Abstract
Most cases of Peutz-Jeghers type polyps of the stomach are associated with mucocutaneous pigmentation and multiple intestinal polyposis. A solitary Peutz-Jeghers type polyp of the stomach is rare. We here report a case of a 71-year-old woman with a solitary Peutz-Jeghers type polyp of the stomach who presented with intolerable epigastric pain and weight loss of 5 kg over the prior two months. During the hospital treatment course for this patient, endoscopic examination revealed a bulging lesion with a central hole, mucosal ulceration, an asymmetrical wall thickness and a narrowing of the gastric lumen. A gastric biopsy further revealed ulceration with moderate dysplasia. The patient received endoscopic ultrasonography which showed a second subepithelial lesion that measured 4 cm × 3 cm. Computed tomography of the abdomen subsequently showed a thickened gastric wall with three visibly enlarged lymph nodes, all greater than 1 cm. The suspected diagnosis was malignant gastric cancer with lymph node metastases. The other lesion, which measured 2 cm × 2 cm × 1 cm was noted in the submucosa of the jejunum during surgery. The patient was treated using a subtotal gastrectomy and partial resection of the jejunal tumor. The final pathological report indicated a gastric Peutz-Jeghers type polyp with proliferation of smooth muscle bundles in the submucosal layer, and hyperplastic glands in the mucosal layer and ectopic pancreas of the jejunum. This is the first reported clinical case of a solitary Peutz-Jeghers type polyp of the stomach accompanying a lymph node enlargement and ectopic pancreas in the jejunum that simulates stomach cancer with lymph node metastases.
Keywords: Peutz-Jeghers type polyp, Submucosa lesion, Stomach cancer, Ectopic pancreas, Endoscopic ultrasonography
INTRODUCTION
A solitary Peutz-Jeghers type polyp of the stomach is rare[1-4] and most cases are associated with mucocutaneous pigmentation and multiple intestinal polyposis[5,6]. Peutz-Jeghers type polyposes occur mainly in the small intestine, colon, and stomach, and these hamartomatous polyps are characterized by hyperplastic epithelia and by the proliferation of smooth muscle bundles around the mucosal glands[5]. We here report a case of a woman who had a rare solitary gastric Peutz-Jeghers type polyp of the stomach that mimicked gastric cancer with lymph node metastases.
CASE REPORT
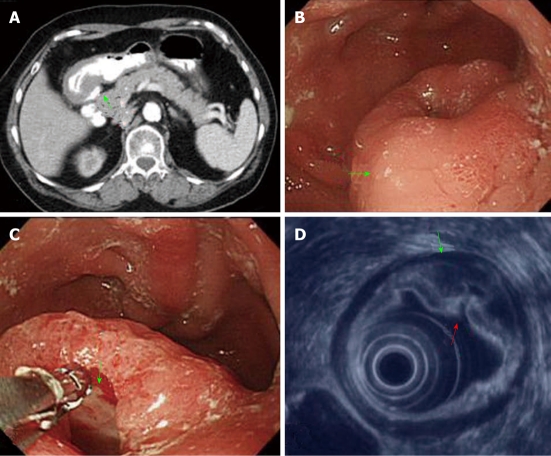
A 71-year-old woman presented at our hospital with an extremely rare case of a solitary gastric Peutz-Jeghers type polyp of the stomach. This patient had experienced intolerable epigastric pain over the previous two months and also 5 kg of weight loss during this time. She attended the emergency room and was subsequently admitted to the hospital to receive treatment for pain. During her hospitalization, emergency computed tomography (CT) scans of the abdomen were performed and revealed a thickened gastric wall in the antrum (Figure 1A). Three enlarged lymph nodes greater than 1 cm were also detected. The CT report thus indicated a diagnosis of gastric cancer with lymph node metastases.
Figure 1.
Image findings of gastric Peutz-Jeghers type stomach polyp. A: Abdominal computed tomography scans of the patient revealing a thickened gastric wall over the antrum of the stomach (arrow); B: Gastroendoscopy revealing a bulging lesion (4 cm × 3 cm) of the antrum (arrow); C: The bulging lesion displayed a central hole (arrow); D: Endoscopic ultrasonography demonstrating that the appearance of a lesion was due to a thickened subepithelial layer (second layer lesion), submucosal layer thickened (third layer, green arrow), and corresponding hole (red arrow) over the antrum of the stomach.
A gastroduodenoscopy was also performed and showed a bulging gastric lesion of 4 cm × 3 cm with a central hole (Figure 1B and C), in addition to an asymmetrical wall thickness and narrowing of gastric lumen in the antrum. A gastric biopsy revealed ulceration with moderate dysplasia of the mucosal glands. The patient’s pain was not relieved by antacids. Further studies via endoscopic ultrasonography showed the presence of a subepithelial lesion of 4 cm × 3 cm with a central hole (Figure 1D).
The patient additionally underwent a diagnostic endoscopic mucosectomy (EMR), and a gastric specimen measuring 1.3 cm × 0.9 cm × 0.2 cm was thereby obtained. The subsequent pathology report identified this specimen as a hamartomatous polyp with proliferation of smooth muscle bundles in the submucosal layer and hyperplastic glands in the mucosal layer. Because the results of the clinical examination and pathology were conflicting, a clinical diagnosis of malignant gastric cancer with lymph node metastases was made. The patient then underwent a subtotal gastrectomy. An additional lesion measuring 2 cm × 2 cm × 1 cm was noted in the submucosa of the jejunum during this surgery. Partial resection of the lesion in the jejunum was thus performed and the specimens were sent for pathological examination.
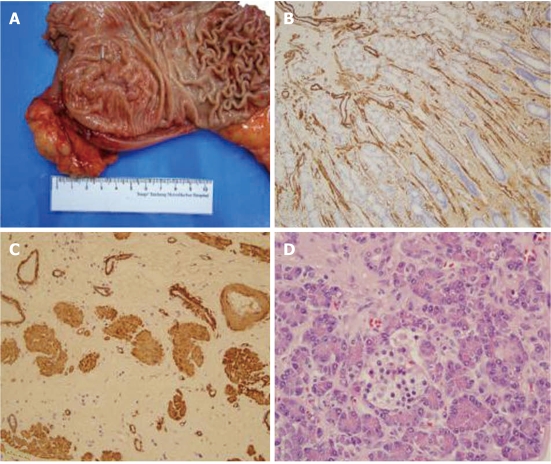
Gross examination of the lesion revealed a 4 cm × 3 cm polypoid tumor, with a central ulceration over the antrum of the stomach after diagnostic endoscopic mucosectomy (Figure 2A). Seventeen lymph nodes were dissected from the perigastric region measuring up to 1.2 cm in diameter. A submucosal lesion measuring 2 cm × 2 cm × 1 cm was also noted in the jejunum region. Histopathological examination of the lesion that had been diagnosed as a hamartomatous polyp of the stomach revealed a characteristic cell growth that increased the thickness of the mucosal glands to a maximum of about 9 mm and of the muscularis propria to 11 mm (Table 1). Smooth muscle bundles were found to be interspersed around the glands (Figure 2B), and smooth muscle bundles were observed to have proliferated over the submucosal layer (Figure 2C).
Figure 2.
Pathological findings of gastric Peutz-Jeghers type stomach polyp. A: Gross examination of a stomach specimen from the patient showed a polyp-like lesion (4 cm × 3 cm) over the antrum following endoscopic mucosectomy; B: Immunohistochemical stains of smooth muscle actin in the mucosal layer revealed a proliferation of smooth muscle bundles (× 200); C: Submucosal layer of the lesion revealed a proliferation of smooth muscle bundles (× 200); D: Photomicrogram demonstrating the presence of an ectopic pancreas in the submucosa of the jejunum and of pancreatic ducts, acini and islet cells (hematoxylin and eosine staining, original magnification × 200).
Table 1.
Comparison between the clinical findings of the current case and the normal characteristics of gastric antrum tissue
| Patient | Normal (n = 3) | |
| Mucosa layer (mm) | 5-9 | 3-5 |
| Smooth muscle bundles | Diffuse increase | Focal few |
| Muscularis mucosa (μm) | 10-30 | 10-30 |
| Submucosal layer (mm) | 3-5 | 3-5 |
| Diffuse increase | Smooth muscle bundles | none |
| Muscle propria (mm) | 5-11 | 5-7 |
The 17 dissected lymph nodes showed reactive hyperplasia without tumor metastasis. The jejunum lesion contained ectopic pancreatic tissue with ducts, acini and islet cells, with interspersed smooth muscle bundles (Figure 2D). Immunohistochemical staining revealed strong cytoplasmic signals for smooth muscle actin between the mucosal glands (Figure 2B) and the submucosal layer (Figure 2C). A gastrointestinal stromal tumor was ruled out by negative staining for c-Kit (c-Kit pharmDx™; Dako Corporation, Glostrup, Denmark). The final pathological determination was a gastric Peutz-Jephers type polyp and jejunal ectopic pancreas. This is therefore the first reported case of a solitary Peutz-Jeghers type polyp of the stomach that presented with clinical signs mimicking a stomach cancer with lymph node metastases.
DISCUSSION
A solitary Peutz-Jeghers type polyp of the stomach is found in fewer than 0.1% of all endoscopic examinations[5]. Bartholomew et al[5] have previously observed that polyps are present in the stomach in only 24% of cases of Peutz-Jeghers syndrome associated with intestinal polyposis, mainly in the small intestine. Moreover, only 27 cases of gastric solitary hamartomatous polyps have been reported thus far in the literature. The predominant components of hamartomas are hyperplastic mucosal glands and smooth muscle bundles in the mucosal layer[1-4]. Some authors have concluded that solitary Peutz-Jeghers type polyps are histologically identical to those in Peutz-Jeghers syndrome[4]. In contrast, other investigators have suggested that solitary Peutz-Jeghers type polyps of the stomach have less branching of the muscularis mucosae than those of the familial form[3]. Our current case demonstrated extensive branching of the muscularis mucosae to the mucosal layer that also extended to the submucosal layers. This distinct finding of a proliferation of smooth muscle bundles in the submucosal layer has not been previously reported.
Gastric hamartomatous polyps are usually asymptomatic, and most cases are found incidentally during a routine gastric endoscopy. Few previous cases have presented with intestinal obstruction or anemia due to chronic blood loss, or were found to be accompanied by a transformation to adenocarcinoma[6-9]. Our patient presented with intolerable epigastric pain and weight loss of 5 kg during the two months prior to admission to our hospital. CT scans of this patient’s abdomen revealed three enlarged lymph nodes, all of which measured more than 1 cm. In addition, a submucosal lesion over the jejunum was noted. Our patient showed extensive proliferation of smooth muscle bundles in the submucosal layer, which gave the gastric lesion the appearance of a submucosal tumor. These characteristics thus need to be differentiated from those of a submucosal gastrointestinal stromal tumor (GIST). A diagnosis of gastric GIST was ruled out in our current case by negative c-Kit (CD117) staining.
In conclusion, this is the first reported case of a solitary Peutz-Jeghers type polyp that was associated with symptoms mimicking a gastric tumor with lymph node metastases. In addition, the association of an ectopic pancreas with solitary Peutz-Jeghers type polyp of stomach has also not been reported previously.
Footnotes
Peer reviewer: Philip H Gordon, Professor, McGill University, 3755 Cote Ste. Catherine Road, Suite G304, Montreal H3T 1E2, Canada
S- Editor Gou SX L- Editor A E- Editor Xiong L
References
- 1.Sakadamis AK, Ballas KD, Fardellas JG, Papanikolaou A. A solitary gastric Peutz-Jeghers type polyp: report of a case. Surg Today. 2001;31:517–520. doi: 10.1007/s005950170113. [DOI] [PubMed] [Google Scholar]
- 2.Tatsuta M, Okuda S, Tamura H, Taniguchi H. Gastric hamartomatous polyps in the absence of familial polyposis coli. Cancer. 1980;45:818–823. doi: 10.1002/1097-0142(19800215)45:4<818::aid-cncr2820450435>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 3.Kuwano H, Takano H, Sugimachi K. Solitary Peutz-Jeghers type polyp of the stomach in the absence of familial polyposis coli in a teenage boy. Endoscopy. 1989;21:188–190. doi: 10.1055/s-2007-1012939. [DOI] [PubMed] [Google Scholar]
- 4.Grisendi A, Lonardo A. Solitary Peutz-Jeghers type polyp of the stomach. Endoscopy. 1990;22:153. doi: 10.1055/s-2007-1012826. [DOI] [PubMed] [Google Scholar]
- 5.Bartholomew LG, Moore CE, Dahlin DC, Waugh JM. Intestinal polyposis associated with mucocutaneous pigmentation. Surg Gynecol Obstet. 1962;115:1–11. [PubMed] [Google Scholar]
- 6.Hunt J, Tindal D. Solitary gastric Peutz-Jeghers polyp and angiolipoma presenting as acute haemorrhage. Aust N Z J Surg. 1996;66:713–715. doi: 10.1111/j.1445-2197.1996.tb00724.x. [DOI] [PubMed] [Google Scholar]
- 7.Sipponen P, Siurala M. Cystic “hamartomatous” epithelial polyps of the stomach. Acta Hepatogastroenterol (Stuttg) 1978;25:380–383. [PubMed] [Google Scholar]
- 8.Sato T, Sakai Y, Ishiguro S, Fujita M, Kuriyama K, Narumi Y. Gastric hamartomatous polyp without polyposis coli: radiologic diagnosis. Gastrointest Radiol. 1988;13:19–23. doi: 10.1007/BF01889016. [DOI] [PubMed] [Google Scholar]
- 9.Aoki M, Yoshida M, Saikawa Y, Otani Y, Kubota T, Kumai K, Wakabayashi G, Omori T, Mukai M, Kitajima M. Diagnosis and treatment of a gastric hamartomatous inverted polyp: report of a case. Surg Today. 2004;34:532–536. doi: 10.1007/s00595-004-2761-1. [DOI] [PubMed] [Google Scholar]