Abstract
Interpersonal psychotherapy (IPT) has demonstrated efficacy in the individual treatment of antepartum and postpartum depression. The current investigation extends prior work by examining the efficacy of a group IPT approach for the treatment of postpartum depression. Depression scores of 17 women diagnosed with postpartum depressive disorder (DSM-IV criteria) decreased significantly from pre- to post-treatment. Follow-up assessments at 6 months revealed continuation of the treatment effect. Results indicate that IPT adapted for a group model has positive implications for the treatment of postpartum depression, demonstrating both short-term and longer-term effects in the reduction of depressive symptomatology. Study limitations include the small sample size, absence of control group, possible bias in therapist's assessments, and lack of monitoring adherence, which may have jeopardized the accuracy of the results.
Keywords: Depression, Postpartum; Psychotherapy, Group; Psychotherapy, Interpersonal (IPT)
Postpartum depression (PPD) is a commonly occurring condition, affecting between 10% and 15% of women in the first few months after childbirth. If PPD is detected and treated early, the prognosis is good.1 Several psychotherapeutic approaches have been adapted specifically for use in treating women suffering from antenatal2 and postpartum depression,3,4 both in group settings and individual therapy.
Interpersonal psychotherapy (IPT) was developed in the United States by Klerman, Weissman, and colleagues5 and was selected by the authors because it is brief and focuses on specific problem areas relevant to pregnancy and the birth of a child. These foci include interpersonal dispute, role transition, grief, and, although less emphasized, interpersonal deficits. IPT has been adapted to address specific postpartum-related issues,4 including the relationship with the baby, the relationship with the partner, and the transition back to work. IPT incorporates specific techniques such as clarification, communication analyses, and behavior change techniques (including role play).
IPT was first adapted for use in a group setting in the treatment of bulimia.6 The current study is a pilot test of a group format of IPT for the treatment of postpartum depression. The group provides an interpersonal milieu for members to work on their identified problem areas. Postpartum women, who tend to be socially isolated, may particularly benefit from the support and empathy provided by the group.
METHODS
Sample
An open-trial pilot of group-format IPT was conducted at a university hospital in Vienna, Austria. This clinical sample presented at 4 to 45 weeks postpartum (mean=19 weeks, SD=12.9) to a maternal mental health service, either after referral or through advertisement. Thirty-four women were recruited, and after screening for depression, 22 were eligible for the treatment trial. The final group of participants comprised 17 Caucasian women (mean age=32 years, range 27–41).
All of the 22 women eligible to participate suffered from a depressive disorder that had developed within 6 months of the birth of a child. Those 5 who chose not to participate attributed their unwillingness to transportation or childcare difficulties or reluctance to be treated in the context of a trial. The study included repeated assessments and videotaping, and as treatment can be obtained easily and free of charge within the Viennese health care system, this represented an inconvenience for several of the participants. All participants had given birth within the last 12 months, were fluent in German, and were physically healthy. Of the 17 participants, 15 had a DSM-IV diagnosis of major depressive disorder and 2 were diagnosed with minor depressive disorder according to DSM-IV diagnostic research criteria.7 Minor depression was included in this treatment trial because it appears to be a relevant disorder for women of childbearing age.8 In addition to the diagnoses, all women who were selected to participate met a specified symptom severity level, specifically, a Hamilton-Rating Scale for Depression (21 items) score greater than 13.9 Exclusion criteria included substance dependence diagnoses, acute suicidality, and current psychosis.
Fifteen participants were on maternity leave (commonly up to 2 years in Austria), 1 was unemployed, and 1 was a housewife. Ten women were primiparous. Fourteen participants had a partner and 3 were single. Ten women had a history of major depression (2 a history of PPD), 9 had current comorbid anxiety and/or phobic disorders, and 3 suffered from a personality disorder (Clusters B and C). After a detailed description of the study to the participants, written informed consent was obtained. Two separate groups (10 and 7 participants) were conducted; each group was led by the first author, who is a certified IPT therapist and received her training at Cornell University Medical College, New York, NY, and a co-therapist who was trained by the first author. Eleven women completed the entire protocol and 6 terminated early (mean number of sessions for all women=8.7). Thirteen women were available for a 6-month follow-up.
Treatment
Adaptations From Other Protocols:
A manualized adaptation of IPT to group therapy was undertaken by Wilfley et al.6 for the diagnosis of binge eating. This IPT group approach was similar to IPT for depression and had equivalent stages, strategies and techniques, and therapeutic style. This time-limited group therapy is defined as semistructured, focuses on outside interpersonal relationships, and is action-oriented.10 It is compatible with an interactive approach that fosters direct communication between members.11 In our pilot study we used the Wilfley group approach with some modifications (described later). Prior to treatment, our participants received two 60-minute individual sessions to explain how IPT works within a group and to identify the focus of treatment. Nine weekly 90-minute group sessions and one 60-minute individual termination session followed. Consistent with other authors,2,4 we also chose 12 as the total number of sessions. Three women needed individual crisis intervention in the middle phase, which augmented their total number of sessions. Wilfley's most recent IPT approach now includes individual sessions for each member in the middle phase in order to emphasize the work on the individual problem area.12 The current investigation also included adaptations of IPT for postpartum depression—in particular, additional problem areas regarding childbirth and motherhood.4,13
Stages of Postpartum Group IPT Approach:
Initial sessions (session 1–2) were held individually and were designed to review the symptoms, the diagnosis, and previous history of disorder with the patient. The medical model of depression was explained to the patient, who was encouraged to accept the “sick role.” The therapist helped the patient to relate her conflicts in the interpersonal or social domain to the onset or maintenance of her illness. Therapist and patient discussed possible conflict areas and began an inventory of past and current relationships in order to understand the patient's interpersonal life. Lastly, the patient and therapist jointly identified the predominant conflict related to the depression and agreed upon making this the main focus of therapy during the group sessions.
Middle sessions (sessions 3–9) were used to address each patient's individual problem areas within the group context and the specific intervention strategies as specified by Weissman et al.;5 these problem areas were easily applied in the group setting. The following group processes need to be considered at this stage in order to manage the group effectively: engagement (patients learn how to interact with one another), differentiation (patients acknowledge that there is conflict and learn coping mechanisms), and the work stage (patients develop intimacy).12
Final sessions (10–12) were spent evaluating the treatment goals and newly developed skills and discussing early symptoms of relapse. The loss of the newly developed bond with the therapist and group members should be the most important theme at the termination phase.12
These stages of developing relationships within the group allow the patients to work through the process of developing intimate bonds and sustaining and ending important relationships.12
Therapeutic Focus:
A group setting has the same goal as individual therapy, namely to improve interpersonal relationships and decrease symptoms. Maintaining a focus on each individual's problem areas while at the same time using the group process as a therapeutic ingredient is a constant challenge for the therapist. The group setting aims to facilitate the transfer of interpersonal skills that are developed during the group meetings so that they will be more readily applicable in the external social arena. Also, conducting a therapy group with patients suffering from the same diagnosis may help the patients to break patterns of social isolation and increase their recognition of how detrimental self-stigmatization can be.12
In the actual treatment, the group members were provided with each other's telephone numbers to facilitate contact and minimize isolation. This contact-enhancing approach was first used in a group psychotherapy model developed for postpartum depression,14 and we applied this approach because we felt it might help to decrease social isolation among group members.
What sets the IPT approach apart from a support group is the structural outline of the three phases of treatment of IPT—the provision of an interpersonal definition of depression, the definition of a problem area, and the use of specific techniques to improve interpersonal relationships outside the therapeutic setting, thus ultimately reducing depressive symptoms of the patient. Within the IPT framework, socializing between group members is discouraged by the Wilfley protocol, reflecting a major difference from our protocol.
A group approach provides an opportunity for members to work on interpersonal issues they experience in the outside world. There are many different types of interpersonal interactions in a group approach, and the interpersonal skills that are developed may be more transferable to the external social arena than is the pattern addressed in an individual setting.6 The difficult task is to maintain the integrity of elements of the individual IPT format while adapting them to the group context.10 The adaptation of IPT across psychiatric disorders and modalities is a difficult but worthwhile task.12
Diagnostic Assessment
Baseline Axis I diagnoses were obtained by a trained psychiatrist (C.K.) via the Structured Clinical Interview for DSM-IV-German version (SCID-I)7 and Axis II diagnosis via the Structured Clinical Interview for DSM-IV-German version (SCID-II).15 The SCID is a semistructured clinical interview based on the Diagnostic and Statistical Manual of Mental Disorders and yields both current and lifetime diagnoses of Axis I and Axis II disorders.
Several assessment measures of depressive symptoms and interpersonal functioning were administered. The Hamilton Rating Scale for Depression–German version (Ham-D-21) is an investigator-based instrument that is widely used in treatment trials to assess severity of depression and change.9 The Edinburgh Postnatal Depression Scale (EPDS) is a 10-item self-rating scale specifically designed to screen for postpartum depression. The items are rated on a scale from 0 to 3 and refer to symptoms of depressed mood, anhedonia, guilt, anxiety, and suicidal ideation, as experienced in the last 7 days. The German version of the EPDS yielded acceptable psychometric properties.16 The Inventory of Interpersonal Problems (IIP)17 is a self-assessment measure of interpersonal problems and the level of distress arising from interpersonal problems; it was used to assess changes in interpersonal functioning. This 64-item IIP scale consists of eight subscales: domineering, vindictive, cold, socially avoidant, nonassertive, exploitable, overly nurturant, and intrusive.
Changes in the marital relationship were assessed with the Dyadic Adjustment Scale (DAS) by Spanier.18 This is a 32-item scale designed for married or unmarried cohabiting couples. Adjustment is rated on four subscales: dyadic satisfaction, dyadic cohesion, dyadic consensus, and affectional expression. The scale distinguishes between married and divorced individuals.
Analytic Strategy
Treatment outcome was evaluated by using measures of depressive symptomatology and interpersonal functioning collected at baseline, at post-treatment, and at 6-month follow-up. The EPDS16 and the Ham-D-219 were used to assess depression severity and change, and the IIP was used to assess changes in interpersonal functioning.17 Changes in the marital relationship were assessed via the DAS.18 Endpoint analysis19 was used to estimate the level of depression and functioning at termination of the therapy regardless of when in the protocol it occurred.
RESULTS
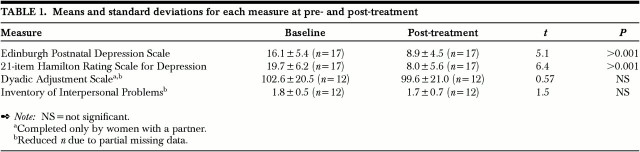
Mean score comparisons revealed a significant change from baseline to post-treatment for both EPDS and Ham-D-21 scores (Table 1). However, there were no significant differences on the IIP or the DAS total scores. Means are reported with standard deviations throughout this section.
TABLE 1. Means and standard deviations for each measure at pre- and post-treatment.
There was no difference on depression scores at the beginning of the treatment between those who completed treatment (n=11) and those who terminated early (n=6). However, these two groups differed on levels of marital satisfaction on the DAS, with the early termination group reporting less satisfaction with their marriages (mean=76.3±7.0) than those who stayed in treatment (110.1±14.5; t= 3.82, df=11, P<0.01).
Examination of individual Ham-D-21 score profiles revealed that 10 of 17 women (58%) demonstrated a full remission (posttreatment score <9). The criterion for full remission is defined as <8 points on the Ham-D 17-item scale.20 Because we used the 21-item scale in our study, we adapted the remission criteria, increasing the value by one point. Five of 17 women (29%) demonstrated a partial remission (score decrease >50%) at the end of treatment. Only 2 participants (11%) demonstrated no improvement.
There was no difference in baseline depression scores between fully remitted women and those who responded only partially or not at all; however, these groups differed on two IIP subscale scores at the time of the first assessment. Specifically, fully remitted women were initially less socially avoidant (mean=10.5±6.5) than women with partial or no remission (21.3±5.3; t=3.50, df=13, P<0.01), and fully remitted women were initially less vindictive (8.9±3.4) than those with partial or no remission (12.8±1.8; t=2.80, df=13, P<0.01). There were no demographic differences in age, parity, marital status, or occupational status between women who terminated early and those who completed the full course of treatment. A subset of the sample (n=13) was available for follow-up assessment at 6 months post-treatment. This subset consisted of 10 of the 11 women who completed the trial and 3 of the 6 who terminated early.
To examine whether treatment effects persisted, two separate multivariate analysis of variance tests were conducted, with the EPDS and Ham-D-21 treated as repeated measures. Participants' depression scores at the 6-month follow-up were significantly lower than at baseline (EPDS: F=24.30, df=1,12, P<0.001; Ham-D-21: F=33.59, df=1,12, P<0.001). Furthermore, participants' depression levels from post-treatment to 6-month follow-up were stable (on the EPDS, F<1), or continued to decrease (on the Ham-D-21, F=4.92, df=1,12, P<0.05).
There was no change in participants' IIP total scores or their DAS scores across the three time points. However, analysis of the IIP subdomains yielded significant differences on participants' nonassertive scale scores from baseline (mean=17.6±5.4) to post-treatment (15.7±6.4; t=2.59, df=13, P<0. 05).
Illustrative Case Example
During the first two individual sessions, the therapist helped each participant to identify one or two primary issues that she believed contributed to the onset of her depression. Interpersonal disputes, including interaction problems with the infant and/or marital conflict, were identified as a key problem area by the majority of the women (n=12). Difficulties with the process of role transition, such as coping with the loss of autonomy and the demands of caring for a dependent newborn, as well as feelings of isolation after taking leave from work, was the second most commonly identified concern (n=4). Two women identified their longstanding difficulties with interpersonal relationships as the key problem area contributing to their depression. One participant, who had previously miscarried, identified grief as the primary issue.
A particular advantage of the group approach to IPT individual therapy was that it allowed the participants to identify and address many shared concerns relating to their experiences of parenting and depression. The following vignette was selected to demonstrate how individuals' particular problem areas were addressed in the context of the group.
Vignette: Role Dispute and Role Transition (Initial Sessions). Mrs. A. was a 32-year-old professional woman who sought treatment following the birth of her first child. During the first several weeks postpartum she experienced a severe depression, leading to her brief admission to a psychiatric hospital prior to entering the treatment trial. The depression was a big surprise for Mrs. A., who generally felt very competent and had a supportive husband.
During the early sessions, Mrs. A. shared with the group her feelings of frustration and inadequacy regarding her new role as a mother and was able to relate these feelings to the onset of her depression. Whereas she had always felt highly competent in her professional life, she now found herself struggling with how to parent and meet the demands of her baby. She insisted that she was a bad mother. This perception was aggravated by a dispute with her own mother, who was very upset that her daughter had developed a depressive episode and resented that she had to take care of the infant during the first weeks. Mrs. A.'s mother was not supportive and made her feel bad about herself.
The group made Mrs. A. aware of how inadequately her own mother behaved. The therapist asked Mrs. A. to describe to the group an interaction with her mother for analyses of communication. When Mrs. A. did so, she was able to express feelings of being hurt and not understood. The group members encouraged Mrs. A. to stand up for herself and set limits to her mother's constant nagging regarding her condition. When Mrs. A. expressed her doubts that she would be able to do so, the therapist proposed to role-play the interaction with the mother. To her surprise, Mrs. A. found it much easier than she had expected during the session, and felt encouraged to try the new skill outside the group. In a subsequent session Mrs. A. reported that she had been successfully setting limits to the criticism of her mother in the last week and that this accomplishment had made her feel good about herself.
Several other participants pointed out that Mrs. A. was actually doing as good a job of parenting as they perceived themselves to be doing, or even at times a better job. Indeed, the group became a powerful source of positive feedback for Mrs. A. Increasingly she developed the interpersonal skill of receiving feedback and support within the group, and subsequently she also succeeded in reaching out for new contacts in her outside life. She was able to mourn the loss of her old role as a competent professional and began to adapt to her new role as a mother. The group provided a safe environment to explore positive and negative aspects of the old and new role.
Comment:
One of the key advantages of conducting IPT within a group setting was the opportunity it afforded for the group members to normalize the challenges they all faced during this important life transition. Group cohesion was well established by emphasizing similarities between group members and the universality of their suffering through discussion of the problem areas. For these women, role transition was a common theme and role dispute was the most common problem area. Most of the women were working on similar issues, which allowed the therapist to focus on each group member's problem area more easily. During the initial sessions the therapist and Mrs. A. identified the transition into parenthood as a primary focus and role dispute as her secondary focus. At the beginning of the group sessions the secondary focus was more important, and only later in the therapy did Mrs. A. address the conflict regarding role transition.
Accepting feedback from the group was a new social skill for Mrs. A. The group acted as a source of positive feedback; this represents the active and supportive stance of the therapist in an individual setting. Wilfley and colleagues10 have noted:
[The group] is a powerful tool to address core-self esteem issues. Members feel they have a responsibility to be supportive as well as to provide constructive help. The group is an ideal setting for identifying “in vivo” the social difficulties and determining ways to improve social skills in the context of a therapeutic social milieu. (p. 62)
The specific technique of improving communication skills was employed in the case of Mrs. A., and more unspecific techniques such as encouragement of affect and exploration of the conflict were also used. IPT strategies specific to role transition applied in the group setting, such as mourning the old role as a professional and trying to accept the new role as a mother caring for an infant, are addressed by this group approach, which also provides the opportunity to connect with a new support system.
DISCUSSION
Whereas prior research demonstrated the efficacy of an individual-format IPT, the results of this open pilot treatment trial suggest that a group IPT approach may be efficacious for the treatment of postpartum depression.
Prior research has established that postpartum depression poses risks for both mother and child. Failure to treat maternal depression in a timely fashion has been associated with increased developmental risks to the young child.1 Furthermore, “treatment as usual,” which usually consists of psychopharmacology or unspecific counseling, may be inadequate for addressing the unique concerns of postpartum depressed women. For example, better child outcomes were observed when a specific treatment of the mother was employed rather than “treatment as usual.”21
Prior research has established the efficacy of several approaches for the treatment of postpartum depression.1,3,4 However, the group IPT approach may potentially offer unique advantages. Although research has demonstrated the relative safety of antidepressant medications,22 many breastfeeding women are nonetheless reluctant to take them. Individual IPT has been demonstrated to be as efficacious as medication in treating mild to moderate major depression,23 and a group approach may be more cost-effective than individual psychotherapy if it is determined to be equally potent. Furthermore, the group approach allows participants to meet other women facing similar challenges, thus normalizing their experiences as mothers of young infants. Participating in a group may minimize the feelings of stigma associated with this illness and may decrease the individuals' sense of isolation. Indeed, many women in this pilot project initiated contact with other members. Thus, group IPT potentially adds to the range of available treatment options, increasing the percentage of women who receive intervention.
The IPT group format was well accepted once women were recruited and the rationale was explained to them. Despite the relatively high number of participants who terminated early (6 out of 17), the mean number of sessions (9) indicated that the duration of the treatment was still within the range of the number of sessions employed by other standardized protocols.24 Some reasons for early termination were favorable for the treatment (e.g., returning to work or school), and others were less favorable (e.g., 2 patients, both diagnosed with a comorbid personality disorder, Cluster B, left the treatment after the initial group session).
The majority of women who completed the treatment showed a significant reduction in their depressive symptoms. Analysis of the data for the two unremitted patients who followed through with treatment revealed that both had comorbid conditions: one obsessive-compulsive disorder and the other a personality disorder (Cluster C). The other 8 patients with comorbid anxiety disorders remitted from their episodes.
All three patients with personality disorder (two Cluster B and one Cluster C) were unable to take advantage of this treatment option. Two dropped out after the first group session and one did not remit. However, judging Axis II diagnosis during an episode of major depression can be difficult because of the challenges involved in differentiating state versus trait characteristics in the depressed patient.
Limitations
Although this study indicated that significant short- and long-term gains were made in the reduction of depressive symptomatology, a number of limitations should be noted. The study treated a relatively small sample, and there was no control group. The small sample size may have occluded our ability to detect certain changes that may have occurred as a function of the group treatment. For example, although changes were evident in the depressive symptomatology, baseline and post-treatment, there was no apparent change involving the indices of interpersonal functioning. A reason for this could be that at the 6-month follow-up, when results regarding improvement of interpersonal functioning are expected to be most evident, the sample size was even smaller. Furthermore, the time allotted between treatment and follow-up may not have been long enough to show significant change in this area. In addition, it is possible that the 12-week duration of the intervention was too short for effecting significant change in this area. Other IPT studies employ 20 weeks of treatment, and this should be a consideration for future controlled trials.
A further limitation is that the assessment might have been biased by the therapist having conducted the investigator-based assessments (SCID, Ham-D) of the treatment outcome. However, most of the subsequent assessments were based on patient self-ratings, thus compensating somewhat for this possible source of bias.
There was no monitoring of adherence to the treatment because such procedures had not yet been developed for group IPT at the time of the study. A treatment adherence form was used to rate tapes for the NIMH trial. The sessions of the current investigation were videotaped for group process evaluation.
Future Goals
Currently the team is working on a manual for an IPT postpartum group therapy model. This manualized intervention will form the basis for a controlled trial in which we will attempt to address the limitations of the present investigation. Furthermore, modifications will be made on the basis of new developments from other IPT-group researchers, namely Wilfley and colleagues' new refinements regarding number of sessions and midtreatment individual sessions.12
The present study is a pilot for a forthcoming randomized clinical trial examining the efficacy of IPT group format versus a “treatment as usual” control group.
Acknowledgments
The authors gratefully acknowledge the support and feedback provided by Myrna M. Weissman and John C. Markowitz. A The first author thanks Bud Feder for his constant inspiration regarding group work and his training in interactive groups. The findings were presented in part at the World Congress on Infant Mental Health, Montreal, Canada, July25–29, 2000; at the 27th Annual Meeting of the North American Society for Psychosocial Obstetrics and Gynecology, Maui, HI, February 28–March 3, 1999; and at the Biennial Meeting of the Marcé Society, Iowa City, IA, June 24–28, 1998.
Grant support was provided by the Medical Scientific Fund, City of Vienna (#1569).
References
- 1.Cooper PJ, Murray L: Postnatal depression. BMJ 1998; 316:1884–1886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spinelli MG: Interpersonal psychotherapy for depressed antepartum women: a pilot study. Am J Psychiatry 1997; 154:1028– 1030 [DOI] [PubMed] [Google Scholar]
- 3.Meager I, Milgrom J: Group treatment for postpartum depression: a pilot study. Aust NZ J Psychiatry 1996; 30:852–860 [DOI] [PubMed] [Google Scholar]
- 4.Stuart S, O'Hara MW: Interpersonal psychotherapy for postpartum depression: a treatment program. J Psychother Pract Res 1995; 4:18–29 [PMC free article] [PubMed] [Google Scholar]
- 5.Weissman MM, Markowitz JC, Klerman L: Comprehensive Guide to Interpersonal Psychotherapy. New York, Basic Books, 2000
- 6.Wilfley DE, Agras WS, Telch CF, et al: Group cognitive-behavioral therapy and group interpersonal psychotherapy for the nonpurging bulimic individual: a controlled comparison. J Consult Clin Psychol 1993; 61:296–305 [DOI] [PubMed] [Google Scholar]
- 7.Wittchen HU, Wunderlich U, Gruschewitz S, et al: Strukturiertes klinisches Interview für DSM-IV Achse-I (SKID-I) [Structured Clinical Interview for DSM-IV (SCID-I)]. Göttingen, Germany, Hofgrefe, 1997
- 8.Klier CM, Geller PA, Neugebauer R: Minor depressive disorder in the context of miscarriage. J Affect Disord 2000; 59:113– 21 [DOI] [PubMed] [Google Scholar]
- 9.Collegium-Internationale-Psychiatriae-Scalarum: Hamilton-Depressions-Skala Fremdbeurteilungsskala C [Hamilton Rating Scale for Depression]. Weinheim, Germany, Beltz Test GmbH, 1986
- 10.Wilfley DE, Mackenzie KR, Welch RR, et al: Interpersonal Psychotherapy for Group. New York, Basic Books, 2000
- 11.Yalom ID: The Theory and Practice of Group Psychotherapy, 4th edition. New York, Basic Books, 1995
- 12.Wilfley DE, Frank MA, Welch RR, et al: Adapting interpersonal psychotherapy to a group format (IPT-G) for binge eating disorder: toward a model for adapting empirically supported treatments. Psychotherapy Research 1998; 8:379–391 [Google Scholar]
- 13.O'Hara M, Stuart S, Gorman L: Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 2000; 57:1039–1045 [DOI] [PubMed] [Google Scholar]
- 14.Gruen DS: A group psychotherapy approach to postpartum depression. Int J Group Psychother 1993; 43:191–203 [DOI] [PubMed] [Google Scholar]
- 15.Fydrich T, Renneberg B, Schmitz B, et al: Strukturiertes Klinisches Interview für DSM-IV Achse-II (SKID-II) [Structured Clinical Interview for DSM-IV (SCID-II)]. Göttingen, Germany, Hofgrefe, 1997
- 16.Muzik M, Klier CM, Rosenblum KL, et al: Are commonly used self-report inventories suitable for screening postpartum depression and anxiety disorders? Acta Psychiatr Scand 2000; 101:1–3 [DOI] [PubMed] [Google Scholar]
- 17.Horowitz LM, Rosenberg S, Bear BA et al: Inventory of Interpersonal Problems: psychometric properties and clinical applications. Journal of Consensus Psychology 1988; 576:885–892 [DOI] [PubMed] [Google Scholar]
- 18.Spanier G: Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family 1976; 38:15–28 [Google Scholar]
- 19.Friedmann RC, Curt DF, De Mets DI: Issues in data analysis, in Fundamentals of Clinical Trials, 2nd edition, edited by Friedman RC, Curt DF, De Mets DL. St. Louis, MO, Mosby-Year Book, 1985, pp 241–266
- 20.Frank E, Prien RF, Jarret RB, et al: Conceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse and recurrence. Arch Gen Psychiatry 1991; 48:851–855 [DOI] [PubMed] [Google Scholar]
- 21.Cooper JC, Murray L: The impact of psychological treatments of postpartum depression on maternal mood and infant development, in Postpartum Depression and Child Development, edited by Murray L, Cooper PJ. New York, Guilford, 1997, pp 201–221
- 22.Yoshida K, Smith B, Kumar R: Psychotropic drugs in mother's milk: a comprehensive review of assay methods, pharmacokinetics and of safety of breastfeeding. J Psychopharmacol 1999; 13:64–80 [DOI] [PubMed] [Google Scholar]
- 23.Elkin I, Shea T, Watkins JT, et al: National Institute of Mental Health Treatment of Depression Collaborative Research Program: general effectiveness of treatment. Arch Gen Psychiatry 1989; 46:971–982 [DOI] [PubMed] [Google Scholar]
- 24.Cramer B: Psychodynamic perspectives on the treatment of postpartum depression, in Postpartum Depression and Child Development, edited by Murray L, Cooper PJ. New York, Guilford, 1997, pp 237–261