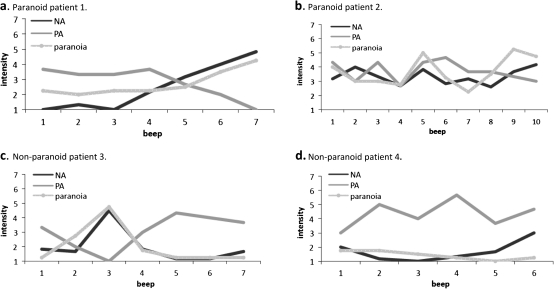
Mood and Symptom Expression in Real Life
In order to illustrate how moment-to-moment and day-to-day fluctuations in symptoms and mood may differ between persons both within and across the 2 patient groups, data are shown for 2 patients within each group. Figure 1 shows the moment-to-moment fluctuation in paranoia, PA, and NA over a 1-day period. For paranoid patient 1, both paranoia and NA levels increase during the day (starting at beep 3) (figure 1a) , with a decrease in PA starting roughly 1 beep later (at beep 4), whereas for paranoid patient 2 (figure 1b), strong fluctuations on all 3 variables are apparent throughout the day. In figure 1c (nonparanoid patient 3), a clear “peak” in paranoia and NA intensity and concurrent “low” PA level is shown around the third measurement moment of the day. The lost balance is restored, however, 1 beep later (ie, a drop in paranoia and NA and an increase in PA). In contrast, for nonparanoid patient 4 (figure 1d), no such “peaks” or “lows” are found. These examples underline the added value of ESM for the assessment of clinical symptoms of individual patients in detecting different moment-to-moment symptom fluctuation patterns throughout the day.
Fig. 1.
Moment-to-moment fluctuation in paranoia, negative, and positive affect.
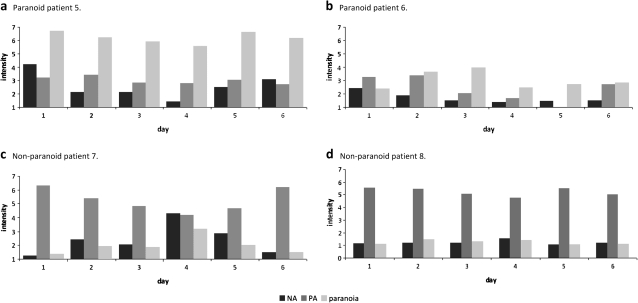
Figure 2 presents the day-to-day fluctuation in levels of paranoia, PA, and NA over the period of 1 ESM week (6 consecutive days). It is shown that day-to-day paranoia levels and fluctuation thereof do vary from 1 patient to another. In addition, these examples show that all 3 variables (NA, PA, and paranoia) vary relatively independent from each other on a day-to-day basis. Figure 2a, for example, shows that on a day with a high average paranoia level, NA level is not necessarily high or PA level low. When comparing paranoid patient 5 and nonparanoid patient 7 (figures 2a and 2c), paranoia levels are rather different for both patients, whereas day-to-day changes in NA and overall NA levels are similar for both of them. Figures 2a and 2b (paranoid patients 5 and 6) visualize that high scores on clinical interview measures of paranoia (eg, the PANSS23) do not necessarily mean that people will experience paranoia every day, all the time.
Fig. 2.
Day-to-day fluctuation in paranoia, negative, and positive affect.
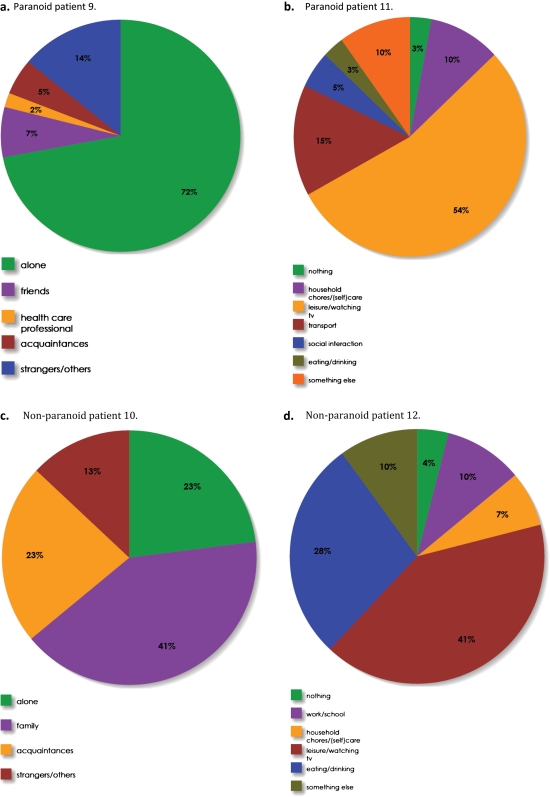
Real-Life Contextual Patterns
We selected 1 participant from each patient group to demonstrate individual differences in time spent in different categories of social company and activities (figure 3). These pie charts show that paranoid patient 9 (figure 3a) is alone most of the time, whereas nonparanoid patient 10 (figure 3c) spent a reasonable proportion of the time with family. Relatively minor differences in “time spent doing different activities” are shown between paranoid patient 11 (figure 3b) and nonparanoid patient 12 (figure 3d). These results show that contextual factors can be quite different or strikingly similar for patients with different scores on clinical symptom measures.
Fig. 3.
Time spent in different categories of ‘social company’ (3a and 3c) and ‘activity’ (3b and 3d).
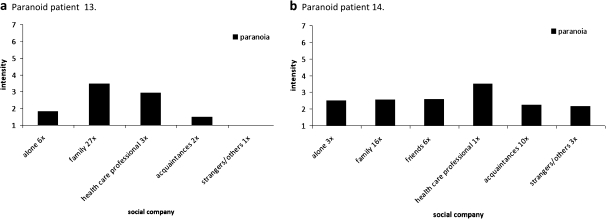
Association Between Daily Context and Paranoia Severity
The combination of providing insight in the association between daily life context (eg, social company) and paranoia level and showing data on how much time is actually spent in these contexts may be particularly powerful in inducing changes in behavior. We calculated standardized mean differences per individual, contrasting 2 conditions (ie, alone/not alone) on paranoia intensity. The standardized mean difference provides an effect size (>0.2 is considered a small effect and >0.5 a moderate effect) that is indicative of the effect of being in the company of others on paranoia level. A positive mean standardized difference indicates decreased paranoia levels when with others compared with when alone (ie, a positive effect of social company on paranoia levels), whereas a negative mean standardized mean difference stands for increased paranoia levels when with others compared with when alone (ie, a negative effect of social company).
A small positive effect of social company on paranoia level was found in 15 paranoid patients (50%) and 12 nonparanoid patients (35%). A moderate positive effect was present in 6 paranoid and 4 nonparanoid patients (20% and 12%, respectively). A small negative effect of social company was found in 4 paranoid patients (13%) and 10 nonparanoid patients (29%). A moderate negative effect was present in 1 paranoid patient (3%) and 4 nonparanoid patients (12%). No effect of social company was found in 11 paranoid patients (37%) and 8 nonparanoid patients (24%). In 4 nonparanoid patients, the effect of social company could not be calculated because they were never alone or did not show any variation in paranoia level. These data underline the differential effects of social context on paranoia intensity at the individual level.
Using ESM data, even more detailed information on the effect of social company can be shown, thereby refining the results of these analyses. Figure 4 shows paranoia levels in different social contexts in paranoid patient 13 and nonparanoid patient 14. Similar graphs could be drawn using other contextual variables such as activity, location, and drug use.
Fig. 4.
Paranoia levels in different social contexts.
Temporal Dynamic Relationships Between Mood and Paranoia
To investigate the dynamic relationship between paranoia and mood in each patient individually, vector auto regressive modeling (VAR)24 was used (Hoenders RHJ, Bos EH, de Jong JTVM, de Jonge P. Unraveling the dynamics between symptom and treatment variables in a lifestyle-oriented approach to anxiety disorder. A timeseries analysis. submitted). VAR is a technique for multivariate time series and especially suited for investigating the temporal dynamics between 2 or more variables, examining bidirectional influences without having to make a priori assumptions about the direction of the effects. By separating the dynamic part of the model (the relationships between the lagged values of the variables) from the simultaneous part (the relationships between the contemporaneous values), the model allows to make inferences about the temporal order of the effects (Hoenders RHJ, Bos EH, de Jong JTVM, de Jonge P. Unraveling the dynamics between symptom and treatment variables in a lifestyle-oriented approach to anxiety disorder. A timeseries analysis. submitted).24 For these analyses, we selected 3 separate mood items (anxiety, irritation, and relaxation) and conducted three 2-variable VARs (paranoia-anxiety, paranoia-irritation, and paranoia-relaxation). The auto regressive models were analyzed using the VAR module in STATA version 11.25 All variables were standardized in order to allow interpretation of the fixed regression coefficient (β) as a Cohen’s d effect size.26 Only associations with at least a moderate effect size (>0.5) are reported.
From the VAR analyses, 15 patients (5 paranoid patients) were dropped because of collinearity (insufficient variability) of paranoia, anxiety, irritation, or relaxation scores. The results of the analyses on the dynamics of mood and paranoia intensity are described in table 2. A positive association indicates that an increase in variable 1 precedes an increase in variable 2 (effect size >0.5). A negative association indicates that an increase in variable 1 precedes a decrease in variable 2 (effect size <−0.5).
Table 2.
Time-lagged Associations
| Positive Association |
Negative Association |
||||
| Low Paranoid Patients | Paranoid Patients | Low Paranoid Patients | Paranoid Patients | ||
| 1 | Anxiety → paranoia | 1 | 0 | 2 | 1 |
| 2 | Paranoia → anxiety | 4 | 4 | 0 | 3 |
| 3 | Irritation → paranoia | 0 | 0 | 0 | 1 |
| 4 | Paranoia → irritation | 6 | 4 | 3 | 2 |
| 5 | Relaxation → paranoia | 1 | 0 | 1 | 0 |
| 6 | Paranoia → relaxation | 3 | 3 | 3 | 7 |
Time-lagged associations between paranoia and mood state with a clinically relevant effect size could be detected in the data. However, the directionality of the associations differed per individual. The analyses show that most associations are found between current paranoia and emotional state at the next moment (n = 42), whereas only a small number of associations between current paranoia and emotional state at the previous moment were found (n = 7; see table 2). The analyses furthermore show that not only the directionality of the associations differed but also that both positive and negative associations between paranoia level and all 3 mood states are present: (1) current paranoia preceding an increase in anxiety at the next moment in 8 patients and preceding an decrease in anxiety in 3 patients, (2) current paranoia predicting an increase in irritation in 10 patients and a decrease in irritation in 5 patients, and (3) current paranoia preceding increased relaxation at the next moment in 6 patients and decreased relaxation in 10 patients. Surprisingly, only 1 positive effect size was found for the association between current paranoia and anxiety one moment before, showing that in this sample, an increase in anxiety rarely precedes a paranoia increase.
Overall, at least one of the mood states were temporally related to paranoia in 54% of patients (n = 36), not related to paranoia in 23% of patients (n = 15) and did not show enough variability to analyze temporal associations in 23% of patients (n = 15).
Discussion
This is the first study establishing the feasibility of mapping individual patient’s dynamic symptom patterns in daily life using real-time data collected with the ESM. The results underscore the added value of momentary assessment in the process of assessment, diagnosis, and treatment planning.
Unraveling Symptom Patterns
Data collected with ESM supplies both the clinician and the patient with a large amount of detailed information about symptoms that could not have been collected using standard clinical interview or retrospective self-report questionnaires. For example, it was shown that patients with current low paranoia scores on an interview-based clinical measure (ie, PANSS scores) nevertheless report considerable levels of paranoid ideation in the flow of daily life. Moreover, the results show that ESM has the capacity to zoom in on the patient’s moment-to-moment variability in symptoms, thereby providing insight into individual symptom patterns. For 1 patient, an ‘overall daily medium paranoia level’ could actually mean only 1 clear ‘peak’ in paranoia level and low paranoia intensity during the rest of the day, whereas for another patient, it may indicate a steady medium paranoia level throughout the day. Mobile assessment might therefore be an elegant and necessary addition to the mobile intervention techniques, which are currently being developed.
Therapeutics
Most patients are not explicitly aware of their own symptom patterns and the contextual factors impacting on those patterns. Momentary mobile assessment equips the patient (and clinician) to bring implicit knowledge about the patient’s own life to the surface, thereby furthering the establishment of a mutual dialectic about the nature and causes of the patient’s problems. The contrasting patterns found in these individualized analyses may aid tailoring treatment to the personal needs of each individual patient.
Person-tailored Psychoeducation
ESM data, uncovering symptom patterns and related factors, may provide an excellent starting point for person-tailored psychoeducation. Current psychoeducation courses are often based on general (group-level) knowledge about symptoms and rely on the patient’s (often diminished) cognitive ability to recognize this general information and apply it to his/her own life. Person-tailored psychoeducation based on real experiences of an individual person may be much more effective. Let us take the example of paranoia and its association with anxiety vs relaxation. It becomes apparent that the individualized findings are different from what is found on overall group levels (with anxiety significantly increasing paranoia levels).6 The results of studies comparing groups would be the reference frame adopted by the clinician. In the current study, however, a different pattern has been found for most individual patients. Some people stay anxious after a paranoid thought came to mind. This may explain why someone is not active or not able to engage in social interactions in the subsequent part of the day. For other patients, paranoia is followed by a state of relaxation. It would be interesting to explore why these patients become more relaxed. Are they able to adopt successful coping strategies? Or do they build up an enormous amount of tension leading to a paranoid peak (ie, “blowing off steam”) resulting in a state of relaxation afterwards? Similarly, the differential effects of social context could be discussed. How can we explain that being with others is beneficial for 70% of the paranoia patients and 47% of the non-paranoid patients, whereas a negative effect on paranoia level has been found for 16% of the paranoid and 41% of the nonparanoid patients?
Momentary Diagnostics-driven Intervention
Momentary assessment gives the clinician and patient a collective reference point that they can deploy to choose the most applicable intervention or “building blocks” for therapy. To illustrate this, we will again zoom in on the example of the patient who remains anxious and the patient who is relaxed after a paranoid moment. For the “anxious-after-paranoia-patient,” who apparently has a problem with “letting go” after the paranoid moment, practicing relaxation strategies or rumination therapy may be helpful. For the “relaxed-after-paranoia-patient,” it may be useful to train the patient to use this adaptive coping style of letting go or “blowing off steam” in other situations where coping is currently less adaptive. Additionally, teaching this patient to avoid building up of tension may eventually help decrease the intensity of the actual paranoid moment.
Limitations and Practical Issues
In order to perform time series analyses on data of an individual patient, we need a sufficient number of beeps. Many ESM studies use a minimum of 20 beeps per participant, which may not be optimal for analyzing data of an individual patient in clinical practice. The number of beeps should be optimized, balancing the time investment and effort for the patient and the amount of useful information that is gathered. An increase in the number of beeps per day, for example, would decrease the time between observations and refine the investigation of temporal relationships (Hoenders RHJ, Bos EH, de Jong JTVM, de Jonge P. Unraveling the dynamics between symptom and treatment variables in a lifestyle-oriented approach to anxiety disorder. A timeseries analysis. submitted). A first study using ESM as a clinical tool in depression revealed that even though participation was experienced as a challenge by the depressed patients to some extent, most patients indicated that they would have wanted to continue the protocol.18
In order to demonstrate the value of ESM for real-time assessment of symptoms and factors impacting on these symptoms, we chose several relevant symptoms and contextual variables. However, these specific variables are used as an illustration and our approach of individual momentary assessment and the analysis thereof can be applied to explore a broad range of other experiences, symptoms, and contextual factors, depending on the specific question of the patient and/or clinician.
In the current article, we showed how the assessment of symptom profiles provides very specific individualized information and can be used as a guideline in treatment. However, when using these individual symptom profiles results, one should consider their potential instability and change over time and treatment should therefore always be a process of continuous measuring, adapting, and tailoring to the needs of the patient. This issue is obviously not specific to our method
The current data were gathered using the traditional paper-and-pencil method for ESM, in which data entry is time consuming and branching or linking new questions to specific responses is not possible. Computerized ESM, using cell phones, Personal Digital Assistants, or tailor-made digital devices such as the PsyMate,12 resolves these constraints and it is a rapidly growing field, including in psychiatry research.19,27,28 Computerized ESM creates the opportunity of actual implementation of momentary assessment in clinical practice because it minimizes the effort and time investment for both the patient (filling in the questions) and the clinician (transcribing and analyzing the data). Furthermore, computerized ESM is instrumental for real-time and real-world delivery of psychological interventions. This procedure, referred to as ecological momentary intervention and described elsewhere,12,13,16–18 offers the opportunity to extend therapeutic interventions for patients with psychosis beyond the clinical setting.
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Funding
This work was supported by a 2006 NARSAD young investigator Award and by the Dutch Medical Research Council (Veni and Vidi grants).
References
- 1.Thorngate W. Behavioral patterns: detection and explanation. In: Valsiner J, editor. The Individual Subject and Scientific Psychology. New York, NY: Plenum Press; 1986. pp. 75–76. [Google Scholar]
- 2.Csikszentmihalyi M, Larson R. Validity and reliability of the experience-sampling method. J Nerv Ment Dis. 1987;175:526–536. doi: 10.1097/00005053-198709000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Myin-Germeys I, Oorschot M, Collip D, Lataster J, Delespaul P, van Os J. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med. 2009;39:1533–1547. doi: 10.1017/S0033291708004947. [DOI] [PubMed] [Google Scholar]
- 4.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 5.Thewissen V, Bentall RP, Lecomte T, van Os J, Myin-Germeys I. Fluctuations in self-esteem and paranoia in the context of daily life. J Abnorm Psychol. 2008;117:143–153. doi: 10.1037/0021-843X.117.1.143. [DOI] [PubMed] [Google Scholar]
- 6.Thewissen V, Bentall RP, Oorschot M, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Clin Psychol. 2011;50:178–195. doi: 10.1348/014466510X508677. [DOI] [PubMed] [Google Scholar]
- 7.Myin-Germeys I, Delespaul P, van Os J. Behavioural sensitization to daily life stress in psychosis. Psychol Med. 2005;35:733–741. doi: 10.1017/s0033291704004179. [DOI] [PubMed] [Google Scholar]
- 8.DelespauldeVries PM. deVries M, van Os J. Determinants of occurrence and recovery from hallucinations in daily life. Soc Psychiatry Psychiatr Epidemiol. 2002;37:97–104. doi: 10.1007/s001270200000. [DOI] [PubMed] [Google Scholar]
- 9.Ellett L, Freeman D, Garety PA. The psychological effect of an urban environment on individuals with persecutory delusions: the Camberwell walk study. Schizophr Res. 2008;99:77–84. doi: 10.1016/j.schres.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 10.Collip D, Oorschot M, Thewissen V, Van Os J, Bentall R, Myin-Germeys I. Social world interactions: how company connects to paranoia. Psychol Med. 2011;41:911–921. doi: 10.1017/S0033291710001558. [DOI] [PubMed] [Google Scholar]
- 11.Henquet C, van Os J, Kuepper R, et al. Psychosis reactivity to cannabis use in daily life: an experience sampling study. Br J Psychiatry. 2010;196:447–453. doi: 10.1192/bjp.bp.109.072249. [DOI] [PubMed] [Google Scholar]
- 12.Myin-Germeys I, Birchwood M, Kwapil T. From environment to therapy in psychosis: a real-world momentary assessment approach. Schizophr Bull. 2011;37:244–247. doi: 10.1093/schbul/sbq164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15:1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beck AT, Rush JA, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guildford Press; 1979. [Google Scholar]
- 15.Kazantzis N, Deane FP, Ronan KR. Assessing compliance with homework assignments: review and recommendations for clinical practice. J Clin Psychol. 2004;60:627–641. doi: 10.1002/jclp.10239. [DOI] [PubMed] [Google Scholar]
- 16.Depp CA, Mausbach B, Granholm E, et al. Mobile interventions for severe mental illness: design and preliminary data from three approaches. J Nerv Ment Dis. 2010;198:715–721. doi: 10.1097/NMD.0b013e3181f49ea3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Killackey E, Anda AL, Gibbs M, et al. Using internet enabled mobile devices and social networking technologies to promote exercise as an intervention for young first episode psychosis patients. BMC Psychiatry. doi: 10.1186/1471-244X-11-80. 2011;11:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wichers M, Hartmann JA, Kramer IM, et al. Translating assessments of the film of daily life into person-tailored feedback interventions in depression. Acta Psychiatr Scand. 2011;123:402–403. doi: 10.1111/j.1600-0447.2011.01684.x. [DOI] [PubMed] [Google Scholar]
- 19.Granholm E, Loh C, Swendsen J. Feasibility and validity of computerized ecological momentary assessment in schizophrenia. Schizophr Bull. 2008;34:507–514. doi: 10.1093/schbul/sbm113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGuffin P, Farmer A, Harvey I. A polydiagnostic application of operational criteria in studies of psychotic illness. Development and reliability of the OPCRIT system. Arch Gen Psychiatry. 1991;48:764–770. doi: 10.1001/archpsyc.1991.01810320088015. [DOI] [PubMed] [Google Scholar]
- 21.Oorschot M, Kwapil T, Delespaul P, Myin-Germeys I. Momentary assessment research in psychosis. Psychol Assess. 2009;21:498–505. doi: 10.1037/a0017077. [DOI] [PubMed] [Google Scholar]
- 22.Delespaul P. Assessing Schizophrenia in Daily Life—The Experience Sampling Method. Maastricht, The Netherlands: University Press; 1995. [Google Scholar]
- 23.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 24.Brandt PT, Williams JT. Multiple Time Series Models. Series: Quantitative Applications in the Social Sciences. Thousand Oaks, CA: Sage Publications Inc; 2007. [Google Scholar]
- 25.StataCorp LP. STATA Statistical Software: Release 11.0. College Station, TX: 2009. [Google Scholar]
- 26.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NY: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 27.Johnson EI, Grondin O, Barrault M, et al. Computerized ambulatory monitoring in psychiatry: a multi-site collaborative study of acceptability, compliance, and reactivity. Int J Methods Psychiatr Res. 2009;18:48–57. doi: 10.1002/mpr.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kimhy D, Delespaul P, Corcoran C, Ahn H, Yale S, Malaspina D. Computerized experience sampling method (ESMc): assessing feasibility and validity among individuals with schizophrenia. J Psychiatr Res. 2006;40:221–230. doi: 10.1016/j.jpsychires.2005.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]