Abstract
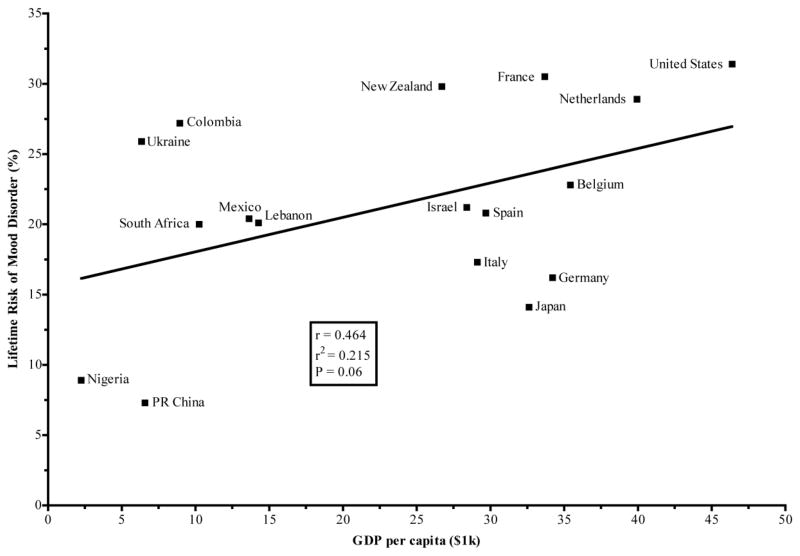
There has been much speculation about modern environments causing an epidemic of depression. This review aims to (1) determine whether depression rates have increased and (2) review evidence for possible explanations. While available data indicate rising prevalence and an increased lifetime risk for younger cohorts, strong conclusions cannot be drawn due to conflicting results and methodological flaws. There are numerous potential explanations for changing rates of depression. Cross-cultural studies can be useful for identifying likely culprits. General and specific characteristics of modernization correlate with higher risk. A positive correlation between a country’s GDP per capita, as quantitative measure of modernization, and lifetime risk of a mood disorder trended toward significance (p=0.06). Mental and physical well-being are intimately related. The growing burden of chronic diseases, which arise from an evolutionary mismatch between past human environments and modern-day living, may be central to rising rates of depression. Declining social capital and greater inequality and loneliness are candidate mediators of a depressiogenic social milieu. Modern populations are increasingly overfed, malnourished, sedentary, sunlight-deficient, sleep-deprived, and socially-isolated. These changes in lifestyle each contribute to poor physical health and affect the incidence and treatment of depression. The review ends with a call for future research and policy interventions to address this public health crisis.
Keywords: evolutionary medicine, depression, modernization, chronic disease, epidemiology, health behaviors
Introduction
Drastic changes in daily life over the past century are fueling the growing burden of chronic diseases, including atherosclerosis, hormone-related and gastrointestinal cancers, osteoporosis, and type 2 diabetes mellitus (Beckman et al., 2002; Eaton and III, 2004; Mokdad et al., 2001; Omenn, 2010; Smith, 2002). These diseases share a high-degree of co-morbidity and behavioral risk factors, are endemic to industrialized nations, and have been associated with a similar physiologic profile of metabolic and inflammatory dysregulation (Beckman et al., 2002; Coussens and Werb, 2002; Libby et al., 2002; Moussavi et al., 2007; Mundy, 2007; Must et al., 1999; Nicklas et al., 2005; Shoelson et al., 2007). Though there is evidence of some human evolution since the advent of agriculture ~10,000 years ago (Perry et al., 2007), Homo sapiens are considered to be most adapted to the diverse array of hunter-gatherer lifestyles characteristic of past evolutionary environments, collectively referred to as the environment of evolutionary adaptedness (EEA) (Barkow et al., 1992; Irons, 1998). The discrepancy between the modern environment and the human EEA serves as the theoretical foundation for understanding the ultimate etiology of the aforementioned chronic diseases (Eaton et al., 2002; Omenn, 2010; Smith, 2002). They are commonly called “diseases of modernity.” As the leading cause of morbidity and mortality, diseases of modernity are the greatest threat to public health in the developed world (Yach et al., 2006). If the mismatch between contemporary and historic lifestyles adequately explains increasing lifetime risk of depression in the modern-industrialized world, then depression should be considered a disease of modernity as well.
“Modernity” is a continuous concept that begins with agriculture, followed by industrialization, urbanization, and ever-accelerating changes in technology and social structure. “Modernization” is loosely defined in this review as the conglomeration of a society’s urbanization, industrialization, technological advancement, secularization, consumerism, and westernization. “Depression” refers to the symptoms that define major depressive disorder (MDD). This review addresses two fundamental questions: a) have depression rates increased? And (b) if so, why?
An epidemic of depression?
All diseases of modernity exhibit the sine qua non characteristic of an increasing incidence over time, because the environment continues to deviate further from the human EEA and individuals live longer within these novel environments. Depression is certainly not new, though its prevalence throughout human history is unknown. The affliction of sorrow, fright, and despondency exhibits remarkable historical continuity from ancient to modern times (Burton, 1845; Jackson, 1986). Evidence for or against the possibility of changing rates over millennia and centuries is wanting. In his encyclopedic account of the subtypes, causes, and treatments of melancholy, from the 17th century, Richard Burton notes its ubiquity:
Being then a disease so grievous, so common, I know not wherein to do a more general service, and to spend my time better, than to prescribe means how to prevent and cure so universal a malady, an epidemical disease, that so often, so much crucifies the body and minds (Burton, 1845)
Systematic epidemiologic study of depression began in the 20th century. Unfortunately, measurement of clinical populations (rather than community sampling), recall bias of retrospective studies, and inconsistent findings from longitudinal surveys bedevil this research. In the 1960’s, clinicians found that patients were younger, more neurotic, and less severely depressed than in earlier decades (Paykel et al., 1970; Rosenthal, 1966). It was suggested this reflected the social trend to view emotional problems as treatable psychiatric conditions and not merely part of the normal vicissitudes of life. The apparent rise in depression has been attributed to changes in diagnostic criteria that fail to account for the context of the symptoms, which has led to the misclassification of normal responses of sadness as a mental disorder (Horwitz and Wakefield, 2007). This review avoids this point of contention by only assessing rates of depression as currently defined symptomatically. A review of family and community studies revealed a higher lifetime probability of developing MDD and an earlier age-of-onset in younger cohorts (Klerman and Weissman, 1989). The largest community-based, cross-sectional studies of mental illness use retrospective methodology. They report a greater lifetime risk of mood disorders (Kessler et al., 2007) and, specifically, MDD in each successive generation (Andrade et al., 2003). A similar cohort effect was found in the US population in the National Comorbidity Survey Replication (NCS-R) (Kessler et al., 2003); although, 12-month prevalence estimates were lower than those measured a decade earlier in the original NCS (Kessler et al., 1996). The investigators attribute this discrepancy to methodological modifications implemented to reduce false-positives in the NCS-R (Kessler et al., 2003). The calculated risk of lifetime-prevalence from these retrospective studies likely reflects a significant degree of recall bias. People often exhibit poor recall and under-report past depressive episodes in community samples (Bromet et al., 1986), especially milder episodes for which no treatment was received (Simon and VonKorff, 1995; Wells and Horwood, 2004).
Longitudinal surveys are less susceptible to recall bias. A community-based study of American adults found the one-year prevalence of MDD rose from 3.33% to 7.06% between 1991–92 and 2001–02 (Compton et al., 2006). A meta-analysis of Minnesota Multiphasic Personality Inventory (MMPI) data of American college (N=63,706) and high school (N=13,870) students found that young adults were 6–8 times more likely to meet the cutoff for a psychopathologic score on the clinical depression scale in 2007 compared to peers in 1938 (Twenge et al., 2010). In measurement of the point prevalence of psychiatric disorders in a Swedish population in 1947, 1957, and 1972, investigators found (a) depression had the largest increase in prevalence for all disorders and (b) there was an increased risk for all age groups with young adults exhibiting a tenfold increased risk from 1957 to 1972 compared to 1947 to 1957 (Hagnell, 1989; Hagnell et al., 1994). One large community study of psychiatric morbidity in Canada found no evidence for a period or cohort effect, reporting a steady 5% prevalence of MDD in 1952, 1970, and 1992 (Murphy et al., 2000). To summarize, retrospective studies claim younger cohorts are more likely to develop depression with an earlier age of onset, but the evidence is confounded by recall bias. Longitudinal studies mostly confirm a rising prevalence of depression. In conclusion, available evidence suggests we may indeed be in the midst of an epidemic of depression.
Possible explanations for changing rates
In spite of accumulating material wealth and a rising standard of living, why would young people have a higher risk of depression than their parents and grandparents? The rest of the review will discuss possible explanations for why depression rates could be increasing. First, a general rise in psychopathology could contribute to this phenomenon because psychiatric disorders have high co-morbidity. Drug and alcohol abuse are often found in conjunction with depression (Regier et al., 1990). Estimates of lifetime prevalence of substance use disorders in the US range from 10.3% to 26.6% (Compton et al., 2007; Kessler et al., 1994) with an increased lifetime risk in younger cohorts (Kessler et al., 2005). Anxiety disorders are the most common class of mental disorders (Kessler et al., 2007; Kessler et al., 2005) and are highly co-morbid with mood disorders (Kaufman and Charney, 2000). Anxiety in children and college students has increased almost one standard deviation from the 1950’s to the 1990’s (Twenge, 2000) with a cohort effect for increased lifetime risk in most countries surveyed (Kessler et al., 2007). The alarming trend of an overall deterioration of mental health supports, and may partially mediate, the possibility of rising rates of depression.
Cross-cultural studies illuminate potential contributing factors. Given the relationship between health, socioeconomic status and depression (Adler et al., 1994), it seems counterintuitive that the most modernized countries, using gross domestic product (GDP) per capita as a quantitative measure of modernization, tend to have higher rates of depression (see Figure 1) (IMF, 2010; Kessler et al., 2007). There are several limitations to this observation. First, national estimates of depression prevalence are inversely proportional to the average impairment associated with depression, which may reflect varying diagnostic thresholds (Chang et al., 2008; Simon et al., 2002), though this bias has not been consistently replicated (Kessler et al., 2009). And second, GDP per capita is a crude measure of modernization that cannot adequately account for large differences in depression rates between ostensibly equally modernized societies. Japan, as one of the most technologically advanced countries, serves as an illustrative exception to this trend. Its exceedingly low prevalence of obesity (OECD, 2010) and high consumption of seafood products, which are rich in long-chain ω-3 polyunsaturated fatty acids (PUFA), may contribute to this phenomenon (Hibbeln, 1998). The Japanese also exhibit a relatively low degree of inequality for a highly modern, capitalistic society (Davies et al., 2008). Cultural emphasis on collectivism, as opposed to individualism (Kitayama et al., 1997; Oyserman et al., 2002), may also add to a social environment protective against the development of depression.
Figure 1.
A correlation between lifetime risk of a mood disorder and gross domestic product (GDP) per capita trended toward statistical significance (IMF, 2010; Kessler et al., 2007).
A correlation between depression and modernization predicts a very low prevalence among hunter-gatherers. Community-based investigations of mental disorders using cross-culturally valid diagnostic tools among traditional populations are needed to assess this possibility. There is scant evidence that depression is rare among people living close to the human EEA, e.g. the Kaluli of New Guinea (Schieffelin, 1986), the Thai-Lao of Thailand (Keyes, 1986), and the Toraja of Indonesia (Hollan and Wellenkamp, 1994; Hollan and Wellenkamp, 1996). The rare case studies of depression reported by anthropologists should be interpreted with extreme caution since there was no systematic community sampling, nor formal diagnostic instruments used. Departure from a hunter-gatherer living is an opportune window for insight into the effects of modernization. The Ik of Uganda purportedly become more depressed upon shifting from hunter-gather to agricultural practices (Stevens and Price, 2000). After indigenous circumpolar peoples rapidly modernized, there was a rampant incidence of diabetes and suicide rates tripled within a decade (Shephard and Rode, 1996).
Other lines of evidence suggest modernization is associated with depression. Indexing modernization by measures of belief in magic, hunting, gathering, agriculture, and technological complexity, a cross-cultural analysis of community women in rural Nigeria, urban Nigeria, rural Canada, and urban U.S. found the degree of modernization to correlate with a higher prevalence of depression in a dose-dependent manner (Colla et al., 2006). Adoption of the American lifestyle appears to explain higher rates of depression in Mexican Americans born in the U.S. compared to Mexican immigrants (Vega et al., 2004). As metropolitan China has undergone rapid cultural transformation over recent decades, the risk of suffering from depression appears to have risen dramatically: in a retrospective study, Chinese born after 1966 were calculated to be 22.4 times more likely to suffer from a depressive episode during their lifetime compared to those born earlier than 1937 (Lee et al., 2007). In developed countries, urban dwellers have a higher prevalence of psychiatric disorders, and specifically mood and anxiety disorders, compared to rural counterparts (Peen et al., 2010). British households rated as more traditional, e.g. church-going, have lower rates of depression (Brown and Prudo, 1981). In an investigation of affective disorder prevalence among the Amish, a community that maintains a traditional agrarian culture with notable unity and social connectedness, the prevalence of MDD was found to equal that of bipolar disorder- about 1% (Egeland and Hostetter, 1983). The above evidence suggests higher depression prevalence and risk is associated with general aspects of modernization.
Key environmental changes
If modernization correlates with an increased risk of depression, then what are the specific components of modern, western culture contributing to this phenomenon? A decline in physical well-being is a prime suspect. Disease-promoting changes in modern daily living include growing waistlines in relation to poor diet and physical inactivity, as well as endocrine dysfunction from inadequate sunlight exposure and sleep. A toxic social environment characterized by increasing competition, inequality, and social isolation may also contribute to a depressiogenic milieu. Each of these aspects of the contemporary environment is associated with diseases of modernity and affects depression incidence and treatment.
Obesity
Obesity is the quintessential disease of modernity. Throughout human history, and indeed life itself, heretofore the struggle has been to procure, store, and conserve energy. Constraints on food intake had, until recently, been environmentally imposed. As a result, individuals in modern societies continually store excess energy as their bodies prepare for a famine that never arrives. Deteriorating health of modern populations via the obesity epidemic (Flegal et al., 2010) is a likely contributing factor to a rising prevalence of depression. Compared to normal-weight peers, obese individuals are at an increased risk of diseases of modernity and their associated health complications (Must et al., 1999), as well as a lower quality of life (Heo et al., 2003). A systematic review of prospective studies found a reciprocal cause-and-effect relationship between obesity/overweight and depression: i.e. obese individuals had a 55% increased risk of developing depression compared to those of normal weight at follow-up, and depressed individuals were 58% more likely to become obese than those not depressed (Luppino et al., 2010). Gender, degree of obesity, socioeconomic status, and other moderating variables complicate this relationship (Atlantis and Baker, 2008; Stunkard et al., 2003).
There are several mechanistic explanations for the association between obesity and depression. First, the decrements in physical health likely increase the risk of depression, since physical well-being is a powerful determinant of emotional well-being (Nesse, 2004). Indeed, there is a high degree of co-morbidity between depression and obesity-related chronic diseases (Moussavi et al., 2007; Stegmann et al., 2010). The physiologic profile of obesity per se may directly contribute to symptoms of depression, as obesity has been characterized as a state of mild, chronic inflammation (Shoelson et al., 2007) and inflammatory signaling has been implicated in the pathogenesis of depression (Raison et al., 2006; Raison et al., 2010). Poor body image in relation to overweight status is associated with psychological distress (Atlantis and Ball, 2007). The western cultural value of individualism may exacerbate this distress via attributing weight status more to personal control and responsibility than external factors. Antidepressant medications may contribute to the weight-gain observed in those suffering from depression (Fava, 2000). The symptoms of MDD, e.g. reduced motor activity, motivation, or changes in appetite, may also be important contributors to weight gain. And lastly, the same lifestyle factors that fuel the development of obesity, e.g. diet and exercise, also contribute to depression- a concept that will be further discussed.
Diet
The composition of the typical Western diet has been implicated as directly contributing to the incidence of obesity and chronic diseases via its alteration of metabolic and endocrine function (Cordain et al., 2005; Eaton et al., 2010; Pollan, 2008). The seven characteristics of the western diet identified are “1) glycemic load, 2) fatty acid composition, 3) macronutrient composition, 4) micronutrient density, 5) acid-base balance, 6) sodium-potassium ratio, and 7) fiber content” (Cordain et al., 2005). While each of these components individually affect health, research suggests a general dietary pattern often has greater health effects than the sum of its nutrient composition (Jacobs et al., 2009; Jacobs and Steffen, 2003). This observation has been attributed to a synergism of nutrients in their natural form and to dietary habits conferring other health benefits that are difficult to account and control for. The Mediterranean diet is one traditional dietary pattern validated in population-based and intervention studies to improve physical health and quality of life (Muñoz et al., 2008; Serra Majem et al., 2006; Sofi, 2009). In fact, a large prospective study found adherence to the Mediterranean diet was protective against the self-reported development of depression (Sánchez-Villegas et al., 2009).
Carbohydrates may contribute to depression. The obesity epidemic and possible increase in depression prevalence coincided with a population-wide increase in the percentage of energy from carbohydrates and a relative decrease in % fat and protein (Briefel, 2004). Depressed individuals tend to consume more carbohydrates, specifically in the form of simple sugar (Christensen, 1996). There is increasing interest in high-protein, low-carbohydrate diets for weight-loss and weight maintenance (Hession et al., 2009; Larsen et al., 2010; Stern, 2004). Optimal macronutrient intake for depression prevention and treatment remains unclear.
There is substantial evidence to support the influence of individual nutrients on mental health. The strongest evidence exists for ω-3 PUFA, whose clinical significance is an active area of research in the fields of child development, cancer, cardiovascular disease, and mental illness (Riediger et al., 2009). The relationship between ω-3 PUFA and depression has been extensively reviewed (Bodnar and Wisner, 2005; Freeman, 2009; Hibbeln, 1998; Ross et al., 2007). The anti-inflammatory effects of ω-3 PUFA (Calder, 2006) may mediate this relationship. Reviews of double-blind placebo-controlled trials have concluded that supplementation appears to reduce depressive symptoms and should be further investigated as a potential adjunctive therapy for MDD (Freeman, 2009; Ross et al., 2007).
Marginal deficiencies of specific micronutrients encountered in the typical Western diet may influence depression in the general population. There is moderate support for the role of folate in the prevention and treatment of depression and more speculative evidence for vitamins B12, C, E, selenium, iron, and zinc (Alpert and Fava, 1997; Bodnar and Wisner, 2005). Diet may be a particularly important mediator of higher risk of depression among individuals at low socioeconomic status (Everson et al., 2002; Hirschfeld and Cross, 1982) since poor nutrition and obesity disproportionately affect this vulnerable population (Everson et al., 2002; Wang and Beydoun, 2007).
Physical Activity
Human bodies have been shaped by natural selection to engage in much higher rates of physical activity than current levels in modern society. The estimated average daily energy expenditure of hunter-gatherers is about 3,000 kcal (Eaton et al., 1997). The reduction in energy expenditure in the US adult population during the past century is calculated to have mainly occurred between 1910 and 1970, and had leveled off by about 1980 (Cutler et al., 2003). Surveys in the US reveal that less than half of adults engage in the recommended amount of physical activity with 37.6% considered “completely inactive” (CDC, 2010). Physical activity has unequivocal health benefits for the prevention and treatment of chronic disease (Warburton et al., 2006). In the general population, exercise correlates with a reduced risk of depression and sedentary behavior with a higher risk (Teychenne et al., 2010). Exercise appears to reduce depressive symptoms (Dunn and Dishman, 1991) and does so in a dose-dependent manner (Dunn et al., 2005). Aerobic exercise has shown to be as effective a treatment as a standard antidepressant (sertraline) for MDD (Blumenthal et al., 2007), with those in the aerobic exercise arm of the study exhibiting a lower rate of relapse (Babyak et al., 2000).
Light and Sleep
Decreased exposure to bright light and circadian dysregulation are the proximate cause of seasonal affective disorder (SAD). Proper endocrine function and increased dopamine and serotonin release are the presumed mechanisms by which light therapy alleviates SAD and MDD (Golden et al., 2005; Lambert et al., 2002; Tuunainen et al., 2004). While there is little systematic documentation of changes in light exposure patterns in the general population, direct sunlight exposure has likely decreased during the past century as a greater percentage of jobs have moved indoors and public health campaigns have disseminated the association between sunlight exposure and skin cancer. Current light exposure patterns in modern society have been blamed for widespread circadian dysfunction in the general population (Pauley, 2004). As an extreme example, long-term shift workers exhibit severe circadian dysfunction and are at an increased risk of chronic diseases, e.g. metabolic syndrome, diabetes mellitus type 2 (Knutsson, 2003; Reddy and O’Neill, 2010), though their relative risk of depression remains unknown. Inadequate sunlight exposure is the principal cause of the modern epidemic of vitamin D deficiency, which has well-documented associations with diseases of modernity (Holick, 2005). MDD has been associated with low vitamin D levels (Hoogendijk et al., 2008) and its role in depression deserves further research (Bertone-Johnson, 2009).
The profound changes in sleep patterns during the past century may further contribute to an increased risk of depression via altered circadian rhythmicity. The National Sleep Foundation recommends 7–9 hours of sleep per night. The average American adult slept about 8 hours in 1960 (Kripke et al., 1979), but now sleeps 6 hrs and 40 minutes on weekdays and 7 hrs and 7 minutes on weekends (NSF, 2009). One third of the US population exhibits at least one symptom of insomnia, with 6% fully meeting the DSM-IV diagnostic criteria (Ohayon, 2002). Less sleep is associated with decrements in physical health, including development of obesity in children and young adults (Nielsen et al., 2010). Acute sleep deprivation decreases glucose tolerance and causes endocrine dysfunction similar to that seen in obesity-related chronic diseases (Spiegel et al., 1999). Reduced amount and/or quality of sleep are not only cardinal symptoms, but also predictors of major depressive disorder. Prospective studies reveal that insomnia doubles the risk of developing depression (Baglioni et al., 2011), and interventions solely directed toward treating comorbid insomnia significantly alleviate MDD (Manber et al., 2008).
Social Environment
I see no hope for the future of our people if they are dependent on the frivolous youth of today, for certainly all youth are reckless beyond words.
-Hesiod, 8th century B.C.
I may indicate briefly what to me constitutes the essence of the crisis in our time. It concerns the relationship of the individual to society… [His] position in society is such that the egotistical drives of his make-up are constantly being accentuated, while his social drives, which are by nature weaker, progressively deteriorate. All human beings, whatever their position in society, are suffering from this process of deterioration. Unknowingly prisoners of their own egotism, they feel insecure, lonely, and deprived of the naive, simple and unsophisticated enjoyment of life. Man can find meaning in life, short and perilous as it is, only through devoting himself to society. The economic anarchy of capitalist society as it exists today is, in my opinion, the real source of evil.
-Albert Einstein, 1949
There seems to exist a human tendency to view current events and social trends as evidence of society’s downfall, but could it actually be happening now? Accumulating evidence indicates that the social environment in modern-industrialized countries, especially in the United States, has become increasingly competitive, threatening, and socially isolating. Increased competition is most obvious in college admissions (Bound et al., 2009) and economically, as workers now compete for jobs on a global scale (Friedman, 2007). Contemporary populations may now be more susceptible to depression because of greater inequality, low social support, intense individual competitiveness, and increased social failure (Gilbert, 2006). Onset of a major depressive episode often coincides with stressful life events (Kendler et al., 1999; Nesse, 2000). The modern social milieu could contribute to rising rates of depression via higher frequency and/or severity of adversity. Many have posited that capitalist values have directly contributed to a decline in social well-being and an increase in psychopathology throughout the western world (Kasser et al., 2007; Putnam, 1995; Walsh, 2011). The high degree of self-determination, at least perceived or expected, in current western societies might affect depression rates; freedom is certainly laudable, but it appears to be a double-edged sword, as excessive choice can lead to paralytic indecision, greater expectations, stress, and eventual dissatisfaction, blame, and regret (Schwartz, 2000). A rise in psychopathology among young adults has been attributed to a shifting cultural emphasis away from intrinsic goals, e.g. social relationships, community, and competence, to extrinsic goals, like money, status, and appearance (Twenge et al., 2010). Similarly, an increase in anxiety among children and college students was preceded by or coincided with measures of lower social connectedness and higher social threat (Twenge, 2000).
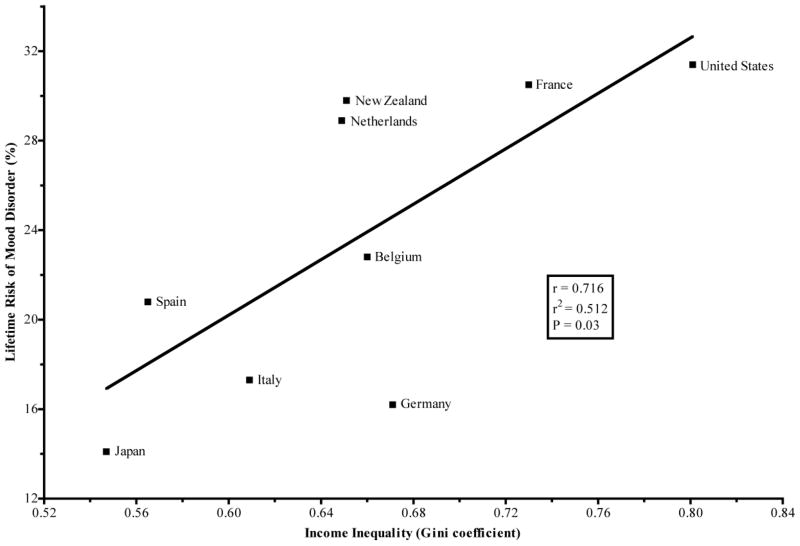
Inequality is another caustic factor of the modern social environment. There is a trend of higher lifetime risk of a mood disorder and a country’s Gini coefficient (a measure of income inequality ranging from 0–1, 1 being the most unequal) when using data from all countries in the World Mental Health survey initiative (p=0.09) (Davies et al., 2008; Kessler et al., 2007). This correlation became statistically significant (p=0.03) when restricting the analysis to developed countries (see Figure 2) (Davies et al., 2008; Kessler et al., 2007). Inequality has risen in modernized countries, and unequal societies tend to have lower overall health and higher levels of social distrust, competition, and status anxiety (Wilkinson et al., 2009; Wilkinson and Pickett, 2006).
Figure 2.
A population’s lifetime risk of a mood disorder is correlated with income inequality in developed countries (Davies et al., 2008; Kessler et al., 2007).
In 1985, the General Social Survey found that the mean and mode for number of confidants, people with whom one can comfortably discuss important issues, were both 3 and 3. In 2004, a repeat of the survey revealed that the mean and mode had respectively dropped to 2 and 0 (McPherson et al., 2006). This trend toward isolation is alarming as loneliness appears to spread through social networks as a contagious process with a positive-feedback loop in which people with fewer friends become increasingly isolated and lonely over time (Cacioppo et al., 2009). Most consider the current social environment of western societies to be a gross deviation from the human EEA, as anthropologists report stronger social cohesion and a near-total absence of time spent alone in traditional foraging societies (Gat, 1999). The extensive risk for physical and mental morbidity, e.g. anxiety, inflammation-related chronic diseases, etc., from social isolation offers support for an environmental mismatch (Cacioppo et al., 2009). Increased geographic mobility may be an important contributing factor to loneliness in modern society, because relocation disrupts social networks, increases stress and family conflicts, and increases the risk of developing depression, at least in women (Weissman and Paykel, 1972). A move toward secularization of modern populations should also be considered, as religious activity is correlated with lower risk of depression and more social support (Koenig and Larson, 2001). Technology may be contributing to an increased risk of depression in a variety of ways (Turkle, 2011). Internet use has been correlated with less family communication, smaller social circles, more depressive symptoms and greater feelings of loneliness (Kraut et al., 1998). Social support confers protection against depression, whereas weak social support exacerbates one’s vulnerability (Egeland and Hostetter, 1983; Prince et al., 1998; Prudo et al., 1984). Interpersonal therapy, which focuses on improving social connectedness with family and friends, is an effective treatment for depression and reduces the risk of relapse (de Mello et al., 2005). In conclusion, the modern social environment is more competitive, inequitable, and lonely. This deterioration of social cohesion among modern-industrialized populations may be a central component to rising rates of depression.
Future directions and implications
This review evaluates the evidence for rising rates of depression as well as specific factors contributing to a possible increase. One may only speculate on depression rates in centuries past. Available epidemiologic evidence equivocally suggests that prevalence has risen over the past century, especially in recent decades, with younger cohorts exhibiting an earlier age-of-onset and increased lifetime risk. Parallel lines of evidence indicate that modernization is generally associated with higher rates of depression. The obesity epidemic and its underlying drivers of poor diet and sedentary lifestyle appear to directly and indirectly contribute to an increased risk. Sunlight and sleep deprivation characteristic of modern-day living are also candidate mediators of rising rates chronic disease and depression. Greater competition, inequality, and loneliness are the principal factors of the modern, western social environment blamed for rising rates of psychopathology, including depression. Put another way, the modern man would likely be much more resilient to the toils of living if he were physically fit, well-rested, free of chronic disease and financial stress, surrounded by close family and friends, and felt pride in his meaningful work. The temporal, cultural, and mechanistic evidence presented here prompt consideration for depression as a disease of modernity. A recent review corroborates this conclusion by offering a parallel evolutionary hypothesis for increasing rates: inappropriate inflammation arising from the loss of ancient relationships with microorganisms in modern environments may be contributing to a reduced ability to cope with psychosocial adversity (Raison et al., 2010).
Robert Burton presciently implicated the quality and quantity of diet, heredity, solitude, idleness, sleep, loss/sorrow, fear, shame, envy, malice, ambition, vanity, excessive study[!], and poverty as causes of melancholy over 350 years ago (Burton, 1845). There has been much progress, but countless questions circling the concept of depression and its origins still remain unanswered. A better understanding of large-scale causes and the complex relationships between modern culture, chronic disease, and depression will be essential for systemic, population-based interventions to address a very common affliction. More research is necessary to unravel the role of specific health behaviors within individual depressive phenotypes, e.g. atypical versus melancholic depression. Do somatic depressive symptoms associate more with health status and non-somatic symptoms with the social milieu? How do these lifestyle factors differentially affect risk by age and gender? How do subcutaneous versus visceral adipose tissues influence the relationship between obesity and depression? Current exposure patterns to environmental toxins, especially endocrine-disrupting chemicals, are alarming (Diamanti-Kandarakis et al., 2009; Welshons et al., 2003) and their role in influencing risk of chronic diseases and depression deserves investigation. It will be interesting to see how the story of microbiota and inflammation in the pathogenesis of depression unfolds (Raison et al., 2010). With technology and social structures mutating faster than ever, measuring and monitoring the effects of these hyperbolic changes on mental health will be important.
This review has several implications for clinical practice and public policy. First, health behavior interventions have untapped potential to reduce suffering related to depression, especially considering that they are relatively inexpensive, safe, sustainable, and benefit overall health (Walsh, 2011). Second, policy interventions to reverse the obesity epidemic may be essential to curb depression in the general population. Taxation, subsidization, and regulatory policies should help make healthy choices the easy choice. Many suggested interventions to combat obesity would not only reduce human suffering, but would be cost-saving (Gortmaker et al., 2011; Swinburn et al., 2011). As an example, urban sprawl is associated with less walking, more time spent in cars, and likelihood of obesity (Ewing et al., 2008; Frank et al., 2004). Urban development and public policies that prioritize public transportation, land use mix, safe recreation space, and foster walking and cycling would likely benefit both human and environmental health. And third, the data relating inequality to worse physical and mental health suggest consideration of taxation policies toward a more equitable distribution of wealth. While these proposed public initiatives would face intense opposition from parties with vested interests in maintaining the status quo, government-led systemic intervention may be our best hope to gain control of this public health crisis.
More money does not lead to more happiness. By appealing to evolutionary proclivities, like a desire for energy-dense food and status competition, the economic and marketing forces of modern society have engineered an environment promoting decisions that maximize consumption at the long-term cost of well-being. In effect, humans have dragged a body with a long hominid history into an overfed, malnourished, sedentary, sunlight-deficient, sleep-deprived, competitive, inequitable, and socially-isolating environment with dire consequences. Hopefully, this theoretical framework will aid in the understanding, prevention, and treatment of depression and other diseases of modernity at the clinical and population level.
Acknowledgments
Funding body agreements and policies
The project was supported by grant number P20 RR016475 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH).
I express deep gratitude toward Stephen Ilardi for his mentorship, guidance, and initial encouragement to write this review. I am indebted to my friends and colleagues who reviewed earlier drafts- Ann Davis, Scott Hawley, Ann Manzardo, Marlies Ozias, Kristina Bridges, and Leigh Wagner. I also thank the anonymous reviewers of the present manuscript and its previous iterations. Any errors are my responsibility.
Acronyms
- EEA
environment of evolutionary adaptedness
- MDD
major depressive disorder
- NCS
National Comorbidity Survey
- NCS-R
National Comorbidity Survey Replication
- MMPI
Minnesota Multiphasic Personality Inventory
- GDP
gross domestic product
- PUFA
polyunsaturated fatty acids
- SAD
Seasonal Affective Disorder
Footnotes
Contributors
Dr. Stephen Ilardi encouraged Mr. Hidaka to write a literature review and guided him toward relevant areas of study. Mr. Hidaka searched and analyzed the literature, did the statistical analyses, and wrote the manuscript. He is the sole contributing author. Colleagues recognized in Acknowledgements offered editorial comments at Mr. Hidaka’s request.
Conflicts of Interest
The author has no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adler N, Boyce T, Chesney M, Cohen S, Folkman S, Kahn R, Syme S. Socioeconomic status and health. American Psychologist. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Alpert JE, Fava M. Nutrition and depression: the role of folate. Nutrition Reviews. 1997;55:145–149. doi: 10.1111/j.1753-4887.1997.tb06468.x. [DOI] [PubMed] [Google Scholar]
- Andrade L, Caraveo anduaga J, Berglund P, Bijl R, Graaf R, Vollebergh W, Dragomirecka E, Kohn R, Keller M, Kessler R. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. International Journal of Methods in Psychiatric Research. 2003;12:3–21. doi: 10.1002/mpr.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atlantis E, Baker M. Obesity effects on depression: systematic review of epidemiological studies. Int J Obes. 2008;32:881–891. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- Atlantis E, Ball K. Association between weight perception and psychological distress. International journal of obesity. 2007;32:715–721. doi: 10.1038/sj.ijo.0803762. [DOI] [PubMed] [Google Scholar]
- Babyak M, Blumenthal JA, Herman S, Khatri P, Doraiswamy M, Moore K, Craighead WE, Baldewicz TT, Krishnan KR. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62:633–638. doi: 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, Riemann D. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. Journal of affective disorders. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Barkow JH, Cosmides L, Tooby J. The Adapted mind: evolutionary psychology and the generation of culture. Oxford University Press; New York: 1992. [Google Scholar]
- Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287:2570–2581. doi: 10.1001/jama.287.19.2570. [DOI] [PubMed] [Google Scholar]
- Bertone-Johnson ER. Vitamin D and the occurrence of depression: causal association or circumstantial evidence? Nutr Rev. 2009;67:481–492. doi: 10.1111/j.1753-4887.2009.00220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, Herman S, Craighead WE, Brosse AL, Waugh R, Hinderliter A, Sherwood A. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med. 2007;69:587–596. doi: 10.1097/PSY.0b013e318148c19a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodnar LM, Wisner KL. Nutrition and depression: implications for improving mental health among childbearing-aged women. Biological Psychiatry. 2005;58:679–685. doi: 10.1016/j.biopsych.2005.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bound J, Hershbein B, Long BT. Playing the admissions game: student reactions to increasing college competition. National Bureau of Economic Research Cambridge; Mass., USA: 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briefel RR. Secular trends in dietary intake in the United States. Annual review of nutrition. 2004;24:401–431. doi: 10.1146/annurev.nutr.23.011702.073349. [DOI] [PubMed] [Google Scholar]
- Bromet EJ, Dunn LO, Connell MM, Dew MA, Schulberg HC. Long-term reliability of diagnosing lifetime major depression in a community sample. Arch Gen Psychiatry. 1986;43:435–440. doi: 10.1001/archpsyc.1986.01800050033004. [DOI] [PubMed] [Google Scholar]
- Brown GW, Prudo R. Psychiatric disorder in a rural and an urban population: 1. Aetiology of depression. Psychol Med. 1981;11:581–599. doi: 10.1017/s0033291700052880. [DOI] [PubMed] [Google Scholar]
- Burton R. The Anatomy of Melancholy. Bradbury and Evans, Printers; Whitefriars, London: 1845. [Google Scholar]
- Cacioppo J, Fowler J, Christakis N. Alone in the crowd: The structure and spread of loneliness in a large social network. Journal of personality and social psychology. 2009;97:977. doi: 10.1037/a0016076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calder PC. n-3 Polyunsaturated fatty acids, inflammation, and inflammatory diseases. The American journal of clinical nutrition. 2006;83:S1505–1519S. doi: 10.1093/ajcn/83.6.1505S. [DOI] [PubMed] [Google Scholar]
- CDC. National Health and Nutrition Examination Survey. 2010. [Google Scholar]
- Chang S, Hahm B, Lee J, Shin M, Jeon H, Hong J, Lee H, Lee D, Cho M. Cross-national difference in the prevalence of depression caused by the diagnostic threshold. Journal of affective disorders. 2008;106:159–167. doi: 10.1016/j.jad.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Christensen L. Nutrition and depression. Diet–behavior relationships: Focus on depression. American Psychological Association; 1996. pp. 89–108. [Google Scholar]
- Colla J, Buka S, Harrington D, Murphy JM. Depression and modernization: a cross-cultural study of women. Soc Psychiatry Psychiatr Epidemiol. 2006;41:271–279. doi: 10.1007/s00127-006-0032-8. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991–1992 and 2001–2002. Am J Psychiatry. 2006;163:2141–2147. doi: 10.1176/ajp.2006.163.12.2141. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Drug Abuse and Dependence in the United States: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, O’Keefe JH, Brand-Miller J. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr. 2005;81:341–354. doi: 10.1093/ajcn.81.2.341. [DOI] [PubMed] [Google Scholar]
- Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D, Glaeser E, Shapiro J. Why have Americans become more obese? The Journal of Economic Perspectives. 2003;17:93–118. [Google Scholar]
- Davies JB, Sandstrom S, Shorrocks AF, Wolff EN. The world distribution of household wealth. United nations university. World institute for development economics research (UNU-WIDER); 2008. [Google Scholar]
- de Mello MF, de Jesus Mari J, Bacaltchuk J, Verdeli H, Neugebauer R. A systematic review of research findings on the efficacy of interpersonal therapy for depressive disorders. Eur Arch Psychiatry Clin Neurosci. 2005;255:75–82. doi: 10.1007/s00406-004-0542-x. [DOI] [PubMed] [Google Scholar]
- Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM, Zoeller RT, Gore AC. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocrine reviews. 2009;30:293–342. doi: 10.1210/er.2009-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn AL, Dishman RK. Exercise and the neurobiology of depression. Exerc Sport Sci Rev. 1991;19:41–98. [PubMed] [Google Scholar]
- Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28:1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Eaton SB, Eaton SB, 3rd, Konner MJ. Paleolithic nutrition revisited: a twelve-year retrospective on its nature and implications. Eur J Clin Nutr. 1997;51:207–216. doi: 10.1038/sj.ejcn.1600389. [DOI] [PubMed] [Google Scholar]
- Eaton SB, III, SBE . Hunter-gatherers and human health. In: Lee RB, Daly R, editors. The Cambridge Encyclopedia Hunters and Gatherers. Cambridge University Press; United Kingdom: 2004. pp. 449–456. [Google Scholar]
- Eaton SB, Konner MJ, Cordain L. Diet-dependent acid load, Paleolithic [corrected] nutrition, and evolutionary health promotion. Am J Clin Nutr. 2010;91:295–297. doi: 10.3945/ajcn.2009.29058. [DOI] [PubMed] [Google Scholar]
- Eaton SB, Strassman BI, Nesse RM, Neel JV, Ewald PW, Williams GC, Weder AB, Eaton SB, 3rd, Lindeberg S, Konner MJ, Mysterud I, Cordain L. Evolutionary health promotion. Prev Med. 2002;34:109–118. doi: 10.1006/pmed.2001.0876. [DOI] [PubMed] [Google Scholar]
- Egeland JA, Hostetter AM. Amish Study, I: Affective disorders among the Amish, 1976–1980. Am J Psychiatry. 1983;140:56–61. doi: 10.1176/ajp.140.1.56. [DOI] [PubMed] [Google Scholar]
- Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. Journal of Psychosomatic Research. 2002;53:891–895. doi: 10.1016/s0022-3999(02)00303-3. [DOI] [PubMed] [Google Scholar]
- Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Urban Ecology. 2008:567–582. doi: 10.4278/0890-1171-18.1.47. [DOI] [PubMed] [Google Scholar]
- Fava M. Weight gain and antidepressants. Physicians Postgraduate Press; 2000. pp. 37–41. [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. American journal of preventive medicine. 2004;27:87–96. doi: 10.1016/j.amepre.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Freeman MP. Omega-3 fatty acids in major depressive disorder. J Clin Psychiatry. 2009;70(Suppl 5):7–11. doi: 10.4088/JCP.8157su1c.02. [DOI] [PubMed] [Google Scholar]
- Friedman TL. The world is flat: A brief history of the twenty-first century. Picador USA: 2007. [Google Scholar]
- Gat A. Social organization, group conflict and the demise of Neanderthals= Organisation sociale, conflit de groupe et la mort de NÈandertal. Mankind quarterly. 1999;39:437–454. [Google Scholar]
- Gilbert P. Evolution and depression: issues and implications. Psychol Med. 2006;36:287–297. doi: 10.1017/S0033291705006112. [DOI] [PubMed] [Google Scholar]
- Golden RN, Gaynes BN, Ekstrom RD, Hamer RM, Jacobsen FM, Suppes T, Wisner KL, Nemeroff CB. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. 2005;162:656–662. doi: 10.1176/appi.ajp.162.4.656. [DOI] [PubMed] [Google Scholar]
- Gortmaker SL, Swinburn BA, Levy D, Carter R, Mabry PL, Finegood DT, Huang T, Marsh T, Moodie ML. Changing the future of obesity: science, policy, and action. The Lancet. 2011;378:838–847. doi: 10.1016/S0140-6736(11)60815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagnell O. Repeated incidence and prevalence studies of mental disorders in a total population followed during 25 years. The Lundby Study, Sweden. Acta Psychiatr Scand. 1989;(Suppl 348):61–77. doi: 10.1111/j.1600-0447.1989.tb05216.x. discussion 167–178. [DOI] [PubMed] [Google Scholar]
- Hagnell O, Ojesjo L, Otterbeck L, Rorsman B. Prevalence of mental disorders, personality traits and mental complaints in the Lundby Study. A point prevalence study of the 1957 Lundby cohort of 2,612 inhabitants of a geographically defined area who were re-examined in 1972 regardless of domicile. Scand J Soc Med Suppl. 1994;50:1–77. [PubMed] [Google Scholar]
- Heo M, Allison DB, Faith MS, Zhu S, Fontaine KR. Obesity and quality of life: mediating effects of pain and comorbidities. Obes Res. 2003;11:209–216. doi: 10.1038/oby.2003.33. [DOI] [PubMed] [Google Scholar]
- Hession M, Rolland C, Kulkarni U, Wise A, Broom J. Systematic review of randomized controlled trials of low-carbohydrate vs. low-fat/low-calorie diets in the management of obesity and its comorbidities. Obesity Reviews. 2009;10:36–50. doi: 10.1111/j.1467-789X.2008.00518.x. [DOI] [PubMed] [Google Scholar]
- Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351:1213. doi: 10.1016/S0140-6736(05)79168-6. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA, Cross CK. Epidemiology of Affective Disorders: Psychosocial Risk Factors. Arch Gen Psychiatry. 1982;39:35–46. doi: 10.1001/archpsyc.1982.04290010013003. [DOI] [PubMed] [Google Scholar]
- Holick MF. The vitamin D epidemic and its health consequences. J Nutr. 2005;135:2739S–2748S. doi: 10.1093/jn/135.11.2739S. [DOI] [PubMed] [Google Scholar]
- Hollan DW, Wellenkamp JC. Contentment and suffering: Culture and experience in Toraja. Columbia Univ Pr; 1994. [Google Scholar]
- Hollan DW, Wellenkamp JC. The Thread of Life: Toraja Reflections on the Life Cycle. University of Hawai’i Press; Honolulu: 1996. [Google Scholar]
- Hoogendijk WJ, Lips P, Dik MG, Deeg DJ, Beekman AT, Penninx BW. Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Arch Gen Psychiatry. 2008;65:508–512. doi: 10.1001/archpsyc.65.5.508. [DOI] [PubMed] [Google Scholar]
- Horwitz A, Wakefield J. The loss of sadness: How psychiatry transformed normal sorrow into depressive disorder. Oxford University Press; USA: 2007. [DOI] [PubMed] [Google Scholar]
- IMF. World Economic Outlook Database-April 2010. International Monetary Fund; 2010. [Google Scholar]
- Irons W. Adaptively relevant environments versus the environment of evolutionary adaptedness. Evol Anthropol. 1998;6:194–204. [Google Scholar]
- Jackson SW. Melancholia and depression: From hippocratic times to modern times. Yale University Press; 1986. [Google Scholar]
- Jacobs DR, Gross MD, Tapsell LC. Food synergy: an operational concept for understanding nutrition. The American journal of clinical nutrition. 2009;89:1543S–1548S. doi: 10.3945/ajcn.2009.26736B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs DR, Steffen LM. Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. The American journal of clinical nutrition. 2003;78:508S. doi: 10.1093/ajcn/78.3.508S. [DOI] [PubMed] [Google Scholar]
- Kasser T, Cohn S, Kanner A, Ryan R. Some costs of American corporate capitalism: A psychological exploration of value and goal conflicts. Psychological Inquiry. 2007;18:1–22. [Google Scholar]
- Kaufman J, Charney D. Comorbidity of mood and anxiety disorders. Depression and Anxiety. 2000;12:69–76. doi: 10.1002/1520-6394(2000)12:1+<69::AID-DA9>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Kendler K, Karkowski L, Prescott C. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156:837. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kessler R, Aguilar-gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, Üstün T, Wang P. Special Articles The global burden of mental disorders: An update from the WHO World Mental Health (WMH) Surveys. Epidemiologia e psichiatria sociale. 2009;18:23. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Berglund P, Demler O, Jin R, Koretz D, Merikangas K, Rush A, Walters E, Wang P. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler R, Nelson C, McGonagle K, Liu J, Swartz M, Blazer D. Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. The British journal of psychiatry. 1996;(Supplement):17. [PubMed] [Google Scholar]
- Kessler RC, Angermeyer M, Anthony JC, RDEG, Demyttenaere K, Gasquet I, GDEG, Gluzman S, Gureje O, Haro JM, Kawakami N, Karam A, Levinson D, Medina Mora ME, Oakley Browne MA, Posada-Villa J, Stein DJ, Adley Tsang CH, Aguilar-Gaxiola S, Alonso J, Lee S, Heeringa S, Pennell BE, Berglund P, Gruber MJ, Petukhova M, Chatterji S, Ustun TB. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-Month Prevalence of DSM-III-R Psychiatric Disorders in the United States: Results From the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Keyes CF. The interpretive basis of depression. In: Kleinman AM, Good B, editors. Culture and depression: Studies in the anthropology and cross-cultural psychiatry of affect and disorder. University of California Press; 1986. pp. 153–174. [Google Scholar]
- Kitayama S, Markus HR, Matsumoto H, Norasakkunkit V. Individual and collective processes in the construction of the self: Self-enhancement in the United States and self-criticism in Japan. Journal of personality and social psychology. 1997;72:1245. doi: 10.1037//0022-3514.72.6.1245. [DOI] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM. Increasing Rates of Depression. JAMA: The Journal of the American Medical Association. 1989;261:2229–2235. [PubMed] [Google Scholar]
- Knutsson A. Health disorders of shift workers. Occupational Medicine. 2003;53:103–108. doi: 10.1093/occmed/kqg048. [DOI] [PubMed] [Google Scholar]
- Koenig HG, Larson DB. Religion and mental health: Evidence for an association. International Review of Psychiatry; 2001. [Google Scholar]
- Kraut R, Patterson M, Lundmark V, Kiesler S, Mukophadhyay T, Scherlis W. Internet paradox: A social technology that reduces social involvement and psychological well-being? American Psychologist. 1998;53:1017. doi: 10.1037//0003-066x.53.9.1017. [DOI] [PubMed] [Google Scholar]
- Kripke D, Simons R, Garfinkel L, Hammond E. Short and long sleep and sleeping pills: Is increased mortality associated? Archives of General Psychiatry. 1979;36:103. doi: 10.1001/archpsyc.1979.01780010109014. [DOI] [PubMed] [Google Scholar]
- Lambert GW, Reid C, Kaye DM, Jennings GL, Esler MD. Effect of sunlight and season on serotonin turnover in the brain. Lancet. 2002;360:1840–1842. doi: 10.1016/s0140-6736(02)11737-5. [DOI] [PubMed] [Google Scholar]
- Larsen TM, Dalskov SM, van Baak M, Jebb SA, Papadaki A, Pfeiffer AFH, Martinez JA, Handjieva-Darlenska T, Kunešová M, Pihlsgård M. Diets with high or low protein content and glycemic index for weight-loss maintenance. New England Journal of Medicine. 2010;363:2102–2113. doi: 10.1056/NEJMoa1007137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Tsang A, Zhang MY, Huang YQ, He YL, Liu ZR, Shen YC, Kessler RC. Lifetime prevalence and inter-cohort variation in DSM-IV disorders in metropolitan China. Psychol Med. 2007;37:61–71. doi: 10.1017/S0033291706008993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–495. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson M, Smith-Lovin L, Brashears M. Social isolation in America: Changes in core discussion networks over two decades. American Sociological Review. 2006;71:353. [Google Scholar]
- Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Mundy GR. Osteoporosis and inflammation. Nutrition Reviews. 2007;65:S147–S151. doi: 10.1111/j.1753-4887.2007.tb00353.x. [DOI] [PubMed] [Google Scholar]
- Muñoz MA, FÌto M, Marrugat J, Covas MI, Schr der H. Adherence to the Mediterranean diet is associated with better mental and physical health. Br J Nutr. 2008;15:1–7. doi: 10.1017/S0007114508143598. [DOI] [PubMed] [Google Scholar]
- Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH. A 40-year perspective on the prevalence of depression: the Stirling County Study. Arch Gen Psychiatry. 2000;57:209–215. doi: 10.1001/archpsyc.57.3.209. [DOI] [PubMed] [Google Scholar]
- Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- Nesse R. Natural selection and the elusiveness of happiness. Philosophical Transactions of the Royal Society B: Biological Sciences. 2004;359:1333. doi: 10.1098/rstb.2004.1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesse RM. Is depression an adaptation? Arch Gen Psychiatry. 2000;57:14–20. doi: 10.1001/archpsyc.57.1.14. [DOI] [PubMed] [Google Scholar]
- Nicklas BJ, You T, Pahor M. Behavioural treatments for chronic systemic inflammation: effects of dietary weight loss and exercise training. CMAJ. 2005;172:1199–1209. doi: 10.1503/cmaj.1040769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen L, Danielsen K, Sørensen T. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obesity Reviews. 2010 doi: 10.1111/j.1467-789X.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- NSF. Sleep in America Poll: Summary of Findings. National Sleep Foundation; 2009. [Google Scholar]
- OECD. OECD Health Statistics 2010. OECD iLibrary; 2010. [Google Scholar]
- Ohayon M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Medicine Reviews. 2002;6:97–112. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- Omenn GS. Evolution in health and medicine Sackler colloquium: Evolution and public health. Proc Natl Acad Sci U S A. 2010;107(Suppl 1):1702–1709. doi: 10.1073/pnas.0906198106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oyserman D, Coon HM, Kemmelmeier M. Rethinking individualism and collectivism: Evaluation of theoretical assumptions and meta-analyses. Psychological Bulletin. 2002;128:3. [PubMed] [Google Scholar]
- Pauley SM. Lighting for the human circadian clock: recent research indicates that lighting has become a public health issue. Med Hypotheses. 2004;63:588–596. doi: 10.1016/j.mehy.2004.03.020. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Klerman GL, Prusoff BA. Treatment Setting and Clinical Depression. Arch Gen Psychiatry. 1970;22:11–21. doi: 10.1001/archpsyc.1970.01740250013003. [DOI] [PubMed] [Google Scholar]
- Peen J, Schoevers R, Beekman A, Dekker J. The current status of urban- rural differences in psychiatric disorders. Acta Psychiatrica Scandinavica. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- Perry GH, Dominy NJ, Claw KG, Lee AS, Fiegler H, Redon R, Werner J, Villanea FA, Mountain JL, Misra R, Carter NP, Lee C, Stone AC. Diet and the evolution of human amylase gene copy number variation. Nat Genet. 2007;39:1256–1260. doi: 10.1038/ng2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollan M. In defense of food: an eater’s manifesto. Penguin Pr; 2008. [Google Scholar]
- Prince MJ, Harwood RH, Thomas A, Mann AH. A prospective population-based cohort study of the effects of disablement and social milieu on the onset and maintenance of late-life depression. The Gospel Oak Project VII. Psychol Med. 1998;28:337–350. doi: 10.1017/s0033291797006478. [DOI] [PubMed] [Google Scholar]
- Prudo R, Harris T, Brown GW. Psychiatric disorder in a rural and an urban population: 3. Social integration and the morphology of affective disorder. Psychol Med. 1984;14:327–345. doi: 10.1017/s0033291700003597. [DOI] [PubMed] [Google Scholar]
- Putnam R. Bowling alone: America’s declining social capital. Journal of democracy. 1995;6:65–65. [Google Scholar]
- Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends in Immunology. 2006;27:24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raison CL, Lowry CA, Rook GAW. Inflammation, Sanitation, and Consternation: Loss of Contact With Coevolved, Tolerogenic Microorganisms and the Pathophysiology and Treatment of Major Depression. Archives of General Psychiatry. 2010;67:1211. doi: 10.1001/archgenpsychiatry.2010.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy AB, O’Neill JS. Healthy clocks, healthy body, healthy mind. Trends Cell Biol. 2010;20:36–44. doi: 10.1016/j.tcb.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. JAMA: The Journal of the American Medical Association. 1990;264:2511. [PubMed] [Google Scholar]
- Riediger ND, Othman RA, Suh M, Moghadasian MH. A systemic review of the roles of n-3 fatty acids in health and disease. J Am Diet Assoc. 2009;109:668–679. doi: 10.1016/j.jada.2008.12.022. [DOI] [PubMed] [Google Scholar]
- Rosenthal SH. Changes in a population of hospitalized patients with affective disorders, 1945–1965. American Journal of Psychiatry. 1966;123:671. doi: 10.1176/ajp.123.6.671. [DOI] [PubMed] [Google Scholar]
- Ross BM, Seguin J, Sieswerda LE. Omega-3 fatty acids as treatments for mental illness: which disorder and which fatty acid? Lipids Health Dis. 2007;6:21. doi: 10.1186/1476-511X-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez-Villegas A, Delgado-Rodriguez M, Alonso A, Schlatter J, Lahortiga F, Majem LS, Martinez-Gonzalez MA. Association of the Mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Archives of General Psychiatry. 2009;66:1090. doi: 10.1001/archgenpsychiatry.2009.129. [DOI] [PubMed] [Google Scholar]
- Schieffelin EL. The cultural analysis of depressive affect: An example from New Guinea. In: Kleinman AM, Good B, editors. Culture and depression: Studies in the anthropology and cross-cultural psychiatry of affect and disorder. University of California Press; 1986. pp. 101–133. [Google Scholar]
- Schwartz B. Self-determination. The tyranny of freedom. Am Psychol. 2000;55:79–88. doi: 10.1037//0003-066x.55.1.79. [DOI] [PubMed] [Google Scholar]
- Serra Majem L, Roman B, Estruch R. Scientific evidence of interventions using the Mediterranean diet: a systematic review. Nutrition Reviews. 2006;64:S27–S47. doi: 10.1111/j.1753-4887.2006.tb00232.x. [DOI] [PubMed] [Google Scholar]
- Shephard RJ, Rode A. The Consequences of ‘modernization:’ Evidence from circumpolar peoples. Cambridge University Press; Great Britain: 1996. [Google Scholar]
- Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. Gastroenterology. 2007;132:2169–2180. doi: 10.1053/j.gastro.2007.03.059. [DOI] [PubMed] [Google Scholar]
- Simon G, VonKorff M. Recall of psychiatric history in cross-sectional surveys: implications for epidemiologic research. Epidemiologic Reviews. 1995;17:221. doi: 10.1093/oxfordjournals.epirev.a036180. [DOI] [PubMed] [Google Scholar]
- Simon GE, Goldberg DP, Von Korff M, Ustun TB. Understanding cross-national differences in depression prevalence. Psychol Med. 2002;32:585–594. doi: 10.1017/s0033291702005457. [DOI] [PubMed] [Google Scholar]
- Smith E. When culture and biology collide: Why we are stressed, depressed, and self-obsessed. Rutgers University Press; 2002. [Google Scholar]
- Sofi F. The Mediterranean diet revisited: evidence of its effectiveness grows. Current opinion in cardiology. 2009;24:442. doi: 10.1097/HCO.0b013e32832f056e. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. The Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- Stegmann ME, Ormel J, de Graaf R, Haro JM, de Girolamo G, Demyttenaere K, Kovess V, Matschinger H, Vilagut G, Alonso J, Burger H. Functional disability as an explanation of the associations between chronic physical conditions and 12-month major depressive episode. J Affect Disord. 2010;124:38–44. doi: 10.1016/j.jad.2009.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern L. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Annals of internal medicine. 2004;140:778. doi: 10.7326/0003-4819-140-10-200405180-00007. [DOI] [PubMed] [Google Scholar]
- Stevens A, Price J. Evolutionary Psychiatry: A New Beginning. Routledge; London: 2000. [Google Scholar]
- Stunkard AJ, Faith MS, Allison KC. Depression and obesity. Biological Psychiatry. 2003;54:330–337. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. The Lancet. 2011;378:804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- Teychenne M, Ball K, Salmon J. Sedentary Behavior and Depression Among Adults: A Review. Int J Behav Med. 2010;17:246–254. doi: 10.1007/s12529-010-9075-z. [DOI] [PubMed] [Google Scholar]
- Turkle S. Alone together: Why we expect more from technology and less from each other. Basic Books; 2011. [Google Scholar]
- Tuunainen A, Kripke DF, Endo T. Light therapy for non-seasonal depression. The Cochrane Library; 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J, Gentile B, DeWall C, Ma D, Lacefield K, Schurtz D. Birth cohort increases in psychopathology among young Americans, 1938–2007: A cross-temporal meta-analysis of the MMPI. Clinical psychology review. 2010;30:145–154. doi: 10.1016/j.cpr.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Twenge JM. The age of anxiety? The birth cohort change in anxiety and neuroticism, 1952–1993. Journal of personality and social psychology. 2000;79:1007. doi: 10.1037//0022-3514.79.6.1007. [DOI] [PubMed] [Google Scholar]
- Vega WA, Sribney WM, Aguilar-Gaxiola S, Kolody B. 12-month prevalence of DSM-III-R psychiatric disorders among Mexican Americans: nativity, social assimilation, and age determinants. The Journal of nervous and mental disease. 2004;192:532. doi: 10.1097/01.nmd.0000135477.57357.b2. [DOI] [PubMed] [Google Scholar]
- Walsh R. Lifestyle and mental health. American Psychologist. 2011;66:579–592. doi: 10.1037/a0021769. [DOI] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA. The obesity epidemic in the United Statesógender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiologic Reviews. 2007;29:6. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. Canadian Medical Association Journal. 2006;174:801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Paykel ES. Moving and depression in women. Society. 1972;9:24–28. [Google Scholar]
- Wells J, Horwood L. How accurate is recall of key symptoms of depression? A comparison of recall and longitudinal reports. Psychological Medicine. 2004;34:1001–1011. doi: 10.1017/s0033291703001843. [DOI] [PubMed] [Google Scholar]
- Welshons WV, Thayer KA, Judy BM, Taylor JA, Curran EM, Vom Saal FS. Large effects from small exposures. I. Mechanisms for endocrine-disrupting chemicals with estrogenic activity. Environmental Health Perspectives. 2003;111:994. doi: 10.1289/ehp.5494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG, Pickett K, Trust E, Foundation ME. The spirit level: why more equal societies almost always do better. Allen Lane London; 2009. [Google Scholar]
- Wilkinson RG, Pickett KE. Income inequality and population health: A review and explanation of the evidence. Social Science & Medicine. 2006;62:1768–1784. doi: 10.1016/j.socscimed.2005.08.036. [DOI] [PubMed] [Google Scholar]
- Yach D, Stuckler D, Brownell KD. Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nat Med. 2006;12:62–66. doi: 10.1038/nm0106-62. [DOI] [PubMed] [Google Scholar]