Abstract
Thrombocytopenia is a common feature among HIV-positive patients. However, there are few reports about this subject after highly active antiretroviral therapy (HAART) introduction. The authors show a retrospective description of epidemiology, clinical aspects, and treatment observed in 55 HIV-positive outpatients with thrombocytopenia treated in two reference centers for HIV treatment in São Paulo, Brazil. Thirty-four (62%) patients were male, 50 (91%) were Caucasian, with median of lymphocytes TCD4 of 394 cells/mm3. In 63.6% patients, the cause of thrombocytopenia was classified as immune thrombocytopenic purpura and non immune in 25.5%. Regular use of HAART was present in 43.6% of the population studied. In 20% HAART was initiated for thrombocytopenia treatment with improvement in platelets count observed after 3 months. Platelet transfusion was needed in 23.7% of the patients and one patient died due to bleeding. Thrombocytopenia is still common among patients infected with HIV, considered a multifactor disorder, commonly due to immune mechanisms in our cases. In the clinical setting, a diagnostic approach related to the hematological consequences of HIV infection is needed for a better therapy option for this population.
Keywords: HIV, AIDS, Thrombocytopenia
Keywords: Medicine & Public Health, Oncology, Human Genetics, Blood Transfusion Medicine, Hematology
Introduction
Thrombocytopenia is commonly observed among patients infected by HIV and could be present as first sign of disease in approximately 5–15% of patients. Forty percent may develop thrombocytopenia during advanced stages of disease. A decrease in this prevalence might be expected after HAART introduction; disorders of hematopoiesis, opportunistic infections and immune causes related to HIV leading to thrombocytopenia could be reverted [1, 2].
There are few reports of the epidemiology and causes of thrombocytopenia after HAART institution. It still remains an important issue, not only because of the risk of bleeding, but it may complicate other treatments for diseases such as C hepatitis infection and use of myelosuppressive agents (cancer, cytomegalovirus infection) in this population [3].
The authors described epidemiology, treatment and outcome in 55 HIV-positive outpatients with thrombocytopenia attended in two reference centers for HIV treatment in São Paulo, Brazil.
Materials and Methods
This study was performed by retrospective analysis of medical records from 55 HIV-positive outpatients with thrombocytopenia, treated at Hematology Section of Instituto de Infectologia Emílio Ribas and Centro de Referência e Treinamento em DST/Aids, São Paulo-Brazil, from January 1999 to December 2007. Both centers are considered reference for HIV patients’ treatment.
Patients included were adults with HIV infection (confirmed by ELISA and Western-blot assays) with platelet count <100.000/mm3 lasting for 3 or more consecutive months and not receiving treatment for cancer or C hepatitis.
Results
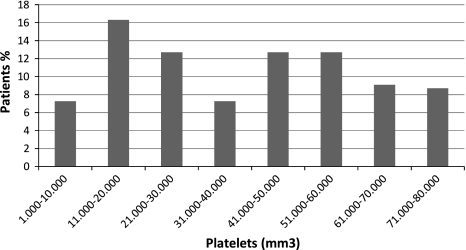
Characteristics of patients are shown in Table 1. Fifty-one (93%) patients were classified as men who have sex with men (MSM) and 4 (7%) heterosexual; among all patients, 2 (3.6%) also had history of intravenous drug use (IVDU). Twenty-eight (51%) patients had CD4 counts above 350 cells/mm3, 12 (22%) with CD4 <200 cells/mm3. Baseline platelet counts in the first visit (outpatient setting) are presented in Fig. 1.
Table 1.
Patient’s characteristics
| N = 55 (%) | |
|---|---|
| Gender | |
| Female | 21 (38) |
| Male | 34 (62) |
| Race | |
| Caucasian | 50 (91) |
| Mulatto | 4 (7.2%) |
| Afro-American | 1 (1.8%) |
| Age | |
| Median (range) | 42 (20–64) |
| CD4 count | |
| Median cells/mm3 (range) | 394 (6–1054) |
| ARV therapy | |
| Regular | 24 (43.6%) |
| No adherence | 17 (31.0%) |
| No use | 14 (25.4%) |
ARV antiretroviral
Fig. 1.
Baseline platelet counts
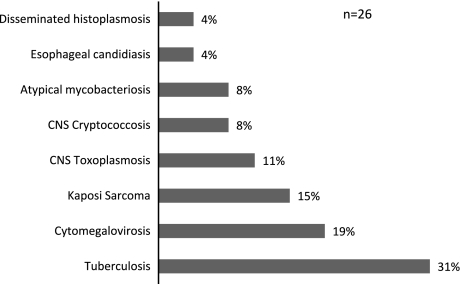
Among associated cytopenias, 12 (22%) patients had anemia and three (5.4%) low white blood cell counts. Twenty-seven bleeding episodes could be observed in 22 patients. Opportunistic conditions were detected in 26 patients and represented in Fig. 2. Tuberculosis was present in eight (31%) patients, six of them with pulmonary disease, one with lymphadenitis and one with disseminated disease.
Fig. 2.
Opportunistic diseases
In 35 (63.6%) patients, the cause of thrombocytopenia was associated to immune purpura and 14 (25.5%) deficiency of platelet production, both secondary to HIV infection. In one patient it was related to hepatitis B infection, one to hepatitis C infection, another one due to hypersplenism and three patients lost follow-up.
Twenty-four (43.6%) patients were in regular use of HAART at thrombocytopenia diagnosis. Nineteen needed therapy to increase platelets count, eleven patients used corticosteroids, two were treated with human intravenous immunoglobulin (IVIG) and six patients were treated with both. The majority of these patients used corticosteroids in a low dose (0.3–0.5 mg/kg) during 6 months maintaining satisfactory counts after therapy used above. In seven cases, change of HAART scheme was performed due to a decrease in CD4 counts and raise in viral load, guided by genotyping.
Eleven (20%) patients started HAART for thrombocytopenia with an increase in platelet counts after 3 months of therapy.
In 17 (31%) patients, irregular use of HAART was observed. Four (23.5%) had a rise in platelet count after using corticosteroids, two (11.7%) after IVIG and five (29.4%) with both.
Median platelets number among patients with response to treatment was 136.000/mm3. Thirteen (23.7%) patients needed platelet transfusion. Among them, two (3.6%) had fatal outcome (gastric bleeding and pneumonia).
Discussion
Immune thrombocytopenic purpura (ITP) is still considered a major cause of thrombocytopenia among HIV-positive patients. In our study, according to literature, the majority of patients were male, Caucasian, with median age of 42 years. There was a predominance of heterosexual patients and those related to unprotected sex; only 3.6% of patients related IVDU. There was a progression in Brazil toward heterosexual exposition, stable numbers of MSM and a decline of IVDU.
A higher number of median CD4 cells counts could be seen in thrombocytopenic patients compared to other studies, in which low platelet counts are related to disease progression (AIDS) [4].
Sloand et al. concluded that severe hemorrhage risk is not common even when platelet counts <50.000/mm3. Bleeding episodes have been described in 75–82% of patients with those counts, although severe events are rare [4]. We could observe in 40% of patients bleeding episodes, and 23.7% needed platelet transfusion. Only one patient died from hemorrhage.
In our report, tuberculosis was the most prevalent opportunistic disease (31%), followed by cytomegalovirus infection (19%), and related to thrombocytopenia. Although corticosteroids can be used for ITP treatment, it is not recommended in very immunosuppressed patients; in these cases, opportunistic infection of bone marrow as a cause for thrombocytopenia should be investigated.
Eleven patients started HAART with recovery in platelet counts. Recently, HAART use especially for immune thrombocytopenia is recommended even in patients with stable numbers of CD4 cells or viral load, which usually had no strict indication to start treatment for HIV infection, with good responses [2, 5–7].
In patients using HAART in a regular basis, only seven presented changes in CD4 counts and VL, needing modification in HAART scheme. However, the action of HAART in other sites infected by HIV as bone marrow is not elucidated, suggesting that thrombocytopenia could occur even in the presence of response for HIV treatment, measured in plasma and blood.
Further studies including higher number of patients are needed to establish prevalence of thrombocytopenia after HAART era, and its significance for morbidity and mortality in this population.
In conclusion, thrombocytopenia seems to be a common feature in HIV-positive patients that can lead to bleeding and difficult therapy for other pathologies, requiring treatment and even with known causes in the clinical setting, diagnostic screening for factors related to the virus, co-infection, opportunistic diseases are still needed for this specific population.
References
- 1.Aragão PM, Marques HH. Trombocitopenia associada ao HIV. J Bras Aids. 2005;6(4):165–188. [Google Scholar]
- 2.Carbonara S, Fiorentino G, Serio G, et al. Response of severe HIV associated thrombocytopenia to highly active antiretroviral therapy including protease inhibitors. J Infect. 2001;42:251–256. doi: 10.1053/jinf.2001.0833. [DOI] [PubMed] [Google Scholar]
- 3.Marks KM, Clarke RM, Bussel JB, Talal AH, Glesby MJ. Risk factors for thrombocytopenia in HIV-infected persons in the era of potent antiretroviral therapy. J Acquir Immune Defic Syndr. 2009;52(5):595–599. doi: 10.1097/QAI.0b013e3181b79aff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sloand EM, Klein HG, Banks SM, et al. Epidemiology of thrombocytopenia in HIV infection. Eur J Haematol. 1992;48:168–172. doi: 10.1111/j.1600-0609.1992.tb00591.x. [DOI] [PubMed] [Google Scholar]
- 5.Ananworanich J, Phanuphak N, Nuesch R, et al. Recurring thrombocytopenia associated with structured treatment interruption in patients with human immunodeficiency virus infection. Clin Infect Dis. 2003;37(5):723–726. doi: 10.1086/376989. [DOI] [PubMed] [Google Scholar]
- 6.Arranz Caso JA, Sánchez Mingo C, Garcia Tena J. Effect of highly active antiretroviral therapy on thrombocytopenia in patients with HIV infection. N Engl J Med. 1999;341:1239. doi: 10.1056/NEJM199910143411617. [DOI] [PubMed] [Google Scholar]
- 7.Scaradavou A. HIV-related thrombocytopenia. Blood Rev. 2002;16:73–76. doi: 10.1054/blre.2001.0188. [DOI] [PubMed] [Google Scholar]