Abstract
Few data address the relationship between ethnic status and psychotherapy outcome. This study reports data from a four-cell, 16-week controlled clinical trial for HIV-positive patients with depressive symptoms. Patients (N=101) were randomized to 16 weeks of treatment with interpersonal psychotherapy, cognitive-behavioral therapy (CBT), supportive psychotherapy, or imipramine plus supportive psychotherapy. Analyses found an ethnicity-by-treatment interaction wherein African-American subjects (n=18) assigned to CBT (n=4) had significantly poorer outcomes than other patients. This is the first study to uncover an ethnicity-by–specific psychotherapy interaction. Its meaning is unclear. This charged topic requires cautious treatment, particularly given the small sample size in this study, but warrants further research.
Keywords: Human Immunodeficiency Virus–Type 1 (HIV), Depression, Ethnicity, Psychotherapy Outcome
More than a quarter of Americans are designated ethnic minorities.1 Researchers and minority advocates often assert the need to assess cultural and ethnic factors that might moderate psychotherapy outcome,2 yet few data actually address this issue. Several reports suggest that African Americans and other minorities are often underrepresented in psychotherapy treatment studies.2,3 “Clinical analog studies” using role-played “therapists” and “patients” have hinted at ethnic issues,4 but these may simply mirror the stereotypes of the actors in these artificial exercises. The few published clinical studies have failed to show a consistent effect of ethnicity on treatment outcome, not validating in particular the concern that African-American patients might fare poorly in treatment with white therapists.3,5,6
Sue et al.7 examined therapist-rated Global Assessment Scale (GAS) scores in a large Los Angeles community sample. They found that Asian Americans, especially when unacculturated, were less likely to drop out and more likely to improve when seeing ethnically matched psychotherapists, as to a lesser degree were Mexican Americans. Whites and African Americans also had lower rates of premature termination when ethnically matched to therapists, but their treatment outcomes on GAS were unrelated to ethnic match.7,8 A later study found ethnic-specific services were associated with less psychotherapy dropout than mainstream services but were not associated with differences in treatment outcome.8
Sue and co-workers,5,6,8 summarizing the literature on psychotherapy and minorities, emphasized the lack of clear-cut findings, the paucity of robust research, and the confusion of ethnic with cultural issues. We are unaware of data suggesting differential response by ethnicity to particular psychotherapies. Our study of treatments for HIV-positive individuals with depressive symptoms9 provided an opportunity to examine the potential moderating effect of ethnicity on treatment outcome.
METHODS
The methodology and outcome of this study have been reported elsewhere.9 Basically, individuals who had a known HIV infection for at least 6 months, had 24-item Hamilton Rating Scale for Depression (Ham-D)10 scores of at least 15, were clinically judged to have significant unipolar depression, and gave informed written consent were randomized to 16 weeks of one of four treatments: interpersonal psychotherapy (IPT), cognitive-behavioral therapy (CBT), supportive psychotherapy (SP), or SP with imipramine (SWI). Exclusion criteria included history of psychosis or mania, current substance abuse, known imipramine intolerance, and inability to speak English. Patients also completed the Beck Depression Inventory (BDI)11 weekly. Sessions were audiotaped and randomly assessed by independent raters, who found high levels of therapist adherence to treatment12 as rated on a modified, 104-item version of the 96-item Collaborative Study Psychotherapy Rating Scale (CSPRS).13
Overall results showed improved depression scores across groups over time, but differential benefits for IPT and SWI relative to CBT and SP. A total of 101 subjects entered the study: 58 white, 21 Hispanic, 18 African American, and 4 Asian American or other. All therapists (4 IPT, 3 CBT, 9 SP, and 6 SWI) were white; 91% were women. To minimize stigmatization of depressed HIV-positive patients, treatment was conducted in offices in a residential building, adjacent to but separate from a large tertiary-care hospital on the East Side of New York City.
Among other exploratory analyses, the researchers compared ethnic groups by using chi-square tests and assessed the moderating effects of ethnic and clinical variables on treatment outcome by using analysis of covariance (ANCOVA).
RESULTS
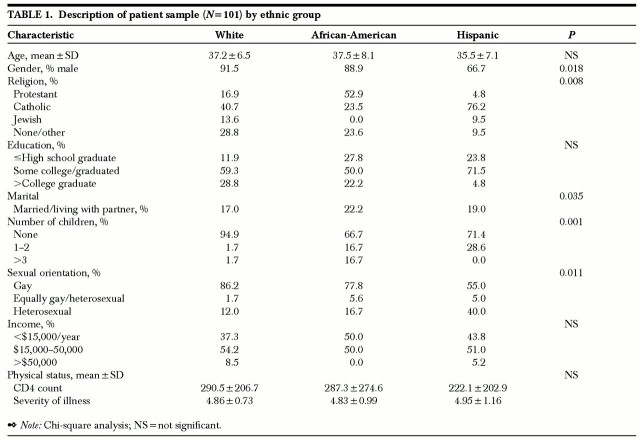
Table 1 presents demographics of the sample. Some ethnic sociodemographic differences emerged, but none was found to moderate treatment outcome. Hispanic patients were more likely than whites and African Americans to be female (χ2=7.99, P=0.018), Catholic (χ2= 29.99, P=0.008), married (χ2=16.59, P=0.035), and exclusively heterosexual (χ2=25.88, P=0.011). Whites were less likely to be separated or divorced (χ2=16.59, P=0.035) and to have children (χ2=25.59, P=0.001). There were no significant differences in income or education levels by ethnicity; no diagnostic differences on Axis I or Axis II by structured interview;14,15 and no significant differences on physical illness measures such as intake CD4 count or Karnofsky16 functional disability severity score. Furthermore, no ethnic differences appeared on independent ratings of therapist treatment adherence using the CSPRS,13 on which CBT therapists scored highest on “facilitative conditions,” a modality-nonspecific subscale of therapist warmth and other supportive behaviors.12
TABLE 1. Description of patient sample (N=101) by ethnic group.
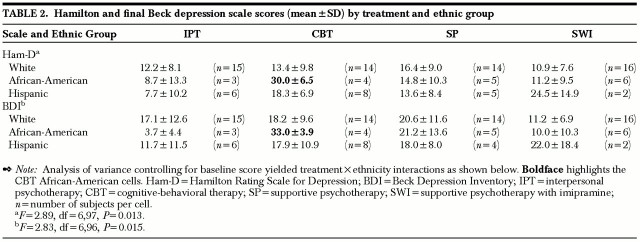
Baseline Ham-D score was 20.8±4.9 (mean±SD), with no difference across groups; final scores appear in Table 2. Analysis of variance controlling for initial score (ANCOVA) on Ham-D, the principal outcome measure, revealed a significant treatment-by-ethnicity interaction (F=2.89, df=6,97, P=0.013). Breaking this into separate analyses of variance (ANOVAs) by ethnicity within each treatment showed significant differences only for CBT (F=5.81, df=2,25, P=0.009). Post hoc (Tukey's honestly significant difference test) showed significant differences between African Americans and whites and between African Americans and Hispanics, but not between whites and Hispanics. Analogous testing of BDI scores by ANCOVA similarly showed a treatment-by-ethnicity interaction (F=2.83, df=6,96, P=0.015), significant only for CBT by ANOVA (F=4.19, df=2,25, P=0.028), with Tukey's again showing differences only for African-American subjects (Table 2). Tests for homogeneity of variance on the ANCOVAs were nonsignificant, supporting the statistical validity of the findings.
TABLE 2. Hamilton and final Beck depression scale scores (mean±SD) by treatment and ethnic group.
Subsequent analyses revealed no group attrition differences by ethnicity or treatment. Two therapists had each treated 2 of the 4 African-American CBT patients. One patient significantly improved; one dropped out for reasons of physical illness, and another dropped out because of covert substance abuse. The only female patient attended a single session, failed to appear for 6 subsequently scheduled sessions, and was finally dropped for noncompliance.
To assess the therapeutic alliance in the African-American CBT cases, an independent rater (M.S.), blind to the ethnicity issue, rated initial sessions of these subjects (n=3 for whom tapes were available) as well as age-matched non–African-American CBT patients (n=3), IPT patients (n=4), and SP patients (n=4), using the Working Alliance Inventory,17 which scores items on 7-point Likert-type scales. No statistically significant differences or obvious trends appeared on the Working Alliance Inventory total scale (mean±SD; African-American CBT patients: 5.2±1.3; other patients: CBT, 5.1±1.1; IPT, 5.3±1.3; SP, 5.5±0.7) or on its therapeutic bond, agreement on goals, or agreement on tasks subscales.
DISCUSSION
This study compared three ethnic groups, two of them minorities, in four treatments. The sample of 101 included 42% minority subjects, greater than the national average and a higher percentage than in many randomized controlled trials. Ethnicities were then dispersed into very small numbers among the four treatment cells. It should be emphasized that ethnicity did not moderate outcome for most of the treatments. An intriguing and unexpected finding, however, was the one interaction between treatment and ethnicity. Controlling for intake Ham-D and BDI scores, analyses revealed that African-American subjects assigned to CBT had poorer outcomes than did subjects from other ethnic backgrounds or in other treatments. Whereas other subjects improved over time, African-American CBT patients markedly worsened. African Americans who received other psychotherapy or pharmacotherapy had outcomes that did not differ from those of other ethnic groups.
These are preliminary data that require cautious interpretation. The sample size is quite small, and the findings had not been hypothesized a priori. They might reflect a Type I statistical error: a fluke finding of statistical significance due to chance alone. A handful of additional subjects who had different outcomes would swamp these results. (Note, for example, that the subsample of two Hispanic patients who received SWI had poor outcomes, but was too small to reach statistical significance.) Moreover, even if the results are meaningful, they might apply only to a subgroup of HIV-positive, depressive African-American subjects, rather than to a wider population.
Many (but not all conceivable) potential confounds were ruled out: neither initial depressive severity, sociodemographic factors, therapist adherence scores, nor therapeutic alliance in the initial session explained the interaction. Although no firm conclusions should be drawn from the data, the results warrant discussion.
Their explanation might lie with the therapists, the therapy, the patients, or some combination of factors. The therapists were caring, committed, and working with high morale on what they considered an important cause. CBT therapists received the highest scores for therapist warmth and other supportive behaviors on the CSPRS. Without revealing the interaction finding, we surveyed therapists after the fact about any ethnic factors they had noticed during the study. Some commented that they and the patients had been more concerned about addressing the stigma of HIV than about race.
Might the subjects have tolerated CBT better had it been delivered by African-American psychotherapists, or in a less white neighborhood? Did the otherwise competent CBT therapists lack “cultural competency,”8 knowledge of the patient's cultural milieu, that affected outcome? There is no evidence from this study that CBT therapists were more or less culturally competent than therapists in any of the other treatment conditions. It would be surprising if cultural competency were associated with some therapies but not others. What could have distinguished the CBT therapists from therapists in the other treatments, or the African-American from the Hispanic minority CBT subjects?
CBT, supportive and encouraging like IPT and SP, was however the most structured, most intrapsychically focused treatment option, and it most directly addressed cognitive distortions. This raises speculation about why African-American patients with HIV and depressive symptoms, presenting for treatment by white therapists in a wealthy white neighborhood, might have reacted negatively to CBT. Might they perhaps have felt intruded upon by the mode of therapy? Whereas IPT— which produced striking improvement in 3 African-American patients—focused on the patient's illness and environmental stressors, and SP provided reflective listening and emotional validation, CBT might have been experienced as more probing and confrontative. CBT is the only therapy in the study that asked patients to do regular homework, albeit agreed-upon homework. (We hasten to add, again, that CBT therapists were rated at least as supportive and empathic as their counterparts.)
Beutler and colleagues18 reported that moderately depressed outpatients with “high resistance potential” (i.e., a high likelihood of resisting a therapist's directives and suggestions), entered in a randomized trial of group psychotherapies, had better outcomes in a supportive, less directive treatment than in a cognitive-behavioral approach. In a similar pattern, patients with internalizing (worrying, self-punitive) coping styles had better outcomes in supportive therapy, whereas externalizing (i.e., impulsive) patients fared better in CBT treatment. These trends remained evident on 1-year follow-up.19 Might African-American subjects in our study have had particularly high “resistance” to the relatively directive CBT psychotherapists, or a particularly internalizing coping style? We unfortunately did not measure these factors.
In defense of CBT, it should be noted that 3 of the 4 African-American depressed HIV-positive subjects dropped out early, while the only completer improved. Hence this study cannot comment on the efficacy of CBT for depressive, HIV-positive African-American subjects who receive an adequate dosage of treatment. The high depression scores of African-American subjects hurt the overall CBT mean. Removing African-American subjects from statistical analyses would alter the overall study findings:9 the treatment effect no longer reaches statistical significance in intent-to-treat analyses, and is weakened to a trend level in completer samples. This, however, largely reflects the effect of diluting statistical power by shrinking the sample size by 18 (18%): the total sample of N=101 had barely reached significance for differences in treatment outcomes at P=0.05.
Could the problem lie with the patients? At one presentation of these data, an audience member warned that in racist hands these findings could be crudely misinterpreted: that the poor outcome of depressed HIV-positive African Americans in a therapy focusing on “cognition” could be taken to reflect poorly on their cognitive ability or intelligence. This idea had never occurred to the investigators, nor was it raised by journal reviewers. Although ridiculous, this distortion, once raised, seemed worth rebutting. First, nothing in the extensive cognitive therapy literature links intelligence to CBT outcome.20,21 Second, the three African-American subjects with poor outcomes for various reasons did not receive adequate exposure to CBT, while the one who did, improved. Third, this would be a global distortion based on an n of 4.
We are unaware of other data suggesting an ethnic moderation of outcome specific to CBT. The National Institute of Mental Health Treatment of Depression Collaborative Research Program study,22 which this HIV study resembled in comparing IPT, CBT, and pharmacotherapy, treated only 21 African Americans, 17 of them at one site, among 250 subjects. Its investigators have not found any effect of ethnicity on outcome (I. Elkin, personal communication, November 1998). Nor has the recent National Institute on Drug Abuse study comparing CBT, supportive expressive psychotherapy, and drug counseling23 found ethnic differences in its preliminary analyses (J. Barber, personal communication, June 1998). That these large, multisite studies recruited so few ethnic minorities underscores the need to recruit minorities, who may be wary of research protocols,24 into treatment trials. Only then can questions like the ones this study raises be definitively answered.
The pharmacotherapy literature provides an interesting related study. Wagner et al.25 treated 118 depressed HIV-positive patients in an 8-week randomized, placebo-controlled fluoxetine trial. Of the subjects, 79 (67%) were white, 22 (19%) African American, and 17 (14%) Latino. The ethnic groups did not differ in demographic or clinical characteristics. Attrition was significantly higher among Latinos (53%) than African Americans (14%) or whites (28%), but linear regression found that only baseline Ham-D scores predicted study completion. Among fluoxetine completers, 50% of African Americans (n=4 of 8) responded, compared with 84% of whites (36 of 43) treated at similar doses. (Only 3 Latinos received fluoxetine, too few for analysis.) A greater percentage of Latino subjects (4 of 5) responded to placebo than did African Americans (4 of 11) or whites (6 of 14).
Our study found no comparable difference in pharmacotherapy outcome among patients treated with imipramine. But the study by Wagner et al. treated a similar population in the same city and suffers from similar limitations. Its sample size of minority subjects was too small to draw clear conclusions, and its authors also noted that HIV status might limit generalizability of findings. We agree. On the other hand, it may be no accident that both of these reports on ethnicity and antidepressant outcome are from studies of HIV-positive patients. Given the difficulty in recruiting adequate minority samples for research studies, and the high prevalence of HIV infection among minority populations, the depressed HIV-positive population might provide the setting in which to explore possible effects of ethnicity on outcome in future research.
Ethnic and cultural issues remain highly charged yet underexplored topics in clinical research. Too much should not be made of the ethnicity-by–psychotherapy treatment interaction in this lone study. Indeed, the finding may be less meaningful in itself than as a starting point for further evidence-based exploration. The relationship between ethnicity and treatment outcome deserves examination in future research.
Acknowledgments
This work was supported in part by Grants MH46250 and MH49635 (Dr. Markowitz) from the National Institute of Mental Health. The authors appreciate the comments of Drs. Bruce Ballard, Paul Crits-Christoph, Arnold Cooper, Jeanne Miranda, Stanley Sue, and Michael Thase on versions of this material.
References
- 1.U.S. Bureau of the Census: Statistical Abstracts of the United States, 114th edition. Washington, DC, U.S. Government Printing Office, 1994
- 2.Alvidrez J, Azocar F, Miranda J: Demystifying the concept of ethnicity for psychotherapy researchers. J Consult Clin Psychol 1996; 64:903–908 [DOI] [PubMed] [Google Scholar]
- 3.Jones EE: Psychotherapists' impressions of treatment outcome as a function of race. J Clin Psychol 1982; 38:722–731 [DOI] [PubMed] [Google Scholar]
- 4.Arroyo JA: Psychotherapist bias with Hispanics: an analog study. Hispanic Journal of Behavioral Sciences 1996; 18:21–28 [Google Scholar]
- 5.Sue S: Psychotherapeutic services of ethnic minorities: two decades of research findings. Am Psychol 1988; 43:301–308 [DOI] [PubMed] [Google Scholar]
- 6.Sue S, Zane N, Young K: Research on psychotherapy with culturally diverse populations, in Handbook of Psychotherapy and Behavior Change, 4th edition, edited by Bergin AE, Garfield SL. New York, Wiley, 1994, pp 783–817
- 7.Sue S, Fujino DC, Hu LT, et al: Community mental health services for ethnic minority groups: a test of the cultural responsiveness hypothesis. Journal of Counseling Psychology 1991; 59:533–540 [DOI] [PubMed] [Google Scholar]
- 8.Sue S: In search of cultural competence in psychotherapy and counseling. Am Psychol 1998; 53:440–448 [DOI] [PubMed] [Google Scholar]
- 9.Markowitz JC, Kocsis JH, Fishman B, et al: Treatment of HIV-positive patients with depressive symptoms. Arch Gen Psychiatry 1998; 55:452–457 [DOI] [PubMed] [Google Scholar]
- 10.Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 25:56–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beck AT: Depression Inventory. Philadelphia, Center for Cognitive Therapy, 1978
- 12.Markowitz JC, Spielman LA, Scarvalone PA, et al: Psychotherapy adherence of therapists treating HIV-positive patients with depressive symptoms. J Psychother Pract Res 2000; 9:75–80 [PMC free article] [PubMed] [Google Scholar]
- 13.Hollon SD: Final Report: System for Rating Psychotherapy Audiotapes. Bethesda, MD, U.S. Department of Health and Human Services, 1984
- 14.Spitzer RL, Williams JBW: Structured Clinical Interview for DSM-III–non-patient version (SCID-NP). New York, Biometrics Research Department, New York State Psychiatric Institute, 1987
- 15.Loranger AW: Personality Disorder Examination (PDE) Manual. Yonkers, NY, DV Communications, 1988
- 16.Karnofsky DA: The clinical evaluation of chemotherapeutic agents in cancer. New York, Columbia University Press, 1949, pp 191–205
- 17.Horvath AO, Greenberg LS: Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology 1989; 36:223–233 [Google Scholar]
- 18. Beutler LE, Engle D, Mohr D, et al: Predictors of differential response to cognitive, experiential, and self-directed psychotherapeutic procedures. J Consult Clin Psychology 1991; 59:333–340 [DOI] [PubMed] [Google Scholar]
- 19.Beutler LE, Machado PPP, Engle D: Differential patient×treatment maintenance among cognitive, experiential, and self-directed psychotherapies. Journal of Psychotherapy Integration 1993; 3:15–31 [Google Scholar]
- 20.Haaga DAF, DeRubeis RJ, Stewart AL, et al: Relationship of intelligence with cognitive therapy outcome. Behavior Research Therapy 1991; 29:277–281 [DOI] [PubMed] [Google Scholar]
- 21.Haaga DAF, Dyck MJ, Ernst D: Empirical status of cognitive theory of depression. Psychol Bull 1991; 110:215–236 [DOI] [PubMed] [Google Scholar]
- 22.Elkin I, Shea MT, Watkins JT, et al: National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry 1989; 46:971–982 [DOI] [PubMed] [Google Scholar]
- 23.Crits-Christoph P, Siqueland L, Blaine J, et al: Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse collaborative cocaine treatment study. Arch Gen Psychiatry 1999; 57:493–502 [DOI] [PubMed] [Google Scholar]
- 24.Gamble VN: A legacy of distrust: African Americans and medical research. Am J Prev Med 1993; 9(6, suppl):35–38 [PubMed]
- 25.Wagner GJ, Maguen S, Rabkin JG: Ethnic difference in response to fluoxetine in a controlled trial with depressed HIV-positive patients. Psychiatric Services 1998; 49:239–240 [DOI] [PubMed] [Google Scholar]