Abstract
The loss of an eye is the most devastating, psychologically damaging experience for a patient. All hope to bring such patients back to their accustomed and comfortable life-style rests on a cosmetically acceptable prosthesis. An intra-orbital ocular prosthesis serves the purpose in those defects where the orbital margins are intact. Though the stock eye may match the natural eye’s iris and sclera in color, the fit of the prosthesis to the tissue bed may not be as good as desired. Herein, a functional ocular impression technique is presented to achieve a better fit of the prosthesis to the defect area. This technique aims to combine cosmetic excellence with comfort for greater benefit to the patient.
Keywords: Impression technique, Ocular prosthesis, Maxillo-facial prosthesis, Body temperature wax
Introduction
The eye is a vital organ in terms of vision and is also an important component of facial expression. A significant number of people sadly acquire facial defects as a result of malignancy, trauma and congenital deformities each year. While modern plastic surgery techniques can help repair and restore some lost tissue, they cannot however, completely replace the lost tissue or organ in such a way that it creates an illusion of the lost organ or mimic a normal/near normal appearance of the same.
Such disfigurement has a crippling effect on the personality of the individual who is desperately in need of help. Prosthetic rehabilitation may probably be the only alternative available to such patients to help restore their confidence and self-esteem. Although implant eye prosthesis has a superior outcome, economic reasons may make it inaccessible to many patients.
The prime requisites of eye prosthesis include a convincingly normal appearance and more significantly a comfortable fit which will motivate the patient to use the prosthesis.
This article describes the use of a functional impression technique for an ocular prosthesis for a 10 year old child who lost an eye due to malignancy (Fig. 1).
Fig. 1.
Pre-treatment photograph of child
Review of Literature
Early records indicate that artificial eyes, ears and nose were found on Egyptian mummies. The Chinese Physicians aided by sculptors and painters also made facial restorations with waxes and resins. Ambrose Pare (1510–1590), one of the pioneers of maxillo-facial prosthetics is said to have used glass and porcelain eyes for eye prosthesis [1].
Various materials and techniques have been used to get an accurate impression of the orbital defect. Benson [2] coated a steel ball of size similar to the socket, covered it with base plate wax and modified it to achieve the desired impression of the tissue bed.
Irreversible hydrocolloid can be used with many techniques. Barlett and Moore [3], Taylor [4] and Welden and Nilranen [5] suggested alginate material as the impression material of choice. Allen and Webster [6], Cain [7], Brown [8] etc. recommended using ophthalmic alginate for making the impression.
Sykes [9] used medium viscosity polyvinyl siloxane impression material. Ow and Amrith [10] advocated the use of tissue conditioners as a reline material because of its biocompatibility and ease of manipulation.
Schneider [11] suggested modifying the wax conformer with body temperature Iowa impression wax. Smith [12] described a reline procedure for an existing ocular prosthesis using Korrecta wax no: 4.
Materials and Method
Materials used were:
Alginate—Plastalgin, Septodont, France
Light body elastomeric impression material—Aquasil Ultra LV, Dentsply, USA
Dental stone—Denstone, Pankaj Enterprises M.P.
Eye shell
Modeling wax—Link, MDM Corp. Delhi
Body temperature wax/Corrective imp. Wax-M.P. Sai Enterprise, Mumbai
Heat cured Acrylic resin—DPI Heat Cure, Mumbai
Method
A complete medical and dental history was elicited. The resected area was examined to determine the extent of defect and post-operative healing. All the routine investigations including a “patch test” for acrylic were done. The procedure and its drawbacks were explained to the patient to determine the motivation of the patient towards the treatment.
An eye shell of appropriate size and shape was selected and tried in the defect.
The inter-pupillary distance was measured and the vertical and horizontal axes were established to orient the prosthesis accurately.
Necessary modification in size, shape and color of eye shell were made.
A special tray in acrylic with a hollow handle to serve as inlet for the impression material was made (Fig. 2). Patient was asked to perform all the functional movements by the normal eye which helped in activating the muscles of the defect as the light bodied elastomer was injected.
Elastomeric impression of the affected area was made and a cast poured in dental stone—two piece gypsum mold (Fig. 3).
A separating medium was applied to the cast; wax was filled in the mould and the prepared eye shell was fixed in position.
This waxed eye shell was tried in the patient’s ocular defect and necessary modifications were made in the position and orientation.
Once approved by patient, 2 mm of the intaglio side of the wax model was removed, body temperature wax was applied to it and it was seated back on the cast.
The inter-pupillary distance was measured and the vertical and horizontal axes were established to orient the prosthesis accurately.
This new wax-up eye shell was seated in the defect and the patient was recalled the next day to allow the prosthesis wax to be completely molded to the defect and movements of the extra ocular muscles.
After rechecking the position of the prosthesis, this wax model was acrylised in a special dental flask.
The final prosthesis was finished as necessary and polished well.
The finished prosthesis was then seated into the defect, rechecking for fit, accuracy of position of eye-piece and comfort (Fig. 4).
Fig. 2.
Special tray with hollow handle
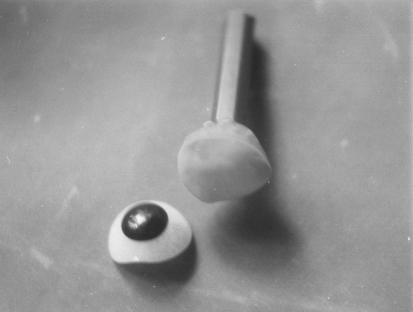
Fig. 3.
Impression made by the light body elastomeric imp. material
Fig. 4.
Photograph of child with the prosthesis
Discussion
The most important objectives of maxillo-facial prosthetics and rehabilitation include:
Restoration of esthetics and cosmetic appearance.
Restoration of function (where applicable).
Protection of tissues.
Therapeutic/healing effect of prosthesis.
Psychological therapy.
The eye prosthesis delivered in this case fulfilled all the above objectives. A well-made and properly planned ocular prosthesis maintains its orientation when patient performs various movements. With the development of newer materials and altered impression techniques the socket can be recorded in full detail on which custom made ocular acrylic prosthesis can be fabricated with accurate fit and esthetics.
The special tray can easily be made with an alginate impression of the selected and modified eye shell and a cylindrical hollow inlet made out of a used pen provides an easy, economical and effective way to make a custom tray for the defect. Thus we get a custom tray individualized for the patient to make an impression of the defect.
Irreversible hydrocolloid has been the material of choice for making an impression of the socket. Its advantage is that it is easy to use, readily available and gives an accurate impression of the full functional anatomic space within the defect. However a light body elastomeric impression material provides an accurate and dimensionally stable impression of the defect which can be poured multiple times and stored over a period of time.
The impression was further refined by the body temperature wax used providing a much closer adaptation of the prosthesis to the tissues. This also provided the patient with a trial prosthesis to be assessed over a period of time in presence of relatives and friends in a more comfortable family environment.
Artificial acrylic resin (PMMA) eyes are preferred to artificial glass eyes because of the following reasons:
There is freedom from fragility and surface etching resulting from dissolution by the socket secretions.
Adjustability to size and form is more easily accomplished to compensate for socket irregularities.
An intra-orbital prosthesis is technically simpler than an extra-orbital prosthesis as the orbital margins are not lost following surgery, so that the prosthesis is retained within the defect and by the eye lids. In this case, the improvement in esthetics contributed greatly to the physical well being and mental attitude of the patient. Patients must be encouraged to report for orbital prosthesis at least within 6–8 weeks following surgery on that prosthetic eye can be made during the healing period.
Conclusion
The tremendous psychological boost and enhanced esthetics provided by a maxillofacial prosthesis cannot be understated. The above method describes a simple and effective way to making a well-fitting ocular prosthesis. The reward for being able to help such an unfortunate patient is immense for a maxillo-facial prosthodontist.
Acknowledgment
I wish to thank my teachers Prof. Dr. Chandrasekharan Nair, Prof. Dr. Suresh Meshram and Prof. Dr. Sabita Ram for their constant support and guidance.
Footnotes
Clinical Relevance
Cosmetics, accuracy of fit, patient comfort and compliance relies greatly on an accurate impression of the underlying mobile tissues that will support the prosthesis.
Contributor Information
Jitendra Jethwani, Email: jitendrajethwani@yahoo.com.
Gayathri S. Jethwani, Email: gayathri_jethwani@yahoo.co.in
A. K. Verma, Email: drakverma30@yahoo.com
References
- 1.Erpt SF. Comparative features of plastic and/or glass in artificial eye construction. Areb Opthalmol. 1953;50:737. doi: 10.1001/archopht.1953.00920030748009. [DOI] [PubMed] [Google Scholar]
- 2.Benson P. The filing and fabrication of a custom resin artificial eye. J Prosthet Dent. 1977;38:532. doi: 10.1016/0022-3913(77)90029-4. [DOI] [PubMed] [Google Scholar]
- 3.Barlett SO, Moore DJ. Ocular prosthesis: a physiologic system. J Prosthet Dent. 1973;29:450–459. doi: 10.1016/S0022-3913(73)80024-1. [DOI] [PubMed] [Google Scholar]
- 4.Taylor TD. Clinical maxillofacial prosthetics. Chicago: Quintessence Publishing; 2000. pp. 76–265. [Google Scholar]
- 5.Welden RB, Niraanen JV. Ocular prosthesis. J Prosthet Dent. 1956;6:272–278. doi: 10.1016/0022-3913(56)90120-2. [DOI] [Google Scholar]
- 6.Allen L, Webster HE. Modified impression method of artificial eye fitting. Am J Opthalmol. 1969;67:189–218. doi: 10.1016/0002-9394(69)93148-1. [DOI] [PubMed] [Google Scholar]
- 7.Cain JR. Custom ocular prosthesis. J Prosthet Dent. 1982;48:690–694. doi: 10.1016/S0022-3913(82)80030-9. [DOI] [PubMed] [Google Scholar]
- 8.Brown KE. Fabrication of an ocular prosthesis. J Prosthet Dent. 1970;24:225–235. doi: 10.1016/0022-3913(70)90149-6. [DOI] [PubMed] [Google Scholar]
- 9.Sykes LM. Custom made ocular prosthesis: a clinical report. J Prosthet Dent. 1996;75:1–3. doi: 10.1016/S0022-3913(96)90409-6. [DOI] [PubMed] [Google Scholar]
- 10.Ow RK, Amrith S. Ocular prosthetics: use of a tissue conditioner material to modify a stock ocular prosthesis. J Prosthet Dent. 1997;78:218–222. doi: 10.1016/S0022-3913(97)70129-X. [DOI] [PubMed] [Google Scholar]
- 11.Schneider RL. Modified ocular prosthesis impression technique. J Prosthet Dent. 1986;55:482. doi: 10.1016/0022-3913(86)90182-4. [DOI] [PubMed] [Google Scholar]
- 12.Smith RM. Relining an ocular prosthesis: a case report. J Prosthodont. 1995;4:160–163. doi: 10.1111/j.1532-849X.1995.tb00333.x. [DOI] [PubMed] [Google Scholar]