Abstract
Background
Fibromyalgia (FM) is a chronic pain syndrome with unknown etiology and a wide spectrum of symptoms such as allodynia, debilitating fatigue, joint stiffness and migraine. Recent studies have shown some evidences demonstrating that oxidative stress is associated to clinical symptoms in FM of fibromyalgia. We examined oxidative stress and bioenergetic status in blood mononuclear cells (BMCs) and its association to headache symptoms in FM patients. The effects of oral coenzyme Q10 (CoQ10) supplementation on biochemical markers and clinical improvement were also evaluated.
Methods
We studied 20 FM patients and 15 healthy controls. Clinical parameters were evaluated using the Fibromyalgia Impact Questionnaire (FIQ), visual analogues scales (VAS), and the Headache Impact Test (HIT-6). Oxidative stress was determined by measuring CoQ10, catalase and lipid peroxidation (LPO) levels in BMCs. Bioenergetic status was assessed by measuring ATP levels in BMCs.
Results
We found decreased CoQ10, catalase and ATP levels in BMCs from FM patients as compared to normal control (P<0.05 and P<0.001, respectively) We also found increased level of LPO in BMCs from FM patients as compared to normal control (P<0.001). Significant negative correlations between CoQ10 or catalase levels in BMCs and headache parameters were observed (r = −0.59, P<0.05; r = −0.68, P<0.05, respectively). Furthermore, LPO levels showed a significant positive correlation with HIT-6 (r = 0.33, P<0.05). Oral CoQ10 supplementation restored biochemical parameters and induced a significant improvement in clinical and headache symptoms (P<0.001).
Discussion
The results of this study suggest a role for mitochondrial dysfunction and oxidative stress in the headache symptoms associated with FM. CoQ10 supplementation should be examined in a larger placebo controlled trial as a possible treatment in FM.
Introduction
Fibromyalgia (FM) is a common chronic pain syndrome with an unknown etiology, which has been associated with a wide spectrum of symptoms such as allodynia, debilitating fatigue, joint stiffness and depression. FM is diagnosed according to the classification criteria established by the American College of Rheumatology (ACR) [1]. Despite being a common disorder that affects at least 5 million individuals in the United States [2], its pathogenic mechanism remains elusive. In addition to the described symptoms, a high prevalence of FM has been found among patients with transformed migraine and headaches [3], [4]. Common genetic basis, synergetically working with other factors (emotional, personality features, stressful events and medication overuse) should cause a chronic antinociceptive system alteration and therefore a progressive increase (hyperalgesia) and diffusion (panalgesia) of pain. It has been hypothesized that episodic migraine, chronic daily headaches and FM may actually be a continuum of the same disorder [5].
Recently, oxidative stress has been proposed as a relevant event in the pathogenesis of FM and headaches [6], [7]. Previously, our group has detected decreased coenzyme Q10 (CoQ10) levels and increased mitochondrial reactive oxygen species (ROS) production in blood mononuclear cells (BMCs) from FM patients [8]. Furthermore, oxidative stress showed a significant correlation with clinical symptoms in FM [6].
CoQ10 levels and mitochondrial dysfunction have also been implicated in the pathophysiology of migraine, and it has been reported that oral CoQ10 supplementation improved clinical symptoms [9].
The aim of this paper was first to establish a possible correlation between oxidative stress parameters and severity of headaches in FM, and secondly to study the effects of oral CoQ10 supplementation on the improvement in headache symptoms.
Patients and Methods
Ethics Statement
Written informed consent and the approval of the ethical committee of University Pablo de Olavide and Universitary Hospital Virgen Macarena from Seville were obtained, according to the principles of the Declaration of Helsinki.
Patients
All samples were obtained after informed consent from patients and the approval of the local ethical committee was obtained according to the principles of the Declaration of Helsinki. The study consisted of 20 women diagnosed with FM and 15 healthy women. The inclusion criteria was fibromyalgia that had been diagnosed for the previous 2 to 3 years, based on the current ACR diagnostic criteria 1. Exclusion criteria were acute infectious diseases in the previous 3 weeks; past or present neurological, psychiatric, metabolic, autoimmune, allergy-related, dermal or chronic inflammatory disease; undesired habits (e.g., smoking, alcohol, etc.); oral diseases (e.g., periodontitis); medical conditions that required glucocorticoid treatment, use of analgesics, statin or antidepressant drugs; past or current substance abuse or dependence and pregnancy or current breastfeeding. Healthy controls had no signs or symptoms of FM and were free of any medication for at least 3 weeks before the study began. All patients and controls had taken no drugs or vitamin/nutritional supplement during the 3 week period prior to the collection of the blood samples. Before the study, the patients reported using paracetamol on demand. Clinical data was obtained from physical examination, and evaluated using the Fibromyalgia Impact Questionnaire (FIQ) including visual analogues scales about general and diffuse pain typical of FM (VAS), and Headache Impact Test (HIT-6).
Blood mononuclear cells
Heparinized blood samples were collected after 12-hours fasting from patients and healthy age and sex-matched control subjects. BMCs were purified from heparinized blood by isopycnic centrifugation using Histopaque-1119 and Histopaque-1077 (Sigma Chemical Co., St. Louis, MO, USA).
Measurement of CoQ10 levels
CoQ10 content in BMCs were analyzed by HPLC (Beckman Coulter, Brea, CA, USA; 166-126 HPLC) with ultraviolet detection (275 nm), according to the method described above [8].
Lipid peroxidation
Lipid peroxidation in cells was determined by analyzing the accumulation of lipoperoxides using a commercial kit from Cayman Chemical (Ann Arbor, Michigan, USA). TBARS are expressed in terms of malondialdehyde (MDA) levels. In these assays, an MDA standard is used to construct a standard curve against which unknown samples can be plotted.
Catalase determination
A spectrophotometric method described by Beer and Sizer (1952) [10] was used for measuring the breakdown of hydrogen peroxide by catalase. Briefly, activity was determined by using 35 µg of cell lysate, prepared in a lysis buffer composed of 0.9% NaCl, 20 mM Tris.ClH, pH = 7.6, 0.1% triton X-100, 1 mM phenylmethylsulfonylfluoride and 0.01% leupeptine with gentle shaking, in a kinetic spectrophotometric assay that measures a decrease in the absorbance of hydrogen peroxide.
ATP levels
ATP levels were determined by a bioluminescence assay using an ATP determination kit from Invitrogen-Molecular Probes (Eugene, OR, USA) according to the instructions of the manufacturer.
Oral CoQ10 supplementation
Ten volunteer patients were supplemented with CoQ10 (Pharma Nord, Vejle, Denmark) with soft gel capsules for 3 months (300 mg/day CoQ10 divided in three doses). After 3 months of treatment, heparinized blood samples were collected after 12-hours fasting and 24 hours after the last dose, and clinical symptoms were evaluated. The CoQ10 formulation consisted of soft gelatin capsules containing 100 mg of ubiquinone emulsified with diglyceryl monooleate, beeswax, soy lecithin and canola oil.
Statistical Analysis
All results are expressed as mean ± SD unless stated otherwise. The unpaired Student's t test was used to evaluate the significance of differences between groups. Statistical analyses included Pearson's correlations between CoQ10, catalase, and MDA levels in compared with Hit-6 score. P values less than 0.05 were considered significant. Data were analysed using the SPSS/PC statistical software package (SPSS for Windows, 19, 2010, SPSS Inc. Chicago, IL, USA).
Results
Oxidative stress in FM
The mean age of patients was 46.6±5 years for the FM group and 44.9±4 years for the control group. The mean duration of symptoms in the FM group was 10.1±4.2 years. The mean tender point score in the FM group was 14.8±1.7 points. According to International Headache Society (IHS) criteria, the headache was tension-type headache. The mean of frequency of headache was 3±1 per week. The duration of headache episodes was 10±2 hours. The patients did not describe any symptoms such as nausea, photophobia, or aura.
The most prominent features of these FM patients were pain and stiffness. They were sedentary people and routine laboratory tests yielded normal results for glucose, urea, uric acid, total protein, creatinine, aspartate aminotransferase, alanine aminotransferase, cholesterol and triglycerides (data not shown). The number and subgroup distribution of BMCs (monocytes and limphocytes) in FM patients were in the normal range (data not shown).
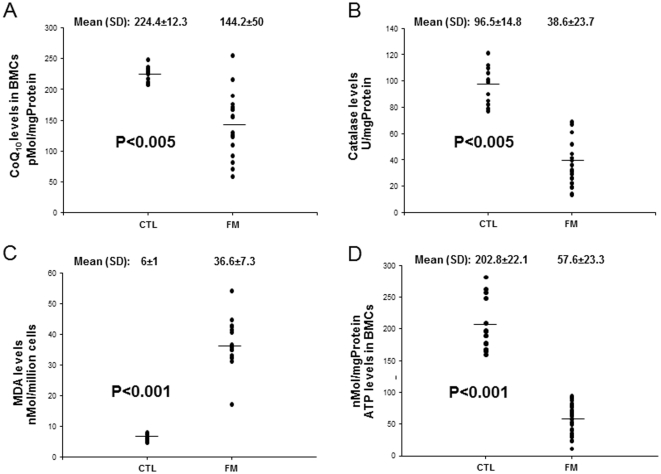
To evaluate the antioxidant system in FM patients, CoQ10 and catalase levels in BMCs were examined and compared to control subjects. Both, CoQ10 and catalase levels were significantly reduced in FM patients, 64.3% and 40% respectively (Figure 1A and 1B). We also determined LPO levels in BMCs from FM patients as a marker of oxidative stress-induced membrane damage by ROS. FM patients showed higher LPO levels in BMCs, 610% with respect to control subjects (Figure 1C).
Figure 1. Coenzyme Q10 levels, catalase levels and lipid peroxidation (MDA levels) in blood mononuclear cells (BMCs) from fibromyalgia (FM) patients and healthy control individuals.
(A) CoQ10 levels were measured by HPLC, as described in Materials and Methods. (B) Catalase was analyzed in BMCs as described in Materials and Methods. (C) LPO was measured as described in Material and Methods. (D) ATP levels were analyzed in BMCs as described in Materials and Methods. Data represent the mean ± SD of three separate experiments.
To determine whether the observed CoQ10 deficiency had an effect on cellular bioenergetics, we measured intracellular ATP levels in BMCs from control and FM patients. ATP levels were reduced to 70% of the control value in BMCs from FM patients (Figure 1D).
Headache correlates with oxidative stress in FM patients
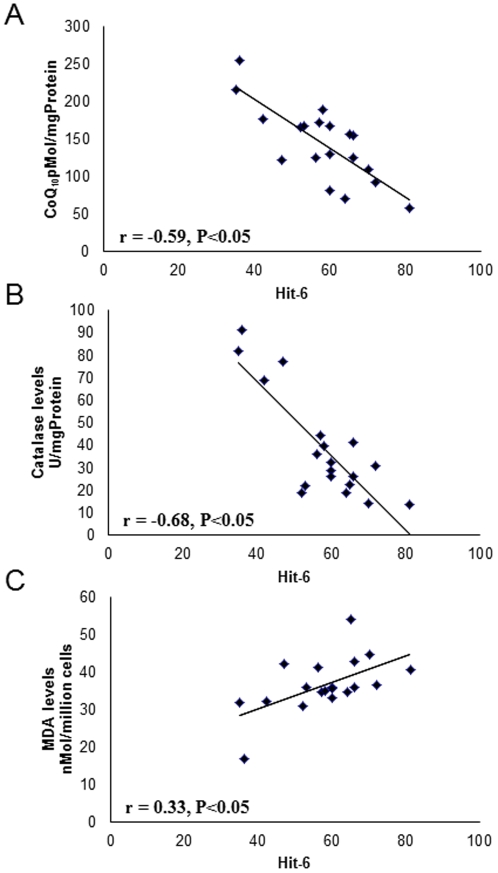
All FM patients showed high HIT-6 scores compared with control subjects (Table 1). To examine whether headache symptoms were associated to increased oxidative stress, Pearson's correlation coefficients (r) were performed between CoQ10, catalase or LPO levels and HIT-6 scores. Figure 2 shows a significant negative correlation between CoQ10 and catalase levels and HIT-6 (r = −0.59, P<0.05; r = −0.68, P<0.05, respectively). Furthermore, LPO levels showed a significant positive correlation with HIT-6 (r = 0.33, P<0.05). No correlation of ATP levels and HIT-6 scores was found (data not shown).
Table 1. Characteristic finding of FM patients and control groups.
| Patients (n = 20) | Control (n = 15) | |||
| Age (yr) | 46.6 | ±5 | 44.9 | ±4 |
| Tender points | 14.8 | ±1.7 | --- | |
| Duration of disease (years) | 10.1 | ±4.2 | --- | |
| FIQ Total score, range 0–100 | 60.2 | ±5.6* | 7.1 | ±1.4 |
| VAS, range 0–10 | 6.9 | ±1.3* | 0.8 | ±0.3 |
| HIT-6, range 36–78 | 61.8 | ±1.3* | 36.1 | ±1.1 |
VAS: Visual Analogue Scale; FIQ: Fibromyalgia Impact Questionnaire; HIT-6: Headache Impact Test. Values are means ±SD,
P<0.001.
Figure 2. Correlation of CoQ10, catalase or lipid peroxidation levels in BMCs from FM patients and HIT-6 levels.
Influence of oral Coenzyme Q10 supplementation
Table 2 shows levels of biochemical markers in control subjects and before and after treatment with CoQ10. In FM patients treated with CoQ10, all levels of oxidative stress markers were similar to those measured in control subjects. CoQ10 supplementation significantly increased levels of CoQ10, ATP and catalase but all levels were lower than those seen in controls. In contrast, MDA in BMCs declined and fell to levels similar to those seen in controls. These biochemical marker changes were associated with improvement of clinical measured by tender points, FIQ VAS and HIT-6 scores.
Table 2. Clinical symptoms and biochemical markers after CoQ10 treatment.
| Pre-treatment (n = 10) | Post-treatment (n = 10) | Control levels (n = 15) | |
| Tender points | 13.9±1.2 | 9±0.5* | --- |
| FIQ total score, range 0–100 | 59.2±4.2† | 30.1±2* | 7.1±1.4 |
| VAS, range 0–10 | 7.1±1.2† | 3.5±0.8* | 0.8±0.3 |
| HIT-6, range 36–78 | 60.8±1.4† | 36.9±1.7* | 36.1±1.1 |
| CoQ10 (pmolQ/mg protein) | 135.6±6.3† | 221.6±11.3* | 224.4±12.3 |
| ATP (nmol/mg protein) | 61.3±4.9† | 191.1±6.7* | 202.8±22.1 |
| Catalase (U/mg protein) | 35.6±10.1† | 85.2±15.3* | 96.5±14.8 |
| MDA in BMCs (nmol/million cells) | 30.3±5.9† | 5.1±1.6* | 6±1 |
VAS: Visual Analogue Scale; FIQ: Fibromyalgia Impact Questionnaire; HIT-6: Headache Impact Test; MDA: Malondialdehyde; BMCs: Blood mononuclear cells. Values are means ±SD,
P<0.001 between pre and post treatment;
P<0.001 between pretreatment and control.
We observed a significant increase of CoQ10 levels after treatment (135.6±6.3 pretreatment and 221.6±11.3 postreatment, P<0.001) (respect to control, 224.4±12.3;P<0.001), ATP levels (61.3±4.9 pretreatment and 191.1±6.7 postreatment, P<0.001) (respect to control, 202.8±22.1;P<0.001) and catalase levels (35.6±10.1 pretreatment and 85.2±15.3 postreatment, P<0.001) (respect to control, 96.5±14.8; P<0.001) in BMCs, a reduction of LPO levels (30.3±5.9 pretreatment and 5.1±1.6 postreatment, P<0.001) (respect to control, 6±1; P<0.001) and a marked improvement of clinical symptoms (FIQ: P<0.01; VAS: P<0.01; HIT-6: P<0.05) (Table 2). No biochemical alterations were detected after CoQ10 treatment: glucose 82,3±10,16 mg/dL (normal range: 76–110), urea 29,7±5,31 mg/dL (normal range: 10–45), uric acid 5,1±1,41 mg/dL (normal range: 2.5–7.5), total protein 7,2±1,01 g/dL (normal range: 6.6–8.7), creatinine 0,9±0,13 mg/dL (normal range: 0.5–1.1), aspartate aminotransferase 24,3±5,17 mU/mL (normal range: 10–40), alanine aminotransferase 21,2±8,11 mU/mL (normal rage: 10–40), total cholesterol 205±9,01 mg/dL (normal range: <220), and triglycerides 168±31,13 mg/dL (normal range: 150–200).
Discussion
In the present study we have confirmed a significant increase of oxidative stress in FM patients, showing a marked decrease of CoQ10, ATP and catalase levels and a significant increase of LPO levels in BMCs compared to control subjects.
Coenzyme Q10 (CoQ10) is present in every membrane of all cells in the body. CoQ10 transfers electrons from complexes I and II to complex III in the mitochondrial respiratory chain and fulfills a critical role in mitochondrial ATP production, playing a crucial role in cellular metabolism; regulating mitochondrial uncoupling proteins, the mitochondrial permeability transition pore, β-oxidation of fatty acids, nucleotide metabolism and production of reactive oxygen species (ROS) [11], [12]. It has been widely demonstrated that CoQ10 is essential for respiratory chain efficacy, and as antioxidant [13], [14], [15]. CoQ10 deficiency has been associated with several diseases with the typical symptoms found in FM patients [16], [17]. Interestingly, CoQ10 deficiency has been detected in depression and chronic fatigue [18], [19], two typical symptoms found in FM patients. Furthermore, both symptoms were markedly improved after CoQ10 supplementation. Our results are in agreement with those of previous reports which have shown that CoQ deficiency is associated with decreased ATP levels and increased oxidative stress [20], [21]. Oxidative stress and, in particular, LPO levels have been implicated in the severity of the clinical symptoms in FM and it has been suggested that antioxidant therapy could be beneficial in FM [6]. On the other hand, the oxidant-antioxidant balance disorders underlie a number of acute and chronic diseases of the central nervous system (CNS) [22]. Clinical conditions affecting the nervous system range from mild cognitive perturbations such as headache or migraine, to life-threatening acute courses such as meningitis, and to chronic neurodegenerative diseases such as multiple sclerosis. One common feature in clinical dysfunctions within the nervous system is redox regulation, with an imbalance in oxidative stress versus antioxidants being characteristic of pathological conditions. It is believed that oxidative stress and LPO play a role in the pathogenesis of migraine by regulating cerebral blood flow and energy metabolism and may constitute a trigger threshold for migraine attacks [23], [24]. Moreover, emerging data suggest that LPO may underlie the neuronal alterations and neurotoxicity observed in numerous neuropathological conditions. Direct application of LPO, either in vivo or in vitro, has been shown to be cytotoxic and to mimic neuronal alterations observed in neuropathological conditions. In addition, prevention of LPO has been demonstrated to be neuroprotective in a variety of neuropathological paradigms [25]. It is known that LPO, as a consequence of oxidative stress, indirectly reflects intracellular ROS generation, and ROS are known to be implicated in the etiology of pain, one of the most prominent symptoms in FM, by inducing peripheral and central hyperalgesia [26].
Our results show an important significant correlation between LPO levels and headache symptoms in FM patients. Antioxidants (CoQ10 and catalase) levels also showed a significant negative correlation with headache symptoms. CoQ10 has two important functions in cells: first, CoQ10 is a mitochondrial cofactor with the potential to boost mitochondrial function, and second, CoQ10 is a powerful free radical scavenger that can mitigate lipid peroxidation and DNA damage caused by oxidative stress [27]. In our study, we have observed a marked improvement in headache symptoms and a significant recovery in oxidative stress markers after CoQ10 supplementation, suggesting that CoQ10 may be involved in the pathophysiology of headache symptoms in FM.
Mitochondria have long been postulated to be involved in the etiology of migraines, although a direct link has not been identified [28]. In addition, the inflammatory component of migraines may produce oxygen free radicals, consuming CoQ10 and inducing CoQ10 deficiency [29].
Clinical studies have generated evidence that FM is associated with immune dysregulation of circulatory levels of pro-inflammatory cytokines, affecting neural function of pain-related neurotransmitters [30]. Cytokines, depending on their concentration, induce symptoms, such as fatigue, fever, sleep, pain, and myalgia [31], all of which develop in FM patients. Alterations in pro-inflammatory cytokine levels have been observed in the serum and skin biopsies of FM patients [32], [33]. Interestingly, several studies have also suggested that inflammatory processes are involved in the physiopathology of migraine [34], [35]. The inflammatory and pain component of FM and migraine is behind the rationale of using nonsteroidal anti-inflammatory drugs (NSAIDs) for the treatment of both symptoms. However, while the use of NSAIDs for fibromyalgia is a fairly common practice, little objective evidence is available upon which to assess the efficacy of these agents [36]. There are multiple mechanisms of action upon which the NSAIDs act. There have been conflicting reports as to whether NSAIDs such as acetylsalicylic acid are effective in protecting neurons against neurotoxicity. Acetaminophen has been shown to rescue neuronal cells from mitochondrial redox impairment, lipoperoxidative products and MDA generation [37]. Furthermore, acetaminophen also reduced the cytoplasmic accumulation of peroxides. Acetylsalicylic acid and acetaminophen inhibit lipid peroxidation and cell damage, in vivo, in the rat hippocampus [38]. The results obtained when NSAIDs are combined with benzodiazepines have also been inconsistent [39]. However, NSAIDs can be helpful in reducing pain flares induced by excessive physical activity, tendinitis or bursitis, although they should only be used on an as needed basis in order to avoid side effects [40].
In addition of pro-inflammatory cytokines, CoQ10 deficiency is also involved in inflammation. A significant negative correlation has been observed between CoQ10 and pro-inflammatory markers in septic shock patients [41], and expression profiling revealed that CoQ10 influences the expression of inflammatory genes suggested that CoQ10 exerts anti-inflammatory properties. In another study, administration of CoQ10 significantly attenuated the increase of oxidative and nitrative stress markers and inflammatory markers in an animal model of metabolic syndrome [42].
In summary, headache symptoms in FM could be a consequence of oxidative stress and both may share common pathophysiologic basis. Furthermore, CoQ10 treatment showed a remarkable improvement in clinical symptoms and headache in FM. Detection of CoQ10 deficiency and subsequent CoQ10 supplementation may result in clinical improvement in FM. Further analysis involving doubled-blind placebo-controlled clinical trials will be required to confirm this observation.
Acknowledgments
We thank all patients for participating in the study.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work has been supported by IV Plan Propio de Investigación (University of Seville, ref. 2010/00000453), FIS PI10/00543 grant, FIS EC08/00076 grant, Ministerio de Sanidad, Spain and Fondo Europeo de Desarrollo Regional (FEDER-Unión Europea), SAS 111242 grant, Servicio Andaluz de Salud-Junta de Andalucía, Proyecto de Investigación de Excelencia de la Junta de Andalucía CTS-5725 and Federación Andaluza de Fibromialgia y Fatiga Crónica (ALBA Andalucía). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–72. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 2.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peres MFP, Young WB, Kaup AO, Zukerman E, Silberstein SD. Fibromyalgia is common in patients with transformed migraine. Neurology. 2001;57:1326–8. doi: 10.1212/wnl.57.7.1326. [DOI] [PubMed] [Google Scholar]
- 4.Marcus DA, Bernstein C, Rudy TE. Fibromyalgia and headache: an epidemiological study supporting migraine as part of the fibromyalgia syndrome. Clin Rheumatol. 2005;24:595–601. doi: 10.1007/s10067-005-1121-x. [DOI] [PubMed] [Google Scholar]
- 5.Centonze V, Bassi A, Cassiano A, Munno I, Dalfino L, et al. Migraine, daily chronic headache and fibromyalgia in the same patient: an evolutive ‘continuum’ of non organic chronic pain? About 100 clinical cases. Neurol Sci. 2004;25:S291–S292. doi: 10.1007/s10072-004-0314-4. [DOI] [PubMed] [Google Scholar]
- 6.Cordero MD, Alcocer-Gómez E, Cano-García FJ, De Miguel M, Carrión AM, et al. Clinical symptoms in fibromyalgia are better associated to lipid peroxidation levels in blood mononuclear cells rather than in plasma. PLoS One. 2011;6:e26915. doi: 10.1371/journal.pone.0026915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta R, Pathak R, Bhatia MS, Banerjee BD. Comparison of oxidative stress among migraineurs, tension-type headache subjects, and a control group. Ann Indian Acad Neurol. 2009;12:167–72. doi: 10.4103/0972-2327.56316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cordero MD, Moreno-Fernandez AM, deMiguel M, Bonal P, Campa F, et al. Coenzyme Q10 distribution in blood is altered in patients with fibromyalgia. Clin Biochem. 2009;42:732–5. doi: 10.1016/j.clinbiochem.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Hershey AD, Powers SW, Vockell AL, Lecates SL, Ellinor PL, et al. Coenzyme Q10 deficiency and response to supplementation in pediatric and adolescent migraine. Headache. 2007;47:73–80. doi: 10.1111/j.1526-4610.2007.00652.x. [DOI] [PubMed] [Google Scholar]
- 10.Beers RF, Jr, Sizer IW. A spectrophotometric method for measuring the breakdown of hydrogen peroxide by catalase. J Biol Chem. 1952;195:133–140. [PubMed] [Google Scholar]
- 11.Turunen M, Olsson J, Dallner G. Metabolism and function of coenzyme Q. Biochim Biophys Acta. 2004;1660:171–199. doi: 10.1016/j.bbamem.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 12.Samorì B, Lenaz G, Battino M, Marconi G, Domini I. On coenzyme Q orientation in membranes: a linear dichroism study of ubiquinones in a model bilayer. J Membr Biol. 1992;128:193–203. doi: 10.1007/BF00231812. [DOI] [PubMed] [Google Scholar]
- 13.Rauchová H, Battino M, Fato R, Lenaz G, Drahota Z. Coenzyme Q-pool function in glycerol-3-phosphate oxidation in hamster brown adipose tissue mitochondria. J Bioenerg Biomembr. 1992;24:235–41. doi: 10.1007/BF00762682. [DOI] [PubMed] [Google Scholar]
- 14.Battino M, Fato R, Parenti-Castelli G, Lenaz G. Coenzyme Q can control the efficiency of oxidative phosphorylation. Int J Tissue React. 1990;12:137–44. [PubMed] [Google Scholar]
- 15.Lenaz G, Battino M, Castelluccio C, Fato R, Cavazzoni M, et al. Studies on the role of ubiquinone in the control of the mitochondrial respiratory chain. Free Radic Res Commun. 1990;8:317–27. doi: 10.3109/10715769009053365. [DOI] [PubMed] [Google Scholar]
- 16.Littarru GP, Tiano L. Clinical aspects of coenzyme Q10: An update. Nutrition. 2010;26:250–4. doi: 10.1016/j.nut.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Lodi R, Rinaldi R, Gaddi A, Iotti S, D'Alessandro R, et al. Brain and skeletal muscle bioenergetic failure in familial hypobetalipoproteinaemia. J Neurol Neurosurg Psychiatry. 1997;62:574–80. doi: 10.1136/jnnp.62.6.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maes M, Mihaylova I, Kubera M, Uytterhoeven M, Vrydags N, et al. Lower plasma Coenzyme Q10 in depression: a marker for treatment resistance and chronic fatigue in depression and a risk factor to cardiovascular disorder in that illness. Neuro Endocrinol Lett. 2009;30:462–9. [PubMed] [Google Scholar]
- 19.Maes M, Mihaylova I, Kubera M, Uytterhoeven M, Vrydags N, et al. Coenzyme Q10 deficiency in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is related to fatigue, autonomic and neurocognitive symptoms and is another risk factor explaining the early mortality in ME/CFS due to cardiovascular disorder. Neuro Endocrinol Lett. 2009;30:470–6. [PubMed] [Google Scholar]
- 20.Rodríguez-Hernández A, Cordero MD, Salviati L, Artuch R, Pineda M, et al. Coenzyme Q deficiency triggers mitochondria degradation by mitophagy. Autophagy. 2009;5:19–32. doi: 10.4161/auto.5.1.7174. [DOI] [PubMed] [Google Scholar]
- 21.Cotán D, Cordero MD, Garrido-Maraver J, Oropesa-Ávila M, Rodríguez-Hernández A, et al. Secondary coenzyme Q10 deficiency triggers mitochondria degradation by mitophagy in MELAS fibroblasts. FASEB J. 2011;25:2669–87. doi: 10.1096/fj.10-165340. [DOI] [PubMed] [Google Scholar]
- 22.Andersen JK. Oxidative stress in neurodegeneration: cause or consequence? Nature Reviews Neuroscience. 2004;5:S18–S25. doi: 10.1038/nrn1434. [DOI] [PubMed] [Google Scholar]
- 23.Tuncel D, Tolun FI, Gokce M, Imrek S, Ekerbiçer H. Oxidative stress in migraine with and without aura. Biol Trace Elem Res. 2008;126:92–7. doi: 10.1007/s12011-008-8193-9. [DOI] [PubMed] [Google Scholar]
- 24.Ciancarelli I, Tozzi-Ciancarelli MG, Di Massimo C, Marini C, Carolei A. Urinary nitric oxide metabolites and lipid peroxidation by-products in migraine. Cephalalgia. 2003;23:39–42. doi: 10.1046/j.1468-2982.2003.00447.x. [DOI] [PubMed] [Google Scholar]
- 25.Keller JN, Mattson MP. Roles of lipid peroxidation in modulation of cellular signaling pathways, cell dysfunction, and death in the nervous system. Rev Neurosci. 1998;9:105–16. doi: 10.1515/revneuro.1998.9.2.105. [DOI] [PubMed] [Google Scholar]
- 26.Wang ZQ, Porreca F, Cuzzocrea S, Galen K, Lightfoot R, et al. A newly identified role for superoxide in inflammatory pain. J Pharmacol Exp Ther. 2004;309:869–78. doi: 10.1124/jpet.103.064154. [DOI] [PubMed] [Google Scholar]
- 27.Tomasetti M, Alleva R, Borghi B, Collins AR. In vivo supplementation with coenzyme Q10 enhances the recovery of human lymphocytes from oxidative DNA damage. FASEB J. 2001;15:1425–7. doi: 10.1096/fj.00-0694fje. [DOI] [PubMed] [Google Scholar]
- 28.Sparaco M, Feleppa M, Lipton RB, Rapoport AM, Bigal ME. Mitochondrial dysfunction and migraine: Evidence and hypotheses. Cephalalgia. 2006;26:361–372. doi: 10.1111/j.1468-2982.2005.01059.x. [DOI] [PubMed] [Google Scholar]
- 29.Moskowitz MA. Neurogenic inflammation in the pathophysiology and treatment of migraine. Neurology. 1993;43:S16–S20. [PubMed] [Google Scholar]
- 30.Staud R. : Evidence of involvement of central neural mechanisms in generating fibromyalgia pain. Curr Rheumatol Rep. 2002;4:299–305. doi: 10.1007/s11926-002-0038-5. [DOI] [PubMed] [Google Scholar]
- 31.Gur A, Oktayoglu P. Status of immune mediators in fibromyalgia. Curr Pain Headache Rep. 2008;12:175–181. doi: 10.1007/s11916-008-0031-4. [DOI] [PubMed] [Google Scholar]
- 32.Lucas HJ, Brauch CM, Settas L, Theoharides TC. Fibromyalgia—new concepts of pathogenesis and treatment. Int J Immunopathol Pharmacol 2006. 2006;19:5–10. [PubMed] [Google Scholar]
- 33.Salemi S, Rethage J, Wollina U, Michel BA, Gay RE, et al. Detection of interleukin lbeta (IL-lbeta), IL-6, and tumor necrosis factor-alpha in skin of patients with fibromyalgia. J Rheumatol. 2003;30:146–150. [PubMed] [Google Scholar]
- 34.Uzar E, Evliyaoglu O, Yucel Y, Ugur Cevik M, Acar A, et al. Serum cytokine and pro-brain natriuretic peptide (BNP) levels in patients with migraine. Eur Rev Med Pharmacol Sci. 2011;2011 15(10):1111–6. [PubMed] [Google Scholar]
- 35.Vanmolkot FH, de Hoon JN. Increased C-reactive protein in young adult patients with migraine. Cephalalgia. 2007;27:843–846. doi: 10.1111/j.1468-2982.2007.01324.x. [DOI] [PubMed] [Google Scholar]
- 36.Wolfe F, Anderson J, Harkness D, Bennett RM, Caro XJ, et al. Health status and disease severity in fibromyalgia: results of a six-center longitudinal study. Arthritis Rheum. 1997;40:1571–1579. doi: 10.1002/art.1780400905. [DOI] [PubMed] [Google Scholar]
- 37.Bisaglia M, Venezia V, Piccioli P, Stanzione S, Porcile C, et al. Acetaminophen protects hippocampal neurons and PC12 cultures from amyloid-peptides induced oxidative stress and reduces NF-κB activation. Neurochem Int. 2002;41:43–54. doi: 10.1016/s0197-0186(01)00136-x. [DOI] [PubMed] [Google Scholar]
- 38.Maharaj H, Maharaj DS, Daya S. Acetylsalicylic acid and acetaminophen protect against oxidative neurotoxicity. Metab Brain Dis. 2006;21:189–199. doi: 10.1007/s11011-006-9012-7. [DOI] [PubMed] [Google Scholar]
- 39.Sarzi-Puttini P, Buskila D, Carrabba M, Doria A, Atzeni F. Treatment strategy in fibromyalgia syndrome: where are we now? Semin Arthritis Rheum. 2008;37:353–65. doi: 10.1016/j.semarthrit.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 40.Sarzi-Puttini P, Atzeni F, Salaffi F, Cazzola M, Benucci M, et al. Multidisciplinary approach to fibromyalgia: what is the teaching? Best Pract Res Clin Rheumatol. 2011;25:311–9. doi: 10.1016/j.berh.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 41.Dupic L, Huet O, Duranteau J. Coenzyme Q10 deficiency in septic shock patients. Crit Care. 2011;15:194. doi: 10.1186/cc10429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kunitomo M, Yamaguchi Y, Kagota S, Otsubo K. Beneficial effect of coenzyme Q10 on increased oxidative and nitrative stress and inflammation and individual metabolic components developing in a rat model of metabolic syndrome. J Pharmacol Sci. 2008;107:128–37. doi: 10.1254/jphs.fp0072365. [DOI] [PubMed] [Google Scholar]