Abstract
Interactions between spores of Bacillus anthracis and macrophages are critical for the development of anthrax infections, as spores are thought to utilize macrophages as vehicles to disseminate in the host. Here we report a novel mechanism for phagocytosis of B. anthracis spores. Murine macrophage-like cell line RAW264.7, bone marrow derived macrophages and primary peritoneal macrophages from mice were used. The results indicated that activation of the classical complement pathway (CCP) was a primary mechanism for spore phagocytosis. Phagocytosis was significantly reduced in the absence of C1q or C3. C3 fragments were found deposited on the spore surface and the deposition was dependent on C1q and Ca2+. C1q recruitment to the spore surface was mediated by the spore surface protein BclA, as recombinant BclA bound directly and specifically to C1q and inhibited C1q binding to spores in a dose-dependent manner. C1q binding to spores lacking BclA (ΔbclA) was also significantly reduced compared to wild type spores. In addition, deposition of both C3 and C4 as well as phagocytosis of spores were significantly reduced when BclA was absent but were not reduced in the absence of IgG, suggesting that BclA but not IgG is important in these processes. Taken together, these results support a model in which spores actively engage CCP primarily through BclA interaction with C1q, leading to CCP activation and opsonophagocytosis of spores in an IgG-independent manner. These findings are likely to have significant implications on B. anthracis pathogenesis and microbial manipulation of complement.
Introduction
The complement system is an essential component of host immune defenses against microorganisms. Activation of the complement system results in opsonization and phagocytosis of microbes, formation of the membrane attack complex (MAC) and generation of inflammatory modulators (anaphylatoxins), all of which are important elements of immune surveillance and defense against microorganisms. Complement deficiencies result in increased susceptibility to microbial infections (1, 2). On the other hand, some pathogenic microbes have evolved strategies to manipulate the complement system, tipping the defense balance in their own favor (1–3).
Some microbial pathogens evolved strategies to either avoid complement recognition or suppress complement activation. For example, Neisseria meningitidis serogroup B strains express a surface protein that is capable of binding human complement regulator factor H and the binding imparts serum resistance to the pathogen (4–6). Vaccines based on the factor H binding protein showed protective efficacy in preclinical and clinical trials (7–11). Staphylococcus aureus has multiple complement evasion mechanisms that target different components of the complement cascade such as C3, C3 convertases, C5, and C5a receptor (3, 12–21). For intracellular pathogens, gaining entry into host cells is critical for the establishment of infections. A number of intracellular pathogens directly activate the complement system to promote their entry into host cells. For example, mycobacteria are known to activate all three of the complement pathways to promote uptake by professional phagocytes (22–24). The human immunodeficiency virus (HIV) glycoprotein gp41 activates the classical complement pathway (CCP) by binding to complement component C1q, which is the ligand recognition subunit of C1. This leads to opsonization of HIV with C3 fragments and entry into host cells by oposonophagocytosis (25, 26). These diverse strategies utilized by microbial pathogens highlight the importance of the complement system in the interplays between pathogens and the host defense system.
Bacillus anthracis is a spore-forming, gram-positive bacterium that causes anthrax infections. The infections are initiated by the entry of B. anthracis spores into the host via cuts or wounds in the skin, the gastrointestinal tract, or the respiratory system. After entry into the host, spores are taken up by macrophages (27–29), dendritic cells (30–32) and epithelial cells (33). The interactions between spores and these different types of host cells are important for the survival of spores, dissemination of spores from the initial sites of exposure to distal organs (27–31, 34) and germination of spores into vegetative bacilli that are capable of producing the anthrax toxins and other virulence factors (35–37). Thus spore entry into host cells is critical for the development of anthrax infections. This is further demonstrated by findings that disruption of spore uptake by macrophages or epithelial cells significantly improved the survival of infected mice and reduced bacterial burden in different tissues in mouse models of anthrax infections (28, 29, 34).
Due to the importance of spore entry into host cells, a number of studies have investigated the molecular mechanisms mediating spore adherence to and uptake by host cells. Complement receptor 3 (CR3) (also known as Mac-1, integrin αMβ2, and CD11b/CD18) was found to be a receptor mediating spore phagocytosis by macrophages (29). CR3-mediated phagocytosis is dependent on BclA (Bacillus collagen-like protein of anthracis), a major glycoprotein on the surface of B. anthracis spores (29). Mice deficient in CR3 were more resistant to challenges by B. anthracis spores compared to wild type mice (29), suggesting that spore uptake by macrophages is important for the pathogenesis of this microorganism. However, whether BclA directly interacts with CR3 or through intermediate molecules was unclear, nor was the role of the complement system in CR3-mediated phagocytosis of spores. Recently, it was demonstrated that BclA was able to directly bind C1q in a dose-dependent and saturable manner (38). Furthermore C1q acted as a bridging molecule between BclA and integrin α2β1 to mediate B. anthracis spore entry into epithelial cells in a complement activation-independent manner (38).
In this study, we investigated the effect of BclA and C1q on complement activation and opsonophagocytosis of B. anthracis spores. The results reveal a novel mechanism of complement manipulation by B. anthracis spores. The importance of these findings to B. anthracis pathogenesis, host defense, and microbial manipulation of complement in general is discussed.
Materials and Methods
Bacteria and preparation of spores. B. anthracis
Sterne strain 7702 (39) and its isogenic BclA deletion mutant (ΔbclA, provided by C. Turnbough, University of Alabama at Birmingham, AL) (40) were used. Spores were prepared from these strains as previously described (39). Briefly, B. anthracis was cultured in PA media at 30°C with shaking for 7 – 10 days and centrifuged. The pellet was suspended in sterile H2O, heated at 68°C for 1 hour and washed thoroughly with sterile H2O. The suspension was then filtered through a 3.0 μM filter, titered and stored at 4°C.
Macrophage cell line and isolation of primary macrophages from mice
The murine macrophage-like cell line RAW264.7 was obtained from ATCC and cultured in Dulbecco’s modified eagle medium supplemented with 10% fetal bovine serum (DMEM/10%FBS) (Invitrogen).
C57BL/6 and CD11b−/− mice in the C57BL/6 background were initially obtained from The Jackson Laboratories and maintained at the animal facility at Texas A&M Health Science Center, Institute of Biosciences and Technology (IBT). To obtain primary peritoneal macrophages (PMs), the peritoneal cavities of mice were lavaged with 10 ml cold RPMI 1640 media. Cells from the lavage fluid were plated at 1 × 106 cells per well in 24-well tissue culture plates or on coverslips in 24-well tissue culture plates in RPMI 1640 supplemented with 10% heat-inactivated FBS. The cells were incubated for 2 hours at 37°C in a humidified incubator with 5% CO2 and then washed and fresh media added. Adherent cells were used in the experiments. Immunofluorescence staining confirmed that > 90% of the cells were CD11b positive. To obtain bone marrow derived macrophages (BMDMs), bone marrow was collected from the femur of mice. Bone marrow cells were cultured in RPMI 1640 supplemented with 10% heat-inactivated FBS and 10 ng/ml mouse GM-CSF (GIBCO) for 8 days. Immunofluorescence staining showed that > 90% of the cells at the end of 8-day incubation were CD11b positive. Cells were then seeded at 1 × 106 cells/well in 24-well tissue culture plates or on coverslips in 24-well tissue culture plates, incubated for 24 hours and used in the experiments. All the animal procedures followed protocols approved by the Institutional Animal Care and Use Committee at IBT.
Spore adherence and phagocytosis assays
This was done using an immunofluorescence and microscopic method as previously described (41) with slight modifications. The assays were performed in Hanks Balanced Salt Solution (serum free media, SFM) or SFM supplemented with 10% normal human serum (NHS), heat-inactivated NHS (HIS), C1q-depleted human serum (C1qD), C3 depleted serum (C3D) or purified complement components at indicated concentrations. All sera and complement components were purchased from Complement Technology, Inc.. Spores were incubated with macrophages at a multiplicity of infection (MOI) of ~ 10, unless otherwise stated, for 30 minutes at 37°C in a humidified incubator with 5% CO2. To inhibit spore germination, D-alanine, a known germination inhibitor, was included in the assay media at a final concentration of 2.5 mM. Cells were then washed, fixed with 2% paraformaldehye without permeabilization, blocked and incubated with rabbit anti-spore antibodies raised against formalin-killed 7702 or ΔbclA spores (1:500 dilution) (Strategic Biosolutions), followed by goat anti-rabbit secondary antibodies conjugated to Alexa-Fluor 594 (1:1000, Invitrogen) to detect extracellular spores. Cells were then permeabilized with 0.1% saponin and incubated with anti-spore antibodies followed by secondary antibodies conjugated to Alexa-Fluor 488 (1:1000, Invitrogen) to detect both intracellular and extracellular spores. The coverslips were then mounted and examined using a Zeiss LSM 510 laser-scanning confocal microscope. On average, approximately 1000 macrophages were counted for each experimental condition. The numbers of intracellular and extracellular adhered spores per macrophage, respectively, were calculated. In some cases, the number of associated spores (intracellular plus extracellular adhered spores) per macrophage was calculated.
Depletion of immunoglobulin G (IgG) from serum
IgG was depleted from NHS by passing NHS through protein G HP SpinTrap columns (GE healthcare) following the manufacturer’s instructions. The procedure was repeated until IgG depletion was confirmed by SDS-PAGE and western blot analysis using anti-human IgG antibodies.
Expression and purification of recombinant BclA (rBclA)
This was done as previously described (38) with slight modifications. Briefly, full-length BclA protein with an N-terminal His tag was expressed in E. coli BL21 Rosetta 2 strain (Novagen). The recombinant protein was purified using Ni++ affinity chromatography and ion-exchange chromatography in an AKTA prime plus FPLC system (GE Healthcare). The purified protein was analyzed by SDS-PAGE and circular dichroism to evaluate the purity and the proper folding of the recombinant protein, as previously described (38).
Binding of C1q to spores
Spores (2.5×107 or 5×107) were incubated in SFM containing purified human C1q (1 μg/ml), at 37°C for 10 minutes in the presence of 2.5 mM D-alanine. The spores were then washed with SFM three times and resuspended in PBS. An aliquot of the spore suspension was dilution plated on LB agar plates to determine the spore titer in each sample. The rest of the suspension was boiled in a reducing SDS sample buffer for 10 minutes and stored at −20°C until ready to be analyzed by SDS-PAGE and western blot. The volume of each sample loaded onto the SDS gels was adjusted so that samples of the same experimental conditions contain the same number of spores. Goat anti-C1q antibodies (1:5000, Complement Technology) and horseradish peroxidase (HRP)-conjugated rabbit anti-goat secondary antibodies (1:10000, Invitrogen) were used in western blot analysis. The intensity of the bands was determined by densitometry using Image J.
To determine if soluble rBclA protein could inhibit C1q binding to spores, C1q (1 μg/ml) was pre-incubated with various concentrations of rBclA at 4°C for 60 minutes before adding to the spores.
Deposition of C3 and C4 fragments on spores
This was done according to a procedure described previously (23) with some modifications. To detect C3 fragments, spores (~ 2×107) were incubated in SFM containing different types of serum (10%) with or without 10 mM EGTA at 37°C for 30 minutes. Spores were then washed three times with SFM, boiled in a reducing SDS sample buffer and applied to SDS-PAGE and western blot analysis using goat anti-C3 polyclonal antibodies (1:5000, Complement Technology) and appropriate secondary antibodies. Purified C3, C3b and iC3b (Complement Technology) were also included in the SDS-PAGE as standards for the different C3 fragments. To detect C4 fragments, spores (2.5×107 or 5×107) were incubated in SFM containing 10% NHS for 10 minutes. Spores were washed and analyzed by western blot using anti-C4 antibodies (CompTech, 1:5000). The intensity of the bands was determined by densitometry using Image J.
Enzyme-linked immunosorbent assay (ELISA)
This was carried out as previously described (38) with slight modifications. Briefly, purified C1q or ovalbumin were coated onto the wells of 96-well plates, blocked and incubated with HBS (10 mM HEPES, 150 mM NaCl, pH 7.4) containing various concentrations of rBclA with or without 10 mM EGTA or EDTA. Bound rBclA was detected with HRP-conjugated anti-His monoclonal antibodies. Apparent KD was calculated using the non-linear regression analysis method in the GraphPad Prism (version 4) program (GraphPad).
Macrophage viability assay
The viability of macrophages infected with spores was measured using a lactate dehydrogenase-based CytoTox-ONE™ Homogeneous Membrane Integrity Assay kit (Promega). RAW264.7 cells (2 × 105 cells/well) were infected with 7702 or ΔbclA spores in the presence of NHS or HIS as described above. After infection, cells were extensively washed and incubated in DMEM/10% FBS containing 5 mM L-alanine, which promotes spore germination, and 100 μg/ml gentamicin for 1hr to eliminate extracellular bacteria. We found that this treatment eliminated > 95% of extracellular spores and bacteria. The cells were then washed and incubated with DMEM/10%FBS containing 2.5mM D-alanine (to inhibit germination and growth of any residual extracellular spores) for 0, 6 or 24 hours. Culture supernatants were collected and LDH release measured by reading fluorescence at 560/590 nm according to the manufacture’s instructions.
Intracellular survival of spores
RAW264.7 cells (2 × 105 cells/well) were infected with 7702 or ΔbclA spores and incubated in DMEM/10% FBS containing 100 μg/ml gentamicin and 5 mM L-alanine for 1 hr as described above. To examine spore intracellular survival, cells were washed and incubated in DMEM/10%FBS containing 100 μg/ml gentamicin for 0, 1, 3, 6, or 24 hours. The cells were washed, lysed and dilution plated to determine the number of viable bacteria.
C1 and C4 activation assays
For C1 activation, recombinant BclA protein (rBclA, 26 μM), heat-denatured rBclA (hrBclA, 26 μM, heated at 50°C for 30 minutes), IgM (10 μg/ml) or buffer only were pre-incubated with HBS containing C1 complex (CompTech, 0.2 μg/μl, 1:10 dilution) for 60 minutes at 4°C followed by incubation at 37°C for 30 minutes in the presence of 0.5 mM Ca2+. For C4 activation, the respective proteins were incubated with HBS containing NHS (1% v/v). The samples were applied to 12% SDS-PAGE gel eletrophoresis and analyzed by western blot using sheep anti-C1s antibody (R&D, 1:5000), or anti-C4 antibody (Comptech, 1:5000) followed by appropriate secondary antibodies.
Statistical analyses
For pairwise comparisons, statistical analysis was performed using Student’s t test. For comparison between multiple groups, ANOVA was used. The GraphPad Prism program was used for the these analyses.
Results
Heat-labile serum factors are important for B. anthracis spore adherence to and phagocytosis by macrophages
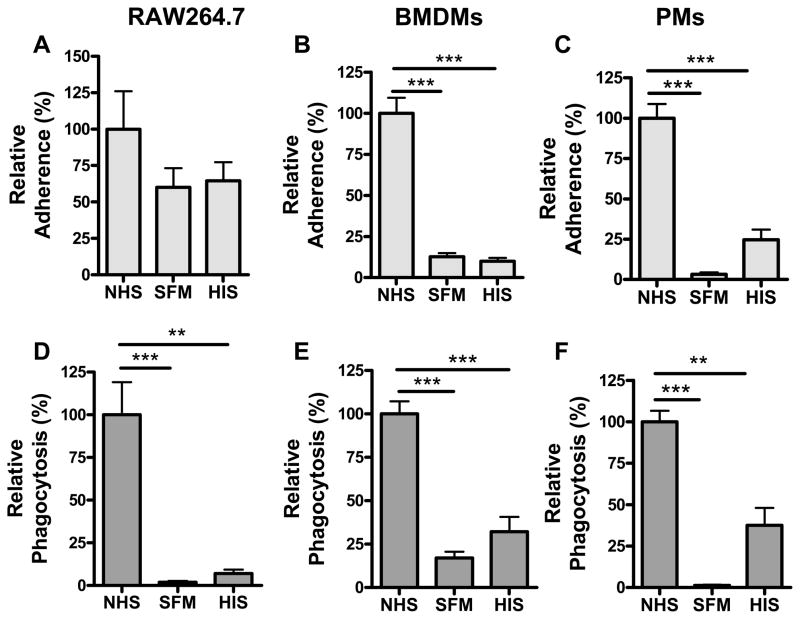
To investigate the role of complement in spore interaction with phagocytes, we first compared spore adherence to and uptake by macrophage cell line RAW264.7 and primary macrophages in SFM, SFM supplemented with 10% NHS or 10% HIS. Compared to adherence in the presence of NHS, spore adherence to RAW264.7 cells in SFM or HIS was decreased, although the decrease was statistically insignificant (Fig. 1, A). The effect of serum on spore adherence was more pronounced in BMDMs (Fig. 1, B) and PMs (Fig. 1, C). Spore adherence to BMDMs and PMs was increased by ~ 8 – 9 and ~ 20 fold, respectively in the presence of NHS compared to that in SFM (p < 0.001). The increase was primarily mediated by heat-labile factors in the serum (Fig. 1, B and C).
Figure 1. Phagocytosis of B. anthracis spores by macrophages requires heat-labile serum factors.
Phagocytosis assays were performed as described in the Materials and Methods section. Briefly, RAW264.7 (A and D), BMDMs (B and E) and PMs (C and F) were seeded onto coverslips in 24-well tissue culture plates and incubated with spores from the Sterne strain 7702 for 30 minutes in SFM, SFM supplemented with 10% normal human serum (NHS) or 10% heat-inactivated serum (HIS). The germination inhibitor D-alanine (2.5 mM) was included in the assays. Extracellular spores were detected by staining unpermeabilized cells with anti-spore antibodies. The cells were then permeabilized and stained again with anti-spore antibodies to detect intracellular spores. Relative adherence (A – C) is the ratio of the number of extracellular adhered spores vs. the number of macrophages examined, normalized to that in NHS. Relative phagocytosis (D – F) is the ratio of the number of intracellular spores vs. the number of macrophages examined, normalized to that in NHS. Results were combined from two to four independent experiments. The actual numbers of spore adherence and phagocytosis are 0.38 ± 0.10 and 0.96 ± 0.18 spores per RAW264.7 cell; 1.75 ± 0.39 and 1.86 ± 0.16 spores per BMDM; 3.33 ± 1.33 and 3.56 ± 1.48 spores per PM, respectively. Approximately 1000 macrophages were analyzed for each condition in each independent experiment. **, p < 0.01; ***, p < 0.001; Student’s t test.
Spore uptake by macrophages was similarly affected by heat-labile serum factors. Compared to that in NHS, phagocytosis was significantly reduced in SFM or HIS, with the sharpest reduction seen in RAW264.7 cells (Fig. 1, D – F).
Spore adherence and phagocytosis was also examined when macrophages were incubated with spores at different MOIs (1, 10 and 100). The effects of serum factors on adherence and phagocytosis were similar at the different MOIs (supplemental Fig. S1). However, the difference in phagocytosis between NHS and SFM or HIS was smaller at an MOI of 100 than those at the lower MOIs, which may suggest that the high MOI is getting close to a saturating dose. For the rest the study, all the phagocytosis and adherence experiments reported were conducted with an MOI of ~ 10.
Taken together, these results suggest that heat-labile serum factors, possibly the complement system, play a major role in spore adherence to and uptake by macrophages.
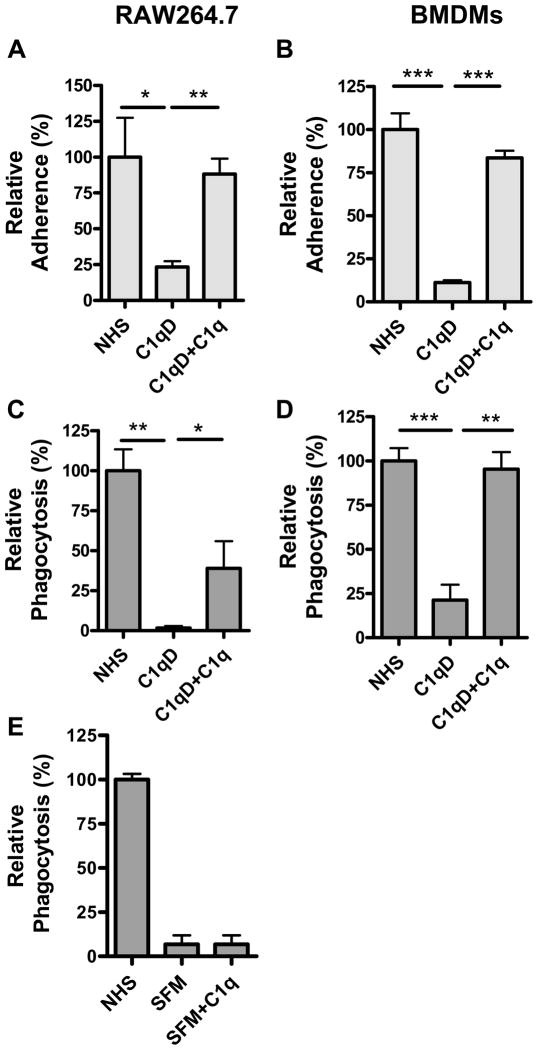
Phagocytosis of spores by macrophages is mediated by the classical complement pathway (CCP) in an IgG-independent manner
To investigate the role of C1q in spore interaction with macrophages, spore adherence and phagocytosis assays were performed in SFM supplemented with 10% C1q depleted serum (C1qD). We observed an approximately 80 – 90% reduction in spore adherence to RAW264.7 macrophages and BMDMs in C1qD compared to that in NHS (Fig. 2, A and B). Addition of purified C1q to C1qD restored spore adherence to these macrophages. Spore uptake by RAW264.7 macrophages and BMDMs in C1qD was also significantly reduced (by ~ 98% and ~ 80%, respectively) compared to that in NHS (p < 0.01 for RAW264.7 and p < 0.001 for BMDMs) (Fig. 2, C and D). Addition of purified C1q to C1qD significantly increased the uptake by RAW264.7 macrophages compared to that in C1qD (Fig. 2, C) and almost restored the uptake by BMDMs to the level seen in NHS (Fig. 2, D). Taken together, these data suggest that C1q plays a major role in spore adherence to and uptake by macrophages.
Figure 2. Phagocytosis of B. anthracis spores requires complement component C1q.
Phagocytosis assays and detection of extracellular and intracellular spores are as described in the legend for Figure 1, except that SFM was supplemented with different types of serum or C1q. The concentration for NHS and C1q depleted serum (C1qD) was 10% and for purified C1q was 10 μg/ml. A and B, relative adherence to RAW264.7 macrophages (A) and BMDMs (B). C – E, relative phagocytosis by RAW264.7 macrophages (C and E) and BMDMs (D). The results were combined from at least three independent experiments. Approximately 1000 macrophages were analyzed for each condition in each independent experiment. *, p < 0.05; **, p < 0.01; ***, p < 0.001; Student’s t test.
C1q may be important in spore phagocytosis by macrophage via two possible mechanisms. One is by activation of CCP, resulting in deposition of C3 fragments on spore surfaces and phagocytosis via C3 receptors. The other is by directly interacting with C1q receptors on macrophages and mediating phagocytosis in a complement activation-independent manner (42, 43), as reported for Listeria monocytogenes (44) and apoptotic cells (45). We investigated if C1q-mediated phagocytosis of spores required complement activation. Purified C1q was added to SFM in the absence of other complement components. The results showed that C1q alone did not increase spore uptake by macrophages compared to that in SFM (Fig. 2, E).
To further determine if complement activation is required for spore uptake, we performed phagocytosis assays in SFM supplemented with C3 depleted serum (C3D). Depletion of C3 almost abolished spore uptake by RAW264.7 macrophages (Fig. 3, A), BMDMs (Fig. 3, B) and PMs (Fig. 3, C). The total number of spores associated with macrophages (intracellular + extracellular adhered spores) was also significantly reduced in C3D compared to those in NHS (Fig. 3, D – F). These results indicate that C3 is important for both spore adherence to and uptake by macrophages.
Figure 3. Phagocytosis of spores requires complement component C3 but not IgG.
Phagocytosis assays and detection of extracellular and intracellular spores are as described in the legend for Figure 1, except that SFM was supplemented with 10% NHS, 10% C3 depleted serum (C3D) or 10% NHS depleted of IgG (IgG-D). Relative phagocytosis (A – C and G) is the ratio of the number of intracellular spores vs. the number of macrophages examined, normalized to that in NHS. Relative association (D – F and H) is the ratio of total extracellular adhered and intracellular spores vs. the number of macrophages examined, normalized to that in NHS. A, D G and H, RAW264.7 macrophages; B and E, BMDMs; C and F, PMs. The results were combined from two to four independent experiments. Approximately 1000 cells were analyzed for each condition in each independent experiment. **, p < 0.01; ***, p < 0.001; Student’s t test.
The most common way to activate CCP is by binding of C1q to antibodies in immune complexes. To investigate the possibility that CCP might be activated by IgG in human serum that bound to the spores non-specifically, we depleted IgG from NHS. IgG depletion was confirmed by SDS-PAGE and western blot analysis of the depleted serum (IgG-D) (supplemental Fig. S2, A and B). Results from phagocytosis assays showed that IgG depletion did not reduce spore phagocytosis by RAW264.7 macrophages (Fig. 3, G) or spore association to macrophages (Fig. 3, H), but rather a modest increase in phagocytosis was observed (Fig. 3, G), suggesting that IgG is not required for the spore phagocytosis process.
Taken together, the above results indicate that phagocytosis of spores by macrophages is dependent on C1q and C3, and independent of IgG. The results also suggest that IgG-independent activation of CCP is the primary mechanism for spore phagocytosis by macrophages.
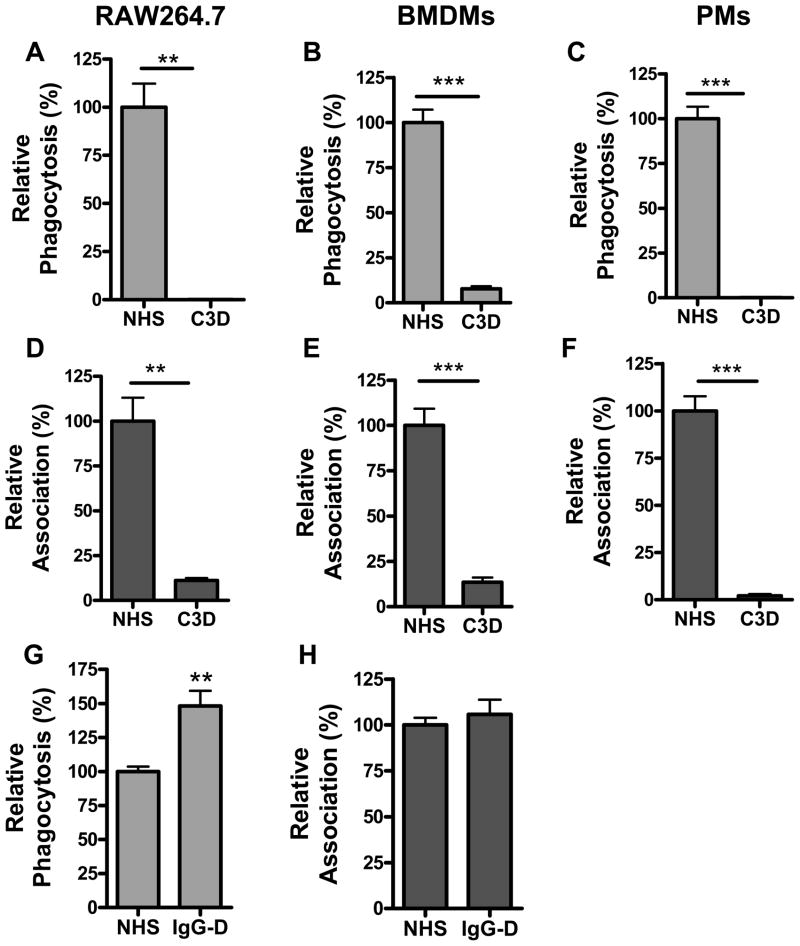
Spore surface protein BclA mediates the binding of C1q to the spore surface
Previously we showed that recombinant BclA (rBclA) bound C1q in a dose-dependent and saturable manner (38). BclA is the major protein on the surface of spores. We investigated if native BclA could mediate C1q binding to the spore surface. Spores from the Sterne strain 7702 and the isogenic BclA deletion mutant (ΔbclA) were incubated in buffer containing purified C1q. C1q bound on the spore surface was detected by western blot analysis using antibodies specific for C1q (Fig. 4, A) and quantified by densitometry (Fig. 4, B). The results showed that the presence of BclA on the spore surface significantly increased the amount of C1q bound to the spores (p < 0.05). Small amounts of C1q could still be detected on the ΔbclA spores, suggesting that there is a minor, BclA-independent secondary mechanism of C1q binding. We further examined if soluble rBclA could block C1q binding to spores. Purified C1q was pre-incubated with increasing concentrations of rBclA or BSA before the addition to 7702 or ΔbclA spores. The results showed that C1q binding to 7702 spores was specifically inhibited by rBclA in a dose-dependent manner (Fig. 4, C and D). As expected, rBclA had no effect on C1q binding to ΔbclA spores.
Figure 4. Spore surface protein BclA mediates C1q binding to spores.
A. 2.5×107 or 5×107 spores from the Sterne strain 7702 and its isogenic mutant bclA, respectively, were incubated with 1 μg/ml purified C1q at 37°C for 10 minutes. C1q binding to spores was determined by western blot as described in the Materials and Methods section. B. Densitometry analysis of the C1q band using Image J. The top bands in the gel were analyzed. The results shown are the mean density ± standard error of the mean (SEM), combined from three independent experiments and normalized to that of 7702 (2.5×107 spores). C and D, recombinant BclA (rBclA) inhibited C1q binding to 7702 spores but not to ΔbclA spore in a dose-dependent manner. Purified C1q was pre-incubated with different concentrations of rBclA or BSA at 4°C for 1 hour prior to incubation with the spores. The samples were analyzed by western blot (C) and quantified using Image J (D). The relative intensities in panel D were combined from three independent experiments. *, p < 0.05; Student’s t test. E, the effect of EGTA and EDTA on rBclA binding to C1q. ELISAs were performed as described in the Materials and Methods section. Non-linear regression analysis was used to calculate the apparent binding affinity (GraphPad Prism).
Ca2+ has been reported to be involved in C1q recognition of ligands such as IgG, IgM, C-reactive protein, pentraxin (46) and gp41 (47), possibly by enhancing the electrostatic stability of the binding interaction. We examined the effect of EGTA and EDTA on C1q binding to rBclA. The results showed that EGTA did not affect the binding compared to that in HBS only whereas EDTA reduced the binding by ~ 9 fold (Fig. 4, E). This suggests that divalent metal ions other than Ca2+ facilitate rBclA binding to C1q.
Taken together, these results demonstrate that BclA binds directly to C1q and is able to recruit C1q to the spore surface.
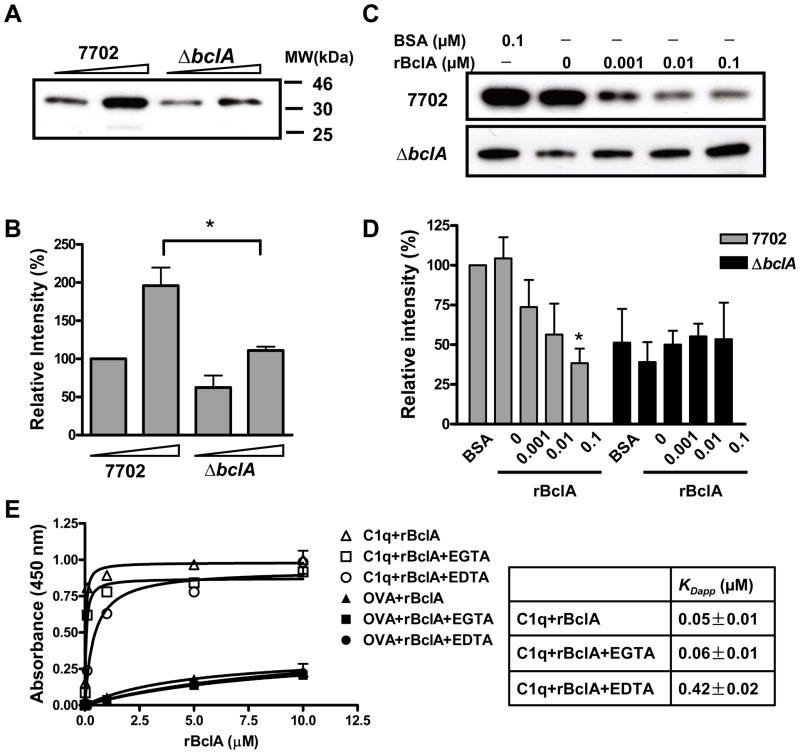
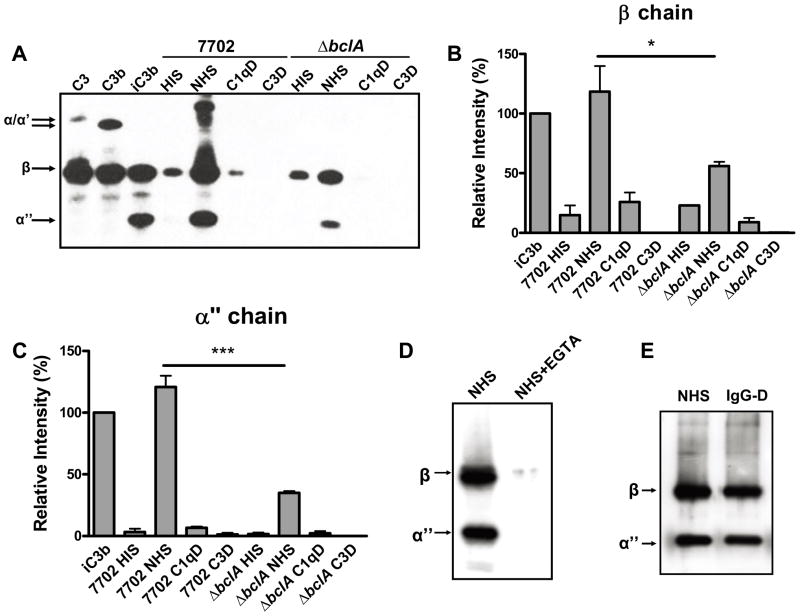
Deposition of C3 on the spore surface is initiated via IgG-independent activation of CCP and is significantly promoted by the presence of BclA
We investigated the deposition of C3 fragments on the surface of 7702 and ΔbclA spores. When 7702 spores were incubated in NHS containing media, C3 fragments were detected on the spore surface (Fig. 5, A). Judging by the presence of the truncated α chain (α″), which is indicative of iC3b, and the intensity of the α″ chain relative to the β chain, which represents total C3 fragments, iC3b is the dominant C3 fragment on the spore surface. The identities of the high molecular weight species were unclear. Upon activation, the thiol-ester bond in C3 is exposed allowing covalent anchorage of C3b as well as its subsequent cleavage fragments to nearby molecules. It is possible that some of the high molecular weight species represent complexes between C3 fragments and spore surface components. It is also possible that some of them were the α chain of C3b. A small amount of C3 β chain was detected on 7702 spores incubated in media containing HIS and was likely due to non-specific association of C3 to spores (Fig. 5, A – C). The amount of C3 deposited on 7702 spores after incubation in C1qD was similar to the background level observed in HIS (Fig. 5, A and B), suggesting that C3 deposition on spore surfaces was mediated by CCP. Nothing was detected when spores were incubated in C3D, indicating that the C3 antibodies were specific. C3 deposition was also examined in the presence of EGTA (Fig. 5, D), which disrupts the activation of CCP but not the alternative complement pathway (ACP). The results showed that EGTA abolished the deposition of C3 fragments on the surface of 7702 spores, further confirming that C3 deposition on the spores was initiated via CCP and not ACP.
Figure 5. C3 deposition on the spore surface is dependent on activation of CCP, promoted by BclA and independent of IgG.
A and B, C3 deposition is dependent on C1q and promoted by BclA. 7702 and ΔbclA spores were incubated with 10% HIS, NHS, C1qD or C3D at 37°C for 30 minutes. C3 deposition on the spore surface was examined by western blot analysis using C3-antibodies (A) as described in Materials and Methods. Purified C3, C3b and iC3b were loaded as protein standards. Different chains of C3/C3b/iC3b were indicated with arrows. The intensity of the β chain (B) and the iC3b α″ chain (C) was determined using Image J and normalized to those in the iC3b standard. The results shown are the mean density ± SEM combined from three independent experiments. *, p < 0.05; ***, p < 0.001 (7702 NHS vs.Δ bclA NHS); Student’s t test. D, C3 deposition is dependent on Ca2+. 7702 spores were incubated in 10% NHS with or without 10 mM EGTA and C3 deposition was examined by western blot analysis. E, C3 deposition is independent of IgG. 7702 spores were incubated in 10% NHS or 10% IgG-D and C3 deposition was examined by western blot.
To determine if CCP activation is initiated by C1q recognition of immune complexes, we examined C3 deposition on 7702 spores in media containing IgG depleted serum. IgG depletion did not affect C3 deposition on 7702 spores (Fig. 5, E), indicating that IgG is not involved in the initiation of CCP activation on the spore surface. These results are in agreement with the phagocytosis results described earlier (Fig. 3, G and H).
To determine the role of BclA, C3 deposition on ΔbclA spores was examined. The amount of both total C3 fragments (represented by the β chain) and iC3b deposited on the surface of ΔbclA spores after incubation in media containing NHS was significantly reduced compared to those on the parent 7702 spores (Fig. 5, A – C), indicating that the presence of BclA significantly promoted C3 deposition on the spore surface. There was a small amount of C3 fragments on ΔbclA spores that was significantly higher than the background level observed in media containing HIS (p < 0.01, t test) and appeared to involve C1q as well, suggesting that there may be a minor secondary mechanism of CCP activation by spores in the absence of BclA. This is in agreement with the C1q recruitment result described earlier in Fig. 4.
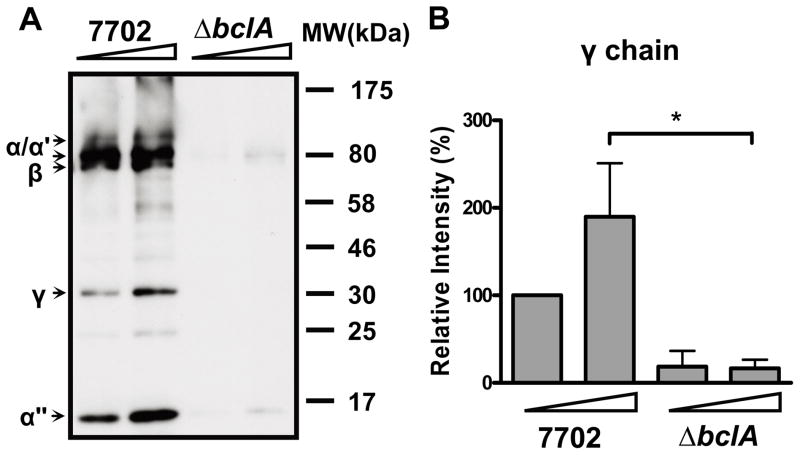
To further determine the role of BclA in CCP activation, C4 deposition on the surface of 7702 and ΔbclA spores was examined. C4 is downstream of C1 in the CCP. The results showed that C4 deposition on 7702 spores was significantly greater than that on ΔbclA spores (Fig. 6, A and B), suggesting that the presence of BclA is important for CCP activation on the surface of spores.
Fig. 6. C4 deposition on the spore surface.
A. 7702 and ΔbclA spores (2.5×107 and 5×107 spores, respectively) were incubated with 10% NHS at 37°C for 10 minutes. C4 deposition on spores was determined by western blot analysis using anti-C4 antibodies and secondary antibodies. Cleaved fragments of C4/C4b were indicated by arrows; the 94-kD α chain; the 84-kD α′ chain; the 75-kD β chain; the 32-kD γ chain; and the 14-kD α″ chain. B. Densitometry analysis of the C4b γ chain using Image J. The results shown are the mean density ± SEM, combined from three independent experiments and normalized to that of 7702 (2.5×107 spores). *, p < 0.05, Student’s t test.
We then investigated if recombinant BclA alone could directly activate CCP. Upon activation, C1q undergoes conformational changes that lead to cleavage of C1r and C1s. Thus, rBclA protein, IgM, heat-inactivated rBclA (hrBclA) or buffer only (HBS) was incubated with purified C1 complex and the samples were analyzed by western blot using anti-C1s antibodies. Cleavage of C1s was greatly enhanced in the presence of IgM, however, there was no significant difference in C1s cleavage between rBclA, hrBclA and buffer only (supplemental Fig. S3). We further examined the cleavage of C4 by incubating rBclA, hrBclA or IgM with NHS. The samples were analyzed with western blot using anti-C4 antibodies. We did not observe any significant difference in C4 cleavage between rBclA, hrBclA and buffer only, whereas IgM induced C4 cleavage (data not shown). These results suggest that rBclA alone is insufficient to activate CCP. Activation of CCP requires either other additional molecules on the spore surface or post-translational modifications of BclA (e.g., glycosylation) that are absent in rBclA.
Taken together, our results suggest that deposition of C3 fragments on the spore surface is initiated by CCP activation in an IgG-independent manner and is significantly promoted by the presence of BclA.
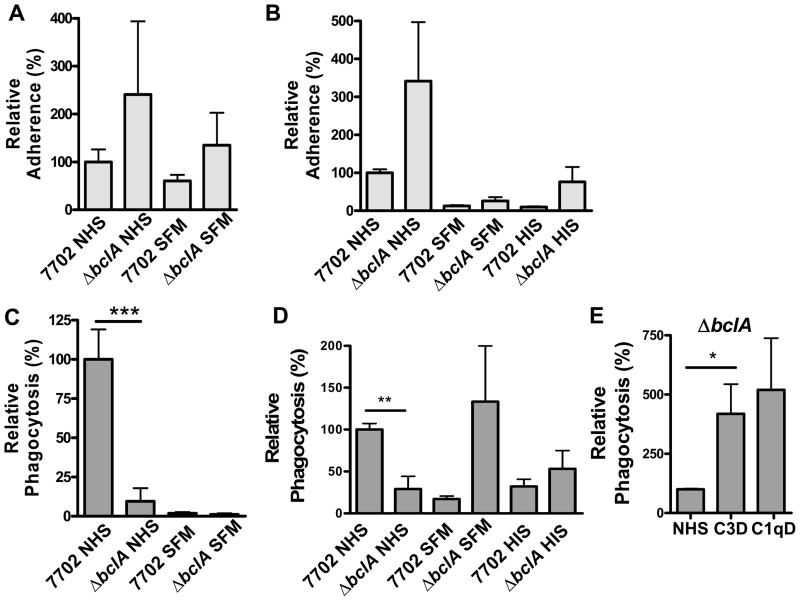
BclA mediates spore phagocytosis by macrophages in a C1q- and C3-dependent manner
We investigated the role of BclA in spore adherence to macrophages and in CCP-mediated phagocytosis of spores. For spore adherence, ΔbclA spores appeared to adhere to both RAW264.7 (Fig. 7, A) and BMDMs (Fig. 7, B) as least as well as or better than (although statistically insignificant) 7702 spores regardless of the media. These results suggest that in the absence of BclA, other spore surface components can also mediate adherence to macrophages.
Figure 7. BclA is required for complement-mediated phagocytosis of spores.
Relative adherence (A and B) and relative phagocytosis (C – E) are as described in the legend for Figure 1. Results were combined from three independent experiments. Approximately 1000 macrophages were analyzed for each condition in each independent experiment. A and C, RAW264.7; B, D and E, BMDMs. *, p < 0.05; **, p < 0.01; ***, p < 0.001; Student’s t test.
For phagocytosis, we compared the uptake of 7702 and ΔbclA spores in SFM or SFM supplemented with NHS or HIS. In the presence of NHS, phagocytosis of ΔbclA spores was significantly lower than that of 7702 spores, i.e., ~ 90% lower (p < 0.001) in RAW264.7 cells (Fig. 7, C) and ~ 70% lower (p < 0.01) in BMDMs (Fig. 7, D). In contrast, in SFM or HIS, phagocytosis of ΔbclA spores was not significantly different compared to that of 7702 spores, suggesting that BclA’s function in the spore phagocytosis process was dependent on complement activities.
We further examined the effect of C1q and C3 depletion on phagocytosis of ΔbclA spores. Contrary to the C1q- and C3-dependent phagocytosis of wild type 7702 spores shown in figures 2 and 3, uptake of ΔbclA spores by macrophages was not reduced but instead was increased in C1qD and C3D compared to that in NHS (Fig. 7, E). Taken together, these results suggest that the effect of BclA on spore phagocytosis is dependent on C1q and activation of CCP. The results also suggest that in the absence of BclA and complement, a distinct mechanism of spore phagocytosis comes into action. The nature of this BclA- and CCP-independent mechanism is currently unknown.
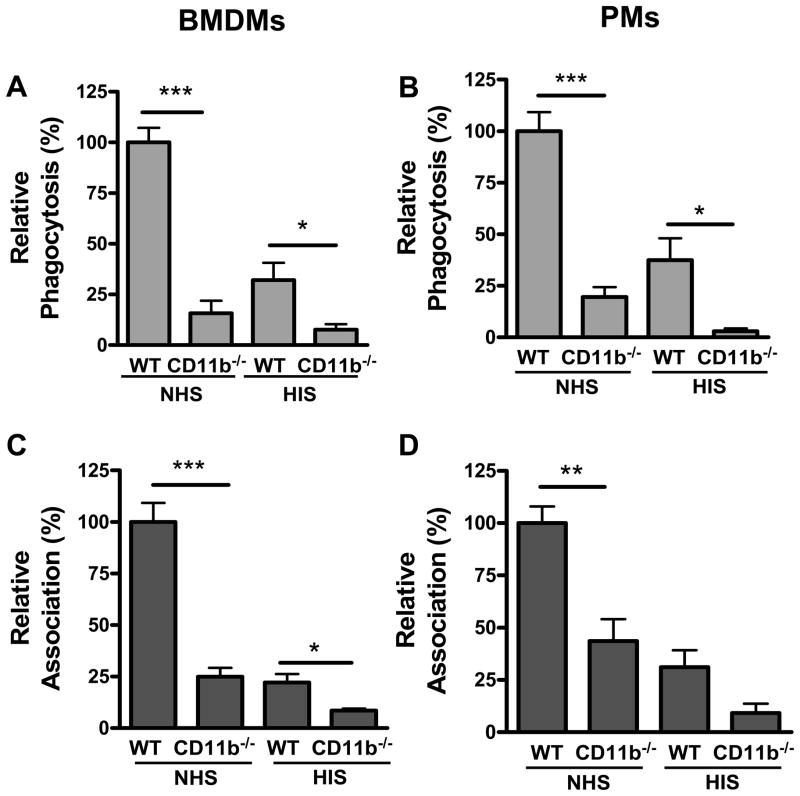
CR3 is the primary phagocytic receptor for spores in the presence of serum
CR3 is the phagocytic receptor for iC3b on macrophages. To determine if CR3 is the receptor in the BclA/CCP-mediated phagocytic pathway, we examined spore uptake by BMDMs and PMs isolated from CD11b−/− mice. The results showed that in the presence of NHS, phagocytosis of 7702 spores by CD11b−/− BMDMs and PMs was significantly reduced compared to that by wild type (WT) macrophages (Fig. 8, A and B). The total number of spores associated with CD11b−/− BMDMs and PMs (extracellular adhered and intracellular spores) was also significantly lower compared to that with WT macrophages (Fig. 8, C and D). These results indicate that in the presence of complement, CR3 is the primary macrophage phagocytic receptor for spores. In the presence of HIS, phagocytosis of 7702 spores by CD11b−/− macrophages was also lower than that by WT macrophages (Fig. 8, A – D), suggesting that CR3 is also involved in spore uptake by macrophages in the absence of complement. This latter result is consistent with the previous data by Oliva et al. (29).
Figure 8. CR3 is the major phagocytic receptor for spores in the presence of serum.
Phagocytosis assays were performed as described in the Materials and Methods section. Relative phagocytosis (A and B) is the ratio of the number of intracellular spores vs. the number of macrophages examined, normalized to that from WT macrophages in NHS. Relative association (C and D) is the ratio of total extracellular adhered and intracellular spores vs. the number of macrophages examined, normalized to that from WT macrophages in NHS. Results shown were combined from two to three independent experiments. Approximately 1000 macrophages were analyzed for each condition in each independent experiment. *, p < 0.05; **, p < 0.01; ***, p < 0.001; Student’s t test. A and C, BMDMs; B and D, PMs.
The effect of different phagocytic mechanisms on the intracellular fate of spores and the viability of macrophages
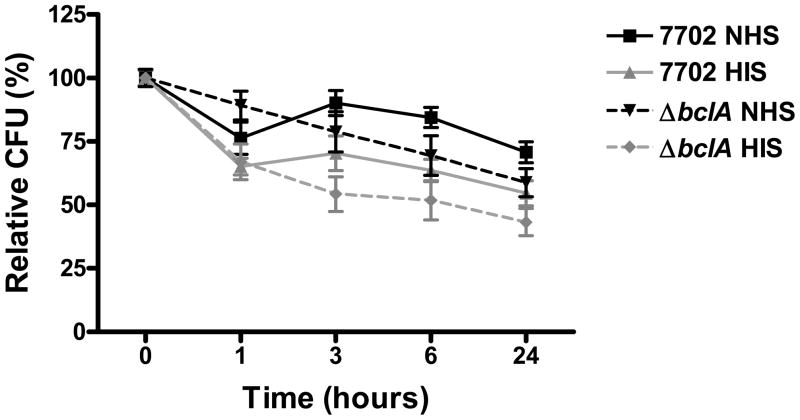
We investigated the survival of spores phagocytosed through different phagocytic pathways. 7702 and ΔbclA spores were phagocytosis by macrophages in the presence of NHS and HIS (complement opsonized vs. no complement opsonization) and intracellular survival was examined over a 24 hour time period. The results showed that 7702 spores phagocytosed in the presence of NHS survived better than that in the presence of HIS, however the difference was not statistically significant except at 6 hours post phagocytosis (p < 0.05, ANOVA) (Fig. 9). Similarly, ΔbclA spores phagocytosed in the presence of NHS survived better than those phagocytosed in the presence of HIS, however the difference was only statistically significant at 1 (p < 0.05) and 3 hours (p < 0.01) post phagocytosis. We observed no significant difference in the survival between the two types of spores either in the presence of NHS or in the presence of HIS. The biggest difference in survival was observed when comparison was made between 7702 spores phagocytosed in the presence of NHS (BclA-mediated and complement opsonized) and ΔbclA spores in the presence of HIS (non BclA-mediated and no complement opsonization) (p < 0.001 at 3 and 6 hrs, p < 0.01 at 24 hrs, ANOVA). Overall, spores phagocytosed via complement opsonization appeared to survive better than spores phagocytosed by other mechanisms.
Fig 9. Intracellular survival of spores phagocytosed by distinct phagocytic mechanisms.
RAW264.7 macrophages were infected with 7702 or ΔbclA spores in the presence of NHS or HIS as described in the Materials and Methods section. Recovered CFUs were normalized to those at time 0 of each condition. Results shown were combined from three independent experiments.
The effect of the different phagocytosis pathways on macrophage viability was also investigated by measuring lactate dehydrogenase activities in the cell culture media in a 24-hour time course. We did not observe any significant difference in macrophage viability when infected with the different spores in the presence of NHS or HIS (data not shown).
Discussions
The complement system is a critical aspect of host defense against microbes. Understanding the dynamic exchanges between pathogens and the complement system at a molecular level will provide important insights into microbial immune manipulation strategies and new possibilities to treat infectious diseases. Here we report that spores of B. anthracis are able to activate CCP to promote uptake by macrophages via opsonophagocytosis. CCP activation is independent of IgG and appears to be primarily initiated by recruitment of C1q to the spore surface via the spore surface protein BclA. This mechanism of complement manipulation is novel for B. anthracis. Complement activities are present in the blood as well as in the fluid lining the mucosal surfaces (1, 2, 48). Therefore the mechanism elucidated here likely takes place as soon as spores enter the host. In addition, spore entry into host cells is a critical event in the establishment of anthrax infections. Thus the mechanism should be relevant and important to understanding the pathogenic mechanisms of B. anthracis at early stages of infections.
That phagocytosis of spores is primarily mediated by activation of CCP is supported by the following results. Spore adherence to and phagocytosis by macrophages was significantly reduced in HIS, C1qD and C3D compared to that in NHS. Addition of purified C1q to C1qD restored spore adherence to and phagocytosis by macrophages; however, addition of C1q to SFM did not increase phagocytosis. Furthermore, C3 deposition on the spore surface was dependent on C1q and Ca2+.
That CCP activation is independent of IgG and is promoted by the spore surface protein BclA is supported by the following results. Neither C3 deposition on the spore surface nor spore phagocytosis was affected by IgG depletion from the serum; however, both were significantly reduced when BclA is absent from the spore surface. In addition, C4 deposition in the spore surface was significantly reduced in the absence of BclA. That BclA mediates C1q binding to spores is supported by the following evidence. Recombinant BclA bound purified C1q in a dose-dependent and saturable manner and inhibited C1q binding to wild type spores but not to ΔbclA spores. In addition, ΔbclA spores bound significantly less C1q than wild type spores.
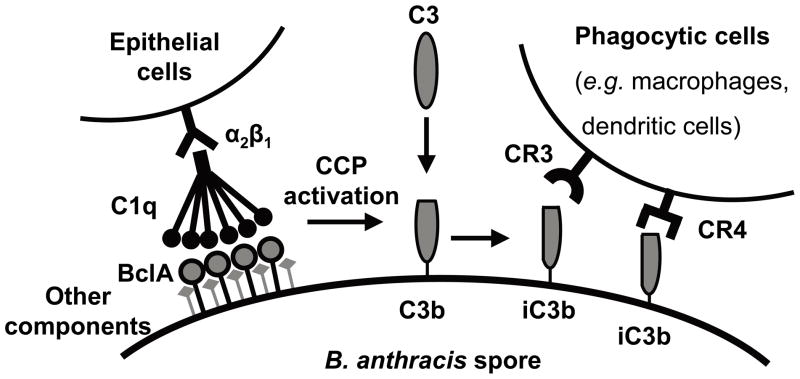
Based on these findings and previous reports, we propose a model in which wild type B. anthracis spores utilize a common initial step, i.e., BclA-C1q interaction, in the pathways to gain entry into different types of host cells (Fig. 10). In the presence of complement (which is the in vivo situation), spore surface protein BclA interacts with C1q. The interaction mediates spore entry into epithelial cells via integrin α2β1, as previously reported (38). The interaction also leads to activation of CCP (likely involving additional factors), resulting in deposition of C4 and C3 fragments on the spores. Our results show that iC3b is the dominant form of C3 fragments on the spore surface. Currently we do not know if the conversion of C3b to iC3b on the spore surface is a result of the normal cleavage process mediated by factor I and cofactors in the serum or spores actively recruit some of these factors to promote the cleavage. Preliminary data from our lab suggests a possibility of active recruitment, which is currently being investigated. In any case, the deposition results in spore phagocytosis via iC3b receptors such as CR3 on macrophages. We further propose that this mechanism should also function to mediate spore uptake by other iC3b receptors such as CR4 (also known as CD11c/CD18, αxβ2) on dendritic cells. When BclA is absent, there is significantly less C1q and C3 fragments on the spore surface and consequently less efficient spore entry into host cells compared to that of wild type spores. As spore entry into host macrophages, dendritic cells and epithelial cells is thought to be critical for spore dissemination and germination into vegetative bacilli, the model described here is likely to play a key role during the early stages of infections.
Figure 10. A working model of the mechanisms for B. anthracis spore entry into host cells.
Spore surface protein BclA binds to complement component C1q. This leads to spore entry into epithelial cells via integrin α2β1 (38). BclA and C1q interaction also leads to activation of CCP, resulting in C3b deposition on the spore surface. C3b is further cleaved into iC3b. Recognition of C3 fragments by CR3 and CR4 results in phagocytosis of spores by phagocytes such as macrophages and dendritic cells.
The outer membrane proteins and lipopolysaccharides (LPS) of a number of gram-negative bacteria (49–57) and the capsular polysaccharide of group B streptococci (58–60) have been reported to bind C1q and activate CCP in an antibody-independent manner. In these cases, the activation leads to increased susceptibility of the bacteria to killing by complement or phagocytes. We did not find any decrease in spore viability after the spores (both WT and ΔbclA spores) had been incubated in normal human serum (data not shown), indicating that activation of CCP does not lead to increased serum susceptibility of spores. This is consistent with the knowledge that spores are generally ‘resilient’ and that spores are enclosed by an exosporium composed of proteins and glycoproteins instead of a lipid bilayer. Therefore the mechanism described here primarily functions to promote spore entry into host phagocytes.
The intracellular fate of phagocytosed spores has been studied by multiple groups. Following phagocytosis spores are trafficked to phagolysosomes as evidenced by colocalization of spores with lysosome-associated membrane protein 1 (LAMP1) (61). There was evidence suggesting that spores germinate in the phagolysosomes and eventually escape from macrophages (62–64). Intracellular germination appears to be important for the escape and is a complex process requiring multiple and diverse genetic loci. These loci include several germination operons as well as intergenic regions with unknown functions (37, 65–67). The anthrax toxins seemed to play a role in escaping from macrophages (63, 64). In addition, B. anthracis encodes several proteases, anthrolysin O and phospholipases that could be important for escaping from phagosomal vesicles and macrophages (68–73). We investigated the effect of different phagocytic mechanisms on B. anthracis intracellular survival and found that BclA-mediated complement opsonization of spores lead to significantly improved intracellular survival compared to non-BclA mediated, no complement opsonized spore phagocytosis. It is possible that distinct phagocytic mechanisms can affect the intracellular trafficking pathway as well as the kinetics of trafficking. These differences can potentially influence the viability of spores, the rate of spore germination, the survival of germinated spores and the expression of factors involved in intracellular survival and escape.
It was previously reported that compared to wild type mice, CR3 knockout mice were more resistant to infections by wild type spores. However, when mice were challenged with ΔbclA spores, the difference in survival between CR3 knockout and wild type mice became statistically insignificant (29). This combined with our finding that BclA-mediated complement opsonized spore phagocytosis leads to significantly better intracellular survival, suggest that the mechanism of spore phagocytosis described in this report is beneficial to the pathogen.
BclA is the major glycoprotein on the surface of B. anthracis spores. It contains a short N-terminal region followed by a collagen-like central domain (CLD) and a C-terminal globular domain (CTD) (40, 74). The CLD forms collagen-like tripe helices in solution as shown by its circular dichroism spectrum (40). The X-ray crystal structure of the BclA CTD resembles that of the globular head of C1q even though the primary amino acid sequences of the two proteins do not show significant homology to each other. This makes BclA similar to C1q in both domain organization and tertiary structure and thus a potential member of the C1q family (75). In addition, rBclA binding to C1q may involve a distinct mechanism from the previously characterized C1q ligands. Thus, BclA is a novel ligand for C1q. It will be interesting to elucidate the molecular details of BclA-C1q interaction, i.e., the region/motif in each protein responsible for binding and if or how the binding affects C1q recognition of immune complexes and association with C1r and C1s. Our data also indicate that rBclA is insufficient to activate CCP. The data on C1q binding to spores suggest that there is a secondary C1q binding site on the spores. It is possible that this additional site functions together with BclA in CCP activation. Alternatively, native BclA is glycosylated (76). It is possible that while the core protein mediates binding to C1q, some of the glycosyl moieties are important for CCP activation. Studies to elucidate the detailed mechanisms of C1q binding and CCP activation are currently underway in our laboratory.
BclA belongs to a family of recently reported bacterial surface proteins that contain collagen-like structures. Other members of the family are the group A streptococcal collagen-like proteins (Scls) (77, 78) and the pneumococcal collagen-like protein (PclA) (79). Scl1 was shown to mediate the internalization of group A streptococci by host cells via direct interactions with integrin α2β1 (80), and has the ability to bind low-density lipoprotein (81) and complement factor H and factor H related protein 1 (82). PclA was shown to promote the adherence and invasion of pneumococci to respiratory epithelial cells (79). Thus there seems to be an emerging theme that members of the bacterial collagen-like protein family are actively involved in interactions with host cells and components of the innate immune system.
The role of BclA in anthrax infections remains to be clarified. Studies using animal models of anthrax infections by different groups indicate that ΔbclA spores are either as virulent as (83) or more virulent than wild type spores (29). On the other hand, CR3 deficiency resulted in significantly less susceptibility of mice to anthrax infections (29), suggesting that entry into macrophages is important for B. anthracis pathogenesis. How to reconcile these observations is unclear. It is possible that the absence of BclA allows other spore surface components to be exposed and these components may interact with host factors that normally are not accessible to them in wild type spores. The observations that ΔbclA spores adhere to epithelial cells (38) and macrophages as well as or better than wild type spores and the increased uptake of ΔbclA spores by macrophages in the absence of C1q or C3 supports this possibility. Furthermore, our recent data indicates that BclA also interacts with additional host factors (unpublished). This complicates the interpretation of the in vivo results from studies using ΔbclA spores. More targeted mutations in BclA that only affects its C1q binding capability but not its targeting to the spore exosporium, the assembly of the exosporium, or its interactions with other host factors will be helpful in elucidating the role of BclA-C1q interaction in anthrax infections. It will also be interesting to examine the impact of C1q deficiency on the development and outcome of anthrax infections.
The role of complement in host defense against B. anthracis has not been investigated previously except for complement C5. Compared to wild type mice, mice deficient in C5 displayed increased susceptibility to B. anthracis infections (84). There was some evidence suggesting that this effect of C5 may be primarily through vegetative bacilli (85), as the increase in susceptibility appeared to be most apparent in infections caused by B. anthracis strains that were unable to produce the capsule, which is only present at the vegetative bacilli stage. These results underscore the idea that the interplays between B. anthracis and the complement system are complex. At different stages of infection, different complement components may have distinct functions and importance with respect to disease progression.
In conclusion, the results presented in the current report elucidate a novel mechanism of complement manipulation by spores of B. anthracis that is likely to be significant to the pathogenesis of this microorganism. In addition, as a novel ligand of C1q, investigations to elucidate the molecular mechanisms of BclA-C1q interaction, its effect on activation of C1 and the overall complement system will provide new insights into C1q-ligand interactions as well as microbial manipulation of complement.
Supplementary Material
Acknowledgments
We thank Mingsong Kang and Ya-Ping Ko, Texas A&M Health Science Center, Institute of Biosciences and Technology, Houston, TX, for providing reagents and technical advice and for careful reading of the manuscript. We thank Zhongcheng Shi, Baylor College of Medicine, Houston, TX, for help with isolating BMDMs and PMs.
Abbreviations used in this article
- CCP
classical complement pathway
- BclA
bacillus collagen-like protein of anthracis
- CR3
complement receptor 3
- BMDMs
bone marrow derived macrophages
- PMs
peritoneal macrophages
- NHS
normal human serum
- SFM
serum free medium
- C1qD
C1q depleted serum
- C3D
C3 depleted serum
- HIS
heat inactivated serum
- IgG-D
IgG depleted serum
- ACP
alternative complement pathway
- LDH
lactate dehydrogenase
- CFU
colony forming unit
Footnotes
This work was supported by NIH AI082306, funding from the Hamill foundation and start-up funds from the Texas A&M Health ScienceCenter to Yi Xu.
References
- 1.Walport MJ. Complement. Second of two parts. N Engl J Med. 2001;344:1140–1144. doi: 10.1056/NEJM200104123441506. [DOI] [PubMed] [Google Scholar]
- 2.Walport MJ. Complement. First of two parts. N Engl J Med. 2001;344:1058–1066. doi: 10.1056/NEJM200104053441406. [DOI] [PubMed] [Google Scholar]
- 3.Lambris JD, Ricklin D, Geisbrecht BV. Complement evasion by human pathogens. Nat Rev Microbiol. 2008;6:132–142. doi: 10.1038/nrmicro1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Granoff DM, Welsch JA, Ram S. Binding of complement factor H (fH) to Neisseria meningitidis is specific for human fH and inhibits complement activation by rat and rabbit sera. Infect Immun. 2009;77:764–769. doi: 10.1128/IAI.01191-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seib KL, Serruto D, Oriente F, Delany I, Adu-Bobie J, Veggi D, Arico B, Rappuoli R, Pizza M. Factor H-binding protein is important for meningococcal survival in human whole blood and serum and in the presence of the antimicrobial peptide LL-37. Infect Immun. 2009;77:292–299. doi: 10.1128/IAI.01071-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunphy KY, Beernink PT, Brogioni B, Granoff DM. Effect of factor H-binding protein sequence variation on factor H binding and survival of Neisseria meningitidis in human blood. Infect Immun. 2011;79:353–359. doi: 10.1128/IAI.00849-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Findlow J, Borrow R, Snape MD, Dawson T, Holland A, John TM, Evans A, Telford KL, Ypma E, Toneatto D, Oster P, Miller E, Pollard AJ. Multicenter, open-label, randomized phase II controlled trial of an investigational recombinant Meningococcal serogroup B vaccine with and without outer membrane vesicles, administered in infancy. Clin Infect Dis. 2010;51:1127–1137. doi: 10.1086/656741. [DOI] [PubMed] [Google Scholar]
- 8.Jiang HQ, Hoiseth SK, Harris SL, McNeil LK, Zhu D, Tan C, Scott AA, Alexander K, Mason K, Miller L, DaSilva I, Mack M, Zhao XJ, Pride MW, Andrew L, Murphy E, Hagen M, French R, Arora A, Jones TR, Jansen KU, Zlotnick GW, Anderson AS. Broad vaccine coverage predicted for a bivalent recombinant factor H binding protein based vaccine to prevent serogroup B meningococcal disease. Vaccine. 2010;28:6086–6093. doi: 10.1016/j.vaccine.2010.06.083. [DOI] [PubMed] [Google Scholar]
- 9.Keiser PB, Biggs-Cicatelli S, Moran EE, Schmiel DH, Pinto VB, Burden RE, Miller LB, Moon JE, Bowden RA, Cummings JF, Zollinger WD. A phase 1 study of a meningococcal native outer membrane vesicle vaccine made from a group B strain with deleted lpxL1 and synX, over-expressed factor H binding protein, two PorAs and stabilized OpcA expression. Vaccine. 2011;29:1413–1420. doi: 10.1016/j.vaccine.2010.12.039. [DOI] [PubMed] [Google Scholar]
- 10.Snape MD, Dawson T, Oster P, Evans A, John TM, Ohene-Kena B, Findlow J, Yu LM, Borrow R, Ypma E, Toneatto D, Pollard AJ. Immunogenicity of two investigational serogroup B meningococcal vaccines in the first year of life: a randomized comparative trial. Pediatr Infect Dis J. 2010;29:e71–79. doi: 10.1097/INF.0b013e3181f59f6d. [DOI] [PubMed] [Google Scholar]
- 11.Vu DM, Wong TT, Granoff DM. Cooperative serum bactericidal activity between human antibodies to meningococcal factor H binding protein and Neisserial heparin binding antigen. Vaccine. 2011;29:1968–1973. doi: 10.1016/j.vaccine.2010.12.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee LY, Liang X, Hook M, Brown EL. Identification and characterization of the C3 binding domain of the Staphylococcus aureus extracellular fibrinogen-binding protein (Efb) J Biol Chem. 2004;279:50710–50716. doi: 10.1074/jbc.M408570200. [DOI] [PubMed] [Google Scholar]
- 13.Lee LY, Hook M, Haviland D, Wetsel RA, Yonter EO, Syribeys P, Vernachio J, Brown EL. Inhibition of complement activation by a secreted Staphylococcus aureus protein. J Infect Dis. 2004;190:571–579. doi: 10.1086/422259. [DOI] [PubMed] [Google Scholar]
- 14.Langley R, Wines B, Willoughby N, Basu I, Proft T, Fraser JD. The staphylococcal superantigen-like protein 7 binds IgA and complement C5 and inhibits IgA-Fc alpha RI binding and serum killing of bacteria. J Immunol. 2005;174:2926–2933. doi: 10.4049/jimmunol.174.5.2926. [DOI] [PubMed] [Google Scholar]
- 15.Bestebroer J, Aerts PC, Rooijakkers SH, Pandey MK, Kohl J, van Strijp JA, de Haas CJ. Functional basis for complement evasion by staphylococcal superantigen-like 7. Cell Microbiol. 2010;12:1506–1516. doi: 10.1111/j.1462-5822.2010.01486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ricklin D, Tzekou A, Garcia BL, Hammel M, McWhorter WJ, Sfyroera G, Wu YQ, Holers VM, Herbert AP, Barlow PN, Geisbrecht BV, Lambris JD. A molecular insight into complement evasion by the staphylococcal complement inhibitor protein family. J Immunol. 2009;183:2565–2574. doi: 10.4049/jimmunol.0901443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia BL, Tzekou A, Ramyar KX, McWhorter WJ, Ricklin D, Lambris JD, Geisbrecht BV. Crystallization of human complement component C3b in the presence of a staphylococcal complement-inhibitor protein (SCIN) Acta Crystallogr Sect F Struct Biol Cryst Commun. 2009;65:482–485. doi: 10.1107/S174430910901207X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jongerius I, Puister M, Wu J, Ruyken M, van Strijp JA, Rooijakkers SH. Staphylococcal complement inhibitor modulates phagocyte responses by dimerization of convertases. J Immunol. 2010;184:420–425. doi: 10.4049/jimmunol.0902865. [DOI] [PubMed] [Google Scholar]
- 19.Rooijakkers SH, Wu J, Ruyken M, van Domselaar R, Planken KL, Tzekou A, Ricklin D, Lambris JD, Janssen BJ, van Strijp JA, Gros P. Structural and functional implications of the alternative complement pathway C3 convertase stabilized by a staphylococcal inhibitor. Nat Immunol. 2009;10:721–727. doi: 10.1038/ni.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rooijakkers SH, Milder FJ, Bardoel BW, Ruyken M, van Strijp JA, Gros P. Staphylococcal complement inhibitor: structure and active sites. J Immunol. 2007;179:2989–2998. doi: 10.4049/jimmunol.179.5.2989. [DOI] [PubMed] [Google Scholar]
- 21.van Wamel WJ, Rooijakkers SH, Ruyken M, van Kessel KP, van Strijp JA. The innate immune modulators staphylococcal complement inhibitor and chemotaxis inhibitory protein of Staphylococcus aureus are located on beta-hemolysin-converting bacteriophages. J Bacteriol. 2006;188:1310–1315. doi: 10.1128/JB.188.4.1310-1315.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carroll MV, Lack N, Sim E, Krarup A, Sim RB. Multiple routes of complement activation by Mycobacterium bovis BCG. Mol Immunol. 2009;46:3367–3378. doi: 10.1016/j.molimm.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 23.Ferguson JS, Weis JJ, Martin JL, Schlesinger LS. Complement protein C3 binding to Mycobacterium tuberculosis is initiated by the classical pathway in human bronchoalveolar lavage fluid. Infect Immun. 2004;72:2564–2573. doi: 10.1128/IAI.72.5.2564-2573.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramanathan VD, Curtis J, Turk JL. Activation of the alternative pathway of complement by mycobacteria and cord factor. Infect Immun. 1980;29:30–35. doi: 10.1128/iai.29.1.30-35.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kojouharova MS, I, Panchev D, Tchorbadjieva MI, Reid KB, Hoppe HJ. Differential binding of IgG and of a HIV gp41 peptide by the B chain and A chain globular head sequences of C1q, respectively. J Immunol. 1998;161:4325–4331. [PubMed] [Google Scholar]
- 26.Ebenbichler CF, Thielens NM, Vornhagen R, Marschang P, Arlaud GJ, Dierich MP. Human immunodeficiency virus type 1 activates the classical pathway of complement by direct C1 binding through specific sites in the transmembrane glycoproteingp41. J Exp Med. 1991;174:1417–1424. doi: 10.1084/jem.174.6.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guidi-Rontani C. The alveolar macrophage: the Trojan horse of Bacillus anthracis. Trends in Microbiology. 2002;10:405–409. doi: 10.1016/s0966-842x(02)02422-8. [DOI] [PubMed] [Google Scholar]
- 28.Oliva C, Turnbough CL, Jr, Kearney JF. CD14-Mac-1 interactions in Bacillus anthracis spore internalization by macrophages. Proc Natl Acad Sci U S A. 2009;106:13957–13962. doi: 10.1073/pnas.0902392106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oliva CR, Swiecki MK, Griguer CE, Lisanby MW, Bullard DC, Turnbough CL, Jr, Kearney JF. The integrin Mac-1 (CR3) mediates internalization and directs Bacillus anthracis spores into professional phagocytes. PNAS. 2008;105:1261–1266. doi: 10.1073/pnas.0709321105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cleret A, Quesnel-Hellmann A, Vallon-Eberhard A, Verrier B, Jung S, Vidal D, Mathieu J, Tournier JN. Lung dendritic cells rapidly mediate anthrax spore entry through the pulmonary route. J Immunol. 2007;178:7994–8001. doi: 10.4049/jimmunol.178.12.7994. [DOI] [PubMed] [Google Scholar]
- 31.Shetron-Rama LM, Herring-Palmer AC, Huffnagle GB, Hanna P. Transport of Bacillus anthracis from the lungs to the draining lymph nodes is a rapid process facilitated by CD11c+ cells. Microb Pathog. 2010;49:38–46. doi: 10.1016/j.micpath.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Tournier JN, Mohamadzadeh M. Key roles of dendritic cells in lung infection and improving anthrax vaccines. Trends Mol Med. 2010;16:303–312. doi: 10.1016/j.molmed.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 33.Russell BH, Liu Q, Jenkins SA, Tuvim MJ, Dickey BF, Xu Y. In vivo demonstration and quantification of intracellular Bacillus anthracis in lung epithelial cells. Infect Immun. 2008;76:3975–3983. doi: 10.1128/IAI.00282-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xue Q, Jenkins SA, Gu C, Smeds E, Liu Q, Vasan R, Russell BH, Xu Y. Bacillus anthracis spore entry into epithelial cells is an actin-dependent process requiring c-Src and PI3K. PLoS One. 2010;5:e11665. doi: 10.1371/journal.pone.0011665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gut IM, Tamilselvam B, Prouty AM, Stojkovic B, Czeschin S, van der Donk WA, Blanke SR. Bacillus anthracis spore interactions with mammalian cells: Relationship between germination state and the outcome of in vitro. BMC Microbiol. 2011;11:46. doi: 10.1186/1471-2180-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guidi-Rontani C, Weber-Levy M, Labruyere E, Mock M. Germination of Bacillus anthracis spores within alveolar macrophages. Mol Microbiol. 1999;31:9–17. doi: 10.1046/j.1365-2958.1999.01137.x. [DOI] [PubMed] [Google Scholar]
- 37.Barua S, McKevitt M, DeGiusti K, Hamm EE, Larabee J, Shakir S, Bryant K, Koehler TM, Blanke SR, Dyer D, Gillaspy A, Ballard JD. The mechanism of Bacillus anthracis intracellular germination requires multiple and highly diverse genetic loci. Infect Immun. 2009;77:23–31. doi: 10.1128/IAI.00801-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xue Q, Gu C, Rivera J, Hook M, Chen X, Pozzi A, Xu Y. Entry of Bacillus anthracis spores into epithelial cells is mediated by the spore surface protein BclA, integrin alpha2beta1 and complement component C1q. Cell Microbiol. 2011;13:620–634. doi: 10.1111/j.1462-5822.2010.01558.x. [DOI] [PubMed] [Google Scholar]
- 39.Russell BH, Vasan R, Keene DR, Xu Y. Bacillus anthracis internalization by human fibroblasts and epithelial cells. Cellular Microbiology. 2007;9:1262–1274. doi: 10.1111/j.1462-5822.2006.00869.x. [DOI] [PubMed] [Google Scholar]
- 40.Boydston JA, Chen P, Steichen CT, Turnbough CL., Jr Orientation within the exosporium and structural stability of the collagen-like glycoprotein BclA of Bacillus anthracis. J Bacteriol. 2005;187:5310–5317. doi: 10.1128/JB.187.15.5310-5317.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Russell BH, Vasan R, Keene DR, Koehler TM, Xu Y. Potential dissemination of Bacillus anthracis utilizing human lung epithelial cells. Cell Microbiol. 2008;10:945–967. doi: 10.1111/j.1462-5822.2007.01098.x. [DOI] [PubMed] [Google Scholar]
- 42.Lu JH, Teh BK, Wang L, Wang YN, Tan YS, Lai MC, Reid KB. The classical and regulatory functions of C1q in immunity and autoimmunity. Cell Mol Immunol. 2008;5:9–21. doi: 10.1038/cmi.2008.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nayak A, Ferluga J, Tsolaki AG, Kishore U. The non-classical functions of the classical complement pathway recognition subcomponent C1q. Immunol Lett. 2010 doi: 10.1016/j.imlet.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 44.Alvarez-Dominguez C, Carrasco-Marin E, Leyva-Cobian F. Role of complement component C1q in phagocytosis of Listeria monocytogenes by murine macrophage-like cell lines. Infect Immun. 1993;61:3664–3672. doi: 10.1128/iai.61.9.3664-3672.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ogden CA, deCathelineau A, Hoffmann PR, Bratton D, Ghebrehiwet B, Fadok VA, Henson PM. C1q and mannose binding lectin engagement of cell surface calreticulin and CD91 initiates macropinocytosis and uptake of apoptotic cells. J Exp Med. 2001;194:781–795. doi: 10.1084/jem.194.6.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roumenina LT, Kantardjiev AA, Atanasov BP, Waters P, Gadjeva M, Reid KB, Mantovani A, Kishore U, Kojouharova MS. Role of Ca2+ in the electrostatic stability and the functional activity of the globular domain of human C1q. Biochemistry. 2005;44:14097–14109. doi: 10.1021/bi051186n. [DOI] [PubMed] [Google Scholar]
- 47.Stoiber H, Ebenbichler CF, Thielens NM, Arlaud GJ, Dierich MP. HIV-1 rsgp41 depends on calcium for binding of human c1q but not for binding of gp120. Mol Immunol. 1995;32:371–374. doi: 10.1016/0161-5890(94)00156-u. [DOI] [PubMed] [Google Scholar]
- 48.Watford WT, Ghio AJ, Wright JR. Complement-mediated host defense in the lung. Am J Physiol Lung Cell Mol Physiol. 2000;279:L790–798. doi: 10.1152/ajplung.2000.279.5.L790. [DOI] [PubMed] [Google Scholar]
- 49.Merino S, Nogueras MM, Aguilar A, Rubires X, Alberti S, Benedi VJ, Tomas JM. Activation of the complement classical pathway (C1q binding) by mesophilic Aeromonas hydrophila outer membrane protein. Infect Immun. 1998;66:3825–3831. doi: 10.1128/iai.66.8.3825-3831.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Merino S, Vilches S, Canals R, Ramirez S, Tomas JM. A C1q-binding 40 kDa porin from Aeromonas salmonicida: cloning, sequencing, role in serum susceptibility and fish immunoprotection. Microb Pathog. 2005;38:227–237. doi: 10.1016/j.micpath.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 51.Roumenina LT, Popov KT, Bureeva SV, Kojouharova M, Gadjeva M, Rabheru S, Thakrar R, Kaplun A, Kishore U. Interaction of the globular domain of human C1q with Salmonella typhimurium lipopolysaccharide. Biochim Biophys Acta. 2008;1784:1271–1276. doi: 10.1016/j.bbapap.2008.04.029. [DOI] [PubMed] [Google Scholar]
- 52.Fulop M, Webber T, Manchee R. Activation of the complement system by Francisella tularensis lipopolysaccharide. New Microbiol. 1993;16:141–147. [PubMed] [Google Scholar]
- 53.Loos M, Euteneuer B, Clas F. Interaction of bacterial endotoxin (LPS) with fluid phase and macrophage membrane associated C1Q. The FC-recognizing component of the complement system. Adv Exp Med Biol. 1990;256:301–317. doi: 10.1007/978-1-4757-5140-6_26. [DOI] [PubMed] [Google Scholar]
- 54.Mintz CS, Arnold PI, Johnson W, Schultz DR. Antibody-independent binding of complement component C1q by Legionella pneumophila. Infect Immun. 1995;63:4939–4943. doi: 10.1128/iai.63.12.4939-4943.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alberti S, Marques G, Camprubi S, Merino S, Tomas JM, Vivanco F, Benedi VJ. C1q binding and activation of the complement classical pathway by Klebsiella pneumoniae outer membrane proteins. Infect Immun. 1993;61:852–860. doi: 10.1128/iai.61.3.852-860.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aubert B, Chesne S, Arlaud GJ, Colomb MG. Antibody-independent interaction between the first component of human complement, C1, and the outer membrane of Escherichia coli D31 m4. Biochem J. 1985;232:513–519. doi: 10.1042/bj2320513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stemmer F, Loos M. Evidence for direct binding of the first component of complement, C1, to outer membrane proteins from Salmonella minnesota. Curr Top Microbiol Immunol. 1985;121:73–84. doi: 10.1007/978-3-642-45604-6_4. [DOI] [PubMed] [Google Scholar]
- 58.Butko P, Nicholson-Weller A, Wessels MR. Role of complement component C1q in the IgG-independent opsonophagocytosis of group B Streptococcus. J Immunol. 1999;163:2761–2768. [PubMed] [Google Scholar]
- 59.Levy NJ, Kasper DL. Antibody-independent and -dependent opsonization of group B Streptococcus requires the first component of complement C1. Infect Immun. 1985;49:19–24. doi: 10.1128/iai.49.1.19-24.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Levy NJ, Kasper DL. Surface-bound capsular polysaccharide of type Ia group B Streptococcus mediates C1 binding and activation of the classic complement pathway. J Immunol. 1986;136:4157–4162. [PubMed] [Google Scholar]
- 61.Hu H, Sa Q, Koehler TM, Aronson AI, Zhou D. Inactivation of Bacillus anthracis spores in murine primary macrophages. Cell Microbiol. 2006;8:1634–1642. doi: 10.1111/j.1462-5822.2006.00738.x. [DOI] [PubMed] [Google Scholar]
- 62.Guidi-Rontani C, Weber-Levy M, Labruyere E, Mock M. Germination of Bacillus anthracis spores within alveolar macrophages. Mol Microbiol. 1999;31:9–17. doi: 10.1046/j.1365-2958.1999.01137.x. [DOI] [PubMed] [Google Scholar]
- 63.Guidi-Rontani C, Levy M, Ohayon H, Mock M. Fate of germinated Bacillus anthracis spores in primary murine macrophages. Mol Microbiol. 2001;42:931–938. doi: 10.1046/j.1365-2958.2001.02695.x. [DOI] [PubMed] [Google Scholar]
- 64.Dixon TC, Fadl AA, Koehler TM, Swanson JA, Hanna PC. Early Bacillus anthracis-macrophage interactions: intracellular survival survival and escape. Cell Microbiol. 2000;2:453–463. doi: 10.1046/j.1462-5822.2000.00067.x. [DOI] [PubMed] [Google Scholar]
- 65.Ireland JA, Hanna PC. Macrophage-enhanced germination of Bacillus anthracis endospores requires gerS. Infect Immun. 2002;70:5870–5872. doi: 10.1128/IAI.70.10.5870-5872.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hu H, Emerson J, Aronson AI. Factors involved in the germination and inactivation of Bacillus anthracis spores in murine primary macrophages. FEMS Microbiol Lett. 2007;272:245–250. doi: 10.1111/j.1574-6968.2007.00766.x. [DOI] [PubMed] [Google Scholar]
- 67.Weiner MA, Hanna PC. Macrophage-mediated germination of Bacillus anthracis endospores requires the gerH operon. Infect Immun. 2003;71:3954–3959. doi: 10.1128/IAI.71.7.3954-3959.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Heffernan BJ, Thomason B, Herring-Palmer A, Shaughnessy L, McDonald R, Fisher N, Huffnagle GB, Hanna P. Bacillus anthracis phospholipases C facilitate macrophage-associated growth and contribute to virulence in a murine model of inhalation anthrax. Infect Immun. 2006;74:3756–3764. doi: 10.1128/IAI.00307-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ramarao N, Lereclus D. The InhA1 metalloprotease allows spores of the B. cereus group to escape macrophages. Cell Microbiol. 2005;7:1357–1364. doi: 10.1111/j.1462-5822.2005.00562.x. [DOI] [PubMed] [Google Scholar]
- 70.Heffernan BJ, Thomason B, Herring-Palmer A, Hanna P. Bacillus anthracis anthrolysin O and three phospholipases C are functionally redundant in a murine model of inhalation anthrax. FEMS Microbiol Lett. 2007;271:98–105. doi: 10.1111/j.1574-6968.2007.00713.x. [DOI] [PubMed] [Google Scholar]
- 71.Mosser EM, Rest RF. The Bacillus anthracis cholesterol-dependent cytolysin, Anthrolysin O, kills human neutrophils, monocytes and macrophages. BMC Microbiol. 2006;6:56. doi: 10.1186/1471-2180-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wei Z, Schnupf P, Poussin MA, Zenewicz LA, Shen H, Goldfine H. Characterization of Listeria monocytogenes expressing anthrolysin O and phosphatidylinositol-specific phospholipase C from Bacillus anthracis. Infect Immun. 2005;73:6639–6646. doi: 10.1128/IAI.73.10.6639-6646.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pomerantsev AP, Kalnin KV, Osorio M, Leppla SH. Phosphatidylcholine-specific phospholipase C and sphingomyelinase activities in bacteria of the Bacillus cereus group. Infect Immun. 2003;71:6591–6606. doi: 10.1128/IAI.71.11.6591-6606.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rety S, Salamitou S, Garcia-Verdugo I, Hulmes DJS, Le Hegarat F, Chaby R, Lewit-Bentley A. The Crystal Structure of the Bacillus anthracis Spore Surface Protein BclA Shows Remarkable Similarity to Mammalian Proteins. J Biol Chem. 2005;280:43073–43078. doi: 10.1074/jbc.M510087200. [DOI] [PubMed] [Google Scholar]
- 75.Ghai R, Waters P, Roumenina LT, Gadjeva M, Kojouharova MS, Reid KB, Sim RB, Kishore U. C1q and its growing family. Immunobiology. 2007;212:253–266. doi: 10.1016/j.imbio.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 76.Daubenspeck JM, Zeng H, Chen P, Dong S, Steichen CT, Krishna NR, Pritchard DG, Turnbough CL., Jr Novel oligosaccharide side chains of the collagen-like region of BclA, the major glycoprotein of the Bacillus anthracis exosporium. J Biol Chem. 2004;279:30945–30953. doi: 10.1074/jbc.M401613200. [DOI] [PubMed] [Google Scholar]
- 77.Xu Y, Keene DR, Bujnicki JM, Hook M, Lukomski S. Streptococcal Scl1 and Scl2 proteins form collagen-like triple helices. J Biol Chem. 2002;277:27312–27318. doi: 10.1074/jbc.M201163200. [DOI] [PubMed] [Google Scholar]
- 78.Lukomski S, Nakashima K, Abdi I, Cipriano VJ, Ireland RM, Reid SD, Adams GG, Musser JM. Identification and characterization of the scl gene encoding a group A Streptococcus extracellular protein virulence factor with similarity to human collagen. Infect Immun. 2000;68:6542–6553. doi: 10.1128/iai.68.12.6542-6553.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Paterson GK, Nieminen L, Jefferies JM, Mitchell TJ. PclA, a pneumococcal collagen-like protein with selected strain distribution, contributes to adherence and invasion of host cells. FEMS Microbiol Lett. 2008;285:170–176. doi: 10.1111/j.1574-6968.2008.01217.x. [DOI] [PubMed] [Google Scholar]
- 80.Caswell CC, Lukomska E, Seo NS, Hook M, Lukomski S. Scl1-dependent internalization of group A Streptococcus via direct interactions with the alpha2beta(1) integrin enhances pathogen survival and re-emergence. Mol Microbiol. 2007;64:1319–1331. doi: 10.1111/j.1365-2958.2007.05741.x. [DOI] [PubMed] [Google Scholar]
- 81.Han R, Caswell CC, Lukomska E, Keene DR, Pawlowski M, Bujnicki JM, Kim JK, Lukomski S. Binding of the low-density lipoprotein by streptococcal collagen-like protein Scl1 of Streptococcus pyogenes. Mol Microbiol. 2006;61:351–367. doi: 10.1111/j.1365-2958.2006.05237.x. [DOI] [PubMed] [Google Scholar]
- 82.Reuter M, Caswell CC, Lukomski S, Zipfel PF. Binding of the human complement regulators CFHR1 and factor H by streptococcal collagen-like protein 1 (Scl1) via their conserved C termini allows control of the complement cascade at multiple levels. J Biol Chem. 2010;285:38473–38485. doi: 10.1074/jbc.M110.143727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bozue J, Cote CK, Moody KL, Welkos SL. Fully virulent Bacillus anthracis does not require the immunodominant protein BclA for pathogenesis. Infect Immun. 2007;75:508–511. doi: 10.1128/IAI.01202-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Harvill ET, Lee G, Grippe VK, Merkel TJ. Complement Depletion Renders C57BL/6 Mice Sensitive to the Bacillus anthracis Sterne Strain. Infect Immun. 2005;73:4420–4422. doi: 10.1128/IAI.73.7.4420-4422.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Welkos SL, Keener TJ, Gibbs PH. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect Immun. 1986;51:795–800. doi: 10.1128/iai.51.3.795-800.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.