Abstract
A randomized controlled trial of two formats of a program ("Women Take PRIDE") to enhance management of heart disease by patients was conducted. Older women (N=575) were randomly assigned to a group or self-directed format or to a control group. Data regarding symptoms, functional health status and weight were collected at baseline, 4, 12 and 18 months. The formats produced different outcomes. At 18 months, the self-directed format was better than control in reducing the number (p ≤ 0.02), frequency (p ≤ 0.03) and bothersomeness (p ≤ 0.02) of cardiac symptoms. The self-directed format was also better than the group format in reducing symptom frequency of all types (p≤ 0.04). The group format improved ambulation at 12 months (p≤ 0.04), weight loss at 18 months (p≤.03), and group participants were more likely to complete the program (p ≤ 0.05). The availability of different learning formats could enhance management of cardiovascular disease by patients.
Keywords: interventions for patients, heart disease, program evaluation, learning formats
Introduction
Heart disease continues to be a leading cause of death and disability in women (AHA, 2006). Although coronary heart disease risk in women lags ten years behind that of men, risk increases progressively with age (Bello & Mosca, 2004). Despite a declining death rate due to cardiovascular disease over the past 20 years, the number of women dying has continued to rise due to an aging population (AHA, 2006). As women age, they are also more likely than men to have concomitant disease such as diabetes and hypertension and may be at higher risk for reduced functional capacity (Ades, 2006; Bello & Mosca, 2004; Davidson et al., 2003).
The ways individuals manage their chronic conditions differ as does the context for their management efforts. Women with heart disease compared to men with heart disease have been shown to be older, widowed, living alone, to report more severe symptoms and to be more likely to avoid physical activity (Sharpe, Clark, & Janz, 1991). They report greater negative effect of their illness on their mobility, ambulation and social interactions (Agewall et al., 2004; Vaccarino et al., 2003; Abbey & Stewart, 2000; Sharpe, Clark, & Janz, 1991). Previous work by the authors has shown that although physicians recommend exercise to both sexes, women are much less likely to be confident that they can adhere to a suggested exercise regimen (Clark et al., 1997). In addition, a study to evaluate an intervention for men and women to enhance how they manage tasks and problems related to the control of their heart disease illustrated that both experienced significant improvement in their quality of life and overall functioning but only men improved their levels of physical activity (Clark et al., 1997).
Subsequent research showed that an intervention that focuses on management problems of women can enhance their symptom status, and physical functioning and reduce weight (Clark et al., 2000; Janz et al., 1999). Given the increase in cardiovascular disease among women and the potential for interventions to assist them, means to reach large numbers of women with effective programs are needed.
Little examination has been undertaken to compare outcomes of different program formats to enable participants to manage a disease at home in accordance with clinicians' instructions. Meta analyses and review of studies of group and individual interventions (Barlow & Parsons, 2002; Norris, Lau, Smith, Schmid, & Engelgau, 2002; van der Bij, Laurant, & Wensing, 2002) suggest that individualized approaches are equally as effective as group ones. However, data are inconclusive. At least one observer has suggested that individual approaches might produce different outcomes than group approaches (van der Bij et al, 2002).. On the other hand, at least one study has suggested that a group program produces better outcomes than an individualized one.
Group meeting formats have been very frequently used to provide patient education (Wilson, 1997). However, not all women take advantage of group format programs as they necessitate greater attention to scheduling, traveling to meeting sites and competing demands of work, family care and related obligations. It has been estimated that between 40 and 50% of women who could benefit from disease management education fail to participate because of the demands of group participation (Clark et al., 2000). Individualized programs on the other hand can be more responsive to particular individual learning constraints and are frequently employed in clinical settings. Nonetheless, few studies have compared outcomes of different learning formats in producing health outcomes and none has explored the question for individuals with cardiovascular disease.
This paper presents findings of a clinical trial conducted as part of a larger study (Janevic et al., 2003) to assess outcomes when comparing a group format with a self-directed format of a program to enable older women to manage their heart disease more effectively. It also compared both formats with a control group. The hypotheses were that a) women assigned to an individualized (self-directed) format would exhibit the same or improved health-related quality of life outcomes, including physical and psychosocial functioning, frequency and severity of symptoms, ambulation, and weight loss as women assigned to a group format, b) women in both formats would achieve better outcomes than the control group and c) differences in program participants by format would be evident.
Methods
Sample and Study Design
Participants in this study were non-institutionalized, ambulatory women identified at five hospital sites in southeastern Michigan. All study procedures were approved by the University of Michigan Institutional Review Board and the Institutional Review Boards of participating hospitals. Inclusion criteria were: 60 years of age or older; diagnosed cardiac condition (i.e., arrhythmia, angina, myocardial infarction, congestive heart failure or valvular disease, as the physicians' recommendations for managing these conditions generally include the common topics of medication use, physical activity, diet, stress reduction, and smoking cessation); treated by daily heart medication; seen by a physician within the past year; and living within one hour of the study site. Lists of potential study participants were compiled from patient rosters in physician offices and outpatient clinics and were then reviewed by the woman’s physician. If, in the physician’s assessment, a woman would not be able to participate fully in the program due to medical reasons (e.g., terminal illness, memory loss or significant hearing loss), she was excluded, although very few potential research participants were excluded in this second step.
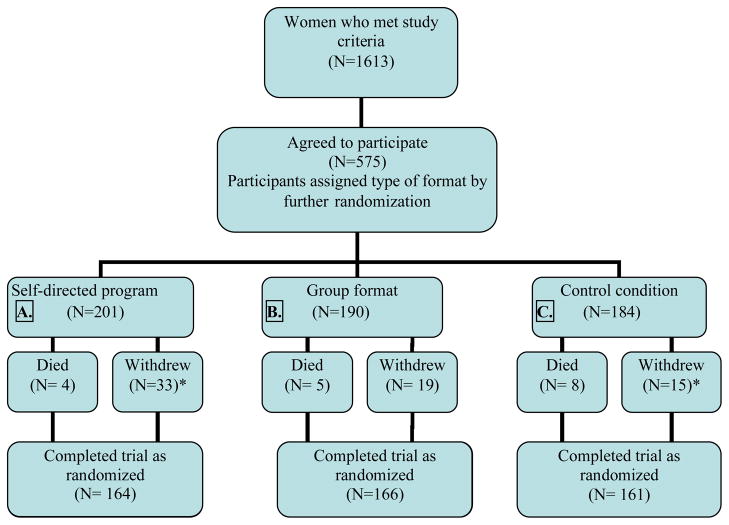
Figure 1 provides the study design and participation from recruitment through completion of the 18-month study. At baseline 1,613 women who met the study criteria were available for recruitment. Potential research participants received an introductory letter explaining the research and their physician’s participation, followed by a telephone contact. All potential participants were told that the purpose of the study was to learn more about what it is like for older women to live with a heart condition and to evaluate the effectiveness of a program tailored to this population. They were told that they would be randomly assigned to one of three groups; the WTP group format, self-directed format, or a “usual care” control group. Women in the "usual care" group would see their physicians on the routine schedule and receive any information that would normally be provided as part of regular care in the practice. They were told that if they were not invited to participate in the program initially, they would have an opportunity to do so at the end of the study if they were interested and if the program were shown to be beneficial. Women who declined participation in the study were asked to respond to a brief (five to ten minute) telephone interview that included questions about reasons for non-participation. A previous article (Janevic, et al., 2003) provides details regarding the nonparticipant data collection. The top two reasons provided for deciding not to participate in the study were participation concerns (e.g. transportation problems, too busy, works full-time) (34%) and not being interested (30%). The 37% participation rate observed in the older women invited to enroll is consistent with other investigations with older populations (for example, see Heid & Schmelzer, 2004; Sears, et al., 2003).
Figure 1.
Recruitment and Retention in the "Women take PRIDE" Study
* Indicate significance difference: p-value <0.05
Of these 1,613 available individuals, 575 consented to participate. Baseline data were collected before women were randomly assigned to a condition. Upon completion of the baseline interview, a procedure for allocation concealment (Pildal et al., 2005) was then used to assign participants in equal numbers to receive one of the two WTP formats or to the control group. The Interview Center coordinator provided the names of the study participants to the study coordinator who used a second set of sealed, opaque and sequentially numbered envelopes (compiled by the research secretary and research assistant using a book of random numbers) to assign them to one of three study conditions: 201 to the self-directed program (A), 190 to the group format program (B) and 184 to a control group (C). In an effort to assure similar care to all participants, no feedback about individual study participants was provided to health care personnel at the study sites. Unless a study participant happened to mention the study during the course of a routine visit, clinical staff had no knowledge of which patients had agreed to participate in the research.
Intervention
The theoretical assumptions underlying the development of the intervention have been described in detail elsewhere (Clark & Dodge, 1999), as have the iterative processes by which the program has evolved over time (Dodge, Janz, & Clark, 2002). The program was initially designed for use with groups of older women with heart disease. Based on social cognitive theory, especially the principles of self-regulation, the goal of the intervention is to enhance overall management by older women of problems arising from and tasks necessitated by the heart condition and to do so in light of their clinicians' recommendations. Using the acronym PRIDE, participants are introduced to the steps of a self regulatory process (Bandura et al 1986, Leventhal et al 2006, Clark & Zimmerman, 1990): problem selecting; researching one’s routine; identifying a management goal; developing a plan to meet the goal; and exploring rewards and expressing reactions. Physician activity (exercise) is used as the model behavior for teaching the steps of the process. The steps are carried out in accordance with the therapeutic plan provided by each woman’s physician related to medications, physical activity, diet and stress management. The content (instructor's manual, videotape, workbook and logs) is tailored to the unique roles, responsibilities and settings in which older women manage their heart disease.
Through examination of focus group data and pilot testing (Dodge, Janz, & Clark, 2002), a self-directed format for the group program was created. In this self-directed format, women engage in the same self regulatory process at home in their own timeframe. The content of and the materials used with the two formats are the same. Both formats consist of six units. In the group format, six to eight women meet for 2–2 1/2 hours on a weekly basis. A trained health educator, with the assistance of a peer leader, facilitates the sessions. In the self-directed format, women attend a single orientation session, then complete the program at home over six weeks. In the self-directed version, motivation and support that are part of the social environment in the group format are provided via an instructional videotape that presents examples of group discussions. Weekly telephone calls from a health educator or a peer leader are also provided. Participants in both formats receive a monthly newsletter for three months following completion of their program. At six months, the group format women are invited to attend a reunion and the self-directed participants receive an in-depth motivational telephone call from the health educator who conducted their initial orientation sessions.
Measures
The study outcomes comprise the general areas of symptom experience, functional health status and weight.
Symptom Experience
Symptom experience is an important determinant of physical functioning and general wellbeing. While several heart-specific instruments addressing symptoms were considered (e.g. Rosenthal, Lohr, Rubenstein, Goldberg, & Brook, 1982), these instruments did not address the diversity of cardiac conditions and symptoms in the target population. Therefore, symptom experience was calculated using an instrument tapping a broad range of heart conditions, the Symptom and Health Problem Profile utilized in previous program evaluations (Janz et al., 1999). Symptom experience was determined by asking about the presence, frequency and level of bother caused by 14 symptoms: chest pain, shortness of breath, fatigue, rapid or irregular heart beat, waking with chest pain, waking with shortness of breath, feeling blue, tense or stressed, worried, trouble falling asleep, trouble sleeping through the night, dizziness, pain other than chest and numbness or cramping in legs. Symptom frequency and bother in the seven days prior to each interview were assessed across a five-point Likert Scale with higher scores representing greater symptom effect. Total symptom frequency and bothersomeness scores were calculated for each research participant and ranged from 0 to 70. In addition, four subcategories were created with consultation from clinical cardiologists and included: cardiac symptoms (chest pain, shortness of breath, waking with chest pain, waking with shortness of breath, palpitations); sleep and rest; mental health; and, general non-specific symptoms. The Symptom and Health Problem Profile has a mean test-retest reliability score of .79 (Clark et al., 1997).
Functional Health Status
Psychosocial and Physical Functioning
The Sickness Impact Profile (SIP) is a 136-item generic instrument assessing functional health status. A total score and two dimension scores (psychosocial and physical) are provided. Independent categories of sleep and rest, eating, work, home management and recreation and pastimes are included in the calculation for the total SIP score. SIP scores are derived by adding the values for the items using predetermined weights for each item within that category and dividing the sum by the maximum possible dysfunction score for that dimension or category. The scores range from 0 to 100 with higher scores representing greater dysfunction or impairment due to health. The SIP has been shown to discriminate in expected directions among different populations at different age levels and for different degrees of disease severity (Patrick & Bergner, 1990). Its psychometric properties have been examined extensively (Bergner, 1985; Bergner, Bobbitt, Carter, & Gilson, 1981; Pollard, Bobbitt, Bergner, Martin, & Gilson, 1976). Test-retest reliability of the measure has been found to be .97 and Cronbach's alpha coefficient .94. In validity trials comparing SIP scores on functioning with clinical assessments of physical limitation made by physicians, correlation results were .50 (McDowell & Newell, 1987). The SIP psychosocial dimension score includes the categories of social interaction, communication, emotional behavior and alertness. The SIP physical dimension score is derived from three categories of items: ambulation, mobility and body care and movement.
Ambulation
The Six Minute Walk test developed by Guyatt et al. (1985) is a self-paced and efficient measure of exercise capacity. Using a premeasured distance, individuals are instructed to walk from end to end, covering as much distance as they can during the allotted time. They are instructed to walk at their own pace and to stop at any time as needed. A set of predetermined encouraging phrases is utilized at regular intervals. At the end of the test the distance walked is recorded. The Six Minute Walk test has been employed by several investigators (Cahalin, Mathier, Semigran, Dec, & DiSalvo, 1996; Hamilton & Haennel, 2000) with heart disease patients and has been found to be highly correlated with other measures of functional status (e.g., the treadmill test). Hamilton and Haennel (2000) evaluated the reliability and validity of the six minute walk in a Phase II/III Cardiac Rehabilitation program and concluded the test had strong test-retest reliability, was linearly associated with maximum metabolic equivalent (MET) values, and moderately correlated with the SF-36 Physical Function subscale.
Weight
Weight and height of each participant were recorded at each of the clinical assessments (see data collection section).
Other
Demographic information collected included age, race, education, employment status, income, marital status and whether living alone. In addition, data were collected regarding the nature of the cardiac diagnosis, and whether the heart condition was perceived as the primary health problem. Items tapping elements of self regulation were also included: goal setting, monitoring, evaluating, outcome expectancy, self-efficacy.
Data Collection
Data were collected at baseline and at 4, 12 and 18 months follow-up by telephone interview and through clinical assessment. Telephone interviews averaged 57 minutes in length. Participants were offered the option of completing the interview in two parts within a week’s time frame in order to reduce participant burden, an option chosen in approximately 35% of the cases. All interviewers completed an extensive training program to assure that standardized interviewing techniques and procedures were employed; ongoing supervision and supplemental training were provided.
In conducting clinical assessments, research study nurses followed a detailed written protocol to conduct the Six Minute Walk test and obtain height and weight measurements. The assessments were conducted at the participating hospitals. Interviewers, research nurses and the participants’ physicians were blind to both the women’s randomization status and participation in the program.
Data Analysis
The data were analyzed using SAS/STAT R software, Version 8 (1999) of the SAS System for SunOS 5.8 platform. As an initial step, the Wilcoxon tests for continuous variables and Chi-square tests for categorical variables were utilized to compare baseline demographic and health outcome variables across the three study conditions: self-directed format, group format; and “usual care” control.
Process data at four months were analyzed to identify changes in self regulation skills targeted in the intervention. First, mean change from baseline in the three groups was assessed using one-way analysis of variance between groups (ANOVA) for overall differences and then post-hoc Bonferroni comparisons were made to identify significant group differences.
Outcome variables measuring SIP physical and psychological functioning were scaled so that higher levels reflect greater impairment due to illness. The SIP and symptom variables were natural log transformed to make the normality assumption more plausible. Even after transformation, there was still considerable deviation from normality. Since normality may not be a reasonable assumption in these data, linear regression using generalized estimating equations (GEE) was used to obtain empirical estimates of the standard errors that were more robust than those used in standard linear regression with the normality assumption (Diggle, Liang, & Zeger, 1994; McCullagh & Nelder, 1989; Liang & Zeger, 1986).
The statistical approach utilized was chosen to meet our specific aim of assessing self regulation processes at 4 months, noted above and outcomes at two primary time points, 12 months from baseline and 18 months from baseline. Our interest was in ultimate results for the two time points. We did not try to assess cumulative effects from time period to time period. The current analysis is a valid alternative to the repeated measures analysis for estimating the intervention effect for answering our specific aims, and making fewer modeling assumptions. It adjusts for the baseline outcome and baseline covariates. Such an analysis provides an estimate of the intervention effect that has a similar efficiency compared to that obtained from repeated measures analysis such as GEEs (Yang and Tsiatsis, 2001). GEE assumes data are missing completely at random. The analysis used is based on maximum likelihood and requires a much weaker assumption about missing data, i.e., missing at random (Little and Rubin, 2002).
Outcome variables were analyzed at each time point controlling for baseline value, age, race, education and recruitment site and analyses were carried out using the women as they were randomized to each of the three study conditions.
There was no significant difference in the death rate between the study conditions. Women who died during the study (n = 17) did not differ significantly on demographic characteristics from those who completed 18 month follow–up, but at baseline did report significantly higher (worse SIP total (p = .006) and SIP physical dimension scores (p = .04). Women who completed versus women who dropped out of the study had higher (p = .01) education level, defined as high school or higher. No other differences were observed. While the rate of withdrawal from the study did not differ significantly between women in the 3 study conditions, those who withdrew compared to those who completed the 18 month follow-up were significantly more likely to have less than a high school education (p=.01) and to report higher (worse) SIP total (P = .006) and SIP psychosocial dimension scores (p=.01) at baseline.
FINDINGS
Table 1 displays the demographics, heart conditions, and health characteristics of the 575 study participants at baseline, stratified by format. The mean age of women in the sample was 72.8 years. The sample was predominately white (82.8%), most women had at least a high school education (81.7%) and 11.0% of the sample was currently employed. Over half (61.8%) of the women had an annual household income greater than $20,000. Approximately half (53.1%) of the women were married, while about one-third (34.0%) lived alone. Women reported ever having been diagnosed with specific heart conditions as follows: arrhythmia (54%), heart attack (42%), angina (38%), heart valve problems (26%), and congestive heart failure (26%). In addition 73% reported having been diagnosed with hypertension and 57% perceived their heart condition to be their primary health problem. When some other condition was reported as the primary health problem, it was most often diabetes (22%) or arthritis (21%). At baseline, there were no significant differences between study conditions in demographic, heart condition, or health characteristic variables.
Table 1.
Baseline demographics, heart diagnoses and health outcomes*
| Total Sample (n=575) | Control (n=184) | Group (n=190) | Self Directed (n=201) | |
|---|---|---|---|---|
| Demographics | ||||
| Age: mean (range) | 72.8 (60–90) | 72.5 (60–90) | 73.1 (61–87) | 72.7 (61–88) |
| Race (% white) | 82.8% | 83.0% | 82.5% | 83.1% |
| Education | ||||
| <HS % | 18.3% | 16.9% | 21.6% | 16.4% |
| =HS % | 37.2% | 41.3% | 33.2% | 37.3% |
| >HS % | 44.5% | 41.9% | 45.3% | 46.3% |
| Employed % | 11.0% | 12.5% | 11.6% | 9.0% |
| Income (%>20k) | 61.8% | 59.7% | 62.8% | 62.8% |
| Married % | 53.1% | 54.4% | 52.6% | 52.2% |
| Living Alone % | 34.0% | 34.8% | 33.8% | 33.3% |
| Heart Conditions Ever Diagnosed | ||||
| Angina | 37.6% | 39.7% | 36.8% | 36.3% |
| Heart attack | 41.7% | 45.7% | 38.4% | 41.2% |
| Arrhythmia | 54.3% | 58.7% | 52.6% | 51.7% |
| Hypertension | 73.0% | 73.4% | 74.2% | 71.6% |
| Congestive Heart Failure | 23.0% | 27.2% | 18.4% | 23.9% |
| Valve Problem | 25.7% | 25.0% | 24.7% | 27.4% |
| Health Outcomes | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| Symptom Experience: | ||||
| Total Symptom Number (0–14) | 4.50 (3.09) | 4.65 (3.02) | 4.39 (3.12) | 4.46 (3.14) |
| Total Symptom Frequency (0–70) | 14.00 (10.35) | 14.56 (10.13) | 13.45 (10.31) | 14.01 (10.61) |
| Total Symptom Bother (0–70) | 14.82 (12.31) | 15.09 (11.76) | 14.57 (12.41) | 14.82 (12.74) |
| Cardiac Symptom Number (0–5) | 1.08 (1.13) | 1.08 (1.10) | 1.09 (1.20) | 1.06 (1.09) |
| Cardiac Symptom Frequency (0–25) | 3.12 (3.53) | 3.15 (3.59) | 3.18 (3.73) | 3.02 (3.28) |
| Cardiac Symptom Bother (0–25) | 3.44 (4.28) | 3.51 (4.21) | 3.55 (4.71) | 3.27 (3.91) |
| Functional Health Status: | ||||
| SIP Physical Dimension score (0–100) | 9.42 (10.29) | 10.71 (11.12) | 8.28 (9.48) | 9.32 (10.16) |
| SIP Psychosocial Dimension score (0–100) | 7.43 (9.96) | 7.92 (10.36) | 6.57 (9.09) | 7.80 (10.38) |
| SIP Total Score (0–100) | 9.83 (9.83) | 10.84 (10.20) | 8.84 (9.11) | 9.83 (10.10) |
| 6-minute walk distance (ft) | 757 (463) | 736(451) | 781(482) | 752 (459) |
| Weight (lbs) : | 167.46 (37.12) | 165.15 (36.23) | 168.67 (38.38) | 168.45 (36.83) |
No significant (p-value ≤ 0.05) within-arm differences were found in any of the demographic, heart diagnoses or health outcomes.
Process evaluation at 4 months showed that women in both group and self directed formats significantly increased their use of two self regulation elements related to the model behavior (exercise). The mean for monitoring activity levels for group women was .34 and for self directed women .38 versus -.11 for control women (p=.001 for both comparisons). The mean for evaluating their activity level was .32 for group women versus −.11 for controls (p=.05) and for self directed women .49 versus controls −.11 (p=.01).
Table 2 presents 12 and 18 month outcome data for symptoms, ambulation, and weight. There were no differences at 12 months between groups and formats on number, frequency or bother of cardiac symptoms, nor symptoms in total. At the 18 month time point, however, significant differences were observed. Women in the self-directed format were significantly more likely to experience a lower number of cardiac symptoms compared to control group women (p ≤ 0.02, A versus C) and marginally lower than group format women (p ≤ 0.06, A versus B). They were also significantly more likely to experience less frequent cardiac symptoms than control women (p≤ 0.03, A versus C) and less frequent cardiac symptoms than women in the group format (p ≤ 0.04, A versus B). The same pattern was evident regarding the bothersomeness of cardiac symptoms. Self-directed women experienced significantly less symptom bother than controls (p ≤ 0.02 A versus C) and marginally less (p ≤ 0.07) than group format women (A versus B). When all types of symptoms were considered, the pattern was again seen, for number and bother of symptoms, but not frequency.
Table 2.
Significant findings regarding the comparison of outcomes between treatment groups (intent-to-treat) controlling for baseline value, age, race, education and site1
| Month 12 | Month 18 | ||||
|---|---|---|---|---|---|
| Outcomes | Comparison b | Estimate | p-value | Estimate | p-value |
| Symptom Experience c | |||||
| Total Symptom Number (0–14) | (A v C) SD v C | 0.29 | 0.531 | −0.57 | 0.039 |
| (B v C) G v C | 0.19 | 0.915 | −0.04 | 0.369 | |
| (A v B) SD v G | 0.10 | 0.622 | −0.53 | 0.258 | |
| Total Symptom Frequency (0–70) | (A v C) SD v C | 0.65 | 0.284 | −1.24 | 0.093 |
| (B v C) G v C | 1.44 | 0.931 | 0.92 | 0.709 | |
| (A v B) SD v G | −0.79 | 0.293 | −2.17 | 0209 | |
| Total Symptom Bother (0–70) | (A v C) SD v C | 0.90 | 0.339 | −2.31 | 0.017 |
| (B v C) G v C | 0.65 | 0.484 | 0.18 | 0.269 | |
| (A v B) SD v G | 0.25 | 0.788 | −2.49 | 0.210 | |
| Cardiac Symptoms | |||||
| Number of Common Cardiac Symptoms (0–5) | (A v C) SD v C | 0.03 | 0.783 | −0.22 | 0.016 |
| (B v C) G v C | −0.04 | 0.412 | −0.03 | 0.546 | |
| (A v B) SD v G | 0.07 | 0.606 | −0.19 | 0.060 | |
| Frequency of Common Cardiac Symptoms (0–25) | (A v C) SD v C | 0.03 | 0.724 | −0.55 | 0.033 |
| (B v C) G v C | 0.03 | 0.494 | 0.18 | 0.915 | |
| (A v B) SD v G | 0.00 | 0.746 | −0.73 | 0.044 | |
| Bother with Common Cardiac Symptoms (0–25) | (A v C) SD v C | 0.30 | 0.905 | −0.73 | 0.018 |
| (B v C) G v C | −0.07 | 0.337 | 0.07 | 0.515 | |
| (A v B) SD v G | 0.37 | 0.421 | −0.81 | 0.071 | |
| 6-minute walk distance (ft) d | (A v C) SD v C | 31.4 | 0.409 | 12.1 | 0.777 |
| (B v C) G v C | 79.7 | 0.036 | 22.5 | 0.585 | |
| (A v B) SD v G | −48.3 | 0.202 | −10.4 | 0.806 | |
| Weight (lbs) d | (A v C) SD v C | −0.44 | 0.676 | 1.50 | 0.305 |
| (B v C) G v C | −1.27 | 0.212 | −1.72 | 0.227 | |
| (A v B) SD v G | 0.84 | 0.412 | 3.22 | 0.026 | |
The total Sickness Impact Profile score and the physical and psychosocial dimension scores are not included as no significant findings between groups were found at 12 and 18 month follow-up.
(A) SD = Self-Directed Format, (B) G = Group Format, (C) C = Control Group.
Analysis utilized log-transformed normal regression
Analysis utilized normal regression
Table 2 also illustrates that at the 12 month time point there was a statistically significant difference in the Six Minute Walk scores of group format women compared to controls (p ≤ 0.04, B versus C), with group format women walking greater distances in the allotted time. At 18 months, women in the group format lost significantly (p≤.03) more weight than women in the self-directed format (B versus A), although neither format was statistically significantly different from control. Estimates of group differences at 18 months were in the direction favoring the group intervention, but were generally diminished and not statistically significant at the 5% level.
At both the 12 month and 18 month time points, there were no statistically significant differences between the control group and either program format nor differences between program formats on the SIP dimension or total scores.
Table 3 illustrates that format had an effect on program participation. Women in the group format were significantly (p ≤ 0.05) more likely to complete sessions of the six session program (3.81 classes out of 6, B versus A) than were self-directed format women likely to complete their six unit program (3.31 classes out of 6). There was also a trend (p ≤.07) for group format women compared to self-directed participants to develop a plan for reaching their behavioral goal as part of the program (B versus A). There were no significant differences between formats in the rate of participant withdrawal from the program or completion of the observation logs used as teaching tools in both formats.
Table 3.
Odds ratios from logistic regression analysis assessing effects of format type on program attendance and adherence, controlling for age, race, education and sitea
| Effect of format: Group vs. Self-Directed | |||
|---|---|---|---|
|
| |||
| ORb | (95%CI) | p-value | |
| Withdrew before treatment ends (yes vs. no) | 1.12 | (0.69,1.82) | 0.637 |
| Completed observation log (score of 1+ vs. 0) | 1.31 | (0.77,2.23) | 0.326 |
| Developed plan for behavioral goal (score of 1+ vs. 0) | 1.47 | (0.97,2.23) | 0.070 |
| Mean | |||
| Number of Classes attended/completed (0–6) | |||
| Group | 3.81 | (3.43,4.18) | |
| SD | 3.31 | (2.96,3.67) | |
| G vs. SD | 0.5 | (0.01,0.98) | 0.045 |
Includes participants in group (G) format (n=190) and self-directed (SD) format (n=201)
Odds ratio >1 indicates a higher probability of event occurring in Group Format
Results indicate that the first study hypothesis (a) was only partially supported. Self-directed format women experienced improved outcomes over group women for symptoms but group women did better regarding weight loss and ambulation. The second hypothesis (b) was also only partially supported. The self-directed format produced better outcomes regarding symptoms compared to controls but the group format did not. The group format produced better results regarding ambulation compared to controls but the self-directed format did not. Neither format was better than controls regarding psychosocial and physical functioning as measured by the SIP. The third hypothesis (c) was supported. Women in the group format exhibited higher levels of program participation then women in the self directed format.
Discussion
To the investigators' knowledge, no controlled trials have examined the relative effects of a group format versus a self-directed format on the health status of older women with heart disease. This study provides findings for two versions of the same intervention: a group version and a self-directed version as they affect symptom experience, psychosocial and physical functioning, ambulation, and weight.
Findings from this study illustrated that after one and a half years women who were assigned to a self-directed format had fewer, less frequent and less bothersome cardiac symptoms. They also experienced less impact of all types of symptoms, that is, symptoms beyond just those associated with their heart condition. On the other hand, women assigned to the group format lost more weight and up to one year subsequent to the program could walk greater distances. These findings support observations (van der Bij AK, et al 2002) that different types of formats produce different outcomes. The findings do not negate the studies of others (Barlow, et al 2002, Norris et al 2002) that suggest both group and individualized formats are effective. Rather, they suggest that different formats are effective in different ways.
An interesting pattern was evident. At 12 months, women in the self-directed format actually experienced somewhat higher although not statistically significant levels of symptoms compared to control and group format women. However, ultimately their symptom experience levels were significantly lower. It may be that the highly individualistic focus on one's condition evident in the self-directed format created initial identification of troublesome symptoms and over time enabled women to derive more effective means to deal with them. Further, given the individual and independent nature of the self-directed format, it may be that the approach demanded that women develop (more than the group format women or controls) greater discipline in managing their condition. Over time these format characteristics produced benefits in the form of fewer symptoms of all kinds.
Neither format produced differences in functioning as measured by the SIP. The program regardless of format may not have been powerful enough to generate changes in women's functioning. Alternatively, as a measure, the SIP may not have been sensitive to small changes occurring in this ambulatory population. Many SIP items are designed to tap significant infirmity (e.g., I stay home most of the time, I am confined to bed, I walk only with help from someone). Fine line distinctions in psychosocial and physical functioning may not have been measurable with this instrument for women less likely to be homebound by their disease.
While the discipline required of the self directed format enhanced women's symptom control, group format women did better regarding weight loss and ambulation. Weight reduction and walking greater distances are tasks where group social support and encouragement are likely to play a role. Data showed that these weight and walking outcomes decayed over time. Ongoing or “booster” interventions may be needed to enable women in learning groups to maintain gains of this type.
Group format women did better on program process related outcomes. They were more likely than the self-directed format women to complete the program sessions/units and more likely to develop a behavioral plan, an objective of program delivery. Interaction with others engendering social support and social comparisons may have encouraged, indeed, motivated group women to participate more fully in their version of the intervention.
At 4 months, shortly after participating in the intervention, women in both formats were more self regulating than control women. Monitoring and evaluating one's behavior are relevant to tasks associated with symptom control and physical activity. More self regulation likely contributed to the improved outcomes observed in both formats although does not explain differences seen by format. The findings support the work of others (Bandura, 1986, Leventhal et al 2006) that suggest self regulation as the mechanism through which changes in health outcomes are achieved.
LIMITATIONS
Women enrolled in the study were not recruited to be representative of the general population of women or any subgroup. The sample was predominantly white and high school educated.
No direct observation of participation of women in the self directed group was possible. Participation was assessed by review of the materials they returned to project staff and reports of health educators providing telephone counseling.
As noted, the SIP measure may not have tapped changes observed in a non house or bed bound individual.
Practice Implications
The intervention formats tested in this trial are relatively easy and inexpensive to provide within a health care system. Each achieved different outcomes and produced results across areas of importance to both patients and health care providers. If further studies support that particular management concerns are best dealt with using specific program formats, practitioners could guide health consumers to a program option most likely to be successful in his/her particular case (e.g., need for improved ambulation or symptom control). Having more than one program format available may also yield greater participation by patients in health education programs given competing demands on their time and learning style preferences. To make results optimum, practitioners might also consider offering programs that emphasize one format e.g. self directed but include some exposure to the other e.g. group.
CONCLUSION
Group formats may be more effective for problems that require more social support such as weight loss and exercise. Self directed formats may be more effective for symptom control. Future research should examine, further, effects of different formats, their relevance to subgroups of women and their utility for achieving different types of outcomes. Reaching and assisting the large number of older women with a heart condition through a variety of proven interventions formats may help to alleviate the disease burden they and their families bear.
Acknowledgments
This research was supported by Grant 5-R01-HL58611 from the Heart Division of the National Heart, Lung, and Blood Institute. We wish to acknowledge and thank our colleagues affiliated with the following medical centers for their assistance with this study: McLaren Regional Medical Center, Flint, Michigan; Genesys Regional Medical Center, Flint, Michigan; Henry Ford Hospital, Detroit, Michigan; Providence Hospital and Medical Centers, Detroit, Michigan; and Ingham Regional Medical Center, Lansing, Michigan. In addition we extend our thanks to Drs. Kim Eagle, Professor of Internal Medicine and Clinical Director of the University of Michigan Cardiovascular Center, and Claire Duvernoy, Assistant Professor of Internal Medicine – Cardiology University of Michigan Medical Center, for their contributions to this study. We also wish to thank Dr. Roderick Little, Professor of Biostatistics at the University of Michigan, for his review of an earlier version of this paper.
Contributor Information
Noreen M. Clark, Email: nmclark@umich.edu.
Nancy K. Janz, Email: nkjanz@umich.edu.
Julia A. Dodge, Email: jadodge@umich.edu.
Xihong Lin, Email: xlin@hsph.harvard.edu.
Britton L. Trabert, Email: btrabert@fhcrc.org.
Niko Kraciroti, Email: nicola@umich.edu.
Lori Mosca, Email: ljm10@columbia.edu.
John R.C. Wheeler, Email: jackwhee@umich.edu.
Steven Keteyian, Email: sketeyi1@hfhs.org.
Jersey Liang, Email: jliang@umich.edu.
References
- Abbey S, Stewart D. Gender and psychosomatic aspects of ischemic heart disease. Journal of Psychosomatic Research. 2000;48:417. doi: 10.1016/s0022-3999(99)00112-9. [DOI] [PubMed] [Google Scholar]
- Ades PA, Savage PD, Brawner CA, Lyon CE, Ehrman JK, Bunn JY, et al. Aerobic capacity in patients entering cardiac rehabilitation. Circulation. 2006;113(23):2706–2712. doi: 10.1161/CIRCULATIONAHA.105.606624. [DOI] [PubMed] [Google Scholar]
- Agewall S, Berglund M, Henareh L. Reduced quality of life after myocardial infarction in women compared with men. Clinical Cardiology. 2004;27(5):271. doi: 10.1002/clc.4960270506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Heart Association. Heart disease and stroke statistics - 2006 update. Dallas, TX: American Heart Association; 2006. [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1986. [Google Scholar]
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling. 2002;48:177. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- Bello N, Mosca L. Epidemiology of coronary heart disease in women. Progress in Cardiovascular Diseases. 2004;46(4):287. doi: 10.1016/j.pcad.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Bergner M. Measurement of health status. Medical Care. 1985;23:696. doi: 10.1097/00005650-198505000-00028. [DOI] [PubMed] [Google Scholar]
- Bergner M, Bobbitt RA, Carter WB, Gibson BS. The sickness impact profile: Development and final revision of a health status measure. Medical Care. 1981;19:787. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- Cahalin LP, Mathier MA, Semigran MJ, Dec W, DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest. 1996;110:325. doi: 10.1378/chest.110.2.325. [DOI] [PubMed] [Google Scholar]
- Clark NM, Zimmerman BJ. A social cognitive view of self-regulated learning about health. Health Education Research. 1990;5(3):371–379. doi: 10.1177/1090198114547512. [DOI] [PubMed] [Google Scholar]
- Clark NM, Dodge JA. Exploring self-efficacy as a predictor of disease management. Health Education & Behavior. 1999;26(1):72. doi: 10.1177/109019819902600107. [DOI] [PubMed] [Google Scholar]
- Clark NM, Janz NK, Dodge JA, Schork MA, Fingerlin TE, Wheeler JRC, et al. Changes in functional health status of older women with heart disease; evaluation of a program based on self-regulation. Journal of Gerontology: Social Sciences. 2000;55B(2):S117. doi: 10.1093/geronb/55.2.s117. [DOI] [PubMed] [Google Scholar]
- Clark NM, Janz NK, Dodge JA, Schork MA, Wheeler JRC, Liang J, et al. Self-management of heart disease by older adults. Research on Aging. 1997;19(3):362. [Google Scholar]
- Davidson PM, Daly J, Hancock K, Moser D, Chang E, Cockburn J. Perceptions and experiences of heart disease: A literature review and identification of a research agenda in older women. European Journal of Cardiovascular Nursing. 2003;2:255. doi: 10.1016/S1474-5151(03)00056-2. [DOI] [PubMed] [Google Scholar]
- Diggle PJ, Liang KY, Zeger SL. Analysis of longitudinal data. New York: Oxford University Press; 1994. [Google Scholar]
- Dodge JA, Janz NK, Clark NM. The evolution of an innovative heart disease management program for older women; integrating quantitative and qualitative methods in practice. Health Promotion and Practice. 2002;3(1):30. [Google Scholar]
- Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, et al. The 6-minute walk; A new measure of exercise capacity in patients with chronic heart failure. Canadian Medical Association Journal. 1985;132:919. [PMC free article] [PubMed] [Google Scholar]
- Halm EA, Mora P, Leventhal H. No symptoms, no asthma: The acute episodic disease belief is associated with poor self-management among inner-city adults with persistent asthma. Chest. 2006;129(3):573–580. doi: 10.1378/chest.129.3.573. [DOI] [PubMed] [Google Scholar]
- Hamilton DM, Haennel RG. Validity and reliability of the 6-minute walk test in a cardiac rehabilitation population. Journal of Cardiopulmonary Rehabilitation. 2000;20(3):156. doi: 10.1097/00008483-200005000-00003. [DOI] [PubMed] [Google Scholar]
- Heid HG, Schmelzer M. Influences on women's participation in cardiac rehabilitation. Rehabilitation Nursing. 2004;29(4):116. doi: 10.1002/j.2048-7940.2004.tb00327.x. [DOI] [PubMed] [Google Scholar]
- Janevic MR, Janz NK, Dodge JA, Lin X, Pan W, Sinco BR, et al. The role of choice in health education intervention trials: A review and case study. Social Science & Medicine. 2003;53:1581. doi: 10.1016/s0277-9536(02)00158-2. [DOI] [PubMed] [Google Scholar]
- Janz NK, Clark NM, Dodge JA, Schork MA, Mosca L, Fingerlin TE. The impact of a disease-management program on the symptom experiences of older women with heart disease. Women & Health. 1999;30(2):1. doi: 10.1300/j013v30n02_01. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13. [Google Scholar]
- McCullagh P, Nelder J. Generalized linear models. London: Chapman and Hall; 1989. [Google Scholar]
- McDowell I, Newell C. Measuring health: A guide to rating scales and questionnaires. New York: Oxford University Press; 1987. [Google Scholar]
- Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- Patrick DL, Bergner M. Measurement of health status in the 1990's. Annual Review of Public Health. 1990;11:165. doi: 10.1146/annurev.pu.11.050190.001121. [DOI] [PubMed] [Google Scholar]
- Pildal J, Chan AW, Hrobjartsson A, Forfang E, Altman DG, Gotzsche PC. Comparisons of descriptions of allocation concealment in trial protocols and the published reports: Cohort study. British Medical Journal. 2005;330(7499):1049. doi: 10.1136/bmj.38414.422650.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard WE, Bobbitt RA, Bergner M, Martin DP, Gibson BS. The sickness impact profile: Reliability of a health status measure. Medical Care. 1976;14:146. doi: 10.1097/00005650-197602000-00004. [DOI] [PubMed] [Google Scholar]
- Rosenthal M, Lohr KN, Rubenstein RS, Goldberg GA, Brook RH. Conceptualization and measurement of physiologic health for adults, volume 5: Congestive heart failure. Santa Monica, CA: Rand Corporation; 1982. (R-2262/5-HHS ed.) [Google Scholar]
- Sears SR, Stanton AL, Kwan L, Krupnick JL, Rowland JH, Meyerowitz BE, et al. Recruitment and retention challenges in breast cancer survivorship research: Results from a multisite, randomized intervention trial in women with early stage breast cancer. Cancer Epidemiology, Biomarkers & Prevention. 2003;12:1087. [PubMed] [Google Scholar]
- Sharpe PA, Clark NM, Janz NK. Differences in the impact and management of heart disease between older women and men. Women & Health. 1991;17(2):25. doi: 10.1300/J013v17n02_02. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Lin ZQ, Kasl SV, Mattera JA, Roumanis SA, Abramson JL, et al. Gender differences in recovery after coronary artery bypass surgery. Journal of the American College of Cardiology. 2003;41(2):307. doi: 10.1016/s0735-1097(02)02698-0. [DOI] [PubMed] [Google Scholar]
- van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: A review. American Journal of Preventive Medicine. 2002;22(2):120. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- Wilson SR. Individual versus group education: Is one better? Patient Education and Counseling. 1997;32:S67. doi: 10.1016/s0738-3991(97)00098-0. [DOI] [PubMed] [Google Scholar]