Abstract
Aims
To provide an initial abuse liability assessment of an electronic cigarette (EC) in current tobacco cigarette smokers.
Design
The first of four, within-subject sessions was an EC sampling session that involved six, 10-puff bouts (30s interpuff interval) with each bout separated by 30-mins. In the remaining three sessions participants made choices between 10 EC puffs and varying amounts of money, 10 EC puffs and a varying number of own brand cigarette (OB) puffs, or 10 OB puffs and varying amounts of money using the multiple-choice procedure (MCP). The MCP was completed six times at 30-min intervals, and one choice was randomly reinforced at each trial.
Setting
Clinical laboratory.
Participants
Twenty current tobacco cigarette smokers.
Measurements
Sampling session outcome measures included plasma nicotine, cardiovascular response, and subjective effects. Choice session outcome was the crossover value on the MCP. Findings: EC use resulted in significant nicotine delivery, tobacco abstinence symptom suppression, and increased product acceptability ratings. On the MCP, participants chose to receive 10 EC puffs over an average of $1.06 or 3 OB puffs and chose 10 OB puffs over an average of $1.50 (p<.003).
Conclusions
Electronic cigarettes can deliver clinically significant amounts of nicotine and reduce cigarette abstinence symptoms and appear to have lower potential for abuse relative to traditional tobacco cigarettes, at least under certain laboratory conditions.
Introduction
Electronic cigarettes (ECs) are marketed to smokers who use them to quit or reduce smoking, to “vape” (i.e. use an EC) in situations where smoking is not permitted, manage craving, and/or improve health [1, 2, 3]. Although design characteristics vary [4, 5], the common feature is an electrically-powered heating element that vaporizes a liquid containing nicotine, humectants (propylene glycol and/or vegetable glycerin), and flavorings. Despite limited safety information, ECs are gaining popularity. For example, across a two-year monitoring period, internet searches for ECs surpassed the number of searches for snus, nicotine replacement therapy, or Chantix® (Champix® or varenicline) in the US by several hundred-fold [6].
Results of two clinical laboratory studies conducted in inexperienced EC users suggest that ECs are inefficient nicotine delivery devices [7, 8]. In one, the effects of two 10-puff bouts from one of two ECs (NJOY NPRO and Crown 7 Hydro) were examined in comparison to own brand and sham smoking (N=32) [8]. Neither EC increased plasma nicotine levels reliably, though both reduced tobacco abstinence symptoms and increased product acceptability ratings [8]. In the other, the effects of an EC (Ruyan®), nicotine inhaler, and tobacco cigarette were examined following a 1-hour ad-lib puffing period [7]. Plasma nicotine levels increased slightly following EC use (i.e., mean=1.3 ng/ml, 95% CI 0.0 to 2.6; N=8) and a reduction of tobacco abstinence symptom ratings was also observed [7]. The apparent growing popularity of ECs indicates a need for further empirical examination of their safety, efficacy and abuse liability [9].
Abuse liability refers to the degree to which a psychoactive drug or drug formulation would be used for non-medical purposes and that abuse of that drug would lead to physical and/or psychological dependence [10]. Abuse liability assessment can include pharmacodynamic and pharmacokinetic evaluation and behavioral testing to examine the reinforcing and rewarding effects of a novel drug/drug preparation [11, 12]. With the passage of the Family Smoking Prevention and Tobacco Control Act abuse liability is no longer relevant to new drugs only: the act gives the US Food and Drug Administration (FDA) the authority to regulate tobacco [13, 14] and extends the need for abuse liability assessment to include new tobacco products. In these cases, where any use is non-medical, the relative abuse liability of novel products as compared to that of currently marketed tobacco products becomes of great interest [15].
The multiple choice procedure (MCP) is an efficient means of examining factors related to abuse liability (e.g., drug reinforcement) in the human laboratory [16]. The MCP has been validated with tobacco products and nicotine [17, 18, 19, 20, 21], corresponds with other measures of reinforcement [16, 17], is sensitive to manipulation of study parameters (e.g., smoking deprivation, smoking cues) [17, 18], and can be used to determine the reinforcing efficacy of cigarettes/nicotine relative to other drugs, doses, or combinations (e.g. relative abuse liability) [19, 20, 21]. With the MCP, participants sample the novel drug and then make two or more discrete choices between it and 1) another drug/preparation or 2) a series of monetary values [16]. Following each series of choices, one is selected randomly and reinforced. The primary outcome measure is either the number of doses chosen or the maximum value of money at which the drug was chosen over money (i.e. crossover value), thus providing a contingency-based estimate of the value of that particular drug/dose/product. For example, in one study participants made choices between one or two packs of cigarettes and varying amounts of money [17]. The crossover values for one and two packs were $1.47 and $2.62, suggesting, as would be expected, that two packs of cigarettes have greater reinforcing value than one pack. Because the MCP has been used with success to evaluate the abuse liability of tobacco cigarettes, it may also be useful in examining EC abuse liability.
The purpose of the present study was to provide an initial abuse liability assessment of an EC. Participants who smoked tobacco cigarettes but not ECs first completed a sampling session consisting of six, 10-puff bouts from an EC with an 18 mg nicotine cartridge; plasma nicotine concentration, heart rate, and subjective effects were measured. Then, in independent sessions, participants completed a series of discrete choices comparing the relative value of the EC with 1) tobacco cigarettes and 2) money. We hypothesized that, in the sampling session, more than two, 10-puff bouts would be required to observe reliable nicotine delivery. We further hypothesized that the EC would be valued significantly lower than tobacco cigarettes on the MCP.
METHOD
Participants
This study and the informed consent were approved by the Institutional Review Board of Virginia Commonwealth University. Forty-one men and women recruited from the Richmond, VA area were consented. Prior to participation in any experimental sessions, 11 individuals were disqualified based on health concerns (e.g., high blood pressure) or failure to meet other inclusion/exclusion criteria. Ten were withdrawn for failure to make and/or keep appointments (n=6), repeated failure to meet the abstinence criterion (n=2), poor venous access (n=1), or a quit attempt (n=1). The remaining 20 participants (9 women, 9 Caucasian) completed the study. Participants smoked ≥15 cigarettes per day (CPD; M=20.5; SD=6.2), were age 18–55 (M=33.2; SD=11.8), provided a screening CO of ≥ 15 ppm (M=22.8; SD=7.7), and a urine cotinine of ≥ four on a seven point scale (0–6; NicAlert, Nymox Corp., Maywood, NJ) (M=6; SD=0). Participants were excluded if they reported chronic mental or physical health conditions, pregnancy or breastfeeding, active menopause, current use of ECs (although some participants had sampled an EC), current smoking cessation attempt, current illicit drug use (other than marijuana), or > 20 days marijuana or alcohol use in the past 30 days.
Materials, Methods and Measures
The “Vapor King” (KR808 model) automatic EC was used in this study (Vapor4Life, Northbrook, IL; http://v4l.com/Vapor_King_Single_Logo_Auto_Battery.html). It was chosen based on suggestions from experienced EC users who reported that this model would be acceptable to new users as it resembles a cigarette, and would produce a consistent vapor. The “Vapor King” consists of a rechargeable 3.7 v battery and air flow sensor with a lighted display end; a disposable cartridge (“cartomizer”) consisting of a metal threading (to fit securely onto the battery), heating element, and wicking that is saturated with nicotine solution. “WOW Cowboy” or “WOW Cowboy Menthol” tobacco flavored cartomizers (18 mg/ml nicotine; commonly used nicotine strength [22]; Vapor4Life) were matched to participants' tobacco cigarette flavorpreference (i.e. non-menthol, or menthol). A new “cartomizer” and fully charged battery were used for each session. Participants' usual brand of tobacco cigarette was used in the OB conditions.
This study was conducted outpatient at the Clinical Behavioral Pharmacology Laboratory on Virginia Commonwealth University's medical campus. Participants completed four, 4-hour long sessions that were separated by at least 48 hours, and were preceded by at least 12-hours of objectively-verified (CO ≤ 10 ppm) cigarette abstinence. The first session was a “sampling” session that familiarized participants with the EC. The remaining three sessions were randomly-ordered “choice” sessions that differed by the options provided.
Sampling Session
Participants arrived at the CBPL and their breath CO was measured to ensure compliance with the overnight abstinence criterion (i.e. CO ≤ 10 ppm; see 23). A catheter was inserted into a forearm vein, physiological monitoring equipment was attached and the session began with continuous monitoring of heart rate and blood pressure. Thirty minutes after session onset, participants completed baseline subjective-effect questionnaires and 7 ml of blood was sampled. Five minutes after the initial blood sampling, participants were presented with the EC and completed their first puffing bout (10 puffs; 30 second inter puff interval). Participants were not instructed regarding puffing behavior unless their initial puffs failed to activate the device, whereupon they were instructed to puff harder. Five minutes after the last puff from the EC, 7 ml of blood was sampled and participants responded to the questionnaires. This sequence of events was repeated five times at 30 minute intervals (i.e., EC administration, blood sampling, questionnaires). After the last blood sample was taken and questionnaires were completed, the catheter was removed, participants were compensated, and additional sessions were scheduled.
Physiological measures
Heart rate was measured every 20 seconds and blood pressure was measured every 5 minutes (Model 506, Criticare Systems). Blood was centrifuged and plasma stored at −70° C for later analysis of nicotine concentration [see 23 for details]. CO was assessed using a BreathCO monitor (Vitalograph).
Subjective-effect questionnaires
Participants responded to a computerized version of the Tiffany Drobes Questionnaire of Smoking Urges Brief (QSU Brief) [24]. The questionnaire consists of 10 items rated from 0 (Strongly disagree) to 6 (Strongly agree). Items are loaded onto two validated factors; factor 1 (intention to smoke) and factor 2 (anticipation of relief from withdrawal).
Participants also responded to visual analog scale (VAS) items in which a word or phrase was centered above a horizontal line anchored on the left with “Not at all” and the right with “Extremely”. A mouse-controlled cursor produced an adjustable vertical mark on the line. Scores on VAS items were calculated as the distance between the vertical mark and the left anchor and expressed as a percentage of line length. Eleven of these VAS items assessed nicotine/tobacco abstinence symptoms [25], 10 assessed the direct effects of nicotine [26] and 14 assessed the direct effects of the product [8].
Choice Sessions
For each choice session, breath CO was first measured to ensure compliance with the overnight abstinence criterion (see above). Thirty minutes after arrival, participants were administered a MCP questionnaire [e.g., 16] and were instructed to circle their choice for each of the 10 pairs of items presented. The choice questionnaire consisted of 2 columns and 10 rows, 10 puffs from the EC or OB was always presented in the left column while varying amounts of money ($.01, .02, .04, .08, .16, .32, .64, 1.28, 2.56, 5.12) or OB puffs (1, 2, 3, 4, 5, 6, 7, 8, 9, 10) was presented in ascending order in the right column. Immediately after the MCP was completed, participants were presented with one of their choices (drawn randomly) and given a 10 minute “consumption” period in which to take puffs or receive money. A 20 minute delay followed the consumption period. This sequence of events (choice procedure, 10 minute consumption, 20 minute delay) was repeated five times throughout each session. After the last consumption period, participants were compensated and, if necessary, additional sessions were scheduled. No blood was sampled or heart rate or subjective response monitored during choice sessions.
Data Analysis
The primary outcome for choice sessions was the “crossover value”: the point at which participants chose to receive money over 10 puffs from the EC or their OB. For the EC versus OB choice condition, the crossover value was defined as the point at which participants chose OB puffs over 10 puffs from the EC. In addition, the percentage of participants choosing puffs over money was examined in each of the money choice conditions.
Data were analyzed using PASW statistics version 18 (Cary, NC). Heart rate values were averaged for five-minute periods prior to each blood sampling. For plasma nicotine, values below the LOQ (2 ng/ml) were replaced by the LOQ as in previous work [26]. A one-way repeated measures ANOVA with Time (baseline, times 1–6) as the factor was performed on all outcome measures from the Sampling session and for crossover values from the EC versus OB multiple-choice procedure. A two-way repeated measures ANOVA with Time (times 1–6) and Condition (EC versus $, OB versus $) as factors was performed on crossover values from the multiple-choice procedure. Separate two-way ANOVAs were conducted to explore differences between conditions (EC versus $, OB versus $) in the average percentage of participants choosing puffs over money at each time-point and at each monetary value. Tukey's HSD post-hoc tests were used to compare means. Effects were considered significant at p < 0.05.
Results
Sampling Session
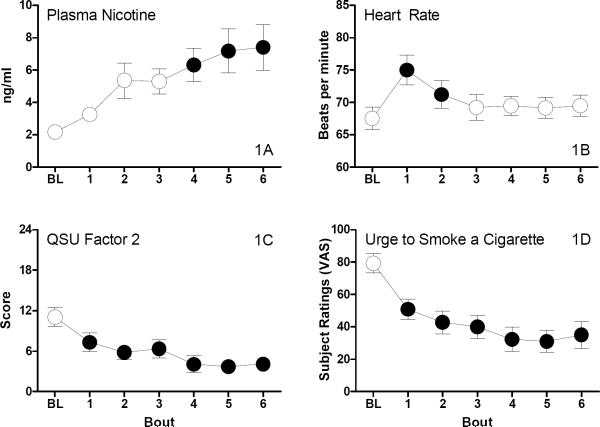
Plasma nicotine
A significant main effect of time (F6,114= 13.5; p<.0001) was observed for plasma nicotine (Figure 1A). Relative to baseline, a significant increase in plasma nicotine concentration was observed after the fourth 10-puff bout. Mean plasma nicotine increased from a pre-administration level of 2.2 (SD=0.78) ng/ml to 7.4 (SD=5.1) ng/ml five minutes after the final 10 puff bout.
Figure 1.
Average plasma nicotine concentration (1A), heart rate (1B), scores from QSU Factor 2 (anticipation of relief from withdrawal; 1C), and ratings of “Urge to smoke a cigarette” across six EC puffing bouts (N=20). BL indicates the baseline value (i.e. value observed at the start of the sampling session, prior to EC puffing). Filled symbols indicate a significant difference from baseline. Tukey's HSD (p < 0.05).
Cardiovascular Measures
A significant main effect of Time (F6,114=13.2, p<.0001) was observed for heart rate (Figure 1B). Heart rate increased from a pre-administration average of 67.5 (SD: 6.2) bpm to 75 (SD: 8.3) bpm five minutes after the first 10 puff bout. Heart rate was elevated following the first two 10 puff bouts only. No effect of EC administration was observed for systolic or diastolic pressure.
QSU Brief
A significant main effect of time was observed for QSU factor 1 (F6,114= 11.1, p<.0001) and factor 2 (F6,114= 11.9, p<.0001; Figure 1C). EC administration decreased factors 1 and 2 scores, relative to baseline following all six bouts.
Nicotine/tobacco abstinence symptoms
Significant main effects of Time were observed on ratings of “anxious”, “craving a cigarette/nicotine”, “impatient”, “irritability/frustration/anger”, “restless”, and “urge to smoke a cigarette” (Fs6,114 > 3.3, ps <.028). Figure 1D displays the data for “urge to smoke a cigarette” the measure with the greatest F value. Scores on these measures decreased relative to baseline.
Direct effects of nicotine
No significant effect of Time was observed for any measure from the direct effects of nicotine questionnaire.
Direct effects of product
Significant main effects of time were observed for ratings of “awake”, “calm”, “concentrate”, “harsh as own brand”, “mild as own brand”, “pleasant”, “smoke another right now”, “satisfying”, “taste good” and “taste like own brand” (Fs6,114>4.5, ps<.005). EC administration increased ratings on these measures. Effects of the highest magnitude were observed for ratings of “pleasant” (F6,114=21.1, p<.0001), “satisfying” (F6,114= 19.5, p<.0001), and “taste good” (F6,114= 20.2, p=.0001). Ratings of “awake”, “calm” and “concentrate” increased significantly only after the first bout, and ratings declined after that point.
Multiple Choice Procedure (Choice Sessions)
Money Choice Conditions
A significant main effect of Condition was observed for crossover values (F5,95=11.2; p<.003). Crossover values were greater in the OB versus $ choice condition relative to the EC versus $ condition. Collapsed across time, the average crossover value was $1.06 (SD=$0.16) in the EC versus $ condition and $1.50 (SD=$0.26) in the OB versus $ condition (Figure 2). A significant main effect of Condition (F5,45=12.7; p<.006) and a significant main effect of Time (F5,45=20.8; p<.0001) were revealed for the percentage of participants choosing puffs over money. Consistent with crossover value results, a higher percentage of participants chose to receive OB puffs relative to EC puffs. The percentage of participants choosing puffs over money declined over time, regardless of choice condition. Significant main effects of Condition (F9,171=5.0, p<.037) and Monetary Value (F9,171=68.7, p<.00001) were also revealed for the percentage of choices of puffs over money. A larger percentage of OB puff choices were observed relative to EC puff choices across monetary values. Choice of puffs over money decreased as monetary values increased, regardless of choice condition.
Figure 2.
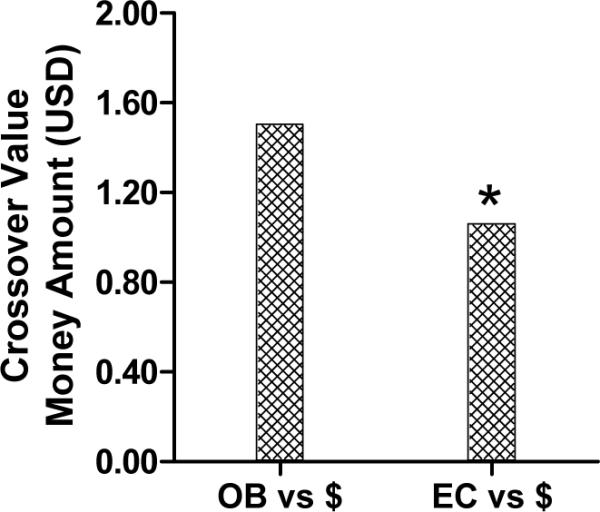
Average crossover values (i.e. the monetary value at which participants chose to receive money over 10 EC or OB puffs) collapsed across time for the OB vs. $ and EC vs. $ choice conditions. An asterisk indicates a significant effect of condition (p < 0.05).
EC versus OB condition
No significant main effect of Time was revealed for crossover values in the EC versus OB choice condition. The average crossover value, collapsed across time was 3 OB puffs (SD=0.4 puffs).
Discussion
The purpose of this investigation was to provide an initial abuse liability assessment of one EC brand/dose in current cigarette smokers. To accomplish this, the nicotine delivery profile, subjective and cardiovascular effects of an EC were examined following six 10-puff bouts with the device. Also, the relative reinforcing efficacy of the EC and own brand cigarettes was determined using a MCP. EC use resulted in reliable nicotine delivery after 40 puffs. We also observed tobacco abstinence symptom suppression and increased product acceptability ratings associated with EC use. MCP data suggest that, for our study sample and using these laboratory methods, the EC was less reinforcing than an own brand cigarette.
The results of this study, in which reliable nicotine delivery was observed only after the fourth 10-puff bout are consistent with our previous work showing that two, 10-puff EC bouts did not produce a significant increase in plasma nicotine concentration [8, 27]. Notably, both the magnitude of plasma nicotine concentration increase and its rapidity were less than that observed with a standard tobacco cigarette [27], suggesting that the current results may reflect more buccal than pulmonary delivery. A slower rate of nicotine delivery has important implications for abuse liability, as the rapidity with which a psychoactive drug (i.e. nicotine) is delivered to the brain is directly related to its potential for abuse and dependence [11, 28, 29]. This finding also has implications for EC use as a cessation aid: individuals accustomed to puffing 10 times from a traditional cigarette will likely need to take many more puffs in order to experience nicotine effects. If ECs are indeed less lethal alternatives to cigarettes, then potential users should be alerted that considerable effort may be needed to achieve at least some nicotine-mediated desired effects.
The results of this study illustrate the need to adapt clinical laboratory methods in order to evaluate novel nicotine/tobacco products within a rapidly evolving market. Nicotine delivery was likely observed in the current, but not the former study because participants engaged in six rather than two 10-puff EC bouts. However, another factor in nicotine delivery may be the brand of EC and cartomizer: brand differences in vapor nicotine content have been observed [1]. User experience may also influence EC nicotine delivery. Consistent with that latter notion, results of two recent studies suggest that experienced EC users are exposed to nicotine reliably [30, 31]. In fact, controlled laboratory evaluation indicates that experienced users puffing from their own ECs may be exposed to nicotine doses that approximate those of a standard cigarette [31]. Taken together, user instruction and product standardization may be required to optimize nicotine delivery, especially for EC-naïve consumers.
With regard to responses on the MCP, the probability of choosing EC or OB puffs decreased as monetary values increased, suggesting that choice behavior for both products was sensitive to this manipulation. Participants valued 10 EC puffs at 3 OB puffs and the average monetary crossover value for EC puffs ($1.06) was significantly lower than that for OB puffs ($1.50). Similarly, the percentage of participants choosing puffs over money was greater in the OB condition relative to the EC condition across time and monetary values, suggesting lower abuse potential of ECs relative to OB in this population. Comparison of ECs to other potential tobacco harm reduction products (snus, tobacco lozenges) or nicotine products (nicotine inhaler, nicotine gum) with the MCP would have provided an estimate of the relative reinforcing effects of ECs and a number of other nicotine/tobacco products [15].
Participants found the EC moderately acceptable as evidenced by increased ratings of “pleasant”, “satisfying” and “taste good”. Ratings on these measures increased after the first bout, despite no significant nicotine delivery, consistent with the notion that non-nicotine factors influence how pleasant or satisfying a product is perceived [8, 27, 32, 33, 34]. EC use also resulted in reduced ratings of “craving a cigarette” and “urge to smoke” as well as decreased scores on Factors 1 and 2 of the QSU. These results are consistent with anecdotal reports from EC users, suggesting that ECs could be an effective alternative to cigarette smoking [2, 3, 4, 5].
No adverse effects of ECs were observed in the current or previous studies [7, 8, 27, 31]. However, use of EC liquids is not without potential hazard, as they can contain trace amounts of impurities and contaminants [35, 36], the toxicant nicotine [37, 38], as well as propylene glycol and/or vegetable glycerin, inhalation of which may have unknown deleterious effects on lung function. The long-term health risks of EC use are unknown. Systematic laboratory evaluation as well as population-level surveillance of adverse events associated with EC use (e.g., nicotine poisoning, complications with pulmonary function, poisoning via contaminants in the liquid) will be necessary.
This study provides an initial abuse liability assessment of an EC in current smokers. Data suggest that the EC has lower abuse potential relative to tobacco cigarettes, at least in this population and under the specific laboratory conditions described here. Other EC models or nicotine liquid strengths may have a different propensity for abuse. Furthermore, the abuse potential and product appeal of ECs to youth, non-smokers, and occasional smokers should be examined. Future laboratory evaluation can build upon these methods and results to determine the ideal conditions under which ECs can substitute for tobacco cigarettes as well as the safety of ECs relative to tobacco cigarettes, including the abuse liability and long-term adverse event profile. These clinical laboratory methods have demonstrable internal and predictive validity and have been used successfully to determine the abuse potential and consequences of drug use for decades. [12; 15] Thus these methods are powerful tools that can be used to predict the effects of novel nicotine and tobacco products as required by FDA regulation.
Acknowledgements
The authors acknowledge, with gratitude, the hard work and dedication of the staff and students of VCU's Clinical Behavioral Pharmacology Laboratory (Ms. Barbara Kilgalen, Ms Janet Austin and Ms. Caroline Cobb) as well as the staff of VCU's Bioanalytical Core Laboratory Service Center. Dr. Eissenberg's effort on this project was supported by R01CA120142 while Dr. Vansickel's was supported by T32DA007027. The sponsor had no role in the design and conduct of the study; or in the preparation, review, or approval of the manuscript. The authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Declaration of Interest: This work was partially funded by the National Cancer Institute, National Institutes of Health RO1CA 120142 (awarded to Dr. Eissenberg). Dr. Vansickel was supported by National Institute on Drug Abuse, National Institutes of Health T32DA 007027. The authors have no conflicts of interest to declare.
References
- 1.Etter JF. Electronic cigarettes: a survey of users. BMC Public Health. 2010;10:231. doi: 10.1186/1471-2458-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heavner K, Dunworth J, Bergen P, Nissen C, Phillips CV. Electronic cigarettes (e-cigarettes) as potential tobacco harm reduction products: results of an online survey of e-cigarette users. Tob Harm Reduction [Internet] 2009 Nov;:15. [cited 2010 Feb 9]; working paper 011. Available from: http://www.tobaccoharmreduction.org/wpapers/011.htm.
- 3.McQueen A, Tower S, Sumner W. Interviews with”vapers”: implications for future research with electronic cigarettes. Nicotine and Tobacco Research. 2011;13:860–67. doi: 10.1093/ntr/ntr088. [DOI] [PubMed] [Google Scholar]
- 4.Trtchounian A, Williams M, Talbot P. Conventional and electronic cigarettes (e-cigarettes) have different smoking characteristics. Nicotine and Tobacco Research. 2010;12:905–12. doi: 10.1093/ntr/ntq114. [DOI] [PubMed] [Google Scholar]
- 5.Foulds J, Veldheer S, Berg A. Electronic cigarettes (e-cigs): views of aficionados and clinical/public health perspectives. International Journal of Clinical Practice. 2011;65:1037–42. doi: 10.1111/j.1742-1241.2011.02751.x. [DOI] [PubMed] [Google Scholar]
- 6.Ayers JW, Ribisi KM, Brownstein JS. Tracking the rise in popularity of electronic nicotine delivery systems (electronic cigarettes) using search query surveillance. American Journal of Preventive Medicine. 2011;40:448–53. doi: 10.1016/j.amepre.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Bullen C, McRobie H, Thornley S, Glover M, Laugesen M. Effect of an electronic cigarette on desire to smoke and withdrawal, user preferences and nicotine delivery: randomized cross-over trial. Tobacco Control. 2010;19(2):98–103. doi: 10.1136/tc.2009.031567. [DOI] [PubMed] [Google Scholar]
- 8.Vansickel AR, Cobb CO, Weaver MF, Eissenberg TE. A clinical laboratory model for evaluating the acute effects of electronic “cigarettes”: nicotine delivery profile and cardiovascular and subjective effects. Cancer Epidemiology, Biomarkers, and Prevention. 2010;19(8):1945–53. doi: 10.1158/1055-9965.EPI-10-0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Etter JF, Bullen C, Fouris AD, Laugesen M, Eissenberg T. Electronic nicotine delivery systems: a research agenda. Tobacco Control. 2011;20:243–48. doi: 10.1136/tc.2010.042168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drug Evaluation [Last accessed on 08/16/2011];Guidance for industry assessment of abuse potential of drugs: Draft guidance. 2010 http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guida nces/UCM198650.pdf.
- 11.Balster RL, Bigelow GE. Guidelines and methodological reviews concerning drug abuse liability assessment. Drug and Alcohol Dependence. 2003;70:S13–40. doi: 10.1016/s0376-8716(03)00097-8. [DOI] [PubMed] [Google Scholar]
- 12.Carter LP, Griffiths RR. Principles of laboratory assessment of drug abuse liability and implications for clinical development. Drug and Alcohol Dependence. 2009;105S:14–25. doi: 10.1016/j.drugalcdep.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Congress Family Smoking Prevention and Tobacco Control Act. Public Law 111-31; One Hundred Eleventh Congress of the United States of America; Congress: US Government Printing Office. 2009 http://frwebgate.access.gpo.gov/cgibin/getdoc.cgi?dbname=111_cong_public_laws&docid=f:publ031.111.pdf.
- 14.Carter LP, Stitzer ML, Henningfield JE, O'Connor RJ, Cummings KM, Hatsukami DK. Abuse liability assessment of tobacco products including potential reduced exposure products. Cancer Epidemiology Biomarkers and Prevention. 2009;18:3241–62. doi: 10.1158/1055-9965.EPI-09-0948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Institute of Medicine (IOM) Scientific standards for studies on modified risk tobacco products. The National Academic Press; Washington, DE: 2012. Available online at: http://www.iom.edu/Reports/2011/Scientific-Standards-for-Studies-on-Modified-Risk-Tobacco-Products.aspx. [Google Scholar]
- 16.Griffiths RR, Troisi JR, Silverman K, Mumford GK. Multiple-choice procedure: an efficient approach for investigating drug reinforcement in humans. Behavioural Pharmacology. 1993;4:3–13. [PubMed] [Google Scholar]
- 17.Griffiths RR, Rush CR, Puhala KA. Validation of the multiple-choice procedure for investigating drug reinforcement in humans. Experimental and Clinical Psychopharmacology. 1996;4:97–106. [Google Scholar]
- 18.Sayette MA, Martin CS, Wertz JM, Shiffman S, Perrott MA. A multi-dimensional analysis of cue-elicited craving in heavy smokers and tobacco chippers. Addiction. 2001;96:1419–32. doi: 10.1080/09652140120075152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmitz JM, Sayre SL, Hokanson PS, Spiga R. Assessment of the relative reinforcement value of smoking and drinking using a multiple-choice measurement strategy. Nicotine and Tobacco Research. 2003;5:729–34. doi: 10.1080/1462220031000158618. [DOI] [PubMed] [Google Scholar]
- 20.Jones HE, Garrett BE, Griffiths RR. Subjective and physiological effects of intravenous nicotine and cocaine in cigarette smoking cocaine abusers. Journal of Pharmacology and Experimental Therapeutics. 1999;288:188–97. [PubMed] [Google Scholar]
- 21.Sobel BF, Sigmon SC, Griffiths RR. Transdermal nicotine maintenance attenuates the subjective and reinforcing effects of intravenous nicotine, but not cocaine or caffeine, in cigarette-smoking stimulant abusers. Neuropsychopharmacology. 2004;29:991–1003. doi: 10.1038/sj.npp.1300415. [DOI] [PubMed] [Google Scholar]
- 22.Etter JF, Bullen C. Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction. 2011;106:2017–28. doi: 10.1111/j.1360-0443.2011.03505.x. [DOI] [PubMed] [Google Scholar]
- 23.Breland AB, Kleykamp BA, Eissenberg T. Clinical laboratory evaluation of potential reduced exposure products for smokers. Nicotine and Tobacco Research. 2006;8(6):727–38. doi: 10.1080/14622200600789585. [DOI] [PubMed] [Google Scholar]
- 24.Cox LS, Tiffany ST, Christen AG. Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine and Tobacco Research. 2001;3(1):7–16. doi: 10.1080/14622200020032051. [DOI] [PubMed] [Google Scholar]
- 25.Kleykamp BA, Jennings JM, Sams C, Weaver MF, Eissenberg T. The influence of transdermal nicotine on tobacco/nicotine abstinence and the effects of a concurrently administered cigarette in women and men. Experimental and Clinical Psychopharmacology. 2008;16:99–112. doi: 10.1037/1064-1297.16.2.99. [DOI] [PubMed] [Google Scholar]
- 26.Blank MD, Sams C, Weaver MF, Eissenberg T. Nicotine delivery, cardiovascular profile, and subjective effects of an oral tobacco product for smokers. Nicotine and Tobacco Research. 2008;10(3):417–21. doi: 10.1080/14622200801901880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eissenberg T. Electronic nicotine delivery devices: ineffective nicotine delivery and craving suppression after acute administration. Tobacco Control. 2010;19(1):87–88. doi: 10.1136/tc.2009.033498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abreu ME, Bigelow GE, Fleisher L, Walsh SL. Effects of intravenous injection speed on responses to cocaine and hydromorphone in humans. Psychopharmacology. 2001;154:76–84. doi: 10.1007/s002130000624. [DOI] [PubMed] [Google Scholar]
- 29.Busto U, Sellers EM. Pharmacokinetic determinants of drug abuse and dependence: a conceptual perspective. Clinical Pharmacokinetics. 1986;11:144–153. doi: 10.2165/00003088-198611020-00004. [DOI] [PubMed] [Google Scholar]
- 30.Etter JF, Bullen C. Saliva cotinine levels in users of electronic cigarettes. European Respiratory Journal. 2011;38:1219–20. doi: 10.1183/09031936.00066011. [DOI] [PubMed] [Google Scholar]
- 31.Vansickel AR, Eissenberg TE. Electronic cigarettes: effective nicotine delivery after acute administration. Nicotine and Tobacco Research. doi: 10.1093/ntr/ntr316. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buchhalter AR, Acosta MC, Evans SE, Breland AB, Eissenberg T. Tobacco abstinence symptom suppression: the role played by the smoking-related stimuli that are delivered by denicotinized cigarettes. Addiction. 2005;100:550–559. doi: 10.1111/j.1360-0443.2005.01030.x. [DOI] [PubMed] [Google Scholar]
- 33.Donny EC, Houtsmuller E, Stitzer ML. Smoking in the absence of nicotine: Behavioral, subjective, and physiological effects over 11 days. Addiction. 2007;102:324–334. doi: 10.1111/j.1360-0443.2006.01670.x. [DOI] [PubMed] [Google Scholar]
- 34.Donny EC, Jones M. Prolonged exposure to denicotinized cigarettes with or without transdermal nicotine. Drug Alcohol Depend. 2009;104:23–33. doi: 10.1016/j.drugalcdep.2009.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Food and Drug Administration Evaluation of e-cigarettes. FDA. 2009 May 4; [Cited 2009 Dec 10]. Available from: http://www.fda.gov/downloads/Drugs/ScienceResearch/UCM173250.pdf.
- 36.Hadwiger ME, Trehy ML, Ye W, Moore T, Allgire J, Westenberger B. Identification of amino-tadalafil and rimonabant in electronic cigarette products using high pressure liquid chromatography with diode array and tandem mass spectrometric detection. Journal of Chromatography A. 2010;1217:7547–55. doi: 10.1016/j.chroma.2010.10.018. [DOI] [PubMed] [Google Scholar]
- 37.Balakumar P, Kaur J. Is nicotine a key player or spectator in the induction and progression of cardiovascular disorders? Pharmacological Research. 2009;60:361–8. doi: 10.1016/j.phrs.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 38.Sjoberg N, Saint DA. A single 4 mg dose of nicotine decreases heart rate variability in healthy nonsmokers: implications for smoking cessation programs. Nicotine and Tobacco Research. 2011;13(5):369–72. doi: 10.1093/ntr/ntr004. [DOI] [PubMed] [Google Scholar]