Abstract
There is considerable evidence that psychosocial treatments benefit younger adults with schizophrenia. However, no studies have been undertaken of such interventions for older patients with schizophrenia. This report describes the development of a novel integrated treatment combining cognitive-behavioral therapy (CBT) and social skills training (SST). This intervention is designed to address the needs of older patients with schizophrenia by challenging beliefs common in this population that interfere with treatment and by providing repetitive practice of behaviors to improve retention and skill development. The authors provide two case reports and pilot data suggesting benefits of this approach.
Keywords: Schizophrenia; Geriatric Psychiatry; Psychotherapy, Cognitive and Behavioral; Social Skills Training
Schizophrenia is arguably the most expensive mental disorder,1,2 and its cost is highest in the oldest patient groups.3 The number of older individuals with schizophrenia (as well as other psychiatric disorders) in the population is expected to increase dramatically over the next several decades.4 Despite the increase in personal and societal costs associated with aging patients with schizophrenia, development and testing of psychotherapeutic interventions for these patients has been practically nonexistent. Trials of manual-guided psychotherapeutic and behavioral interventions for complementing the therapeutic effects of antipsychotic medications for older patients with schizophrenia are urgently needed. By improving independent social functioning of older patients with schizophrenia, such interventions may prevent excess disability and premature institutionalization of these patients and reduce the burden and stress on families and caregivers.
A growing literature suggests that treatments such as cognitive-behavioral therapy (CBT) and social skills training (SST) are effective in improving the quality of life of younger adults with schizophrenia.5–7 However, these interventions have not been used to address the specific needs of older patients with schizophrenia. The purpose of this article is to describe the development of an integrated intervention based on CBT and SST designed to improve the functioning and quality of life of older individuals with schizophrenia. We first review published studies of CBT or SST in younger schizophrenia patients, then describe the development of an integrated model, and finally present initial data on the use of this new therapy in a group of older patients.
REVIEW OF CBT AND SST FOR PATIENTS WITH SCHIZOPHRENIA
The theoretical basis for using CBT and SST can be derived from the biopsychosocial stress-vulnerability model of schizophrenia.8–10 Within this framework, stressors impinge upon cognitive and psychobiological vulnerabilities, leading to symptom exacerbation and decreased social functioning. Cognitive vulnerabilities, such as neurocognitive decline and beliefs about a decreased ability of older people to change, tend to increase with aging, and many typical stressors occur more frequently in older than in younger adults (e.g., physical illness, social isolation, developmental role changes, losses of close friends and relatives, and financial problems). CBT and SST can potentially improve functioning by
Reducing cognitive vulnerabilities (e.g., rigidity of thinking; self-defeating beliefs).
Improving the individual's ability to cope with stressors (e.g., developing larger social networks; learning to ask for support).
Improving adherence to treatments that modify biological factors (e.g., pharmacotherapy).
Mounting evidence indicates that psychotherapeutic interventions, when combined with careful pharmacotherapy, can improve functional outcome and symptom control in younger adults with schizophrenia.7,11–18
Cognitive-Behavioral Therapy for Schizophrenia
There has been a recent upsurge in the use of CBT for schizophrenia.15–18 CBT was originally developed as an intervention for depressive disorders19 but has been modified to address the needs of patients experiencing a variety of other mental illnesses, including anxiety disorders,20 substance dependence,21 and personality disorders,22 as well as psychotic disorders.15–18 CBT trains patients to identify problematic thoughts and behaviors and to engage in exercises (both cognitive and behavioral) that help dispute irrational or unhelpful beliefs.
Several studies15–18 have recently shown that CBT designed to challenge the beliefs underlying delusions can reduce delusional conviction, general symptomatology, and depressive symptoms in patients with schizophrenia.15 CBT directed at a patient's beliefs regarding the nature of auditory hallucinations (e.g., that voices need to be obeyed) led to reduced conviction in those beliefs, reduced distress, increased adaptive behavior, and reduced auditory hallucinations.16 Sensky et al.6 demonstrated that both CBT and a “befriending” intervention control led to reductions in psychotic symptoms. However, at 9 months post-treatment the CBT participants continued to show improvement, and those in the control condition did not. Other CBT interventions that focused on improving coping skills have also been shown to reduce positive psychotic symptoms.17,18
Social Skills Training for Schizophrenia
SST interventions employ behavioral and social learning principles to teach skills involving medication management, early detection and self-management of symptoms, coping with life stress, grooming and hygiene, interpersonal problem-solving, and conversation skills. Goals of treatment are explicit (e.g., “telling my doctor I'm experiencing side effects” as opposed to “improving communication”), sessions are clearly planned, agendas are provided in manuals and patient workbooks, and homework assignments (in vivo practice) are given. Pre-packaged SST modules23 are available that include manuals for therapist training, patient workbooks, and demonstration videos.
When used in conjunction with pharmacotherapy, SST has been validated as effective for patients with schizophrenia.7,11–14 Benton and Schroeder5 conducted a meta-analysis of 27 studies of schizophrenia patients that used SST modules and concluded that SST resulted in reduced length of hospital stay; reduced relapse rates; significant acquisition, durability, and generalization of social skills; and improved social adaptive functioning.
Limitations of CBT and SST for Schizophrenia
Although both CBT and SST have been shown to be beneficial, there are also limitations to these interventions. They are recommended only as adjunctive treatments, in the context of adequate pharmacotherapy, rather than as primary treatments.24 In addition, although studies generally show improvement in symptoms and functioning, patients do not usually become symptom-free. Rather, patients continue to have significant levels of symptoms and functional impairment.5,15–18
Older patients may have particular issues, such as health concerns and belief systems, that present special challenges. Health problems may prevent some patients from engaging in the repetitive practice required by SST and may also demoralize them. In addition, because of beliefs common among older adults (e.g., “an old dog can't learn new tricks”), some patients may hesitate to practice skills or to even engage in treatment. These problems could be alleviated by CBT interventions that focus on testing limitations and trying out new skills while learning to challenge unhelpful beliefs about aging. On the other hand, the repetitive and concrete nature of SST may provide a better learning model than CBT to compensate for neurocognitive impairments. In addition, some older patients may be less willing to be involved in “psychotherapy” because of age cohort–related biases, but more willing to participate in skills training “classes” such as SST.
Other age-related factors may limit patients' ability to benefit from SST and CBT. Many patients with schizophrenia have neurocognitive deficits in attention, memory, and executive functions. Several of these neurocognitive functions decline further with aging. Additionally, a lifetime of comorbid factors (e.g., poor education, lack of work, physical illness, poor nutrition, poverty, side effects of medications) may negatively affect cognition in older patients with schizophrenia. Greater neurocognitive impairment has been found to be associated with medication adherence problems, impaired social adaptive functioning, and poor response to psychosocial interventions,9,11,25–30 whereas severity of positive symptoms appears to be a less useful predictor of social adaptive functioning and outcome.31 Therefore, in planning interventions for older patients with schizophrenia, compensatory or remediation strategies are needed to address the neurocognitive impairments of this cohort.
In summary, integrating CBT and SST could be beneficial because
Both have been shown to be effective at reducing symptoms and in facilitating medication adherence in younger patients.
They derive from a common rationale and are complementary interventions.
Older patients have specific beliefs about not being able to change that CBT may be effective in modifying.
Older patients have specific stressors such as loss of role, loss of supports, and health problems for which CBT and SST each provides useful coping strategies.
The repetitive, concrete, practice-learning model of SST may help compensate for neurocognitive impairments.
At the same time, CBT and SST address different needs. Whereas CBT explicitly identifies distorted thinking and provides individuals with skills to modify thinking and improve functioning, SST focuses on repetitive practice of behavioral skills without emphasizing cognitions. Although the two theories overlap in common practice, to our knowledge there has not been a systematic integration of these two models designed to draw on the strengths of each. By combining these interventions, we hope to address issues that are particularly problematic in middle-aged and older patients with schizophrenia.
In addition to combining these two treatment approaches, we have incorporated additional changes to make the treatment more beneficial for older patients. Areán32 makes several recommendations for CBT with older adults, including the use of mnemonic strategies, multiple learning modalities, repetitive communication, and graded task assignments to improve retention and compensate for neurocognitive deficits. CBT interventions that include such modifications have been shown to be effective treatments for older depressed patients.33 By combining CBT and SST, with specific modifications for older individuals, we hope to improve the functioning and well-being of older patients with schizophrenia.
METHODS
Participants
A group of 10 middle-aged and older patients with schizophrenia who were enrolled in an Interventions Research Center (IRC) consented to be in this pilot study. One patient dropped out of the study before the group started. Eligibility criteria were 1) being over 45 years of age, 2) having a diagnosis of schizophrenia or schizoaffective disorder based on the Structured Clinical Interview for DSM-IV (SCID),34 and 3) being physically and psychiatrically stable enough to undergo the various assessments. The participants were representative of the IRC population, with a mean age of 62.6 years (SD=8.7, range 53–74), a mean education level of 12.8 years (SD=2.2), and with a majority of the sample being male (7 of 9) and Caucasian (6 of 9; 1 participant was African American and 2 were Hispanic). All but one participant was currently taking antipsychotic medication; 3 were on typical antipsychotic medication and 4 on atypical medication (one switched from typical to atypical antipsychotic medication during the course of the study). We were unable to determine medication type for one patient who was enrolled in a double-blind research protocol comparing typical and atypical medications. The patients had a mean baseline score on the 18-item Brief Psychiatric Rating Scale (BPRS)35 of 41.1 (SD=7.9).
Assessments
Baseline assessment for the group participants included a clinical interview to obtain a detailed history and information about current symptoms and medications. Participants completed the Sheehan Disability Scale (SDS)36 both before and after treatment, and filled out a Goals Questionnaire before treatment. The participants were asked to provide anonymous comments on their group experience at the end of treatment.
The SDS is a three-item questionnaire that assesses the degree to which a person's feelings or emotional problems disrupt his or her work, social life, and family life/home responsibilities. The scale ranges from 0 (no disruption) to 10 (marked disruption). The Goals Questionnaire, given prior to treatment, was designed for this study to ascertain which goals the patients hoped to accomplish by participating in the group. At the end of treatment, patients were asked if their goals had been met.
Development of the Intervention
We relied on several sources of information to identify critical areas to target for our intervention, including a review of the literature on the use of psychotherapeutic management of schizophrenia, our own clinical experience in working with older patients with schizophrenia, and a survey of patients in our IRC asking them about their potential treatment goals for a psychotherapy group. The intervention method that we developed included both CBT and SST components (CBSST). The CBT training was based on a manual developed by Muñoz and Miranda (unpublished). We chose this manual because it was designed to be simple and easily understood, and emphasized coping with ongoing difficulties that older people face (e.g., health problems, financial limitations) to a greater extent than other CBT interventions. Both schizophrenia and older age are associated with greater cognitive deficits, and thus the intervention included multiple modalities (written materials, group discussion, posters, and lecture) to provide information, training in mnemonic compensatory strategies, repetition of basic themes throughout the course of the group, and extensive skills practice. We chose to draw from the SST interventions developed by Liberman et al. because of evidence37 supporting their efficacy.
The intervention included three 4-session modules, for a total of 12 weekly 1-hour sessions. One module focused on cognitive-behavioral skills. The process of thought-challenging was described by using a mnemonic called the “three C's”: Catch the thought (identify cognitions), Check it (assess whether the thought contains any distortions and/or interferes with functioning), and Change it (develop alternative thoughts). This module included
Training patients in basic thought-challenging skills.
Using those skills to increase adherence with treatment recommendations, including medication and group homework compliance.
Training in coping with and preventing symptoms.
Reducing conviction regarding delusional beliefs and beliefs about hallucinations.
CBT involves identifying patient behaviors that lead to unwanted outcomes (e.g., poor medication compliance); identifying thoughts and beliefs that lead to these behaviors (e.g., “I don't need medications, they never help”); identifying the distortions in those beliefs (e.g., all-or-nothing thinking distortion such as “medication never helps”); and gathering evidence that contradicts unhelpful beliefs (e.g., “I am able to stay out of the hospital when I stay on my medication; that suggests that it helps in some way”). Patients were trained to use this process to examine their thinking, then modify their thoughts to increase healthy thoughts and behaviors. The module addressed specific issues faced by older patients with schizophrenia, including beliefs regarding ability to change; coping with chronic medical problems; coping with stressors (e.g., loss of role or supports); and dealing with sequelae of long-term neuroleptic treatment.
The next module focused on symptom self-management. In this module, several skill areas (e.g., problem-solving; identifying warning signs of relapse; managing warning signs) from the Symptom Management Module of the UCLA Social and Independent Living Skill Series23 were modified for use with elderly patients. Sessions focused on identifying relapse warning signs and developing an “emergency plan” for coping with these symptoms and preventing relapse through self-monitoring homework and role-plays on discussing symptoms with a physician. Thus, the module attempted to increase knowledge and awareness of psychiatric illness and provide coping skills for improving medication adherence and communicating better with health care providers and social support systems. Patients received information and completed exercises in workbooks (e.g., self-monitoring forms, worksheets) that emphasized communication skills and self-observation. Skills training in this module relied heavily on feedback and praise during behavioral role-plays carried out by patients in groups, as well as in vivo practice and homework assignments. The module incorporated a number of age-relevant content modifications, including age-relevant role-play situations (e.g., talking with a primary care physician about medical or sensory problems), social support (e.g., enlisting a resource person to identify warning signs in the development of the “emergency plan”), and stressors (e.g., differentiating warning signs from stress reactions to loss).
A third module focused, in part, on skills for managing persistent symptoms from the Symptom Management Module23 and was supplemented with CBT and mnemonic strategies for coping with symptoms and promoting treatment adherence. The primary focus was on coping with persisting symptoms through medication adherence strategies as well as cognitive and behavioral strategies. Mnemonic aids and environmental structuring were also provided to promote medication adherence. Patients were asked to identify and monitor persisting symptoms and practice cognitive skills (e.g., silent self-talk and “check-it-out”) and behavioral skills (e.g., distraction by music or activities) to cope with persisting hallucinations and delusions. Problem-solving and role-play techniques were also used to address the problem of persisting symptoms.
All of the patients received weekly homework assignments in all modules that were based on the three C's and the current topics of the week, and these homework assignments were reviewed in group. The final session was an evaluation and feedback session, in which patients could comment on their group experiences and discuss how to continue to use skills they had learned. The group was administered by the third and fourth authors (Ph.D.-level psychologists) under supervision by the first and second authors.
RESULTS
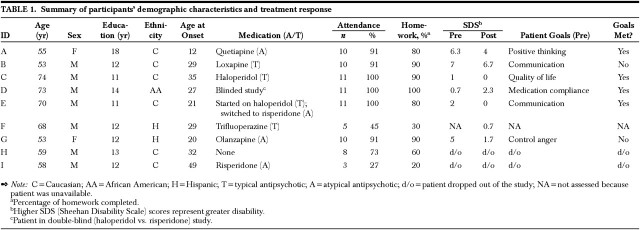
Table 1 provides a summary of responses to treatment for all participants. Because of holiday scheduling, patients received 11 sessions, with the last two treatment sessions being combined. Of the 9 patients who began group treatment, 6 attended 10 or 11 sessions, 1 attended eight, 1 attended five (missing four because of a medical illness), and 1 attended three sessions. There were 10 homework assignments, and 6 participants completed at least 80% of their homework assignments, 1 completed 60%, and another 2 (including the one with medical illness) completed at least 20% of the assignments. On the CBSST group evaluations at the end of treatment, participants' comments included the following: “Instructions were sensible and easy to follow”; “Homework size was just right”; “More time [needed for the group]”; “I gained some insights about my mental problems that I feel are important to me”; “The 3-C's [technique] is a good idea”; and “[The group] was very clear—really enjoyed hearing the other group members share.”
TABLE 1. Summary of participants' demographic characteristics and treatment response.
CASE EXAMPLES
Case 1. Ms. A. was a 55-year-old single Caucasian woman who complained of an inability to communicate assertively with family members. Ms. A. stated that her family was “in denial” about her illness and expected her to routinely provide daycare for a sibling's young children and to engage in other high-responsibility tasks. This was overwhelming for Ms. A., who said that her symptoms, including paranoid delusions, worsened as a result of these added responsibilities.
In the initial phase of treatment Ms. A. applied the 3-C's exercise to her distorted thinking, in particular her paranoid ideation. Ms. A. reported that she could use the 3-C's to reduce her endorsement of paranoid beliefs. In the second module, Ms. A. practiced assertive communication in role-plays with the therapist and other group members. Over the course of the group sessions, she said that she was able to tell her family members “no” to high-responsibility tasks with which she felt uncomfortable. Ms. A. also said that she was able to help her family better understand her illness so they would have a better sense of her capabilities and limitations. On the SDS, which assesses the extent to which a person's feelings or emotional problems disrupt work, social, and family functioning, Ms. A.'s baseline scores decreased from marked disruption to mild-to-moderate disruption following treatment.
Six months after completing the group, Ms. A. reported that she was better able to communicate with a variety of people because of the skills she had learned in the CBSST group. She remarked that she had recently read some medical texts and became convinced that she had “brain cancer.” She was concerned about speaking to her doctor, so she first role-played the situation with her boyfriend prior to speaking with her doctor. When she spoke with her primary care physician regarding her concern, he provided her with evidence contrary to her belief and suggested she immediately stop reading the book. On the basis of the data from her doctor, she labeled her belief about cancer a false belief and was able to effectively challenge her fear. Ms. A.'s description emphasized both the CBT and SST components of the intervention.
Case 2. Mr. B. was a 53-year-old married Caucasian male veteran with 12 years of education. Mr. B. had a long history of chronic paranoid schizophrenia. Mr. B. suffered from ideas of reference and paranoid delusions, including the belief that the therapists were members of the Mafia. In addition, during the fourth session of treatment Mr. B. reported that he regularly heard voices and experienced command hallucinations.
Mr. B. actively participated in the CBSST group. He was always punctual, attending all sessions but one, and compliant with his homework activities. During the initial phase of treatment, we encouraged him to apply the 3-C's to his auditory hallucinations and delusions of reference by checking the evidence for the thought that the therapists belonged to the Mafia. Mr. B. did not find these exercises particularly helpful and continued to endorse suspicions and the belief that he needed to obey his auditory hallucinations. During the second module, however, Mr. B. appeared to develop increased social awareness of others in the group and a decreased sense of mistrust and guardedness. Through the use of interactive role-playing, the emphasis on nonverbal and verbal communication techniques, and the interchange of similar experiences via class and homework activities, Mr. B. interacted more appropriately with both the group members and the group leaders, and, as a consequence, received more positive feedback.
At the end of the group therapy, Mr. B. noted that he still experienced paranoia and auditory hallucinations, but also that he had “gained insights into his mental problems” and that he felt he had been heard by the group members. In addition, he reported that for the first time he felt the psychiatric community not only understood what schizophrenia really was, but had also made genuine efforts to understand how it really feels.
Six months later during a follow-up, Mr. B. reported doing well. He had been keeping track of his warning signs, felt more trusting of his doctor, and was complying with his medications. He reported using the 3-C's technique “once in a while” but did not feel it was automatic and suggested that we have longer group sessions with more time to practice. Despite his chronic paranoia and auditory hallucinations, this group member after 12 weeks was able to interact more effectively with people, increase his trust with others, make use of simple techniques long after the group was over, monitor and manage his symptoms, adhere to his treatment plan with the doctor, and gain some insight into his illness.
DISCUSSION
This report describes the development and pilot administration of an intervention designed to provide the necessary skills for older patients with schizophrenia to manage their illness and improve their functioning. We sought to integrate two well-established, empirically validated interventions. Although our preliminary findings are limited, patients reported that they found a variety of components helpful. This feedback suggests that future evaluations of this intervention hold promise. In addition, the high levels of participation and compliance with homework suggest that participants were able to engage effectively in these exercises.
This project demonstrates 1) the feasibility of recruiting older patients with schizophrenia to participate in therapy group; 2) the active participation of members in cognitive and skills-building activities in and out of group; and 3) good treatment adherence by a majority of participants.
Nonetheless, several caveats are in order. Although some participants filled out the SDS at both pre- and post-treatment, we did not report statistical analyses because of the small sample size and uncertain reliability of the measure. In future studies, investigators should use interview- and observation-based assessments of functioning and symptom change to assess the impact of treatment, particularly since patients with schizophrenia may not provide reliable responses on self-report instruments.
There are limits to the intervention as developed, as well. The intervention tested is quite brief. Previous studies have involved interventions that lasted several months to years, and in future studies it will be necessary to address the length of treatment necessary to effect change. The current intervention allowed little time for repeated practice of each skill learned in session, and lower-functioning patients in particular may need more in-class training. Also, the use of a group format may be difficult for some patients. The patient who missed the most sessions had difficulty with paranoia, which may have been exacerbated in the group setting. It may be important to have individual therapy available for some patients.
To address some of these issues, randomized, controlled trials, in which a relevant comparison group is included, are necessary to determine whether the combined CBSST intervention adds benefits beyond standard pharmacotherapy and simple supportive contact. It will also be necessary to measure hypothesized mediators of change (e.g., social skills, improved cognitive functioning, reduced negative beliefs) to determine which proposed mechanisms of improvement are in fact contributing to better functioning. We believe that the preliminary study presented here points to a need for further work in this promising approach to treatment.
Acknowledgments
The authors are grateful to the staff of the Interventions Research Center for Psychosis in Older Adults, University of California, San Diego, for their participation in this study, especially to Ruth Rodriguez for her help in recruiting participants. The authors also thank Drs. Robert Liberman and Patricia Areán, Robert Scinta, CNS, and Patricia Cutler, CNS, for their suggestions and consultation on intervention development. Support for this work was provided, in part, by a pilot grant from the National Institute of Mental Health (Grants P30 MH49693 and MH45131), a Merit Review Grant from the Department of Veterans Affairs, and the Joseph S. Scher Young Investigator Award from the National Alliance for Research on Schizophrenia and Depression.
References
- 1.Knapp M, Kavanagh S: Economic outcomes and costs in the treatment of schizophrenia. Clin Ther 1997; 19:128–138 [DOI] [PubMed] [Google Scholar]
- 2.Williams R, Dickson RA: Economics of schizophrenia. Can J Psychiatry 1995; 40:S60–S67 [DOI] [PubMed]
- 3.Cuffel BJ, Jeste DV, Halpain M, et al: Treatment costs and use of community mental health services for schizophrenia by age-cohorts. Am J Psychiatry 1996; 153:870–876 [DOI] [PubMed] [Google Scholar]
- 4.Jeste DV, Alexopoulos GS, Bartels SJ, et al: Consensus statement. The upcoming crisis in geriatric mental health: challenges and opportunities. Arch Gen Psychiatry 1999; 56:848–853 [DOI] [PubMed] [Google Scholar]
- 5.Benton MK, Schroeder TJ: Social skills training with schizophrenics: a meta-analytic evaluation. J Consult Clin Psychol 1990; 58:741–747 [DOI] [PubMed] [Google Scholar]
- 6.Sensky T, Turkington D, Kingdon D, et al: A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry 2000; 57:165–172 [DOI] [PubMed] [Google Scholar]
- 7.Wallace CJ, Liberman RP, MacKain SJ, et al: Effectiveness and replicability of modules for teaching social and instrumental skills to the severely mentally ill. Am J Psychiatry 1992; 149:654–658 [DOI] [PubMed] [Google Scholar]
- 8.Hafner IH, Gattaz WF, Janzarik W: Search for the Causes of Schizophrenia. Berlin and Heidelberg, Springer, 1987
- 9.Yank GR, Bentley KJ, Hargrove DS: The vulnerability-stress model of schizophrenia: advances in psychosocial treatment. Am J Orthopsychiatry 1993; 63:55–69 [DOI] [PubMed] [Google Scholar]
- 10.Zubin J: Chronic schizophrenia from the standpoint of vulnerability, in Perspectives in Schizophrenia Research, edited by Baster C, Melnichuk T. New York, Raven, 1980, pp 289–294
- 11.Liberman RP: Psychosocial treatments for schizophrenia. Psychiatry 1994; 57:104–114 [DOI] [PubMed] [Google Scholar]
- 12.Penn DL, Mueser KT: Research update on the psychosocial treatment of schizophrenia. Am J Psychiatry 1996; 153:607–617 [DOI] [PubMed] [Google Scholar]
- 13.Scott JE, Dixon LB: Psychological interventions for schizophrenia. Schizophr Bull 1995; 21:621–630 [DOI] [PubMed] [Google Scholar]
- 14.Bellack AS, Mueser KT: Psychosocial treatment for schizophrenia. Schizophr Bull 1993; 19:317–336 [DOI] [PubMed] [Google Scholar]
- 15.Garety PA, Kuipers L, Fowler D, et al: Cognitive behavioural therapy for drug-resistant psychosis. Br J Med Psychol 1994; 67:259–271 [DOI] [PubMed] [Google Scholar]
- 16.Chadwick P, Birchwood M: The omnipotence of voices: a cognitive approach to auditory hallucinations. Br J Psychiatry 1994; 164:190–201 [DOI] [PubMed] [Google Scholar]
- 17.Tarrier N, Beckett R, Harwood S, et al: A trial of two cognitive-behavioral methods of treating drug-resistant residual psychotic symptoms in schizophrenic patients, I: outcome. Br J Psychiatry 1993; 162:524–532 [DOI] [PubMed] [Google Scholar]
- 18.Tarrier N, Sharpe L, Beckett R, et al: A trial of two cognitive behavioural methods of treating drug-resistant residual psychotic symptoms in schizophrenia patients, II: treatment-specific changes in coping and problem-solving skills. Soc Psychiatry Psychiatr Epidemiol 1993; 28:5–10 [DOI] [PubMed] [Google Scholar]
- 19.Beck AT, Rush AJ, Shaw BF, et al: Cognitive therapy of depression. New York, Guilford, 1979
- 20.Barlow DH: Anxiety and Its Disorders: The Nature and Treatment of Anxiety and Panic. New York, Guilford, 1988
- 21.Monti PM, Abrams DB, Kadden RM, et al: Treating Alcohol Dependence: A Coping Skills Training Guide. New York, Guilford, 1989
- 22.Linehan MM: Cognitive-Behavior Therapy for Borderline Personality Disorder. New York, Guilford, 1993
- 23.Psychiatric Rehabilitation Consultants: Modules in the UCLA Social and Independent Living Skill Series. Camarillo, CA, Psychiatric Rehabilitation Consultants, 1991
- 24.Kingdon D, Turkington D: Cognitive-Behavioral Therapy of Schizophrenia. New York, Guilford, 1994
- 25.Green MF: Cognitive remediation in schizophrenia: is it time yet? Am J Psychiatry 1993; 150:178–187 [DOI] [PubMed] [Google Scholar]
- 26.Bowen L, Wallace CJ, Glynn SM, et al: Schizophrenic individual's cognitive functioning and performance in interpersonal interactions and skills training procedures. J Psychiatr Res 1994; 28:289–301 [DOI] [PubMed] [Google Scholar]
- 27.Lysaker PH, Bell MD, Zito WS, et al: Social skills at work: deficits and predictors of improvement in schizophrenia. J Nerv Ment Dis 1995; 183:688–692 [PubMed] [Google Scholar]
- 28.Lysaker PH, Bell MD, Bioty SM: Cognitive deficits in schizophrenia: prediction of symptom change for participators in work rehabilitation. J Nerv Ment Dis 1995; 183:332–336 [PubMed] [Google Scholar]
- 29.Penn DL, Mueser KT, Spaulding W, et al: Information processing and social competence in chronic schizophrenia. Schizophr Bull 1995; 21:269–281 [DOI] [PubMed] [Google Scholar]
- 30.Marder SR: Facilitating compliance with antipsychotic medication. J Clin Psychiatry 1998; 59:21–25 [PubMed] [Google Scholar]
- 31.Green MF: What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 1996; 153:321–330 [DOI] [PubMed] [Google Scholar]
- 32.Areán PA: Cognitive behavioral therapy with older adults. The Behavior Therapist 1993; 17:236–239 [Google Scholar]
- 33.Wilson KC, Scott M, Abou-Saleh M, et al: Long-term effects of cognitive-behavioural therapy and lithium therapy on depression in the elderly. Br J Psychiatry 1995; 167:653–658 [DOI] [PubMed] [Google Scholar]
- 34.First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV Axis I Disorder–Patient Edition (SCID-I/P). New York, Biometrics Research Department, New York State Psychiatric Institute, 1995
- 35.Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychol Rep 1962; 10:799–812 [Google Scholar]
- 36.Leon AC, Olfson M, Portera L, et al: Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int J Psychiatry Med 1997; 27:93–105 [DOI] [PubMed] [Google Scholar]
- 37.Liberman RP, Putten TV, Marshall BD, et al: Optimal drug and behavior therapy for treatment-refractory schizophrenic patients. Am J Psychiatry 1994; 151:756–759 [DOI] [PubMed] [Google Scholar]