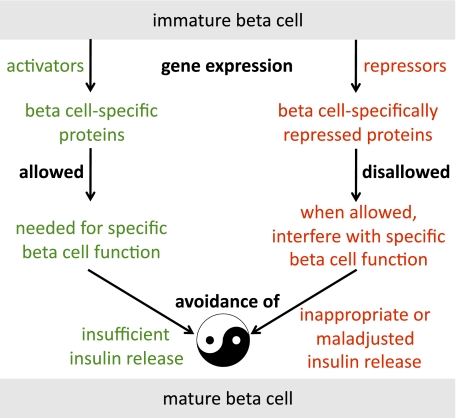
What makes β-cells unique is their continuous responsibility to produce, store and release the required amount of insulin to keep blood glucose normal. This is no trivial task because daily insulin demands fluctuate acutely (as happens during meals) or chronically (e.g., the adaptation to obesity or pregnancy). Moreover, normal blood glucose has two borders that need continuous protection. Insufficient insulin secretion should be avoided as this leads to hyperglycemia. Moreover, insulin excess causes hypoglycemia, a situation that jeopardizes brain function. Therefore, the optimal amount of β-cell activity is needed for normal health and this depends on an adequate plasticity of the functional β-cell mass (1). This Perspective examines the idea that protection of the two borders of blood glucose requires a genetically programmed β-cell phenotype with two unique faces (Fig. 1). The first depends on transcription factors that activate expression of specific proteins that mediate β-cell function. The second face depends on β-cell–specific repression of a small set of genes. We start to understand how expression of the latter genes may impair normal β-cell function. The best examples of expression of such “disallowed” genes in β-cells lead to inappropriate insulin release (2).
FIG. 1.
A balance between two faces of the mature β-cell. The general working hypothesis in this Perspective is that the mature β-cell needs to defend both the upper and lower normal limits of circulating glucose levels, thereby preventing the occurrence of episodes of hyperglycemia and hypoglycemia. A genetically determined β-cell program is responsible for the appropriate expression level of proteins in β-cells that allow a physiological response in terms of sufficient release of insulin when the organism needs the hormone. In parallel, some genes are specifically repressed in β-cells in order to avoid situations where β-cells respond inappropriately (induction by the wrong stimuli) or in a maladjusted manner (wrong amplitude of insulin release after normal stimuli). As concerns the latter possibility, one can speculate that protection might exist against excessive amounts of circulating insulin by repressing genes whose encoded proteins would allow an abnormally enlarged β-cell mass.
How islet-specifically repressed genes were identified
The idea of “disallowed” β-cell genes originated from studies on glucose phosphorylation, the first flux-generating step of glucose signaling in β-cells. Four different genes encode for enzyme isoforms that can catalyze this step, but only glucokinase (hexokinase 4) is expressed in mature β-cells, whereas the other hexokinases, in particular hexokinase 1, are profoundly repressed (3). Evolution has favored a developmental program based on repression of low Km-hexokinases in maturing β-cells because this prevents insulin release in the fasted state, when circulating glucose is low (2). Another “disallowed” gene in β-cells is Mct1 (Slc16a1) (4). The encoded protein is a monocarboxylate transporter that facilitates diffusion of lactate and pyruvate across the plasma membrane of most cells in order to sustain ATP production by anaerobic glycolysis. In β-cells, however, MCT1 protein needs to be very low in order to prevent inappropriate insulin release triggered by circulating pyruvate. In a rare genetic disease called exercise-induced hyperinsulinism a mutation in the Mct1 promoter leads to MCT1 production in β-cells, causing hypoglycemia (4).
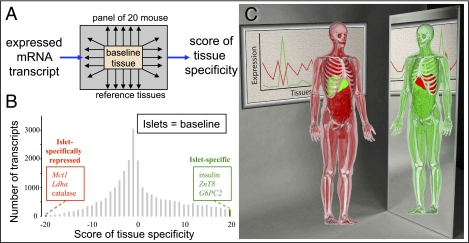
These examples suggesed that other proteins could also be repressed in β-cells in order to allow normal insulin release. In order to find genes that are preferentially or specifically expressed in mouse islets, we compared the mRNA expression profiles of freshly isolated islets with a panel of 20 other mouse tissues (Fig. 2A) (5). On the basis of these comparisons, we calculated a tissue specificity score for each of the expressed mRNA species in the panel. This resulted in a distribution plot shown for islets in Fig. 2B for the collective transcriptome. The rightmost category contains a group of genes that are preferentially or specifically expressed in pancreatic islets, insulin 1 and insulin 2 and the other islet hormone genes being examples. On the basis of this information, we further studied some of these genes in detail (6–8). Unexpectedly, at the extreme left of the same plot there is a category of mRNA species that are significantly more expressed in all tissues in the panel than in islets (5). This result further illustrated the idea that large differences exist between tissues in the expression level of ubiquitously expressed genes (9). We confirmed the result by a Bayesian approach based on the intersection-union test (5) and found a largely overlapping set of genes that are islet-specifically repressed. In order to get an overall error rate of 0.05 for the total of 17,344 tested genes, the intersection-union test was performed with multiple comparison correction resulting in a significance level of 3 × 10−6 for individual tested genes. The used strategy was applicable to any tissue in the panel, indicating that tissue-specifically repressed genes may have a broad biological significance that still largely needs to be defined. The chosen strategy for finding tissue-specific gene repression was also applied to the liver as baseline instead of islets (5), and this resulted in the identification of liver-specifically repressed genes as the mirror situation of liver-specific genes (Fig. 2C). Thus, we can draw the conclusion that the specialized phenotype of any particular cell type may not only reflect expression of tissue-specific genes but also an opposite phenomenon of cell type–specific gene repression.
FIG. 2.
Tissue-specific repression of gene expression. A: The phenomenon was discovered by performing genome-wide mRNA expression analysis of total mRNA extracted from freshly isolated islets as compared with 20 different tissues from the same mice. For all transcripts that are expressed in one or more tissues, statistical analysis allows to search for islet-specifically repressed genes (5). B: One way to visualize such genes is to plot for all transcripts the distribution of the sum score of significant comparisons (20 comparisons made between islets and members of the panel and for each comparison a score of −1, 0, and +1 when the transcript is less, equally, or more abundant in islets, respectively). The category with a sum score of −20 contains the islet-specifically repressed genes. C: The same concept can be applied to other tissues and organs such as the liver (5). At the left side of this cartoon, a liver-specific gene is shown with high expression (green) in contrast with background mRNA expression (red) in the rest of the organism. This situation is mirrored by a liver-specifically repressed gene such as Oxct1, for which mRNA is abundant in all tissues (green) except in the liver (red). This gene encodes a key enzyme of ketone body breakdown, whereas the liver is a ketone body–exporting tissue.
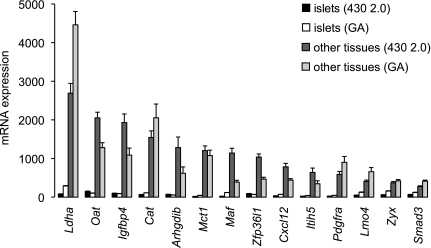
We next considered potential artifacts that may give false-positive or false-negative results. One source of false positives is transcript variation. Indeed, it is possible that a gene is truly expressed in all tissues, but that it forms one transcript variant that is not produced in islets. The probe set that would measure this variant would generate data suggesting that the gene is not expressed in islets. To investigate this possibility, we repeated the analysis with exon-oriented Affymetrix Gene microarrays and found good overlap with the results obtained with 3′UTR-oriented Affymetrix 430 2.0 arrays (Fig. 3). False-positives can also result from common cell types that are present in the tissue panel but that are artificially excluded in the baseline tissue. This is important for collagenase-isolated islets because a possible artifact is that circulating blood cells are washed out. We shortened the collagenase isolation to 3 min digestion followed by several sedimentation steps at 1 × g in order to obtain ex vivo RNA (10). As a result, significant amounts of blood cells were still present, and abundant erythrocyte and lymphocyte mRNA signals (e.g., α- and β-globins, Ly6 genes) were in the range of the tissues panel. More false-positives of this type are expected when purified β-cells are compared with the tissue panel. On the other hand, when islets are used instead of pure β-cells, false-negatives occur because repression in β-cells is masked by high expression in contaminating exocrine cells and/or non–β-cells. This point was illustrated before by measuring hexokinase 1 in purified pancreatic β-cells and acinar cells (3). In order to assess this contamination effect, we measured mRNA expression for islet-repressed genes in fluorescence-activated cell sorter–purified β-cells and obtained even lower signals (5). Together, the approach with a tissue/organ reference panel requires properly isolated islets as a baseline. In order to refine the search for genes that are selectively repressed in β-cells, a new reference panel with other purified primary cell types will be needed.
FIG. 3.
Islet-specifically repressed genes in the mouse. Data are from Thorrez et al. (5) and represent mean mRNA expression signals + SEM for 14 genes that were identified with two different types mRNA expression arrays as being specifically repressed in isolated islets as compared with a panel of mouse tissues. Islet expression levels are black and white bars, and mean tissue panel expression are dark and light gray bars. Dark shades, Affymetrix 430 2.0 array (oriented to the 3′UTR of transcripts); light shades, Affymetrix Mo Gene 1.0 arrays (probes oriented to all exons). GA, gene array.
Islet-specific gene repression starts when β-cells mature
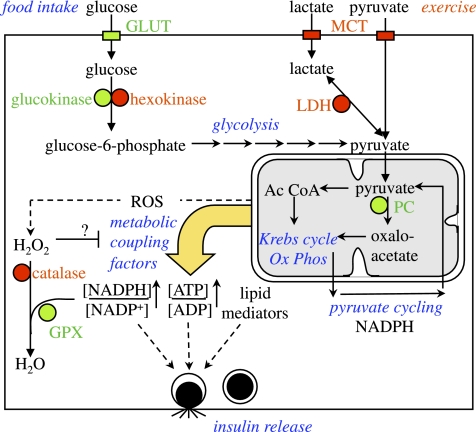
Progress in regenerative medicine brings closer the idea of replacing the functional β-cell mass in patients with type 1 diabetes with an alternative source of cells (11). Considering the hypothesis of Fig. 1, it may be important to understand how normal β-cells mature not only in terms of β-cell–specific function and specialized metabolic signaling (12) but also in terms of avoiding inappropriate insulin release. Together with Susan Bonner-Weir and Frederic Lemaigre, we observed that tissue-specific repression of genes unfolds in parallel with tissue-selective gene expression, both in neonatal rat islets and in fetal liver (5). One example is the important crossroad of pyruvate metabolism (Fig. 4): β-cell maturation can be measured both as increased pyruvate carboxylase expression and repression of lactate dehydrogenase. In adult β-cells, pyruvate carboxylase is abundant and lactate dehydrogenase deeply repressed, explaining anaplerosis and lack of anaerobic glycolysis (13). For the liver, metabolic specialization favors ketogenesis over ketone body oxidation, which is in agreement with liver-specific repression of Oxct1 as opposed to high expression of Hmgcs2 (5).
FIG. 4.
Appropriate versus inappropriate insulin release. Normal stimulation of insulin release as occurs after ingesting a carbohydrate-containing meal, which results in a rise in circulating glucose, uptake of the sugar via glucose transporters (GLUT) in β-cells, and metabolism that starts with glucokinase. Glycolysis ends with pyruvate that readily enters the mitochondria where it is oxidizes or starts several metabolic cycles, requiring pyruvate carboxylase (PC) as anaplerotic enzyme. This metabolism generates coupling factors that trigger exocytosis of secretory granules. Inappropriate insulin release is induced by proteins encoded by the islet-repressed genes hexokinase, Ldha, and Mct1 (red). Low Km hexokinases cause elevated basal release in the fasted state, whereas LDHA and MCT1 could mediate exercise-induced release. The rationale for low catalase in β-cells is not known. One possibility is that H2O2 breakdown without catalase requires glutathion peroxidases (GPX) and NADPH, which is formed when glucose levels rise. If H2O2 acts as a signal that counteracts metabolic coupling factors or promotes β-cell apoptosis, the absence of catalase makes this signal glucose regulated. Contribution of hormones and neurotransmitters to the control of insulin release has been omitted in this cartoon.
The regulators that are responsible for the reciprocal time course of preferentially expressed and disallowed genes when β-cells mature need to be further defined. It is possible that overlap exists in the transcription factors that activate/repress in a context-dependent manner. Genome-wide analysis of the histone code in islets and other mouse tissues indicates that activation and repression marks for gene transcription arise when β-cells differentiate (14). In agreement with this idea, trimethylation of lysine-27 of histone 3, a mark for polycomb-mediated gene inactivation, is high in the gene promoter region of Ldha, Mct1, and other repressed islet genes in the mouse (5). Posttranscriptional regulation by microRNAs could further contribute to tissue-specific repression as is suggested by experiments in the maturing liver where miR-122 repressed Oxct1 mRNA (5). We further predicted that other tissue-specifically repressed mRNAs can be targeted by microRNA isoforms, which are abundant in the tissue where mRNA repression occurs (5). For Mct1 and β-cells, experimental evidence was indeed provided for repression via miR-29 (15), but a developmental context still needs to be established. Both histone modifications and microRNA’s create a multitier mechanism of islet-specific repression of genes.
One important area of further research is the possible failure of islet-specific gene repression in diabetes. Very little is known about this subject in human diabetes. In animal models, however, detailed information is known for Ldha. In a pioneering article, Jonas et al. (16) showed that significant upregulation of Ldha mRNA is the result of chronic exposure of isolated rat islets to hyperglycemia. Laybutt et al. (17) then showed that this derepression of the Ldha gene in islets also occurs in vivo in diabetic animals, and that this loss of repression is paralleled by a loss of expression of the β-cell transcription factors PDX1, NKX6–1, and PAX6. As the epigenetic marks of the Ldha-gene in the adult mouse islets are strongly repressive (5), it is of interest to understand how derepression occurs. One possibility is that PDX1, NKX6–1, or PAX6 (or a combination of these) act as repressors of the Ldha gene so that reduced expression of these factors causes both loss of β-cell maturation and derepression of the Ldha-gene.
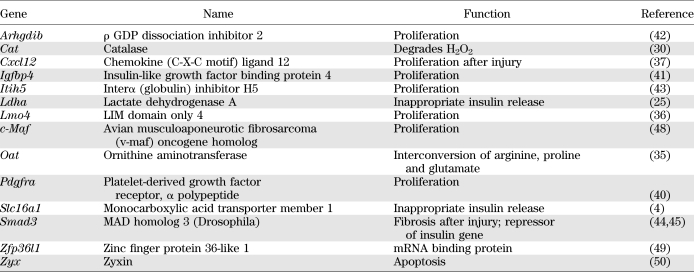
Another issue that needs to be better understood is why some genes need to be specifically repressed in β-cells. For most of these genes, we can only speculate how repression contributes to β-cell function. Some may protect against excessive β-cell growth or inappropriate secretion of insulin, whereas others might reduce insulin production by interfering with the work of normal β-cell proteins. It should be emphasized at this stage that, although there is reasonable amount of evidence to support the concept of inappropriate insulin release, the idea of protection against excessive β-cell growth is more speculative and needs to be further investigated. In the next two sections, we will discuss the idea that at least some of the genes in Table 1 and Fig. 3 would, when not repressed, cause either inappropriate insulin release or rates of insulin release induced by physiological stimuli that are poorly adjusted to physiological demands.
TABLE 1.
Function of mouse islet-specifically repressed genes
Islet-specific gene repression to prevent inappropriate release of insulin
Inappropriate release of insulin means that β-cells secrete insulin under conditions where the organism does not need extra insulin. This is in contrast with physiological stimulation of insulin release as occurs after a meal when blood glucose levels rise (Fig. 4). For the sake of brevity, we do not consider in this Perspective the important contribution of hormones (incretins, glucagon, somatostatin, adrenaline) and neurotransmitters (noradrenaline, acetylcholine) that modulate the amplitude of glucose-induced insulin release of β-cells. Instead, we will focus on some aspects of glucose stimulation. Normal β-cells respond within minutes to elevated extracellular glucose, as these cells use glucose metabolism as a sensing and signaling system (18). Metabolic control in normal β-cells is different from regulatory strategies that other cell types use to maintain ATP, ADP, and other important metabolites as constant as possible. The importance of high-Km glucokinase to control glycolytic flux in β-cells (19) was already emphasized above. Glycolysis ends with pyruvate, which most cells partially reduce to lactate. In β-cells, however, pyruvate is very efficiently taken up by the mitochondria where it is either oxidized to CO2 or used as substrate for different metabolic cycles (20) that are linked to NADPH production (21) and generation of lipid messengers (22). In most other cell types, MCT1 and LDHA ensure anaerobic glycolysis during hypoxia. Production and cellular efflux of lactate and pyruvate maintains ATP production, even when mitochondrial oxidation is low. In contrast, β-cells exhibit an aerobic glycolysis (13) and contain low amounts of LDHA (23) and MCT1 (24). This is explained by the fact that the Mct1 and Ldha genes are deeply and islet-specifically repressed (5). The rationale of this repression is illustrated by in vitro experiments and by a human genetic disease. Forced expression of MCT1 in INS1 cells caused pyruvate-stimulated insulin release, while overexpression of both MCT1 and LDHA were needed for lactate-stimulated release (25). In exercise-induced hyperinsulinism, inappropriately high levels of circulating insulin are found shortly after physical exercise or after pyruvate injection (26). These patients have mutations in the Mct1 promoter (4), and it is believed that such mutations destroy regulatory site(s) that allow repression in mature β-cells. From an evolutionary standpoint, such inappropriate insulin release would seem problematic because the struggle for life usually requires exercise; when this would lead to hypoglycemia it would impair the brain’s ability to plan a survival strategy. Although other cell types need MCT1 and LDHA to adapt metabolism to hypoxia, it remains to be understood how β-cells can cope with insufficient oxygen supply when these genes are not expressed. Very high blood flow rates may protect against hypoxia. Indeed, islet tissue represents less than 1% of pancreatic mass but receives 6% of pancreatic blood flow; when calculated per minute and per gram tissue, islet blood flow is among the highest in the organism (27). However, local variations in islet oxygenation exist in the normal pancreas, and it was recently proposed that the poorly oxygenated islets represent a functional reservoir (28). This could indicate that, in addition to other aspects of heterogeneity among individual β-cells (29), normal pancreatic β-cells may differ in the degree of repression of islet-specifically repressed genes, but there is no experimental evidence to support this idea.
In addition to LDHA, two other enzymes—catalase and ornithine aminotransferase—are selectively repressed in mouse islets (Fig. 3), but a direct influence of this repression on insulin release has not been demonstrated so far. For many years it has been known that rodent β-cells contain very low levels of catalase (30), and this lack may explain the great sensitivity of β-cells for oxidative stress (31). Catalase reconverts hydrogen peroxide (H2O2) to water and oxygen. An interesting difference exists with glutathion peroxidases (Fig. 4) because the latter enzymes require NADPH. Because NADPH levels in β-cells strongly depend on glucose metabolism (21), it is possible that the accumulation of H2O2 at low glucose levels may serve to prevent inappropriate insulin release. However, it should be mentioned that the role of repression of catalase to allow physiological control of insulin release is hypothetical because mice with overexpression of a catalase transgene in β-cells did not have abnormal insulin release (32). This could still mean that if repression of catalase prevents inappropriate insulin release, the conditions under which this might occur have not yet been identified. Another possibility that needs perhaps further investigation is that low catalase in β-cells could allow the buildup of oxidative stress at chronic low glucose in order to favor β-cell apoptosis (33). One can only speculate about the profound repression of ornithine aminotransferase (OAT) in β-cells. In the liver, this enzyme connects arginine and glutamate metabolism (34), and congenital enzyme deficiency causes hyperammonemia and blindness due to gyrate atrophy of the choroid and retina (35). Lack of this mitochondrial enzyme in β-cells could for instance help prevent anaplerosis of amino acid carbon into the Krebs cycle when circulating amino acids rise without an elevation of blood glucose, such as occurs after a protein-rich carbohydrate-depleted meal.
Islet-specific gene repression to prevent maladjusted insulin secretion induced by physiological stimuli
In addition to inappropriate insulin release, the amount of secretion after physiological stimuli can be maladjusted to the amounts that are needed. One can speculate about the possibility that islets repress expression of growth promoting genes in order to prevent the pancreatic β-cell mass from expanding too much. This hypothesis can be made on the basis of the observation that several genes shown in Table 1 and Fig. 3 are linked to cell proliferation in general and β-cell proliferation specifically in some recent studies. LIM-domain only 4 (Lmo4) encodes a transcriptional regulatory protein that is responsible for multiple protein-protein contacts in the nucleus. LMO4 overexpression is found in mammary gland tumors and pancreatic cancer. LMO4 silencing resulted in G2/M arrest of the cell cycle, interfering with a mitotic signaling pathway that depends on activation of Erbb2, a member of the epidermal growth factor–receptor tyrosine kinase family (36).
Another example of a widely expressed gene that stimulates cell proliferation is Cxcl12, also known as stromal cell–derived factor-1. The encoded protein is a small chemokine that binds primarily to CXC receptor 4 (CXCR4) leading to enhanced β-cell proliferation triggered by the activation of the protein kinase Akt and WNT signaling (37). In a recent study, Habener and colleagues (38) propose that Cxcl12 expression is present in the neonatal pancreas but declines to undetectable levels at 2 months of age. Interestingly, the expression of Cxcl12 in mature β-cells could be boosted by β-cell injury, and the authors propose that this reactivation may be an essential component of the capacity of rodent β-cells to regenerate after injury (38).
Perhaps the same is true for Pdgfra, the gene that encodes the platelet-derived growth factor receptor α polypeptide, a widely expressed tyrosine kinase receptor that stimulates cell proliferation in many tissues. A pioneering study on growth factor receptors indicated that overexpression of PDGF β-receptor stimulated β-cell replication, whereas cotransfection with the PDGF α-receptor limited this growth response (39). However, more recent work by Kim and colleagues (40) indicated that a crucial stimulatory alpha-type platelet-derived growth factor receptor (PDGFRA)-dependent pathway for pancreatic β-cell growth exists. One of the key observations in this study was that PDGFRA expression in mouse and human islets declines with age in a manner that may explain the loss of β-cell replicative potential in older individuals. An interesting aspect of the study is that forced overexpression of the receptor in PDGFRA-transgenic mice led to a phenotype with three times higher β-cell mass, significantly lower postprandial blood glucose, and improved glucose tolerance (40). It will be interesting to see how these mice tolerate the fasted state.
Four more genes listed in Table 1 influence proliferation, but the link to islet biology is uncertain. Insulin-like growth factor binding protein 4 (Igfbp4) is highly expressed in many tissues, and encodes a small secreted protein that regulates insulin-like growth factor 1; in some circumstances this protein can promote cellular growth (41). Rho GDP dissociation inhibitor 2 (Arhgdib) plays a role in tumor growth and metastasis (42). The same applies to interα (globulin) inhibitor H5 (Itih5) that acts as a tumor suppressor that stabilizes the extracellular matrix and prevents tumor metastasis (43).
A special case among the islet-specifically repressed genes is mothers against decapentaplegic (MAD) homolog 3 (Drosophila) (Smad3), because the maladjustment that needs to be avoided is insufficient insulin release triggered by normal stimuli. In many tissues, SMAD3 is a key factor in the fibrotic response to chronic injury accompanied by transforming growth factor β receptor stimulation (44). In pancreatic β-cells, however, SMAD3 binds on the E2-box of the insulin promoter so that it represses insulin gene transcription (45). Low expression of Smad3 in β-cells may therefore beneficial to allow normal control of the insulin gene by PDX1 and other β-cell transcription factors, resulting in normal insulin biosynthesis after glucose stimulation. Although Smad3 seems to be an exception to the model presented in Fig. 3, it forms a unifying theme together with Cxcl12 and Pdgfra: the idea that wound healing factors that aid to the regeneration response in other tissues need to be restrained in β-cells in order to keep circulating insulin levels in the normal range. One could argue that, as long as β-cells are properly controlled by glucose, an increased β-cell number would not be a risk factor for hypoglycemia. It is conceivable however that the newly replicated β-cells in adult pancreata start as immature cells that are not properly controlled by metabolic coupling factors, analogous to what was found in neonatal β-cells (12). In particular, further investigation is needed to assess when newly formed β-cells (that arise in models of enhanced β-cell proliferation or β-cell neogenesis) repress genes that would predispose to inappropriate or maladjusted insulin release.
From islet-specific repression in mice to “disallowed” human β-cell genes
In this article we have discussed the available evidence for the idea that a genetically programmed phenomenon of islet-specific gene repression contributes to the avoidance of inappropriate insulin release. Moreover, as some of the islet-specifically repressed genes encode proteins that stimulate β-cell proliferation, one can speculate that another level of protection against excess circulating insulin is the avoidance of a too high pancreatic β-cell mass. More research is needed in order to better understand how each of the islet-specifically repressed genes contributes to the phenotype of normal β-cells. Is the function of the encoded protein really detrimental for β-cells, so that we can call the gene “disallowed” in β-cells (2)? Or do we measure the extreme end of a stochastical distribution of mRNA expression levels among tissues, in the sense that β-cells can work normally with very low levels of gene expression but would also functionally tolerate higher expression levels? The distinction between these two possibilities can perhaps be made by measuring the consequence of forced gene expression experiments, either by transfection in vitro or by transgenic mice. When consequences of forced expression experiments in β-cells are significant, it will be relevant to better understand the precise development of the repressive machinery during β-cell maturation. Another aspect that needs further study is whether or not mouse data of islet-specific repression can be extrapolated to human β-cells. As was shown before for glucose transport (46) and oxygen radical-induced repair (47), major differences can exist between rodent and human islets. At the level of tissue panels, we found reasonable overlap for genes that are tissue-specifically repressed in mice and humans, but islets were not included in the analysis (5). When repression in β-cells is evolutionarily conserved, as appears to be the case for MCT1, the important conclusion is that two faces of the mature phenotype of human β-cells are needed to protect against excursions across the borders of normoglycemia. Further studies of this novel concept will be necessary to understand the true identity of primary β-cells; this knowledge will help research efforts aiming at the generation of β-cells from stem cells. Finally the protection against maladjusted insulin release by restraining growth and wound repair gene signaling in β-cells needs further investigation as novel insight might contribute to understanding the problem of a low functional β-cell mass in patients with type 2 diabetes.
ACKNOWLEDGMENTS
Studies of islet-specifically repressed genes in the laboratory of the authors are financially supported by the Juvenile Diabetes Research Foundation (JDRF Grant 2006-182), the Fonds voor Wetenschappelijk Onderzoek Vlaanderen (FWO Grant G.0672.12), the Belgian Science Policy (Interuniversity Attraction Poles Program [PAI 6/40]), and the Katholieke Universiteit Leuven (GOA/2009/10).
F.S. researched data and wrote the manuscript. L.V.L. and M.G. researched data and reviewed and edited the manuscript. L.G. and G.d.F. contributed to discussion and reviewed and edited the manuscript. A.S. researched data, contributed to discussion, and reviewed and edited the manuscript. K.L. researched data, wrote the manuscript, and contributed to discussion. F.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Dr. Susan Bonner-Weir and Dr. Gordon Weir (Joslin Diabetes Center, Boston, MA) and Timo Otonkoski (Biomedicum Stem Cell Centre, University of Helsinki, Helsinki, Finland) for insightful discussion and comments after reading the manuscript; and Lieven Thorrez and Stefan Lehnert (Katholieke Universiteit Leuven, Belgium) for making Figure 2C.
REFERENCES
- 1.Bernard-Kargar C, Ktorza A. Endocrine pancreas plasticity under physiological and pathological conditions. Diabetes 2001;50(Suppl. 1):S30–S35 [DOI] [PubMed] [Google Scholar]
- 2.Quintens R, Hendrickx N, Lemaire K, Schuit F. Why expression of some genes is disallowed in beta-cells. Biochem Soc Trans 2008;36:300–305 [DOI] [PubMed] [Google Scholar]
- 3.Schuit F, Moens K, Heimberg H, Pipeleers D. Cellular origin of hexokinase in pancreatic islets. J Biol Chem 1999;274:32803–32809 [DOI] [PubMed] [Google Scholar]
- 4.Otonkoski T, Jiao H, Kaminen-Ahola N, et al. Physical exercise-induced hypoglycemia caused by failed silencing of monocarboxylate transporter 1 in pancreatic beta cells. Am J Hum Genet 2007;81:467–474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thorrez L, Laudadio I, Van Deun K, et al. Tissue-specific disallowance of housekeeping genes: the other face of cell differentiation. Genome Res 2011;21:95–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colsoul B, Schraenen A, Lemaire K, et al. Loss of high-frequency glucose-induced Ca2+ oscillations in pancreatic islets correlates with impaired glucose tolerance in Trpm5-/- mice. Proc Natl Acad Sci USA 2010;107:5208–5213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lemaire K, Moura RF, Granvik M, et al. Ubiquitin fold modifier 1 (UFM1) and its target UFBP1 protect pancreatic beta cells from ER stress-induced apoptosis. PLoS ONE 2011;6:e18517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lemaire K, Ravier MA, Schraenen A, et al. Insulin crystallization depends on zinc transporter ZnT8 expression, but is not required for normal glucose homeostasis in mice. Proc Natl Acad Sci USA 2009;106:14872–14877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thorrez L, Van Deun K, Tranchevent LC, et al. Using ribosomal protein genes as reference: a tale of caution. PLoS One 2008;3:e1854 [DOI] [PMC free article] [PubMed]
- 10.Van Lommel L, Janssens K, Quintens R, et al. Probe-independent and direct quantification of insulin mRNA and growth hormone mRNA in enriched cell preparations. Diabetes 2006;55:3214–3220 [DOI] [PubMed] [Google Scholar]
- 11.Aguayo-Mazzucato C, Bonner-Weir S. Stem cell therapy for type 1 diabetes mellitus. Nat Rev Endocrinol 2010;6:139–148 [DOI] [PubMed] [Google Scholar]
- 12.Jermendy A, Toschi E, Aye T, et al. Rat neonatal beta cells lack the specialised metabolic phenotype of mature beta cells. Diabetologia 2011;54:594–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schuit F, De Vos A, Farfari S, et al. Metabolic fate of glucose in purified islet cells. Glucose-regulated anaplerosis in beta cells. J Biol Chem 1997;272:18572–18579 [DOI] [PubMed] [Google Scholar]
- 14.van Arensbergen J, García-Hurtado J, Moran I, et al. Derepression of Polycomb targets during pancreatic organogenesis allows insulin-producing beta-cells to adopt a neural gene activity program. Genome Res 2010;20:722–732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pullen TJ, da Silva Xavier G, Kelsey G, Rutter GA. miR-29a and miR-29b contribute to pancreatic beta-cell-specific silencing of monocarboxylate transporter 1 (Mct1). Mol Cell Biol 2011;31:3182–3194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jonas JC, Sharma A, Hasenkamp W, et al. Chronic hyperglycemia triggers loss of pancreatic beta cell differentiation in an animal model of diabetes. J Biol Chem 1999;274:14112–14121 [DOI] [PubMed] [Google Scholar]
- 17.Laybutt DR, Hawkins YC, Lock J, et al. Influence of diabetes on the loss of beta cell differentiation after islet transplantation in rats. Diabetologia 2007;50:2117–2125 [DOI] [PubMed] [Google Scholar]
- 18.Malaisse WJ, Sener A, Herchuelz A, Hutton JC. Insulin release: the fuel hypothesis. Metabolism 1979;28:373–386 [DOI] [PubMed] [Google Scholar]
- 19.Matschinsky FM. Glucokinase as glucose sensor and metabolic signal generator in pancreatic beta-cells and hepatocytes. Diabetes 1990;39:647–652 [DOI] [PubMed] [Google Scholar]
- 20.Jensen MV, Joseph JW, Ronnebaum SM, Burgess SC, Sherry AD, Newgard CB. Metabolic cycling in control of glucose-stimulated insulin secretion. Am J Physiol Endocrinol Metab 2008;295:E1287–E1297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ivarsson R, Quintens R, Dejonghe S, et al. Redox control of exocytosis: regulatory role of NADPH, thioredoxin, and glutaredoxin. Diabetes 2005;54:2132–2142 [DOI] [PubMed] [Google Scholar]
- 22.Nolan CJ, Prentki M. The islet beta-cell: fuel responsive and vulnerable. Trends Endocrinol Metab 2008;19:285–291 [DOI] [PubMed] [Google Scholar]
- 23.Sekine N, Cirulli V, Regazzi R, et al. Low lactate dehydrogenase and high mitochondrial glycerol phosphate dehydrogenase in pancreatic beta-cells. Potential role in nutrient sensing. J Biol Chem 1994;269:4895–4902 [PubMed] [Google Scholar]
- 24.Zhao C, Wilson MC, Schuit F, Halestrap AP, Rutter GA. Expression and distribution of lactate/monocarboxylate transporter isoforms in pancreatic islets and the exocrine pancreas. Diabetes 2001;50:361–366 [DOI] [PubMed] [Google Scholar]
- 25.Ishihara H, Wang H, Drewes LR, Wollheim CB. Overexpression of monocarboxylate transporter and lactate dehydrogenase alters insulin secretory responses to pyruvate and lactate in beta cells. J Clin Invest 1999;104:1621–1629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Otonkoski T, Kaminen N, Ustinov J, et al. Physical exercise-induced hyperinsulinemic hypoglycemia is an autosomal-dominant trait characterized by abnormal pyruvate-induced insulin release. Diabetes 2003;52:199–204 [DOI] [PubMed] [Google Scholar]
- 27.Lifson N, Lassa CV, Dixit PK. Relation between blood flow and morphology in islet organ of rat pancreas. Am J Physiol 1985;249:E43–E48 [DOI] [PubMed] [Google Scholar]
- 28.Olsson R, Carlsson PO. A low-oxygenated subpopulation of pancreatic islets constitutes a functional reserve of endocrine cells. Diabetes 2011;60:2068–2075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schuit FC, In’t Veld PA, Pipeleers DG. Glucose stimulates proinsulin biosynthesis by a dose-dependent recruitment of pancreatic beta cells. Proc Natl Acad Sci USA 1988;85:3865–3869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lenzen S, Drinkgern J, Tiedge M. Low antioxidant enzyme gene expression in pancreatic islets compared with various other mouse tissues. Free Radic Biol Med 1996;20:463–466 [DOI] [PubMed] [Google Scholar]
- 31.Elsner M, Gehrmann W, Lenzen S. Peroxisome-generated hydrogen peroxide as important mediator of lipotoxicity in insulin-producing cells. Diabetes 2011;60:200–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li X, Chen H, Epstein PN. Metallothionein and catalase sensitize to diabetes in nonobese diabetic mice: reactive oxygen species may have a protective role in pancreatic beta-cells. Diabetes 2006;55:1592–1604 [DOI] [PubMed] [Google Scholar]
- 33.Martens GA, Cai Y, Hinke S, Stangé G, Van de Casteele M, Pipeleers D. Glucose suppresses superoxide generation in metabolically responsive pancreatic beta cells. J Biol Chem 2005;280:20389–20396 [DOI] [PubMed] [Google Scholar]
- 34.Brosnan ME, Brosnan JT. Hepatic glutamate metabolism: a tale of 2 hepatocytes. Am J Clin Nutr 2009;90:857S–861S [DOI] [PubMed] [Google Scholar]
- 35.Ramesh V, McClatchey AI, Ramesh N, et al. Molecular basis of ornithine aminotransferase deficiency in B-6-responsive and -nonresponsive forms of gyrate atrophy. Proc Natl Acad Sci USA 1988;85:3777–3780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Montañez-Wiscovich ME, Seachrist DD, Landis MD, Visvader J, Andersen B, Keri RA. LMO4 is an essential mediator of ErbB2/HER2/Neu-induced breast cancer cell cycle progression. Oncogene 2009;28:3608–3618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu Z, Habener JF. Stromal cell-derived factor-1 promotes survival of pancreatic beta cells by the stabilisation of beta-catenin and activation of transcription factor 7-like 2 (TCF7L2). Diabetologia 2009;52:1589–1598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu Z, Stanojevic V, Avadhani S, Yano T, Habener JF. Stromal cell-derived factor-1 (SDF-1)/chemokine (C-X-C motif) receptor 4 (CXCR4) axis activation induces intra-islet glucagon-like peptide-1 (GLP-1) production and enhances beta cell survival. Diabetologia 2011;54:2067–2076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Welsh M, Claesson-Welsh L, Hallberg A, et al. Coexpression of the platelet-derived growth factor (PDGF) B chain and the PDGF beta receptor in isolated pancreatic islet cells stimulates DNA synthesis. Proc Natl Acad Sci USA 1990;87:5807–5811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen H, Gu X, Liu Y, et al. PDGF signalling controls age-dependent proliferation in pancreatic β-cells. Nature 2011;478:349–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ning Y, Schuller AG, Conover CA, Pintar JE. Insulin-like growth factor (IGF) binding protein-4 is both a positive and negative regulator of IGF activity in vivo. Mol Endocrinol 2008;22:1213–1225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cho HJ, Baek KE, Park SM, et al. RhoGDI2 expression is associated with tumor growth and malignant progression of gastric cancer. Clin Cancer Res 2009;15:2612–2619 [DOI] [PubMed] [Google Scholar]
- 43.Veeck J, Chorovicer M, Naami A, et al. The extracellular matrix protein ITIH5 is a novel prognostic marker in invasive node-negative breast cancer and its aberrant expression is caused by promoter hypermethylation. Oncogene 2008;27:865–876 [DOI] [PubMed] [Google Scholar]
- 44.Flanders KC. Smad3 as a mediator of the fibrotic response. Int J Exp Pathol 2004;85:47–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lin HM, Lee JH, Yadav H, et al. Transforming growth factor-beta/Smad3 signaling regulates insulin gene transcription and pancreatic islet beta-cell function. J Biol Chem 2009;284:12246–12257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.De Vos A, Heimberg H, Quartier E, et al. Human and rat beta cells differ in glucose transporter but not in glucokinase gene expression. J Clin Invest 1995;96:2489–2495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Eizirik DL, Pipeleers DG, Ling Z, Welsh N, Hellerström C, Andersson A. Major species differences between humans and rodents in the susceptibility to pancreatic beta-cell injury. Proc Natl Acad Sci USA 1994;91:9253–9256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nishimura W, Bonner-Weir S, Sharma A. Expression of MafA in pancreatic progenitors is detrimental for pancreatic development. Dev Biol 2009;333:108–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bell SE, Sanchez MJ, Spasic-Boskovic O, et al. The RNA binding protein Zfp36l1 is required for normal vascularisation and post-transcriptionally regulates VEGF expression. Dev Dyn 2006;235:3144–3155 [DOI] [PubMed] [Google Scholar]
- 50.Hervy M, Hoffman LM, Jensen CC, Smith M, Beckerle MC. The LIM protein zyxin binds CARP-1 and promotes apoptosis. Genes Cancer 2010;1:506–515 [DOI] [PMC free article] [PubMed] [Google Scholar]