Abstract
This is a complete report of an open trial of manualized psychodynamic psychotherapy for treatment of panic disorder, Panic-Focused Psychodynamic Psychotherapy (PFPP). Twenty-one patients with PD were entered into a trial of twice-weekly, 24-session treatment. Sixteen of 21 experienced remission of panic and agoraphobia. Treatment completers with depression also experienced remission of depression. Improvements in symptoms and in quality of life were substantial and consistent across all measured areas. Symptomatic gains were maintained over 6 months. This report was prepared specifically to describe 6-month follow-up on these patients. Psychodynamic psychotherapy appears to be a promising nonpharmacological treatment for panic disorder.
Keywords: Panic Disorder; Psychotherapy, Brief Psychodynamic
Psychodynamic psychotherapy is the most widely practiced form of psychotherapy in this country, yet empirical studies demonstrating whether or not it has utility for the treatment of specific psychiatric disorders are sparse. Almost no empirical data exist about its indications, with rare exceptions such as the work of Crits-Christoph1,2 and Luborsky.3–5 This lack of data highlights a great disjunction between clinical practice and treatment research. Further systematic study of its efficacy, therefore, is essential. A complication to this endeavor is that a wide variety of treatment techniques are described as “psychodynamic psychotherapy.” The specific psychotherapeutic techniques we are studying will be outlined below and are more thoroughly described in the PFPP treatment manual.6
Patients with panic disorder constitute one population who may benefit from psychodynamic treatment. Panic disorder is a serious public health problem. This prevalent, chronic, and debilitating syndrome is associated with high rates of medical and psychiatric utilization of services. Markowitz et al.7 found that panic sufferers in the community had social and health consequences similar to those of people with major depression. They reported poor physical health, poor emotional health, a higher incidence of alcohol and drug abuse, and a higher incidence of attempted suicide than normal subjects.8 Patients with panic disorder have the highest odds ratio for visiting general medical services six or more times within six months compared with other groups of psychiatric patients.9,10 Panic patients have the highest rate of morbidity and health care utilization relative to patients who have any other psychiatric diagnosis, or to medical patients with no psychiatric diagnosis. Patients with panic disorder account for 20% to 29% of all emergency room visits11,12 and are 12.6 times as likely to visit emergency rooms as the general population.7
Several forms of therapy, including pharmacotherapy and cognitive-behavioral therapy, have shown efficacy in short-term treatment studies of panic disorder, but long-term outcome data from these interventions are inconclusive.13 Naturalistic follow-up studies of specific antipanic treatments report high rates of relapse, ongoing impairment in functioning, and continued intermittent participation in psychiatric treatment in many patients who initially experienced symptomatic relief from these therapies. In a review of the 17 largest clinical follow-up studies of anxiety neurosis and panic disorder from 1950 through the early 1990s, only 3% to 43% of patients were classified as “recovered,” with most studies citing rates in the high teens to low twenties for recovery, whereas 9% to 45% of treated patients remained in the “no change” category.14 Of course, most patients in these studies did not receive standard antipanic treatment. Relapse is common following discontinuation of medication treatments that were initially efficacious.15–23
Cognitive-behavioral therapy (CBT) is surely the most powerful studied treatment for panic disorder. Many long-term outcome studies for panic disorder report impressive response rates to CBT.24–27 Nonetheless, even in the most closely controlled sample that reports a high response rate,24 38% of patients remained symptomatic after completing their CBT trial. This limit to response makes it essential to investigate other potentially beneficial antipanic psychotherapies. Furthermore, despite the research success of CBT and pharmacotherapy, in clinical practice many panic patients are unable or unwilling to tolerate medication, and some have difficulty complying with behavioral treatment.27,28 In addition, very few panic studies have assessed broader quality-of-life aspects of treatment response.
PSYCHODYNAMIC BACKGROUND
In 1895, Freud29 described a syndrome very similar to that which is currently designated “panic disorder” in DSM-IV. His description of “anxiety neurosis” included many of the associated traits from which panic patients suffer, such as difficulty in asserting themselves, chronic anxious expectation that frightening things will happen to them and to the people whom they love, and high levels of anxiety experienced during separations from important love objects.
In 1991, Milrod and Shear30 found 35 cases in the literature, with symptomatic descriptions accurate enough for both authors to make the diagnosis of DSM-III-R panic disorder, that had been successfully treated with psychodynamic psychotherapy or psychoanalysis alone. Since then, other successful psychodynamic treatments for patients with panic disorder have been reported.31–35 These reports suggest that psychodynamic treatment alone can bring symptomatic relief, often as rapidly as psychopharmacologic or cognitive-behavioral interventions. Additionally, Wiborg et al.36 demonstrated in a pilot randomized controlled trial that a 3-month, weekly manualized psychodynamic psychotherapy in conjunction with clomipramine significantly reduced relapse rate over 18 months among patients with panic disorder relative to patients treated with clomipramine alone.
In spite of this suggestive evidence, there has been almost no systematic study of psychodynamic psychotherapy as monotherapy for panic disorder. Given the prevalent usage and wide availability of this type of treatment, there is an urgent need for such studies.
METHODS
Twenty-one patients with DSM-IV panic disorder were treated with Panic-Focused Psychodynamic Psychotherapy, which consisted of 24 twice-weekly sessions (12 weeks). Follow-up assessments took place at treatment termination and at 6 months after treatment termination. Patients were not permitted to engage in nonstudy forms of psychiatric treatment, including medication use, during the treatment phase or follow-up phase of this study. Six therapists, all graduates of psychoanalytic institutes, underwent a specific training course in the performance of this therapy. Adherence standards were closely monitored. Adherence rating scales contain seven items that specifically monitor psychodynamic focus and attention to panic and related symptoms. Total intraclass correlations were calculated to be 0.92. All therapists adhered to study protocol, with an average therapist adherence rating of 5.5 on Likert-type scales scored from 1 to 6.
Subjects
Twenty-one patients with DSM-IV panic disorder with or without agoraphobia who gave informed written consent were recruited. All participants received study treatment without charge.
Patients were eligible for inclusion if they were between the ages of 18 and 50 and met DSM-IV criteria for panic disorder with or without agoraphobia as their primary psychiatric diagnosis.
Subjects must have had at least one panic attack per week for the month prior to study entry. In order to determine the immediate and 6-month follow-up effects of the study treatments alone on panic, participants were asked to discontinue all psychotropic medication and to disengage from ongoing psychotherapy treatments. Patients on medication at the time of study entry were eligible to enter the study only if they met criteria for active panic disorder while on medication. Medication taper was accomplished by the Principal Investigator (B.M.) or the patient's personal physician in a slow, gradual, and tolerable taper. Patients were medication-free for at least 4 weeks before beginning the 3-week pre-treatment panic diary phase that constituted the start of the study. They agreed to avoid psychotropic medication for the duration of the treatment.
Patients who were unable to taper off of psychotropic medication were excluded, as were patients with substance abuse (current or with less than 6 months' remission), active major depression with melancholia, or a lifetime history of mania, schizophrenia, delirium, or dementia.
Treatment: Panic-Focused Psychodynamic Psychotherapy (PFPP)
PFPP is a 24-session, manualized psychodynamic psychotherapy delivered over 12 to 14 weeks in twice-weekly sessions, with leeway allowed for vacations. Sessions last for 45 minutes. The PFPP manual incorporates the authors' extensive clinical experience treating panic patients with psychodynamic psychotherapy.6 PFPP is a modified form of psychodynamic psychotherapy that maintains the central psychodynamic principles of the importance of unconscious mental dynamisms and fantasies, free association, and the centrality of the transference while the therapist focuses attention on all of these processes as they are connected to the patient's experience of panic. General principles of psychological dynamisms that are common to most panic patients and have been noted by psychoanalytic authors previously,37,38 such as their difficulty with separations and ambivalent attachments, are used to inform interpretive efforts. As with all forms of psychotherapy, until relevant process studies are accomplished, it is difficult to pinpoint which of the myriad interventions that take place are primarily responsible for observed therapeutic changes. The following is an overview of this treatment. The number of sessions allotted to different phases of treatment varies from patient to patient.
Phase I: Treatment of Acute Panic.
In order to lessen panic symptoms, from a psychodynamic view, we hypothesize that it is necessary to uncover the unconscious meaning of these symptoms. In this respect, the psychodynamic approach is in direct contrast to the atheoretical and acontextual DSM definition of “out-of-the-blue” panic disorder phenomenology. The following strategy is used:
-
Initial evaluation and early treatment:
- Exploration of circumstances and feelings surrounding panic onset.
- Exploration of personal meanings of panic symptoms.
- Exploration of feelings and content of panic episodes.
-
Psychodynamic conflicts in panic disorder:
- Separation and independence.
- Anger recognition; management and coping with expression.
- Sexual excitement and its perceived dangers.
-
Expected responses to Phase I of treatment:
- Panic symptom relief.
- Reduction in agoraphobic symptoms.
Phase II: Treatment of Panic Vulnerability.
To lessen vulnerability to panic, from a psychodynamic perspective, we hypothesize that core “dynamisms” must be understood and altered. In order to do this, these dynamisms must be identified with the patient in the course of the psychotherapy, often through their emergence in the transference. The following strategy is used:
Addressing the nature of the transference.
Working through.
-
Expected responses to Phase II of treatment:
- Improvement in relationships.
- Less conflicted and anxious experience of separation, anger, sexuality.
- Reduction in panic recurrence.
Phase III: Termination.
To address panic patients' severe difficulties with separation and independence, the psychodynamic view hypothesizes that the experience of termination in this time-limited psychotherapy will permit the patient to reexperience these conflicts directly with the therapist so that underlying fantasies can begin to be articulated, understood, and rendered less magical and frightening. Patient reaction to termination must be aggressively addressed for a minimum of the final one-third (i.e., one month) of the treatment.
Reexperiencing of central separation and anger themes in the transference as termination approaches.
-
Expected responses to phase III of treatment:
- Possible temporary recrudescence of symptoms as these feelings are experienced in the therapy.
- New ability to manage separations and independence.
Assessments
Subjects were assessed in accordance with the recommendations of the NIMH collaborative study on panic disorder.39 Subjects receiving a diagnosis of panic disorder based on the Anxiety Disorders Interview, Schedule-IV-L (ADIS),40 were offered entry. Patients were also assessed with the Anxiety Sensitivity Inventory (ASI),41 which rates anticipatory anxiety; the Marks and Matthews Fear Questionnaire (FQ),42 which serves as a rough measure of phobic avoidance and severity; the Panic Disorder Severity Scale (PDSS; M.K. Shear et al., available from Dr. Shear), which is a diagnosis-based composite global rating of severity; and the Social Adjustment Scale (SAS),43 which serves as a measure of functional impairment in multiple areas of patients' lives. These measures contain secondary, predictive variables. The Hamilton Rating Scale for Anxiety (Ham-A)44 served as a dimensional measure of non–panic-related anxiety (i.e., how generally aroused and anxious the patient is in situations not linked to panic attacks). The Hamilton Rating Scale for Depression (Ham-D)45 was similarly used as a dimensional measure of depression. The Sheehan Disability Scale (SDS)46 was used as a measure of social, family, and vocational impairment; this measure has been found to be sensitive and reliable in populations of panic patients.47
Data Analysis
This pilot study was designed to estimate the magnitude of symptom change over the course of the study. An objective of the study was to gather pilot data that could be used to design our larger, ongoing, placebo-controlled clinical trial of PFPP. The Wilcoxon paired rank sum test was used for within-subject comparisons of symptoms and impairment pre and post treatment. We calculated within-group effect sizes (Cohen's d) that correspond with each Wilcoxon paired rank sum test. The intent-to-treat strategy was employed, using the last observation carried forward (LOCF) for the observations during the first 16 weeks of the study (i.e., 3-week panic diary baseline ratings and 12 weeks of treatment, with assessment at the start of week 16). In the statistical tests of pre–post change (i.e., baseline vs. week 16 and baseline vs. week 40), we have chosen to adjust for multiple comparisons (i.e., 9 dependent variables), using a Bonferroni-adjusted alpha level of 0.006 (i.e., 0.05/9). Comparison of week 16 with follow-up excluded those without week 16 assessments. Inferential tests did not compare dropouts (n=4) and completers (n=17) because of limited statistical power.
RESULTS
Twenty-one subjects entered this open treatment trial. Four subjects dropped out during the course of treatment, 3 of whom had tapered off ineffective benzodiazepine trials (after which active panic remained) 4 to 8 weeks prior to study entry. The number of dropouts was too few to meaningfully compare with completers on demographic variables; nevertheless, all baseline versus 16-week comparisons include 21 subjects, using LOCF as described above.
Sixty-six percent of study entrants were female; 76% were white, 19% were black, and 4% were Asian; 43% were married, 43% single, and 4% each were cohabiting, separated, and divorced; 95% were employed; and 33% had children. The mean current age was 32 years (SD=8). Of the study entrants, 76% had primary DSM-IV panic disorder with agoraphobia, and 24% had primary DSM-IV panic without agoraphobia. Average severity of panic was 5.7 on a scale of 1 to 8 on the ADIS. Eighty-one percent of this sample had at least one active comorbid DSM-IV Axis I diagnosis of clinical severity: 24% had comorbid generalized anxiety disorder, 24% had specific phobia, and 14% had social phobia. In addition, 24% had comorbid major depression and 24% had dysthymia. Mean length of the current panic episode was 3 years (SD=1.7). Prior to study entry, 38% of subjects underwent medication taper from ineffective antipanic regimens.
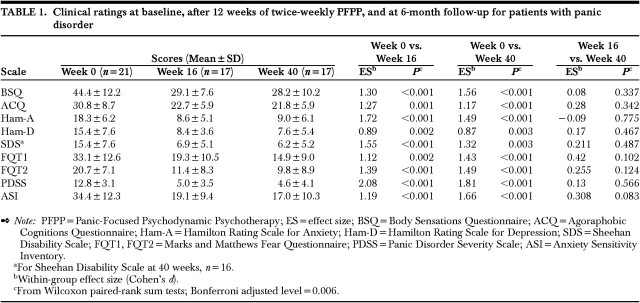
The data (shown in Table 1) indicate substantial reduction not only in panic attacks and preoccupation with panic attacks per se, but also in a wide range of anxious cognitions that frequently affect patients with panic disorder: concerns about their bodies, fears, and general arousability and high levels of resting anxiety. Impairments in quality of life, a serious problem for these patients, improved as well. Moreover, there was no decline in function across any measured symptomatic area at 6-month follow-up, after a 6-month no-treatment period.
TABLE 1. Clinical ratings at baseline, after 12 weeks of twice-weekly PFPP, and at 6-month follow-up for patients with panic disorder.
DISCUSSION
Sixteen of 21 study entrants (and of 17 treatment completers) experienced convincing remission of panic and agoraphobia, more than meeting the remission criteria used in the multicenter panic study.48 Patients were significantly impaired by panic and agoraphobia on study entry, and improvements were significant and clinically meaningful across all measured outcome variables—in primary psychiatric symptoms, in phobic sensitivity, and in overall quality of life—as a result of this brief psychodynamic intervention. The magnitude of therapeutic change is indicated by the very large within-group effect size changes observed across this relatively small study population.
The one completer who failed to respond to treatment had comorbid DSM-IV obsessive-compulsive disorder, the only patient in the sample with this comorbidity. She experienced no change in most symptomatic and quality-of-life measurements. Four patients dropped out of study treatment, all of whom were counted in the intent-to-treat analysis as nonresponders. Of these four, two dropped out within the first two sessions, one because of scheduling difficulties and dislike of her study therapist's approach, the other because of intolerable panic experienced while attempting to get to his therapist's office. This latter patient had a history of opiate dependence and had tapered himself off of an ineffective benzodiazepine prior to study entry. Two dropouts occurred after session 13. Both late dropout patients had comorbid major depression and borderline personality disorder, and both had tapered themselves off of ineffective combinations of medications including benzodiazepines two months before study entry. Although the number of dropouts in this sample is too small to analyze data or draw conclusions, three of the four dropouts had recently discontinued medication, 2 had active comorbid major depression, and one had a recent history of intravenous opiate dependence in remission. The Principal Investigator felt that all three dropouts who had just tapered medication required further pharmacological treatment, rather than continuation in this medication-free protocol. It cannot be determined how these patients would have responded had they entered this psychotherapy protocol while continuing antipanic medication. Five treatment remitters had also been tapered successfully off of ineffective antipanic medication in order to enter the study; two of these five had been on benzodiazepines.
Although there were substantial within-subject reductions in symptomatic severity, this open study did not test the efficacy of psychodynamic psychotherapy for panic disorder; there was no comparison treatment. It is clear that such a study must be undertaken. Several encouraging points can be made about the use of this approach in this population, from the open trial data. Patients treated in this study were significantly more symptomatic from panic disorder and agoraphobia than those treated in some recent trials,48 and yet their degree of recovery and significant diminution in impairment was substantial. Almost half of this group had comorbid major depression or dysthymia, thus belonging to a population of panic patients that is known to respond more poorly to all studied therapeutic interventions.14 In depressed patients who completed the treatment, depression remitted as well as panic. Two dropouts had comorbid major depression, and thus 25% of patients carrying this comorbidity did not respond. Larger samples of patients will have to be studied to determine whether psychodynamically based interventions can efficaciously treat patients with this comorbidity.
Finally, the study therapists who participated in this treatment trial were senior, well-trained, and experienced clinicians, far more so than the average providers of psychotherapeutic services in many psychotherapy studies. It may well be that the very positive responses observed in these patients would not have been observed had less experienced clinicians delivered this manualized treatment. Whether PFPP can be effectively taught to nonpsychoanalysts remains to be determined. However, brief, panic-focused psychodynamic psychotherapy appears to be a promising nonpharmacological alternative for patients with highly symptomatic panic disorder with a broad range of comorbidities.
ACKNOWLEDGEMENTS
Funding for this work was provided by two grants from the American Psychoanalytic Association's Fund for Psychoanalytic Research, through a fund established by DeWitt Wallace in The New York Community Trust and a private grant by William Frosch, M.D.
References
- 1.Crits-Christoph P, Connoly MB, Azarian K, et al: An open trial of brief supportive-expressive psychodynamic psychotherapy in the treatment of generalized anxiety disorder. Psychotherapy 1996; 33:418-430 [Google Scholar]
- 2.Crits-Christoph P, Siqueland L, Blaine J, et al: The National Institute on Drug Abuse Cocaine Collaborative Treatment Study: rationale and methods. Arch Gen Psychiatry 1997; 54:721-726 [DOI] [PubMed] [Google Scholar]
- 3.Luborsky L, Diguer L, Cacciola J, et al: Factors in outcome in short-term dynamic psychotherapy for chronic vs. nonchronic major depression. J Psychother Pract Res 1996; 5:152-159 [PMC free article] [PubMed] [Google Scholar]
- 4.Woody GE, Luborsky L, McLellan AT, et al: Psychotherapy for opiate addicts: does it help? Arch Gen Psychiatry 1983; 40:639-645 [DOI] [PubMed] [Google Scholar]
- 5.Woody GE, McLellan AT, Luborsky L, et al: Psychotherapy in community methadone programs: a validation study. Am J Psychiatry 1995; 152:1302-1308 [DOI] [PubMed] [Google Scholar]
- 6.Milrod B, Busch F, Cooper A, et al: Manual of Panic-Focused Psychodynamic Psychotherapy. Washington, DC, American Psychiatric Press, 1997
- 7.Markowitz JS, Weissman MM, Ouellette R, et al: Quality of life in panic disorder. Arch Gen Psychiatry 1989; 46:984-992 [DOI] [PubMed] [Google Scholar]
- 8.Rosenbaum JF: Panic disorder: making clinical sense of the latest research. J Clin Psychiatry 1997; 58:127-134 [DOI] [PubMed] [Google Scholar]
- 9.Klerman GL, Weissman MM, Ouellete R, et al: Panic attacks in the community: social morbidity and health care utilization. JAMA 1991; 265:742-746 [PubMed] [Google Scholar]
- 10.Simon G, Von Korff M: Somatization and psychiatric disorder in the NIMH epidemiologic catchment area study. Am J Psychiatry 1991; 148:1494-1500 [DOI] [PubMed] [Google Scholar]
- 11.Swenson RP, Cox BJ, Woszezy CB: Use of medical services and treatment for panic disorder with agoraphobia and for social phobia. CMAJ 1992; 147:878-883 [PMC free article] [PubMed] [Google Scholar]
- 12.Weissman MM, Klerman GL, Urankowitz J: Suicidal ideation and suicide attempts in panic disorder and attacks. N Engl J Med 1989; 321:1209-1216 [DOI] [PubMed] [Google Scholar]
- 13.Milrod B, Busch F: The long-term outcome of treatments for panic disorder: a review of the literature. J Nerv Ment Dis 1996; 184:723-730 [DOI] [PubMed] [Google Scholar]
- 14.Noyes R, Holt CS, Woodman CL: Natural course of anxiety disorders, in Long-term Treatments of Anxiety Disorders, edited by Mavissakalian MR, Prien RF. Washington, DC, American Psychiatric Press, 1996, pp 1-37
- 15.Mavissakalian M, Michelson L: Two-year follow-up of exposure and imipramine treatment of agoraphobia. Am J Psychiatry 1986; 143:1106-1112 [DOI] [PubMed] [Google Scholar]
- 16.Nagy LM, Krystal JH, Woods SW, et al: Clinical and medication outcome after short-term alprasolam and behavioral group treatment in panic disorder: 2.5 year naturalistic follow-up study. Arch Gen Psychiatry 1989; 46:993-999 [DOI] [PubMed] [Google Scholar]
- 17.Noyes R Jr, Garvey MJ, Cook BL: Follow-up study of patients with panic disorder and agoraphobia with panic attacks treated with tricyclic antidepressants. J Affect Disord 1989; 16:249-257 [DOI] [PubMed] [Google Scholar]
- 18.Noyes R Jr, Reich J, Christiansen J, et al: Outcome of panic disorder: relationship to diagnostic subtypes and comorbidity. Arch Gen Psychiatry 1990; 47:809-818 [DOI] [PubMed] [Google Scholar]
- 19.Noyes R Jr, Garvey MJ, Cook B, et al: Controlled discontinuation of benzodiazepine treatment for patients with panic disorder. Am J Psychiatry 1991; 148:517-523 [DOI] [PubMed] [Google Scholar]
- 20.Pollack MH, Otto MW, Tesar GE, et al: Long-term outcome after acute treatment with alprasolam and clonazepam for panic disorder. J Clin Psychopharmacol 1993; 13:257-263 [PubMed] [Google Scholar]
- 21.Rickels K, Case G, Downing RW, et al: One-year follow-up of anxious patients treated with diazepam. J Clin Psychopharmacol 1986; 6:32-36 [PubMed] [Google Scholar]
- 22.Sheehan DV: One-year follow-up of patients with panic disorder after withdrawal from long-term anti-panic medication. Paper presented at the Conference on Biological Research on Panic Disorder, Washington, DC, April 1986
- 23.Tyrer P: Clinical effects of abrupt withdrawal from tricyclic antidepressants and monoamine oxidase inhibitors after long-term treatment. J Affect Disord 1984; 6:1-7 [DOI] [PubMed] [Google Scholar]
- 24.Marks IM, Swinson RP, Basoglu M, et al: Alprasolam and exposure alone and combined in panic disorder with agoraphobia. Br J Psychiatry 1993; 162:776-787 [DOI] [PubMed] [Google Scholar]
- 25.Craske MG, Brown TA, Barlow DH: Behavioral treatment of panic disorder: a two-year follow-up. Behavior Therapy 1991; 22:289-304 [Google Scholar]
- 26.Clark DM, Salkovskis PM, Hackman A, et al: A comparison of cognitive therapy, applied relaxation, and imipramine in the treatment of panic disorder. Br J Psychiatry 1994; 164:759-769 [DOI] [PubMed] [Google Scholar]
- 27.Fava GA, Zielezny M, Savron G, et al: Long-term effects of behavioral treatment for panic disorder with agoraphobia. Br J Psychiatry 1995; 166:87-92 [DOI] [PubMed] [Google Scholar]
- 28.American Psychiatric Association: Practice Guideline for Treatment of Patients With Panic Disorder and Related Anxiety Disorders. Am J Psychiatry 1998; 155(May suppl) [PubMed]
- 29.Freud S: On the grounds for detaching a particular syndrome from neurasthenia under the description of “anxiety neurosis” (1895), in The Standard Edition of the Complete Psychological Works of Sigmund Freud, vol 3, translated and edited by Strachey J. London, Hogarth Press, 1962, pp 87-117
- 30.Milrod B, Shear MK: Dynamic treatment of panic disorder: a review. J Nerv Ment Dis 1991; 179:741-743 [DOI] [PubMed] [Google Scholar]
- 31.Milrod B: The continued usefulness of psychoanalysis in the therapeutic armamentarium for the treatment of panic disorder. J Am Psychoanal Assoc 1995; 43:151-162 [DOI] [PubMed] [Google Scholar]
- 32.Stern G: Anxiety and resistance to changes in self-concept, in Anxiety as Symptom and Signal, edited by Roose S, Glick RA. Hillsdale, NJ, Analytic Press, 1995, pp 105 -120
- 33.Renik O: The patient's anxiety, the therapist's anxiety, and the therapeutic process, in Anxiety as Symptom and Signal, edited by Roose S, Glick RA. Hillsdale, NJ, Analytic Press, 1995, pp 121 -130
- 34.Busch F, Milrod B, Cooper A, et al: Panic-focused psychodynamic psychotherapy (grand rounds). J Psychother Pract Res 1996; 5:72-83 [PMC free article] [PubMed] [Google Scholar]
- 35.Milrod B, Busch F, Hollander E, et al: A twenty-three-year-old woman with panic disorder treated with psychodynamic psychotherapy. Am J Psychiatry 1996; 153:698-703 [DOI] [PubMed] [Google Scholar]
- 36.Wiborg IM, Dahl AA: Does brief dynamic psychotherapy reduce the relapse rate of panic disorder? Arch Gen Psychiatry 1996; 53:689-694 [DOI] [PubMed] [Google Scholar]
- 37.Deutsch H: The genesis of agoraphobia. Int J Psychoanal 1929; 10:51-69 [Google Scholar]
- 38.Milrod B: Unconscious pregnancy fantasies in patients with panic disorder. J Am Psychoanal Assoc 1998; 46:673-690 [DOI] [PubMed] [Google Scholar]
- 39.Shear MK, Maser JD: Standardized assessment for panic disorder research: a conference report. Arch Gen Psychiatry 1994; 51:346-354 [DOI] [PubMed] [Google Scholar]
- 40.DiNardo PA, Brown TA, Barlow DH: Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version, (ADIS-IV-L). New York, Graywinds, 1995
- 41.Peterson RA, Reiss S: Manual for the Anxiety Sensitivity Index, 2nd edition. Worthington, OH, International Diagnostic Services, 1992
- 42.Marks IM, Mathews AM: Brief standard self-rating for phobic patients. Behav Res Ther 1979; 17:263-267 [DOI] [PubMed] [Google Scholar]
- 43.Weissman MM, Bothwell S: The assessment of social adjustment patient self-report. Arch Gen Psychiatry 1976; 33:1111-1115 [DOI] [PubMed] [Google Scholar]
- 44.Hamilton M: The assessment of anxiety states by rating. Br J Med Psychol 1959; 32:50-55 [DOI] [PubMed] [Google Scholar]
- 45.Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sheehan DV: The Anxiety Disease. New York, Charles Scribner and Sons, 1983
- 47.Barlow DH, Gorman JM, Shear MK, et al: Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: a randomized controlled trial. JAMA 2000; 283:2529-2536 [DOI] [PubMed] [Google Scholar]
- 48.Leon AC, Shear MK, Portera L, et al: Assessing impairment in patients with panic disorder: the Sheehan Disability Scale. Social Psychiatry and Psychiatric Epidemiology 1992; 27:78-82 [DOI] [PubMed] [Google Scholar]