Abstract
Acquired pseudoaneurysm of the left ventricle is a very rare disorder and mostly occurs after large transmural myocardial infarction (MI) with peak creatine phosphokinase-MB levels greater than 150 IU/mL. Patients developing left ventricular (LV) pseudoaneurysm usually present with angina or heart failure symptoms. Although different imaging modalities exist, coronary angiography is the gold standard for diagnosis. Surgery is the treatment of choice for LV pseudoaneurysms detected in the first months after MI. Here we report the case of a 74-year-old woman who presented with a relatively small inferior MI due to right coronary artery occlusion and complicated by LV pseudoaneurysm.
Keywords: Left ventricular pseudoaneurysm, myocardial infarction, surgery
Left ventricular (LV) pseudoaneurysm is defined as an incomplete rupture of the left ventricle, contained by pericardium, organizing thrombus, and hematoma.1 Unlike a true LV aneurysm, there is a lack of endocardial or myocardial elements in the pseudoaneurysm sac. Although LV pseudoaneurysms may occur after cardiac surgery, trauma, or infective endocarditis,2 the most common cause is myocardial infarction (MI).3 The incidence of LV pseudoaneurysm after MI is 0.2 to 0.3%.2 Inferior infarcts have approximately a 2 times higher incidence than anterior infarcts.3 Postinfarction LV pseudoaneurysms occur more frequently in elderly and in male patients. LV pseudoaneurysms are mostly seen after large infarcts with peak creatine phosphokinase-MB (CPK-MB) levels >150 IU/mL.4 The most common presenting symptoms are congestive heart failure, chest pain, and dyspnea, but ~12% of the patients appear asymptomatic at the time of diagnosis.3 Because of the high probability of rupture, surgical correction is usually mandatory.5 Timing of surgery depends on the time period from MI to diagnosis. Surgery is urgently recommended when a pseudoaneurysm is detected within 2 to 3 months after MI.5 However, if diagnosis is made years after MI, the necessity of surgery is usually determined by symptoms rather than risk of rupture.5 Here we report a case with LV pseudoaneurysm that occurred after a relatively small-sized inferior MI.
CASE REPORT
A 74-year-old Turkish woman was admitted to a referring hospital with the complaint of severe chest pain. She had undergone a coronary artery bypass graft operation 1 year ago with a saphenous vein conduit to the left anterior descending artery (LAD). Her ECG showed ST segment elevation in leads D2, D3, and aVF. Thrombolytic therapy with tissue plasminogen activator was immediately started with the diagnosis of inferior MI. Her pain subsequently diminished, and the ST segment elevation was resolved. Peak CPK level was 585 IU/mL and CPK-MB level was 98 IU/mL. Her echocardiographic examination 2 days after infarction showed only inferior hypokinesia with mild systolic dysfunction (ejection fraction [EF] 45 to 50%) and mild to moderate mitral regurgitation (MR). The patient was discharged from the hospital on the 5th day with good recovery. One month later, she was readmitted to the hospital because of progressive dyspnea. Her initial ECG did not show new ischemia, and only signs of recent inferior MI were detected. Auscultation revealed an apical systolic murmur and basal-mid pulmonary rales were present. Cardiac enzyme levels were within normal range. She was treated with intravenous diuretic therapy and nitroglycerin. Her clinical condition improved after 2 days. After that, coronary angiography was planned.
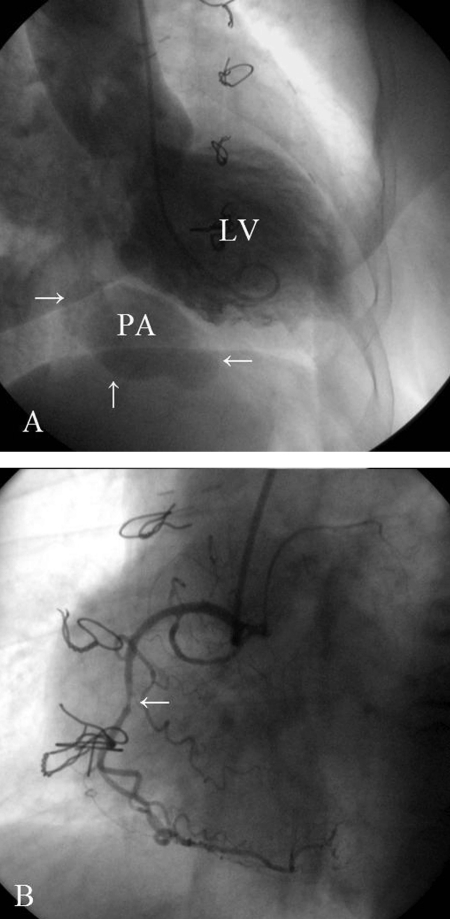
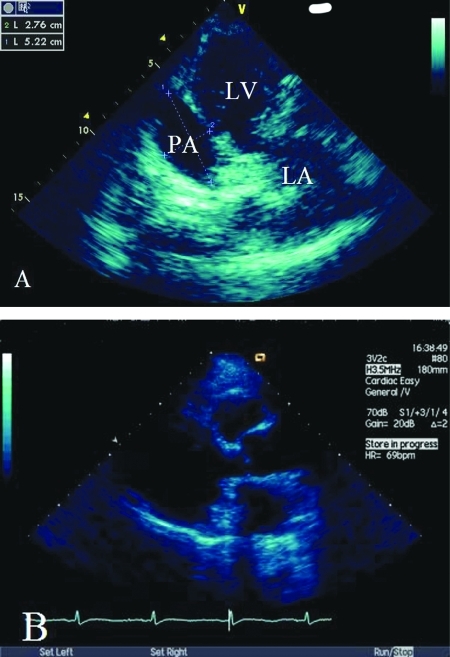
She was referred to our tertiary care hospital for cardiac catheterization. Coronary angiography demonstrated two-vessel disease. The LAD was totally occluded from the proximal segment, and there was 90% stenosis at the middle portion of the right coronary artery (Fig. 1). The saphenous vein conduit from aorta to mid-LAD was patent. Left ventriculography revealed inferior hypokinesia, moderate MR, and a pseudoaneurysm sac located at the inferoposterior wall of the left ventricle (Fig. 1). Transthoracic echocardiography showed a pseudoaneurysm sac with 5.2 × 3 cm diameter located at the posterior wall of the left ventricle and moderate MR with global EF of 40% (Fig. 2). The pseudoaneurysm cavity was resected surgically, and mitral valve replacement with a mechanical prosthesis (No. 27, St. Jude Medical Inc., St. Paul, MN) was performed. Control echocardiography showed no signs of previous LV pseudoaneurysm (Fig. 2). She made an uneventful recovery and was sent home after 10 days. At follow-up 1 year after the event, the patient was free of symptoms.
Figure 1.
(A) Left ventriculography demonstrating pseudoaneurysm sac (arrows). (B) Ninety per cent stenosis at middle portion of right coronary artery (arrow). LV, left ventricle; PA, pseudoaneurysm.
Figure 2.
(A) Apical two-chamber view showing pseudoaneurysm sac. (B) Postoperative parasternal long axis view with no signs of pseudoaneurysm. LA, left atrium; LV, left ventricle; PA, pseudoaneurysm.
DISCUSSION
Left ventricular pseudoaneurysm is a free wall rupture sealed by adherent pericardium together with organizing thrombus, and most commonly occurs after transmural infarctions.3 The other causes are surgery, trauma, and infection.3 Patients usually present with symptoms such as dyspnea, heart failure, or angina. However, ~10% of patients are asymptomatic at the time of diagnosis.3 On physical examination, a systolic murmur can be heard when there is an associated MR. Sometimes a to-and-fro murmur can be noticed, which is produced by blood flowing in and out of the pseudoaneurysm.6 LV pseudoaneurysm occurs more frequently in elderly patients. It is most commonly seen after inferior MI and usually located at the posterior wall.3 Compared with primary percutaneous coronary intervention, the risk of rupture after MI is higher with thrombolytic therapy.7 Myocardial rupture and LV pseudoaneurysms are mostly seen after large infarcts with peak CPK-MB levels >150 IU/mL.4 On the contrary, in our case the size of infarction was not large, with the highest value of CPK-MB level being 98 IU/mL. LV pseudoaneurysms occur most commonly 1 to 4 days after infarction, and because of this, initial evaluation of the patient may not reveal any abnormality.3 Although different imaging modalities exist, the most reliable method for diagnosing LV pseudoaneurysm is angiography.3 Other imaging methods are echocardiography, computed tomography, and magnetic resonance imaging. Once the diagnosis is established, urgent surgery is recommended for LV pseudoaneurysms detected in the first 3 months after MI because the risk of fatal rupture is high.8 Published series report postoperative mortality rates ranging between 7 and 30%.3,9 However, management of chronic LV pseudoaneurysms is controversial, and risk of rupture and embolism should be weighed against the estimated risk of surgery. Moreno et al reported a cumulative survival of 74.1% at 4 years with conservative management of patients with chronic LV pseudoaneurysm.10
Our case has similar properties to those in the previous reports published in the literature. However, the interesting point is that a small-sized infarction with a peak CPK-MB level of 98 IU/mL was the cause of LV pseudoaneurysm. In conclusion, LV pseudoaneurysm should be suspected in patients presenting with heart failure symptoms after an asymptomatic period following acute MI. Urgent surgery is lifesaving in this condition.
References
- Dachman A H, Spindola-Franco H, Solomon N. Left ventricular pseudoaneurysm. Its recognition and significance. JAMA. 1981;246:1951–1953. [PubMed] [Google Scholar]
- Csapo K, Voith L, Szuk T, Edes I, Kereiakes D J. Postinfarction left ventricular pseudoaneurysm. Clin Cardiol. 1997;20:898–903. doi: 10.1002/clc.4960201021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frances C, Romero A, Grady D. Left ventricular pseudoaneurysm. J Am Coll Cardiol. 1998;32:557–561. doi: 10.1016/s0735-1097(98)00290-3. [DOI] [PubMed] [Google Scholar]
- Pohjola-Sintonen S, Muller J E, Stone P H, et al. Ventricular septal and free wall rupture complicating acute myocardial infarction: experience in the Multicenter Investigation of Limitation of Infarct Size. Am Heart J. 1989;117:809–818. doi: 10.1016/0002-8703(89)90617-0. [DOI] [PubMed] [Google Scholar]
- Eren E, Bozbuga N, Toker M E, et al. Surgical treatment of post-infarction left ventricular pseudoaneurysm: a two-decade experience. Tex Heart Inst J. 2007;34:47–51. [PMC free article] [PubMed] [Google Scholar]
- Turgeman Y, Antonelli D, Rosenfeld T. Intermittent to-and-fro murmur in cardiac pseudoaneurysm: Doppler echocardiographic findings. Int J Cardiol. 1990;26:376–377. doi: 10.1016/0167-5273(90)90099-q. [DOI] [PubMed] [Google Scholar]
- Birnbaum Y, Chamoun A J, Anzuini A, Lick S D, Ahmad M, Uretsky B F. Ventricular free wall rupture following acute myocardial infarction. Coron Artery Dis. 2003;14:463–470. doi: 10.1097/00019501-200309000-00008. [DOI] [PubMed] [Google Scholar]
- Milgalter E, Uretzky G, Levy P, Appelbaum A, Borman J B. Pseudoaneurysm of the left ventricle. Thorac Cardiovasc Surg. 1987;35:20–25. doi: 10.1055/s-2007-1020191. [DOI] [PubMed] [Google Scholar]
- Yeo T C, Malouf J F, Oh J K, Seward J B. Clinical profile and outcome in 52 patients with cardiac pseudoaneurysm. Ann Intern Med. 1998;128:299–305. doi: 10.7326/0003-4819-128-4-199802150-00010. [DOI] [PubMed] [Google Scholar]
- Moreno R, Gordillo E, Zamorano J, et al. Long term outcome of patients with postinfarction left ventricular pseudoaneurysm. Heart. 2003;89:1144–1146. doi: 10.1136/heart.89.10.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]