Abstract
The authors report preliminary results of Brief Supportive Psychotherapy (BSP) in the Beth Israel Brief Psychotherapy Program for a sample with primarily Cluster C Axis II disorders. This study compares 24 patients treated with BSP with 25 patients treated with Short-Term Dynamic Psychotherapy (STDP). STDP was chosen because its confrontational methods contrast dramatically to BSP, which emphasizes building self-esteem, reducing anxiety, and enhancing coping mechanisms. Videotaped therapies were based on manualized 40-session protocols. Similar degrees of improvement were seen in BSP and STDP at termination and at 6-month follow-up. A study of therapeutic alliance in BSP showed stable and high levels of alliance in good-outcome cases and more variability in poor-outcome cases. These preliminary findings are consistent with other studies and suggest supportive psychotherapy may be effective for many patients, leading to significant and lasting change. (The Journal of Psychotherapy Practice and Research 1998; 7:261–271)
In recent years, more attention has been paid to supportive therapy, with the publication of reviews,1–5 texts and manuals,6–9 and some psychotherapy outcome studies.10–13 However, clinicians rarely view supportive therapy as a first-line treatment. In clinical practice, supportive therapy is generally reserved for patients believed to be unsuitable for expressive therapy (or other approaches)—individuals with severe personality disorders or chronic Axis I disorders, or those lacking motivation or insight. In psychotherapy research, supportive therapy is often included as a control in studies of “active” treatments, whether behavioral or psychodynamic, rather than as a modality to be studied on its own merits. In some studies,10,12,14 psychotherapy researchers have determined that an “active” treatment is no better than the “control” of supportive therapy. Although such findings may indicate the efficacy of “nonspecific factors” in psychotherapy, they also raise the possibility that supportive therapy may be more efficacious than has been traditionally believed.
We are reporting here on preliminary results of supportive therapy as studied at Beth Israel Medical Center's Brief Psychotherapy Research Program.15,16 This project has compared several forms of psychotherapy in a prospective, randomized fashion, using videotapes and a variety of therapist-, patient-, and observer-rated measures of process and outcome. Initially the Brief Psychotherapy Project compared Short-Term Dynamic Psychotherapy (STDP), an intense, highly confrontive treatment developed by Davanloo,17,18 with Brief Adaptive Psychotherapy (BAP), a traditional “insight-oriented” psychotherapy19 designed to be similar to that practiced by dynamically oriented therapists in the community. Other cells now include Cognitive-Behavioral Therapy (CBT)20 and Brief Relational Therapy (BRT).21
Brief Supportive Psychotherapy (BSP) was added to the Brief Psychotherapy Research Project in 1988 to broaden the range of treatment approaches under study. Like STDP and the other treatments, BSP was a time-limited, manual-based psychotherapy. We have published a manual7 and several papers and book chapters15,16,22 providing a definition of supportive therapy and a rationale for considering it to be an active form of psychotherapy, potentially as effective a means for structural psychological change as the more traditionally “exploratory” or “expressive” therapies.
Our model-based (and literature-based) belief in the effectiveness of supportive therapy has until now been supported only by the anecdotal experience with the Brief Psychotherapy Research Project, where many BSP cases had positive outcomes. We hypothesize that BSP may be effective not only with the low-functioning patients to whom it has long been prescribed, but also with higher-functioning patients who have traditionally been treated in expressive psychotherapy. In assessing treatment outcome, this study reverses the traditional question of psychotherapy research. Rather than investigating whether another therapy is as good as or better than supportive psychotherapy, our hypothesis is that BSP has equal or greater efficacy compared with a “control” of STDP, as measured by a variety of outcome measures. In previous work,23 STDP has been demonstrated to be superior to a wait-list control condition.
In addition, we are interested in beginning to characterize and describe the quality of therapeutic alliance in BSP. Despite its importance, there has been little systematic work in this area. In one study, Salvio et al.24 compared alliance in cognitive, gestalt, and supportive/ self-directed therapy by using the Working Alliance Inventory (WAI) and the Barrett-Lennard Relationship Inventory (which measures therapist qualities of empathy, positive regard, and congruence), measuring alliance four times during treatment. Salvio et al. found little variation from the beginning to the end of therapy, and no significant difference in quality of the alliance among the three therapies.
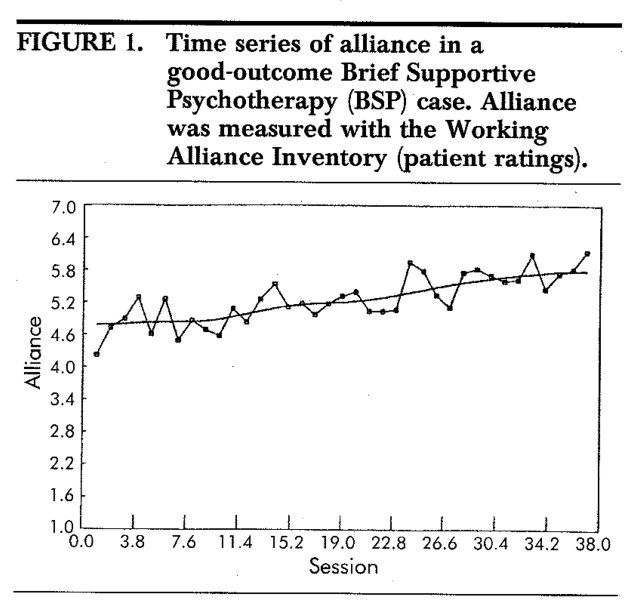
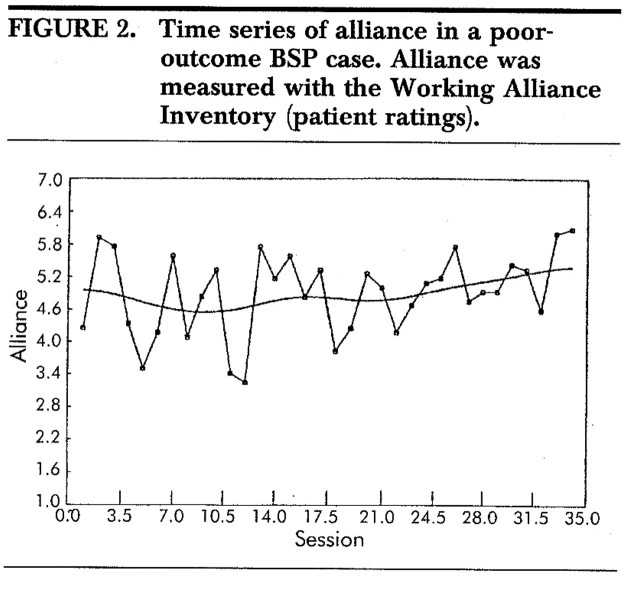
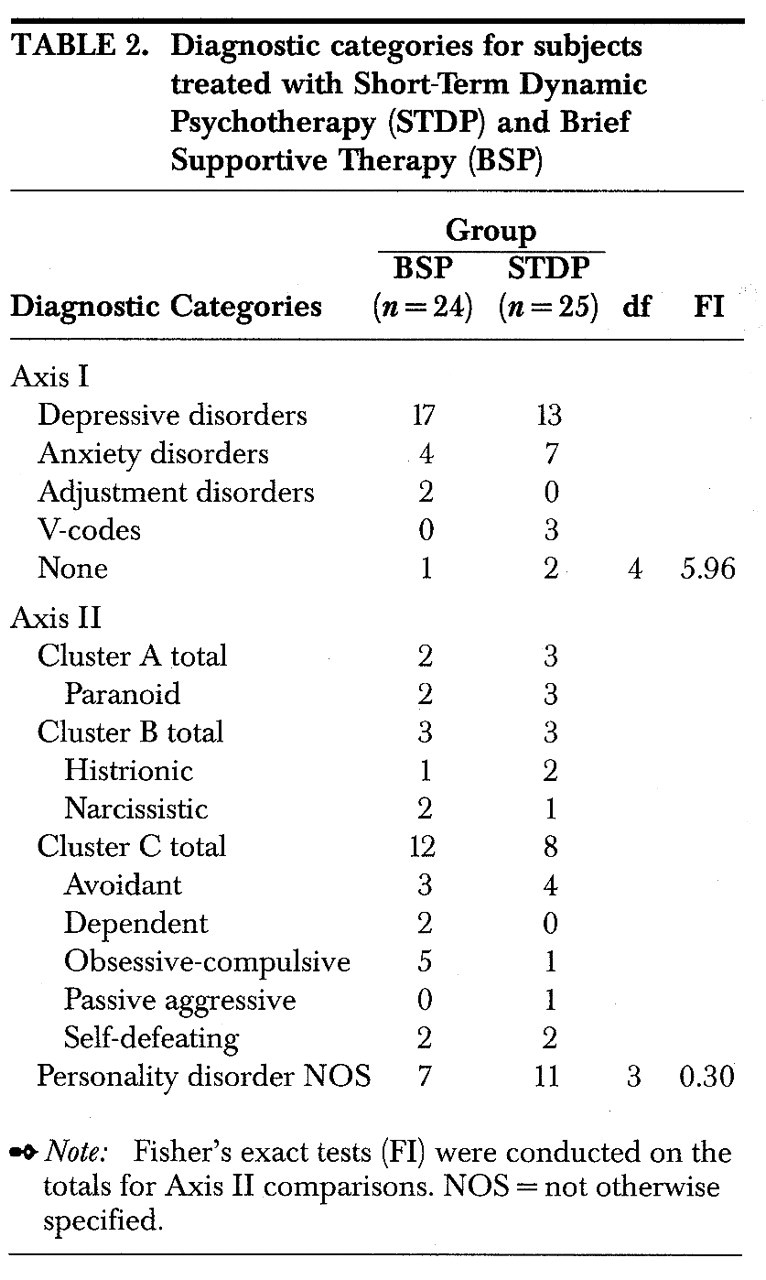
In studying BSP, we expect that the alliance will be positive and stable throughout therapy in good-outcome cases, whereas in problematic or poor-outcome cases, we expect that alliance will be less positive and will fluctuate widely. We hypothesize that the alliance in BSP will differ from alliance in dynamic psychotherapy, especially STDP, which is a confrontational, anxiety-provoking treatment. The friendly, anxiety-reducing approach of the BSP therapist, we believe, should allow the patient to feel more comfortable early in treatment and to feel more “understood” in early sessions. If the BSP treatment is going well, we would expect the level of alliance to remain stable and high. In contrast, in STDP, patients may experience the frequent interpretations and the anxiety-inducing techniques of that treatment as threatening and foreign, and thus there may be significant fluctuations in the therapeutic alliance even in good-outcome cases.
Methods
Subjects
Patients in this study were treated at Beth Israel Medical Center in the Brief Psychotherapy Project. After providing informed consent, patients were assessed for suitability for this study. Inclusion criteria included 1) age 18–60 years; 2) evidence of at least one close relationship; and 3) presence of Axis II personality disorder. Exclusion criteria included 1) evidence of psychosis, organic brain disease, or mental retardation; 2) active medical condition (DSM-III-R Axis III); 3) current substance abuse; 4) history of significant violent or suicidal behavior; or 5) use of psychotropic medication (neuroleptic, antidepressant, mood stabilizer) within the past 1 year.
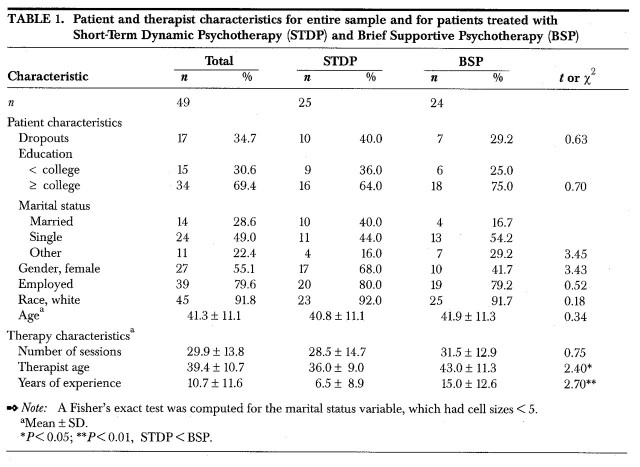
For a summary of characteristics of patients and therapists who participated in this study, see Table 1 and Table 2 in the Results section.
TABLE 1.
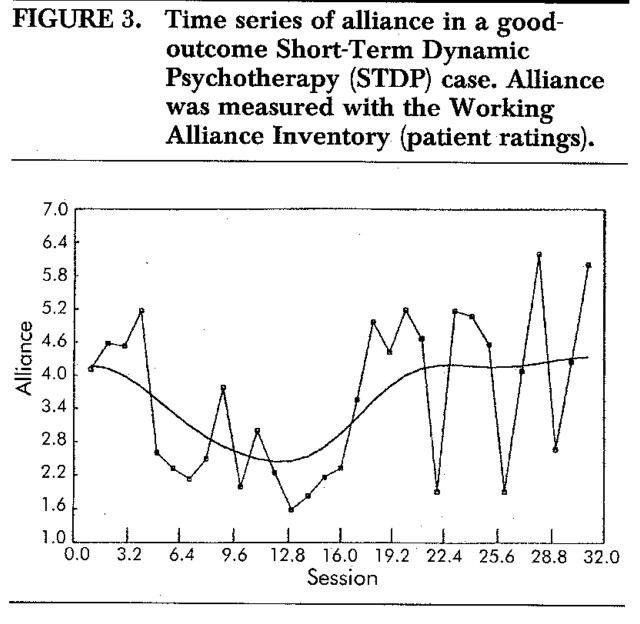
TABLE 2.
Initial evaluation consisted of a diagnostic assessment using the Structured Clinical Interview for DSM-III-R (SCID25; SCID-II26). Patients also completed a psychosocial history and a variety of rating scales described below.
Following acceptance into the Brief Psychotherapy Study, patients were randomly assigned to one of five different psychotherapies: BSP, STDP, CBT, BAP, or BRT. For purposes of this paper, we are reporting on two cells of this study, BSP and STDP. This data analysis compares 24 patients treated in BSP with 25 patients treated with STDP. Patients were enrolled between the years 1991 and 1996; the cohort of STDP patients included in this study was treated later than those reported previously.23
Therapies, Adherence, and Completion
Following our definition of Supportive Psychotherapy,7 BSP emphasizes building self-esteem, reducing anxiety, and enhancing coping mechanisms. Supportive psychotherapy is conversational in style and commonly uses techniques such as clarification, suggestion, praise, education, and examination of the influence on present life of patterns originating in the past. Supportive therapy rarely uses techniques such as prolonged silent listening, “neutrality,” confrontation of resistance, or transference interpretations; wherever possible, therapy-induced anxiety is avoided.
The STDP condition18,27 was used as a comparison group because its efficacy had been established with this population of patients in previous work.23 STDP had been shown23 to be comparable in efficacy to BAP, another dynamically oriented therapy, and superior to a wait-list control group. Also, its high reliance on confrontation, elicitation of affect, and interpretation of transference issues provide a marked contrast to the methods of supportive psychotherapy. Frequently used STDP techniques include confrontation of resistance, early interpretation of transference, and direct evocation of anxiety and other affects with the goal of mobilizing psychological change.
Both therapies were based on manualized protocols, and all sessions were videotaped. In both therapies, treatment was designed to last up to 40 sessions, but patients and therapists could decide to end treatment between sessions 30 and 40 and the treatment would be considered completed.
There were 32 therapists participating in this study, 11 providing BSP and 23 providing STDP (2 therapists provided both treatments). All therapists attended a peer group weekly seminar in which videotaped material was presented and critiqued. Adherence to the treatment was monitored by research assistants using a structured approach based on the treatment manuals.
We have previously reported data on adherence with BSP and STDP. In STDP,28 a 12-item adherence scale was developed that covered the essential elements of that technique, with each item rated on a 5-point Likert-type scale. Thirty-nine sessions of 13 patients treated by 12 therapists were rated; they had mean ratings of 3.0 (SD = 0.44) on these items, and 10 of 12 therapists had adequate adherence ratings. In a study of BSP patients,29 raters evaluated the fifth session of treatment for 10 therapists. A scale was developed for each of the five therapies being studied, in which three questions were selected for each therapy, reflecting essential aspects of each treatment. Rating of the BSP sessions showed that 6 of 10 therapists rated adhered with a mean score of 3 or more on the three BSP items, whereas none adhered to the other therapy items—those for BAP, STDP, CBT, or BRT. In these studies, interrater reliability was 0.83 for STDP and 0.89 for BSP, indicating adequate levels of interrater reliability.
The total number of sessions completed by each patient was tabulated, and the frequency of premature terminators and treatment completers was divided according to treatment quartile. In this study, premature terminators were defined as patients who dropped out prior to session 30 (i.e., within the first, second, or third quartile). Those who attended at least 30 of the 40 session protocols were considered treatment completers. Premature termination was a unilateral decision made by the patient; therapists encouraged patients to complete the initial agreement of 40 sessions but could not force their patients to remain in treatment. Although dropouts were included in the demographic and diagnostic summaries, only treatment completers were asked to fill out the termination battery of questionnaires.
Measures of Outcome, Alliance, and Target Complaints
Overall outcome was measured by using the Symptom Checklist-90 Global Symptom Index (SCL-90-R GSI),30 which assesses psychiatric symptomatology; the Inventory of Interpersonal Problems (IIP),31 which assesses interpersonal functioning; and the patient-rated Target Complaints (PTC),32 an idiographic measure of the patient's three major presenting problems, rated on a Likert-type scale. These outcome assessments were obtained at four points: Intake, Midphase (week 20), Termination, and Follow-up (6 months after Termination).
Patients completed the Working Alliance Inventory (WAI)33,34 following each session. The WAI consists of three subscales (Task Agreement, Goal Agreement, and Bond Development) and yields scores for each of these, as well as an overall alliance index. Each subscale consists of 4 items scaled in a 7-point Likert-type format. Tracey and Kokotovic35 have demonstrated adequate reliability for the short-form version of the WAI. Internal consistency estimates of alpha were 0.98 for the overall patient scale, with subscale alphas of 0.90 to 0.92. Data regarding the predictive validity of the WAI have been reviewed by Horvath and Symonds36 in their meta-analysis. (See also Samstag et al.37)
Patients were permitted to define up to three presenting target complaints (TC).32 Each complaint was rated independently by both patients and therapists in terms of how problematic it was currently for the patient. Ratings were made on a Likert-type scale, ranging from 1 (“not at all”) to 13 (“couldn't be worse”). Overall mean TC scores were used in the present study: that is, for each patient the total score for all target complaints was divided by the number of complaints to give an average TC severity score.
Data Analysis
A series of analyses of variance (ANOVAs) was conducted comparing change across treatment and differences between the two therapies, controlling for years of therapist clinical experience. These analyses represented an initial assessment of overall outcome. Because of the amount of missing data, a multivariate analysis was not feasible.
Alliance was measured throughout the course of treatment with the WAI, using a single case study method. Using the SCL-90-R (GSI) and the IIP in single case analysis, we evaluated 3 patients treated in supportive therapy as having good outcomes and 2 patients as having poor outcomes, based on statistically significant change (reliable change coefficient) from admission to termination.38 One patient treated in STDP, used as a comparison case, was evaluated as having good outcome.
We performed time series analyses of WAI mean ratings for each session for individual patients. These analyses involved the application of exponential smoothing, which has been found to be most effective when the parameters describing time series may be changing slowly over time. The smoothing method reduces the fluctuations in the time series data by using a moving average; that is, by replacing individual ratings with a mean of each rating and the ratings on either side of it. This method serves to make any trends in the data more apparent. The moving average used in this study was based on a procedure recommended by Tukey39 and calculated by the program SIMSTAT.40
Results
Patient, Therapist, and Treatment Variables
Of 49 patients admitted to treatment in the 2 cells (25 to STDP and 24 to BSP), 17 (34.7%) did not complete 40 sessions of treatment. The rate of dropout, 10/25 (40%) for STDP and 7/24 (29%) for BSP, did not differ between groups. Of patients in BSP, 3, 1, and 3 patients discontinued treatment in the first, second, and third quartile, respectively; and of patients in STDP, 4, 3, and 3 patients terminated in the first, second, and third quartile (Fisher's exact test, FI = 1.32, df = 3, not significant).
Patient and therapist characteristics (n and mean ± SD) are as shown in Tables 1 and 2. Briefly, patients averaged 41.3 ± 11.1 years of age; 91.8% were Caucasian; 55.1% were female; 69.4% had 4 or more years of college education; 79.6% were employed; 71.4% were single, divorced, or widowed; and 28.6% were married. Diagnoses primarily reflected Cluster C disorder on Axis II, or “NOS” (not otherwise specified) diagnoses on Axis II, which generally included Cluster C features. The predominant Axis I diagnoses were mood disorders. There were no significant differences between STDP and BSP subjects on these descriptive and diagnostic variables.
Therapists averaged 39.4 ± 10.7 years of age for the entire sample; STDP therapists were significantly younger (36.0 ± 9.0 years) than BSP therapists (43.0 ± 11.3 years; t = 2.40, df = 47, P < 0.05) and had fewer years of postdoctoral experience (6.5 ± 8.9 years vs. 15.0 ± 12.6 years; t = 2.70, df = 41.26, P < 0.01). In order to determine if therapist age and years of experience should be included as covariates in the analyses of treatment outcome differences between the two groups, a series of partial correlations was conducted. There were no significant correlations between intake and termination scores, controlling in one analysis for therapist age and in another for years of experience, on any of the three outcome measures (PTC, IIP, SCL-90). Therefore, since these therapist variables were found to have no statistically significant impact on overall treatment outcome (i.e., pre to post change), they were not used as covariates in subsequent comparisons. Notably, correlations controlling for therapist age showed a trend on one measure, the PTC (r = 0.40, P = 0.062; see Discussion).
The mean duration of treatment was 29.9 ± 13.8 weeks for the sample as a whole, or 28.5 ± 14.7 sessions for STDP patients versus 31.5 ± 12.9 sessions for BSP patients. This was not a significant difference.
Outcome Measures
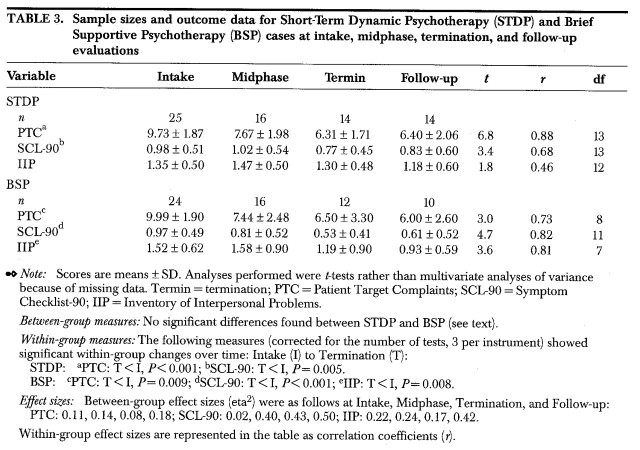
Table 3 displays raw scores, reported as means ± SD. We compared the STDP and BSP samples on a number of outcome measures, including PTC, SCL90, and the IIP, using a series of independent t-tests, for ratings obtained during the Intake, Midphase, Termination, and Follow-up periods. We conducted t-tests rather than a multivariate analysis because of the number of missing data points. There were no significant differences between STDP and BSP groups on PTC, SCL90, or IIP at any of these times. The effect sizes41 of these between-group analyses were mostly small, with some of medium size.
TABLE 3.
In addition, within-group changes over time were calculated (using paired t-test, two-tailed) on each of the inventories, comparing Intake with Termination scores (see Table 3 note, Within-group measures). These demonstrated a time effect for both STDP and BSP, with a significant decrease in severity on the PTC, SCL90, and IIP for BSP and a significant decrease in the PTC and SCL-90 for STDP between Intake and Termination. The decrease in IIP score for the STDP group did not reach significance (P = 0.104). The results of these within-group analyses yielded large effect sizes41 across the board.
Single Case Studies of Alliance
As part of an early effort to characterize the pattern of therapeutic alliance in BSP, alliance was assessed by using patient-rated postsession questionnaires for a small sample of our BSP study population, dividing between good-outcome and poor-outcome cases (n = 3 and n = 2, respectively). On the patient-rated WAI, the 3 good-outcome supportive cases had mean scores and standard deviations of 5.12 ± 0.55, 5.25 ± 0.46, and 4.72 ± 0.46; the two poor-outcome supportive cases had mean scores and standard deviations of 4.89 ± 0.76 and 5.02 ± 0.81. Time series analyses for selected single case analyses of alliance are presented in Figures 1 and 2. There was little fluctuation in the WAI in the good-outcome cases, as demonstrated by relatively flat time series analyses (see Figure 1) and by small standard deviations. In the poor-outcome cases, there was a great deal of fluctuation in the WAIs, especially early in treatment (see Figure 2). A time series analysis of a good-outcome STDP case is shown in Figure 3. In contrast to the good-outcome BSP cases, this case reveals very wide fluctuations in the WAI from session to session, with WAI mean and standard deviation of 3.60 ± 1.39.
FIGURE 1.
FIGURE 2.
FIGURE 3.
Discussion
Positive Outcome in Supportive Therapy
Our findings suggest that supportive psychotherapy (BSP) deserves serious consideration as an active modality of psychotherapy, and one that appears to have comparable efficacy to a highly structured, confrontational, transference-based psychodynamic psychotherapy (STDP). In the various measures employed in this study design, BSP appears to be at least equally effective in leading to alleviation of patients' target complaints, in decreasing symptomatology as measured by the SCL90, and in leading to improvement of interpersonal problems. It is important to note that study patients were relatively high-functioning individuals, predominantly employed college graduates, with Cluster C Axis II disorders and Axis I mood disorders. Such patients traditionally are felt to be more suitable for expressive than supportive psychotherapy. Indeed, our previous studies23 show that varying forms of expressive therapy (BAP and STDP) are effective for such patients.
In this study, therapists applying a manualized form of supportive therapy also appear to be successful in retaining patients in treatment, in building a high degree of therapeutic alliance, and in attaining a positive outcome on a variety of measures. These findings support our hypothesis that supportive therapy may be efficacious even for high-functioning patients and that it should be considered as a viable therapeutic approach for these patients. Supportive therapy may have efficacy comparable to that of expressive therapy, and, indeed, Wallerstein13 has suggested that much of the benefit in expressive therapy may result from its supportive elements.
Stable Alliance in Supportive Therapy
Our preliminary evidence suggests that the therapeutic alliance in brief supportive psychotherapy may be stable throughout the course of therapy in good-outcome cases (as measured by the patient WAI in 3 cases). This was not the case in 2 poor-outcome BSP cases, which had considerably higher standard deviations on the WAI and more fluctuation on the time series analysis. In contrast, a good-outcome dynamic psychotherapy case (STDP) had major alliance fluctuations on the WAI during the entire treatment. BSP may thus belong among those therapies that use the therapeutic alliance as a foundation for treatment,42,43 rather than as a vehicle for change.44–47 In a transference-based treatment such as STDP, the therapeutic relationship itself (which may be perceived by the patient as stormy, intense, and difficult) is thought to be the vehicle for change, and change in the patient's interpersonal relationships may occur as a result of improvements in the therapeutic alliance. In contrast, in treatments where the alliance is the “foundation” for change, therapy ideally provides a nonthreatening environment in which the patient and therapist can work on issues relevant to the patient's outside life. In such therapies, it would be important to establish an alliance that remained stable and positive throughout the course of treatment and to minimize fluctuations from session to session. Our pilot data suggest that this may indeed occur in good-outcome BSP cases.
Indeed, the techniques generally used in supportive psychotherapy are ideal for promoting and maintaining a positive, stable therapeutic alliance.15 Communicating warmth, respect, and empathy for the patient, although important in all therapies, is a central goal of supportive therapy.3 The therapist's stance is nonchallenging, and the therapist actively uses anxiety-reducing techniques. The therapist supports the patient's higher-level defenses, when appropriate, and uses praise and positive feedback to enhance the patient's self-esteem. In supportive therapy, transference is not interpreted or worked with unless it is negative. Again, this approach tends to ensure a stable alliance by providing a safe, secure holding environment and by deliberately not interfering with or delving into an apparently positive relationship.
Limitations of the Study
Our study is limited by several methodological factors. First, there is no untreated or placebo-treated control group in this analysis. Changes observed in symptom severity may thus not be related to treatment per se. They may result from the passage of time, or from nonspecific factors such as attention, rather than from specific therapeutic orientation. However, as mentioned above, previous analyses23 have determined that patients treated with STDP showed significantly more improvement than a wait-list control group (n = 26) on measures including Target Complaints, SCL90, and Social Adjustment Scale. Thus, STDP appears to be an active treatment, appropriate for use as a comparison group in a study of supportive therapy. Second, sample sizes are small, particularly at follow-up, and data are absent for study dropouts. Third, our samples differed in therapist experience and age. Although these differences were generally not statistically significant in predicting outcome (with the exception of a trend on the PTC), in future studies we would attempt to eliminate such differences. Fourth, brief dynamic psychotherapies vary widely in their approaches, and STDP may not represent “typical” brief psychodynamic therapies practiced in the community. Hence, our conclusions must remain tentative at this point.
However, our study has certain strengths as well. Therapists were trained according to manual-based therapies; the study has a randomized prospective design; and all sessions are videotaped and thus available for retrospective review regarding therapist adherence and competence as well as therapeutic process. Also, data include postsession ratings by patients as well as a variety of rating inventories for areas including target complaints, psychiatric symptomatology, and interpersonal problems.
Conclusions
In the debate about Smith and colleagues' meta-analyses48,49 of psychotherapy outcomes, Luborsky and colleagues have asked50,51 whether “everyone has won and all must have prizes.” In this spirit, our group has somewhat facetiously claimed for supportive therapy that “in case of a tie, we win.”52 Our current data do not definitively demonstrate the equivalency of therapeutic approaches, which would require a much larger sample size. However, they do suggest potential benefits for supportive psychotherapy. The approaches of supportive therapy may be more familiar and comfortable for many patients than the abstaining (or confrontational) approaches of expressive therapies. Supportive psychotherapy may also be applicable to a wider range of patients than traditional expressive therapy.
Our preliminary findings suggest the need for more serious attention from psychotherapy researchers. Theorists might also pay more significant attention to supportive therapy and might reconceptualize belief systems about the mechanisms of change in psychotherapy. Further, given the widespread use of this modality of treatment,2 our findings suggest22 that mental health clinicians should be taught the modality of supportive therapy with formal didactic training and supervision, similar to training in expressive or cognitive-behavioral therapies.
References
- 1.Conte HR, Plutchik R: Controlled research in supportive psychotherapy. Psychiatric Annals 1986; 16:530–533 [Google Scholar]
- 2.Rockland LH: A review of supportive therapy:1986–1992. Hosp Community Psychiatry 1993; 44:1053–1060 [DOI] [PubMed] [Google Scholar]
- 3.Winston A, Pinsker H, McCullough L: A review of supportive psychotherapy. Hosp Community Psychiatry 1986; 37:1105–1114 [DOI] [PubMed] [Google Scholar]
- 4.Buckley P: Supportive therapy: a neglected treatment. Psychiatric Annals 1986;16:515–521
- 5.Kernberg OF: Supportive psychotherapy, in Severe Personality Disorders: Psychotherapeutic Strategies. New Haven, CT, Yale University Press, 1984, pp 147–164
- 6.Novalis PN, Rojcewicz SJ, Peele R: Clinical Manual of Supportive Psychotherapy. Washington, DC, American Psychiatric Press, 1993
- 7.Pinsker H, Rosenthal R: Beth Israel Medical Center supportive psychotherapy manual, in Social and Behavior Sciences Documents Abstracts, no 18. Washington, DC, American Psychological Association, 1988, #2886
- 8.Rockland LH: Supportive Therapy: A Psychodynamic Approach. New York, Basic Books, 1989
- 9.Luborsky L: Principles of Psychoanalytic Psychotherapy: A Manual for Supportive-Expressive (SE) Methods. New York, Basic Books, 1984
- 10.Zitrin CM, Klein DF, Woerner MG: Behavior therapy, supportive psychotherapy, imipramine, and phobias. Arch Gen Psychiatry 1978; 35:307–316 [DOI] [PubMed] [Google Scholar]
- 11.Klein DF, Zitrin CM, Woerner MG, et al: Treatment of phobias. Behavior therapy and supportive psychotherapy: are there any specific ingredients? Arch Gen Psychiatry 1983; 40:139–145 [DOI] [PubMed] [Google Scholar]
- 12.Gunderson JG, Frank AF, Katz HM, et al: Effects of psychotherapy in schizophrenia, II: comparative outcome of two forms of treatment. Schizophr Bull 1984; 10:564–598 [DOI] [PubMed] [Google Scholar]
- 13.Wallerstein RS: The psychotherapy research project of the Menninger Foundation: an overview. J Consult Clin Psychol 1989; 57:195–205 [DOI] [PubMed] [Google Scholar]
- 14.Stanton AH, Gunderson JC, Knapp PH, et al: Effects of psychotherapy in schizophrenia, I: design and implementation of a controlled study. Schizophr Bull 1984; 10:520–563 [DOI] [PubMed] [Google Scholar]
- 15.Pinsker H, Rosenthal RN, McCullough L: Supportive dynamic psychotherapy, in Handbook of Short-Term Dynamic Therapy, edited by Crits-Christoph P. New York, Basic Books, 1991, pp 220–247
- 16.Hellerstein DJ, Pinsker H, Rosenthal RN, et al: Supportive therapy as the treatment model of choice. J Psychother Pract Res 1994; 3:300–306 [PMC free article] [PubMed] [Google Scholar]
- 17.Davanloo H: Short-Term Dynamic Psychotherapy. New York, Jason Aronson, 1980
- 18.Laikin M, Winston A, McCullough L: Intensive short-term dynamic psychotherapy, in Handbook of Short-Term Dynamic Psychotherapy, edited by Crits-Christoph P, Barber JP. New York, Basic Books, 1991, pp 80–109
- 19.Pollack J, Flegenheimer W, Winston A: Brief adaptive psychotherapy, in Handbook of Short-Term Dynamic Psychotherapy, edited by Crits-Cristoph P, Barber JP. New York, Basic Books, 1991, pp 199–219
- 20.Turner AW, Muran JC: Cognitive behavioral therapy for personality disorders: a treatment manual (abstract), in Social and Behavioral Sciences Documents Abstracts, no 18. Washington, DC, American Psychological Association, 1992, #2885
- 21.Safran JD, Muran JC: Negotiating the Therapeutic Alliance: A Relational Treatment Manual. New York, Guilford (in press)
- 22.Pinsker H: The role of theory in teaching supportive therapy. Am J Psychother 1994; 4:530–542 [DOI] [PubMed] [Google Scholar]
- 23.Winston A, Laikin M, Pollack J, et al: Short-term psychotherapy of personality disorders. Am J Psychiatry 1994; 151:190–194 [DOI] [PubMed] [Google Scholar]
- 24.Salvio MA, Beutler LE, Wood JM, et al: The strength of the therapeutic alliance in three treatments for depression. Psychotherapy Research 1992; 2:31–36 [Google Scholar]
- 25.Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1987
- 26.Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). New York, New York State Psychiatric Institute, Biometrics Research, 1987
- 27.Laikin M, Winston A: Short-term dynamic psychotherapy manual (STDP), in Social and Behavioral Sciences Documents Abstracts, no 18. Washington, DC, American Psychological Association, 1988, #2887
- 28.Flegenheimer W: Therapist adherence and compliance. Presented at the American Psychiatric Association annual meeting, New York, NY, 1990. Washington, DC, American Psychiatric Association, CME Syllabus and Proceedings Summary, pp 190–191
- 29.Winston A, Pinsker H, Muran JC,et al: Adherence to Brief Supportive Psychotherapy (BSP). World Journal of Psychosynthesis 1991; 20:12–16 [Google Scholar]
- 30.Derogatis LR: Symptom Checklist-90–Revised (SCL-90-R): Administration, Scoring and Procedures Manual, II. Towson, MD, Clinical Psychometric Research, 1983
- 31.Horowitz LM, Rosenberg SE, Baer EA, et al: Inventory of Interpersonal Problems: psychometric properties and clinical applications. J Consult Clin Psychol 1988; 56:885–892 [DOI] [PubMed] [Google Scholar]
- 32.Battle CC, Imber SD, Hoehn-Saric R, et al: Target complaints as criteria of improvement. Am J Psychother 1966; 20:184–192 [DOI] [PubMed] [Google Scholar]
- 33.Horvath AO, Greenberg LS: The Working Alliance. New York, Wiley, 1994
- 34.Horvath AO, Greenberg LS: The development and validation of the Working Alliance Inventory. Journal of Counseling Psychology 1989; 36:223–233 [Google Scholar]
- 35.Tracey T, Kokotovic A: Factor structure of the Working Alliance Inventory. Psychological Assessment 1989; 1:207–210 [Google Scholar]
- 36.Horvath AO, Symonds BD: Relation between working alliance and outcome in psychotherapy: a meta-analysis. J Consult Clin Psychol 1991; 38:139–149 [Google Scholar]
- 37.Samstag LW, Batchelder ST, Muran JC, et al: Early identification of treatment failures in short-term psychotherapy: an assessment of therapeutic alliance and interpersonal behavior. J Psychother Pract Res 1998; 7:126–143 [PMC free article] [PubMed] [Google Scholar]
- 38.Jacobson NS, Traux P: Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991; 59:12–19 [DOI] [PubMed] [Google Scholar]
- 39.Tukey JW: Exploratory Data Analysis. Reading, MA, Addison-Wesley, 1977
- 40.Pelandeau N: SIMSTAT: Version 3.0. Montreal, QC, Provalis Research, 1994
- 41.Cohen J: Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ, Lawrence Erlbaum, 1988
- 42.Hartley DE, Strupp HH: The therapeutic alliance: its relationship to outcome in brief psychotherapy, in Empirical Studies of Psychoanalytical Theories, vol 1, edited by Masling J. Hillsdale NJ, Analytical Press, 1983, pp 1–27
- 43.Mallinckrodt B: Session impact, working alliance, and treatment outcome in brief counseling. Journal of Counseling Psychology 1993; 40:25–32 [Google Scholar]
- 44.Allen JG, Tarnoff G, Coyne L: Therapeutic alliance and long-term hospital treatment outcome. Compr Psychiatry 1985; 26:187–194 [DOI] [PubMed] [Google Scholar]
- 45.Henry WP, Schacht TE, Strupp HH: Structural Analysis of Social Behavior: application to a study of interpersonal process in differential psychotherapeutic outcome. J Consult Clin Psychol 1986; 54:27–31 [DOI] [PubMed] [Google Scholar]
- 46.Lansford E: Weakenings and repairs of the working alliance in short-term psychotherapy. Professional Psychology: Research and Practice 1986; 17:64–366 [Google Scholar]
- 47.Safran JD: Breaches in the therapeutic alliance: an arena for negotiating authentic relatedness. Psychotherapy 1993; 30:11–24 [Google Scholar]
- 48.Smith ML, Glass GV: Meta-analysis of psychotherapy outcome studies. Am Psychol 1977; 132:752–760 [DOI] [PubMed] [Google Scholar]
- 49.Smith ML, Glass GV, Miller TI: The Benefits of Psychotherapy. Baltimore, Johns Hopkins University Press, 1980
- 50.Luborsky L, Singer B, Luborsky L: Comparative studies of psychotherapies: is it true that “everyone has won and all must have prizes”? Arch Gen Psychiatry 1975; 32:995–1008 [DOI] [PubMed] [Google Scholar]
- 51.Beutler LE: Have all won and must all have prizes? Revisiting Luborsky et al.'s verdict. J Consult Clin Psychol 1991; 59:226–232 [DOI] [PubMed] [Google Scholar]
- 52.Hellerstein DJ: Panel session: Defining and Studying Supportive Psychotherapy (Pinsker H, Rosenthal RN, Hellerstein DJ: Supportive therapy and supportive elements in treatment; Hellerstein DJ, Samstag LW, et al: A randomized prospective study comparing supportive and dynamic therapies: alliance and outcome; Rosenthal RN, Hellerstein DJ, Pinsker H: Testing effectiveness of supportive therapy: model and scope). Program Abstracts, Society for Psychotherapy Research, Vancouver, BC, 1995, pp 123–126