Abstract
The authors compared the outcomes of 35 outpatients with dysthymic disorder randomized to receive either treatment with moclobemide and interpersonal therapy (IPT) or moclobemide and routine clinical management. Diagnosis was based on the ICD-10 symptom checklist. Patients were evaluated by trained raters using the 17-item Hamilton Rating Scale for Depression (Ham-D), Montgomery-Åsberg Depression Rating Scale (MADRS), Global Assessment of Functioning, and Quality of Life and Satisfaction Questionnaire at baseline, 12, 24, and 48 weeks. Patients in both treatment groups showed statistically significant improvement in all measures across time. There was a nonsignificant trend toward lower scores on Ham-D and MADRS for patients in the moclobemide plus IPT group. Longer, better-powered trials should be carried out to study the efficacy of IPT plus antidepressant medication in the treatment of dysthymic disorder.
Keywords: Psychotherapy, Interpersonal (IPT); Dysthymic Disorder; Moclobemide
Prospective studies of treatment outcomes for depressive disorders have attracted increasing interest in the last 15 years. About 12% of depressed patients do not recover in 5 years, 7% do not recover in 10 years,1 and 50% of remitters relapse within 2 years.2,3 The risk of chronicity increases with each new episode.3 About 25% of depressed patients had had intermittent minor depressive symptoms or dysthymic disorder prior to the index episode, and most of them continue to have symptoms after remission of the episode (residual major depression or dysthymic disorder).4,5 Depression may present clinically in a more severe form (single-episode major depression, recurrent major depression, or bipolar disorder) or as a more subtle and chronic clinical form of depression (dysthymic disorder). The severe and chronic forms may occur together in so-called double depression.
Empirical studies in the 1970s influenced psychiatric nosology, underscoring the recurrence of major depressive disorder and improving and validating the diagnosis of dysthymic disorder. However, dysthymic disorder is still underrecognized and undertreated.6 It has a lifetime prevalence of about 3% to 6% in the general population and up to 36% among psychiatric outpatients. Most dysthymic patients present with comorbidity, and 40% have associated major depressive episodes (double depression).6
Studies consistently show that antidepressants are effective in the treatment of double depression. Studies with pure dysthymic patients show improvement with selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs).7 Unfortunately, this efficacy is not always spectacular: about 50% of patients do not respond to medication, others cannot tolerate adverse effects, some refuse to take it, and some become hypomanic.8 A multicenter controlled, randomized double-blind clinical trial compared the efficacy of 12 weeks of sertraline, imipramine, and placebo for “pure” dysthymic patients (with no major depression associated)6 and found significant improvement with active drug treatment. However, a significantly greater number of patients in the imipramine group discontinued the treatment because of adverse effects. Placebo response rates for dysthymia, usually around 20%,9 were surprisingly high in this clinical trial, around 40%.6 In other studies, moclobemide, a reversible MAOI, has been used successfully and has been well tolerated with dysthymic patients.10,11
Studies on the efficacy of psychotherapy in dysthymia are not as advanced. Dysthymic disorder is a challenging potential field for psychotherapy research because of its low placebo response rate. A major study in this area has just been published. It compared nefazodone alone, CBASP (Cognitive-Behavioral Analysis System of Psychotherapy—an amalgam of cognitive, behavioral, interpersonal, and psychodynamic techniques) and combined nefazodone/CBASP in 682 patients with either chronic major depression or double depression. In the 12-week acute phase, roughly half of subjects in each monotherapy responded, compared with 75% of patients on combined therapy.12
Cognitive-behavioral therapy (CBT), a brief, structured psychotherapy developed by Beck et al.,13 has proven efficacious in a series of clinical trials for major depression. Several cognitive approaches have been tested in dysthymia treatment.14–16 Most of the studies had small samples and heterogeneous populations, used varying outcome measures, and sometimes employed a single therapist.
Interpersonal therapy (IPT), like CBT, is a manualized, time-limited psychotherapy that has had its efficacy tested in controlled clinical trials for major depression and other diagnoses.17,18 In IPT, the therapist helps the patient recognize the links between depressed mood and interpersonal experiences. The therapy is focused on one or more of four interpersonal problems areas: grief, role dispute, role transition, or interpersonal deficits.8 Some authors found positive results when using interpersonal approaches for dysthymic patients.19–22 Researchers at Cornell University Medical College developed a manual that adapts IPT to dysthymic disorder (IPT-D).8,9 IPT has been tested in some trials,23,24 and large trials are under way, including one by John C. Markowitz, M.D. (J.C.M.) and colleagues. Steiner et al.25 compared IPT, sertraline, and IPT plus sertraline in 707 dysthymic patients in the community. Sertraline with or without IPT appeared to have greater efficacy than IPT alone and combined treatment, and combined treatment was no better than sertraline. But IPT was associated with lower follow-up health care and social service costs, making it cost-effective and the combined treatment group the best overall.25
The prevalence of dysthymic disorder in developing countries such as Brazil is not well established. Psychotherapies adapted for testing in empirical studies, such as IPT, have not been widely disseminated in Portuguese. Our study aimed to evaluate the applicability of IPT with Brazilian patients of lower socioeconomic background. Such data might help in planning a larger clinical trial to test the effectiveness of IPT with patients with dysthymic disorder from developed settings.
METHODS
Participants were selected from referrals to the psychiatric outpatient clinics of a public hospital (Hospital do Servidor Publico Estadual) and a teaching hospital (Santa Casa de São Paulo). Trained psychiatrists carried out a diagnostic assessment using the ICD-10 symptom checklist.26 Participants were eligible for the trial if they were between 18 and 60 years old and met diagnostic criteria for dysthymic disorder (ICD-10). A concurrent diagnosis of major depression was permissible. Patients were classified according to early or late onset and presence of psychiatric comorbidity such as anxiety and personality disorders. Subjects were excluded if they had a current or lifetime diagnosis of bipolar disorder; substance abuse in the prior 6 months; psychosis; or dementia. Major medical diseases and history of seizures were also excluding criteria. Women who might get pregnant during the study period had to be using a reliable contraceptive method. Patients who were already in psychotherapy or taking antidepressants were excluded.
Patients who met eligibility criteria and signed the informed consent were randomized to either the experimental (IPT+moclobemide) or control (moclobemide+routine care) groups. Randomization was stratified by gender and early or late onset.
The study used flexible doses of medication. Moclobemide was administered at 150 mg bid during the first week and at 300 mg bid thereafter. Psychiatrists were encouraged to follow the dosing schedule but were free to adjust dosage for each patient. Patients received medication for 8 months (acute plus maintenance phase). This scheme was used for patients in both the experimental and the control groups, and all patients received the same number of medical consultations. During clinical consultations, patients in the control group received unstructured psychoeducational orientation as well as clinical assessments. Psychiatrists were oriented to avoid psychotherapeutic interventions. The four psychiatrists responsible for the clinical management of patients in both groups attended a basic communicational, psychotherapeutically oriented intervention course run by the main investigator (M.F.M.) and were supervised throughout the study.
Patients in the experimental group received IPT adapted to dysthymic disorder (IPT-D). A senior psychiatrist (M.F.M.) with psychotherapy experience provided IPT-D. IPT training was acquired by reading published IPT material, by attending an IPT course at the American Psychiatric Association Annual Meeting, and by contacts with an IPT therapist (J.C.M.). Patients received 16 weekly sessions during the acute phase and 6 monthly booster sessions during maintenance phase.
Baseline status and outcome were assessed by using a number of measures: The Global Assessment of functioning Scale (GAF);27,28 the last part (general activities) of the Quality of Life Enjoyment and Satisfaction Questionnaire (QOLE);29 the Hamilton Rating Scale for Depression, 17-item version (Ham-D);30,31 and the Montgomery-Åsberg Depression Rating Scale (MADRS).32 Trained interviewers completed all assessments at baseline and at 12, 24, and 48 weeks. They were blind to treatment assignment, and subjects were oriented not to tell them which group they were in.
Categorical variables were compared by type of treatment, using Fisher's exact test. Mean scores on the Ham-D, MADRS, GAF, and QOLE were compared by using an analysis of variance model (ANOVA) for two factors, treatment (medication alone [with clinical follow-up] and IPT+medication) and observation times (baseline and 12, 24, and 48 weeks). Tukey's method was used to indicate at which points in time statistically significant differences in mean scores were observed.
The clinical trial followed ethical requirements for medical research in Brazil. The hospitals' Ethical Committees approved it, and patients signed an informed consent form. Treatment was free of charge, and patients who dropped out of the study continued to receive regular clinical treatment.
RESULTS
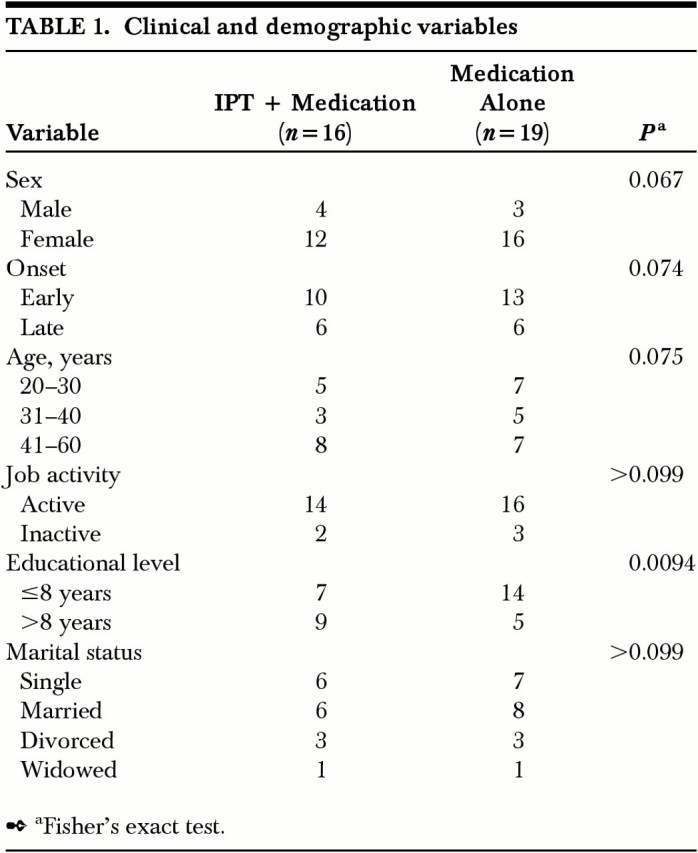
Thirty-five patients were included in the study and were randomized to receive either IPT plus medication (n=16) or medication alone (n=19). The two groups did not differ by sex, type of onset, age, job activity, or civil status (Table 1). There was a difference, not statistically significant, in educational level between groups, with a higher proportion of individuals with lower education in the control group. Thirty-two patients (91%) had double depression. Other psychiatric comorbidities included 9 patients (26%) with somatoform disorder, 9 (26%) with generalized anxiety disorder, 5 (14%) with panic disorder, 4 (11%) with social phobia, and 3 (9%) with agoraphobia. The two groups received similar mean doses of moclobemide during the trial (IPT+medication group: 460.71 mg/day, SD=124.71; moclobemide-alone group: 490.90 mg/day, SD=117.93).
TABLE 1. Clinical and demographic variables.
Six patients (37.5%) from the IPT group dropped out of the study. One of them was assessed at 12 and 24 weeks and was included in the analysis; this patient changed medication because of a lack of efficacy after 24 weeks and left the study. The other 5 patients who dropped out did so for unknown reasons before the second assessment. Eleven patients (57.9%) from the medication-alone group dropped out of the study. Six were assessed before 24 weeks and were included in the analysis; of these, 3 abandoned the trial because of treatment inefficacy, 2 because of medication intolerance, and 1 because of a manic episode. Five other patients initially assigned to the medication-alone group abandoned the trial for unknown reasons before a second assessment.
Dropouts differed from subjects who completed the study. They had lower education and more job inactivity, and they tended to be younger or older (Table 2). They did not differ in mean depression severity at baseline, as measured by the Hamilton Rating Scale for Depression (dropouts, 24.6; completers, 25.9; P=0.88).
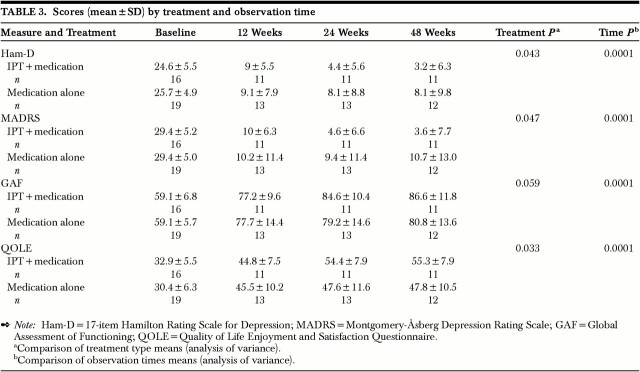
TABLE 3. Scores (mean±SD) by treatment and observation time.

Therefore, of the 35 patients initially randomized, 25 had at least one outcome assessment (14 in the medication-alone group and 11 in the IPT+medication group) and were included in the analysis. Eighteen patients completed the 48-week trial.
ANOVAs showed statistically significant associations between time and mean scores on Ham-D, MADRS, GAF, and QOLE. For both treatment groups, mean scores decreased with time, particularly between baseline and 12-week assessments. Tukey's method with global 95% confidence coefficient confirmed that for all scales, improvement was due to the difference between baseline and 12-week assessments. For QOLE, the 12-week assessment also differed from the 24-week and 48-week assessments. ANOVA did not show statistically significant differences in mean scores of Ham-D, MADRS, GAF, and QOLE between the experimental and control groups (for all scores, P>0.30). However, there was a trend for patients in the experimental group to continue to improve after 12 weeks of follow-up (Table 3 and Figure 1).
TABLE 2. Clinical and demographic variables and dropout.
FIGURE 1.
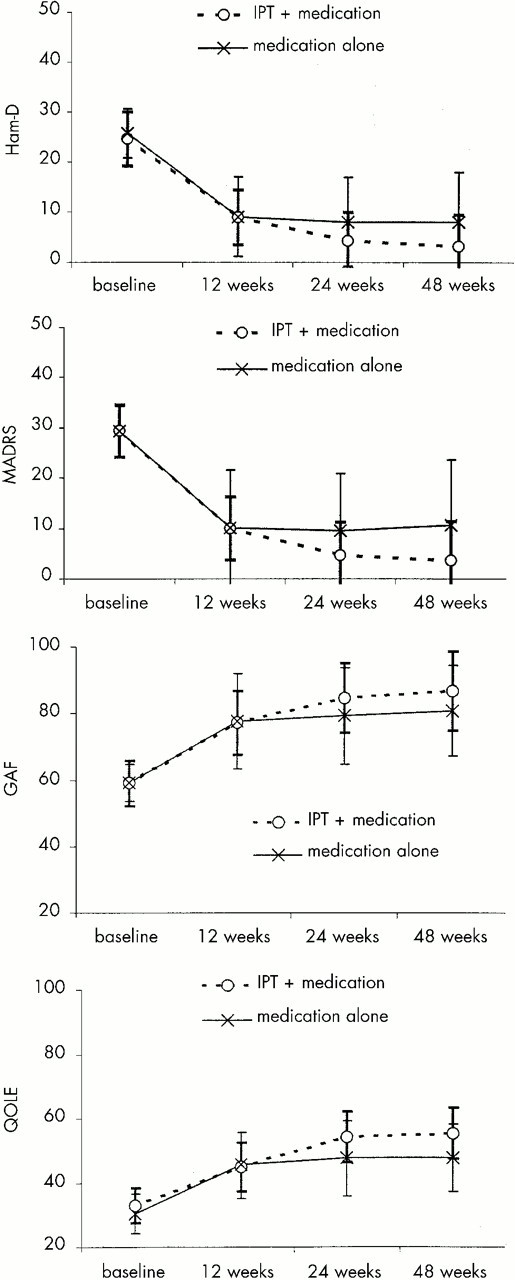
Mean scores by treatment and observation time
DISCUSSION
Both groups in the present study improved over time, and there was a nonsignificant trend for additional gains in the IPT+medication group. The main limitation of this study is its sample size, which was too small to detect statistically significant differences between experimental and control groups. Another limitation was the use of a single psychotherapist. The study might also have benefited from a longer period of treatment and the assessment of social skills and therapeutic alliance with standardized scales.
Patients in the IPT+medication group developed a good therapeutic alliance, and fewer dropped out than in the control group (6/16 and 11/19, respectively). After initially seeming skeptical, patients became involved with the IPT propositions, accepting the therapeutic optimism and seeking success experiences. The trend toward continuous improvement in the experimental group makes sense considering that medication shows its benefits early and psychotherapy usually takes longer to work. Klerman et al.33 found that it took months to measure the new social skills in IPT patients as opposed to medication patients. Perhaps some patients initially profited from the moclobemide and then were able to use those gains to work better in psychotherapy.
The present study was a pilot study; the results point to the need for larger trials with enough statistical power to detect modest effects when comparing IPT+medication with medication alone in the treatment of dysthymia. Results also showed that IPT conducted in Portuguese can be applicable to Brazilian dysthymic patients of lower socioeconomic status.
The high likelihood of a chronic course for depression underscores the need to identify treatments that are more efficient. Lima and Moncrieff,34 in a systematic review of 15 selected clinical trials, found a similar efficacy for the TCAs, SSRIs, MAOIs, and others (sulpiride, amineptine, and ritanserin) for treatment of dysthymic disorder. The average dose in the studies reviewed was 200 mg per day of imipramine or equivalent. TCA dropout tended to be related to adverse reactions to medication. On the basis of available evidence, antidepressant medication should be considered the treatment of choice for dysthymic patients. However, the combination treatment (pharmacology and psychotherapy) deserves further study. A SPECT study35 showed that IPT promotes cerebral blood flow changes different from those seen for venlafaxine in patients with major depression. The efficacy of psychotherapies for dysthymic disorder, both as adjunctive treatment and as monotherapy, must be evaluated.
Dysthymic disorder remains a treatment challenge for the psychiatrist. Besides the great pain that dysthymic disorder provokes in sufferers and their families, it also has a huge social and economic impact. Therefore, it cannot be seen as a soft diagnosis.
Acknowledgments
The authors give special thanks to John C. Markowitz, M.D., who generously did a careful review of this paper.
This trial was partially funded by Fundaçãao de Amparo à Pesquisa do Estado de São Paulo, Grants 97/1511-4 and 97/04734-4.
References
- 1.Mueller TI, Keller MB, Leon AC, et al: Recovery after 5 years of unremitting major depressive disorder. Arch Gen Psychiatry 1996; 53:794–799 [DOI] [PubMed] [Google Scholar]
- 2.Belsher G, Costello CG: Relapse after recovery from unipolar depression: a critical review. Psychol Bull 1988; 104:84–96 [DOI] [PubMed] [Google Scholar]
- 3.Coryell W, Winokur G: Course and outcome, in Handbook of Affective Disorders, 2nd edition, edited by Paykel ES. New York, Guilford, 1992, pp 89–98
- 4.Keller MB, Lavori PW, Endicott J, et al: “Double depression”: two year follow-up. Am J Psychiatry 1983; 140:689–694 [DOI] [PubMed] [Google Scholar]
- 5.Keller MB, Lavori PW, Rice J, et al: The persistent risk of chronicity in recurrent episodes on non bipolar major depressive: a prospective follow-up. Am J Psychiatry 1986; 143:24–28 [DOI] [PubMed] [Google Scholar]
- 6.Thase MS, Fava M, Halbreich U, et al: A placebo-controlled randomized clinical trial comparing sertraline and imipramine for the treatment of dysthymia. Arch Gen Psychiatry 1996; 53:777–784 [DOI] [PubMed] [Google Scholar]
- 7.Friedman RA, Kocsis JH: Pharmacotherapy for chronic depression. Psychiatr Clin North Am 1996; 19:121–132 [DOI] [PubMed] [Google Scholar]
- 8.Markowitz JC: Psychotherapy for dysthymic disorder. Psychiatr Clin North Am 1996; 19:133–149 [DOI] [PubMed] [Google Scholar]
- 9.Markowitz JC: Interpersonal Psychotherapy for Dysthymic Disorder. Washington, DC, American Psychiatric Press, 1998
- 10.Stabl M, Biziere K, Schmid-Burgk W, et al: Review of comparative clinical trials: moclobemide vs. TCAs and vs. placebo in depressive states. J Neural Transm 1989; 28(suppl):66–89 [PubMed]
- 11.Versiani M, Amrein R, Stabl M: Moclobemide and imipramine in chronic depression (dysthymia): an international double-blind, placebo-controlled trial. International Collaborative Study Group. Int Clin Psychopharmacol 1997; 12:183–193 [DOI] [PubMed] [Google Scholar]
- 12.Keller MB, McCullough JP, Klein DN, et al: The acute treatment of chronic major depression: a comparison of nefazodone, cognitive behavioral analysis system of psychotherapy, and their combination. N Engl J Med 2000; 342:1462–1470 [DOI] [PubMed] [Google Scholar]
- 13.Beck AT, Rush AJ, Shaw BF, et al: Cognitive Therapy for Depression. New York, Guilford, 1979
- 14.Gonzalez LR, PM, Clarke GN: Longitudinal follow-up of unipolar depressives: an investigation of predictors of relapses. J Consult Clin Psychol 1985; 53:461–469 [DOI] [PubMed] [Google Scholar]
- 15.Harpin RE, Liberman RP, Marks I, et al: Cognitive-behavior therapy for chronically depressed patients: a controlled pilot study. J Nerv Ment Dis 1982; 170:295–301 [DOI] [PubMed] [Google Scholar]
- 16.McCullough JP: Psychotherapy for dysthymia: a naturalistic study of ten patients. J Nerv Ment Dis 1991; 179:734–740 [PubMed] [Google Scholar]
- 17.Weissman MM, Markowitz JC, Klerman GL: Comprehensive Guide to Interpersonal Psychotherapy. New York, Basic Books, 2000
- 18.Klerman GL, Weissman MM: New Applications of Interpersonal Therapy. Washington, DC, American Psychiatric Press, 1993
- 19.Akiskal AS: Towards a definition of dysthymia: boundaries with personality and mood disorders, in Dysthymic Disorder, edited by Burton SW, Akiskal AS. London, Gaskell, 1990, pp 1–12
- 20.Cassano GB, Perugi G, Maremmani I, et al: Social adjustment in dysthymia, in Dysthymic Disorder, edited by Burton SW, Akiskal AS. London, Gaskell, 1990, pp 78–85
- 21.Goldberg DP, Bridges KW: Epidemiological observations on the concept of dysthymic disorder, in Dysthymic Disorder, edited by Burton SW, Akiskal AS. London, Gaskell, 1990, pp 104–122
- 22.Hirschfeld RMA: Personality and dysthymia, in Dysthymic Disorder, edited by Burton SW, Akiskal AS. London, Gaskell, 1990, pp 75–77
- 23.Mason BJ, Markowitz J, Klerman GL: IPT for dysthymic disorder, in New Applications of Interpersonal Therapy, edited by Klerman GL, Weissman MM. Washington, DC, American Psychiatric Press, 1993, pp 225–264
- 24.Markowitz JC, Moran ME, Kocsis JH, et al: Prevalence and comorbidity of dysthymic disorder among psychiatric patients. J Affect Disord 1992; 24:63–71 [DOI] [PubMed] [Google Scholar]
- 25.Steiner M, Browne G, Roberts J, et al: Treating dysthymia in primary care: sertraline versus interpersonal therapy, in New Research Program and Abstracts, 153rd Annual Meeting of the American Psychiatric Association (abstract). Washington, DC, American Psychiatric Association, 2000, p N92B
- 26.Sartorius N, Janca A: Psychiatric assessment instruments developed by the World Health Organization. Soc Psychiatry Psychiatr Epidemiol 1996; 31:55–69 [DOI] [PubMed] [Google Scholar]
- 27.Endicott J, Spitzer RL, Fleiss JL, et al: The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33:766–771 [DOI] [PubMed] [Google Scholar]
- 28.American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th edition. Washington, DC, American Psychiatric Association, 1994
- 29.Endicott J, Nee J, Harrison W, et al: Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacol Bull 1993; 29:321–326 [PubMed] [Google Scholar]
- 30.Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamilton M: Symptoms and assessment of depression, in Handbook of Affective Disorder, edited by Paykel ES. Edinburgh, Churchill Livingstone, 1982, pp 42–46
- 32.Montgomery AS, Åsberg MA: A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 139:382–389 [DOI] [PubMed] [Google Scholar]
- 33.Klerman GL, DiMascio A, Weissman MM, et al: Treatment of depression by drugs and psychotherapy. Am J Psychiatry 1974; 131:186–191 [DOI] [PubMed] [Google Scholar]
- 34.Lima MS, Moncrieff J: Drug versus placebo for dysthymia. Cochrane Reviews, in The Cochrane Library (CD-ROM and Internet). Oxford, UK, Update Software Ltd., 1999, issue 1; abstract at www.update-software.com/ccweb/cochrane/revabstr/ ab001130.htm
- 35.Martin SD, Rai SR, Martin E, et al: SPECT changes with interpersonal psychotherapy versus venlafaxine for depression. American Psychiatric Association Annual Meeting: Syllabus and Proceedings Summary. Washington, DC, American Psychiatric Association, 2000, p 45