Abstract
In 2004, community health became the 4th mission of the University of Rochester Medical Center, along with education, clinical care, and research. In that same year, a novel clerkship was added to the 4th-year curriculum that focuses on the “practice” of community health and preventive medicine. The goal is to offer intensive experiential training to develop skills in community health improvement by partnering with community agencies involved in health promotion and disease prevention. The learning objectives addressed include: community health assessment, risk behavior change, assurance of personal health services, advocacy and policy change, environmental interventions, community organization and partnership-building, and program evaluation. The clerkship involves 3 full days of didactic instruction, followed by 4 weeks of program development and implementation. Each student chooses a project that focuses on a specific target population, then designs it and incorporates public health knowledge, skills, and attitudes learned during the didactic component. Course directors then mentor students during project implementation. Students can begin “longitudinal” experiences in their first or second years to fold into the required clerkship. Innovations include a novel “Advocacy and Policy Change” module and a highly rated “Cultural Determinants of Health” lecture, and a resource-based course website. The clerkship was initially offered as an elective, and has since become a required course. In the clerkship to date, three hundred and forty students have launched hundreds of community-level interventions within various settings locally, nationally, and internationally. Evaluation efforts to date indicate the clerkship has been received favorably by both faculty and students.
Historically, clerkships have been the fundamental means by which medical students learn and practice the skills required of a physician, including information gathering, therapeutic planning, and interventions. The experiential learning and formative feedback from preceptors in clerkships are an effective means of teaching and learning procedural skills in undergraduate medical education, but rarely expand the skills from the level of the individual patient to that of the community 1-3. However, such an expansion has been recommended by serious entities. The World Health Organization, for example, has recommended changes in medical education that emphasize public health and preventive medicine training 4. The Pew Health Professions Commission has challenged health professions schools to ensure that their students are competent in community-based care 5, 6. At the same time, the Association of American Medical Colleges, in its Medical School Objectives Report (MSOP) has made several recommendations for educational outcomes, among which is cultivating physicians who are dutiful and who “collaborate and use systematic approaches for promoting, maintaining, and improving the health of individuals and populations” 7. Future physicians are expected not only to be adept clinicians, but also to understand and work within the family, community, and cultural contexts in which their patients live.
Medical students cannot acquire these insights and skills through didactic learning alone, but when didactic learning about population health is combined with the practical experience offered in typical clinical clerkships (e.g., in medicine, pediatrics, etc.), they can learn how to apply prevention knowledge in real-life settings. Yet such clerkships blending population health knowledge with practical experience are seldom offered and rarely required, indicating a paucity of opportunities and protected time for experiential learning of community health skills. Illustrating this problem, 32.1% of graduating medical students in 2006 reported that inadequate time during medical school was devoted to the role of community health and social service agencies, 32.1% noted this for public health, 21.4% for community medicine, 19.5% for clinical epidemiology, and 14.3% for health promotion and disease prevention 8. In addition, a large proportion of students reported that inadequate time during medical school was devoted to health policy, health services financing, environmental health, global health issues, biological/chemical terrorism, and disaster management.
Many different clinical and basic science disciplines should share responsibility and commitment for education in community health 7. Such education is inherently collaborative and requires the involvement of multiple disciplines. The intended outcome, as reported in the MSOP, is that “a population health perspective encompasses the ability to assess the health needs of a specific population, implement and evaluate interventions to improve the health of that population, and provide care for individual patients in the context of the culture, health status, and health needs of the populations of which that patient is a member 7.” Many health professions schools are developing programs to address issues of population-based health and interdisciplinary teamwork while providing students with community-based experiences and a broader understanding of the social and cultural milieu of health and disease 9-14. Many of these community-based programs have emphasized prevention at the clinical and individual level in order to provide students with experience in community-oriented primary care and, particularly, in underserved rural and urban communities 15, 16. Fewer programs have addressed the social and environmental factors that contribute to the excess burden of disease and disability in these communities. The University of Rochester School of Medicine and Dentistry (URSMD) decided to create a novel clerkship to address these gaps in medical education.
In this article we describe the development of a community health improvement clerkship, which specifically addresses the need for medical students to review population science concepts, hone social group interaction skills rather than individual-level interaction skills, and apply knowledge and expertise in a practical setting. We will describe the development of this clerkship, its current content and operation, and some early evaluation results.
The most important anticipated outcome from this clerkship is physicians who will actively incorporate community health principles and practice in their future careers as health care leaders. We also hope for improved health in underserved, underrepresented populations, enhanced multidisciplinary collaboration in health prevention, and an increased number of medical students who decide to pursue careers that formally integrate population health research and practice.
Creating the Community Health Improvement Clerkship
In 1998, URSMD completely revised and updated its curriculum, creating the Double Helix Curriculum, a practice-based learning oriented educational program that emphasizes integration of basic science and clinical medicine across the spectrum of Engel’s Biopsychosocial model 17. As part of this integrated approach, previous courses in epidemiology, biostatistics, and community medicine in Years I and II were replaced by a single four-week course in epidemiology, biostatistics, and evidence-based medicine (titled Mastering Medical Information) that initiates Year I. Although this course was designed to improve preventive medicine and epidemiology knowledge in URSMD students, additional preventive medicine instruction was required as part of the ambulatory medicine curriculum. Yet, after two years or so, it was clear that the principles and practice of community health were lacking in the curriculum despite the Biopsychosocial Model’s inclusion of community, culture, society, and biosphere as important determinants of the patient’s health 17. Several models to rectify this deficiency were considered, including an elective community health improvement course offered to undergraduate nursing and medical students that emphasized experimental learning 18. However, the few medical students who participated in the elective course chose to do so before their 4th year, prior to their primary clinical experiences in which they would have the opportunity to apply this knowledge in a practical setting. A multidisciplinary curriculum design team then set out to create a medical student clerkship which emphasized interactions in social groups rather than in individuals through supervised experiences in community agencies supported by didactic learning sessions 19, 20. The Community Health Improvement Clerkship (CHIC) was created for fourth-year medical students and for its first two years (2002, 2003) was offered as an elective. It has, since 2004, been required for the MD degree at URSMD.
Goals
The overarching goal of CHIC is for students to learn how to improve the health of a target community through community-based interventions directed at a significant health issue. The specific learning objectives of the clerkship are community health assessment, community risk behavior change, assurance of personal health services, environmental change, health disparities and cultural determinants of health, community organization and partnership building, advocacy and policy change, and program evaluation (Table 1).
Table 1.
Learning Objectives in the Community Health Improvement Clerkship with Examples and Resources Used by Medical Students
| Learning objective | Community health examples | Resources for medical students |
|---|---|---|
| Community health assessment | Interpret population-based surveillance data |
Lectures, online databases, health departments (county and state) |
| Community behavior change | Provide health education for diet and physical activity, referrals to free smoking cessation resources |
Lectures, online modules, previous student projects, health departments |
| Assurance of personal health services |
Offer health screenings, vaccinations |
Health departments, “voluntary” health agencies (e.g., American Cancer Society) |
| Environmental change | Include healthy choices in vending machines, make homes free of lead exposure |
Lectures, online modules, health departments |
| Health disparities and cultural determinants of health |
Evaluate the impact of personal demographics on health care- seeking behaviors |
Lectures, neighborhood associations, social service agencies, health departments |
| Advocacy and policy change | Facilitate clean indoor air laws and mandatory lead assessments for housing |
Lectures, workshop, advocacy events, online modules, health departments |
| Community organization and partnership building |
Work within health department programs, voluntary health agencies, faith-based and other community organizations, worksites |
Lectures, online modules, previous student projects, course director contacts and mentoring |
| Program evaluation | Conduct formative, process, outcome, and impact evaluation |
Lectures, faculty mentoring, interdisciplinary academic departments |
Design
CHIC, after 2 years as an elective, is now a required fourth-year clerkship at URSMD. Students can take this clerkship either as a 4-week intensive experience or as a culminating longitudinal experience with community health improvement activities across all 4 years. By January of their first year, students must declare their intention to pursue this longitudinal track. The longitudinal track helps to structure and focus the community health-related activities of the students who choose this option. In addition to participating in community health-related activities across the four years of medical school, students who choose this track also receive didactic instruction and resources through online modules. Although the instruction provided in the online modules is not as intensive as the didactic instruction they receive in the 4-week clerkship during their 4th year (which they attend along with the rest of the 4th year students), the students on the longitudinal track are prepared with the requisite knowledge, attitudes, and skills necessary to assume the role of the physician as more than a practitioner in a one-to-one patient-physician relationship. Rather, they develop skills that allow them to assume the role of a population-based health facilitator focusing on the one-to-many physician–group relationship to help effect positive changes in health on a broader scale 21. Students in the longitudinal track complete evaluations of the online modules along the way (allowing us to track their mastery of the material), and we track all students during the 4th year CHIC through attendance at lectures, progress notes, module evaluations, and final papers. Students who complete the longitudinal track are considered for receiving the honor of Distinction in Community Service, which is explained below.
During the 4th year 4-week CHIC, students participate in didactic and interactive lectures delivered by faculty from a variety of disciplines and representatives from local agencies for the first three days of the clerkship, read through supplemental online didactic modules, and then spend the rest of their four weeks developing and implementing community health projects. Students are encouraged to build off of projects previously begun by past or current CHIC students, encouraging the ongoing sustainability of projects and partnerships that are beneficial to a target community. The CHIC project is meant to challenge students to think beyond the comfort zone of their perception of the world of health care to see how community-level approaches can affect health on a larger scale than what they have typically encountered in one-to-one care.
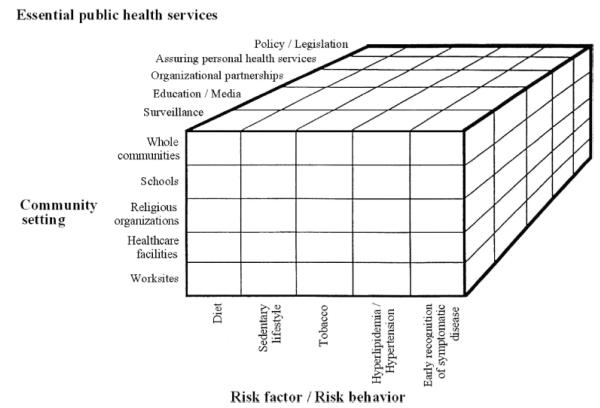
To focus the students’ projects appropriately, we encourage them to use a model for conceptualizing community interventions that requires them to identify three dimensions: 1) behaviors targeted for change; 2) community settings for interventions; and 3) interventions (services) to change behaviors. Framing their projects around these three dimensions helps students identify the specific behaviors which are important determinants of a health problem of interest, such as cardiovascular health (Figure 1). Since an interventionist can become quickly overwhelmed by the complexity of issues that are a threat to community health, it is helpful to focus project efforts on one behavior, one community setting, and one intervention. A community service project can then be quickly conceptualized on such a three-dimensional “grid”. A cardiovascular health project, for example, could include reducing smoking among teens (the target behavior for change) in local schools (the community setting) by offering free smoking cessation classes (the actual intervention).
Figure 1.
Illustration of the three-dimensional approach to community service programs required of medical students in the Community Health Improvement Clerkship at the University of Rochester School of Medicine and Dentistry, Rochester, New York. This example considers the three dimensions of public health services, community setting, and risk factors relating to cardiovascular health.
Source: Pearson TA, Wall S, Lewis C, Jenkins PL, Nafziger A, Weinehall L. Dissecting the “black box” of community intervention: Lessons from community-wide cardiovascular disease prevention programs in the US and Sweden. Scand J Public Health Suppl. 2001;56:69–78. Reproduced with permission.
Students engaging in local community-based projects have access to office space and computers (provided by our Department of Community and Preventive Medicine) which are located within a specific target community in the inner city of Rochester. Although this target community is only one of many of our sites in the metropolitan area, this office space was chosen for its accessibility to key community partners. The office space is located within the same building as an elementary school, a neighborhood action coalition, a dental center, and a community health center. Information on these agencies and their relation to CHIC are provided to the students to consider during their project planning. Although students can engage with projects in other local, national, and global communities, this unique setting facilitates ample opportunities for a wide variety of projects, and allows for the “sustainability” of long-term projects 19. It also fosters long-term relationships between URSMD and specific community agencies and members.
Curriculum Elements
Didactic lectures
The CHIC has approximately 10 organized lectures (the didactic component of the clerkship) given by faculty, organization representatives, and guest lecturers during the first 3 days of the clerkship (Table 2). Some of the content refreshes information from Year I and II courses, but most is new material.
Table 2.
Lecture Schedule for the Community Health Improvement Clerkship at the University of Rochester School of Medicine and Dentistry, Rochester, New York
| Format | Title | Description |
|---|---|---|
| Day 1 | ||
| Lecture | Introduction | Learning objectives, clerkship requirements, examples, community partners, and current opportunities |
| Lectures | Community health models |
Role and essential elements of community health programs and population-based medicine |
| Lecture | Chronic care model | Chronic care model of preventive medicine |
| Day 2 | ||
| Lectures | Health disparities and cultural determinants of health |
Impact of culturally-determined factors at the personal, provider, health-care system, and societal levels exemplified by specific cases |
| Lecture | Emergency preparedness | Short-term and long-term impact of local community health crises |
| Presentations | Partnership-building | Local, regional, and national partnership-based programs and opportunities, from American Cancer Society and American Heart Association |
| Day 3 | ||
| Lecture | Community health assessment |
Historical and current methods of surveillance data in identifying the prevalence and impact of community-level health issues |
| Workshop | Advocacy and policy change |
Mock legislative lobbying effort to impact public health policy, with legislators and public health officials role- playing policy-makers |
| Workshop | Program evaluation | Needs assessments, formative evaluation, process evaluation, outcome evaluation, and impact evaluation concepts tailored to specific student projects |
Several novel lectures and workshops have been successfully introduced. One example is a session about advocacy and policy change. An online module was developed and published 22 that describes advocacy and policy change as they relate to the roles physicians could play in affecting public health policy. A workshop during the didactic portion of the clerkship brings in a local policy-maker (e.g., county legislative representative, health department director, city mayor) for an interactive role-play. In the lecture, the students are taught specific “lobbying” techniques, and a fictional health policy issue is presented (e.g., state law regarding mandatory colorectal cancer screening, indoor-air tobacco control laws, etc.). After strategizing, students are taken to another room where they play various roles (doctor, cancer survivor, stakeholder, etc.) in a mock legislative lobbying activity with the guest policy-maker. After the role-play, a debriefing with the policy-maker reviews how “successful” the students’ lobbying event was (i.e., how well they used persuasive tactics, medical information, surveillance data, etc.), and incorporates real-life examples to further emphasize the roles that physicians can play in affecting policy changes.
Faculty from a variety of academic departments contribute to the lectures, serve as ad-hoc preceptors for specific projects, and are generally available to serve as mentors. In this way, one-on-one expertise is available from a wide variety of disciplines, such as Medicine, Preventive Medicine, Epidemiology, Psychology, Psychiatry, Anthropology, Environmental Health, Biostatistics and Ethics.
Community-based projects
Since its inception in 2002, CHIC has resulted in over 190 unique community health improvement projects. Through development and implementation of feasible short- and long-term projects (sustainable by involving new students across time), students learn how to assess and address common community health problems including, but not limited to lead poisoning, pediatric obesity, smoking, disparities in access to health care, violence and conflict, cancer, cardiovascular disease, diabetes, and injury risks (Table 3).
Table 3.
Past Projects by Topic Completed by Medical Students in the Community Health Improvement Clerkship at the University of Rochester School of Medicine and Dentistry, Rochester, New York.
| Topic | Total |
|---|---|
| Chronic diseases/conditions | |
| Obesity | 41 |
| Lead/toxins | 15 |
| Cardiovascular disease & hypertension | 26 |
| Smoking | 15 |
| Nutrition | 46 |
| Diabetes | 12 |
| Cancer | 15 |
| Asthma | 2 |
| Alcohol | 17 |
| Osteoporosis | 4 |
| Blindness | 5 |
| HIV | 5 |
| Huntington’s disease | 3 |
| Suicide/depression | 9 |
| Mental health | 5 |
| Organ donation | 2 |
| Total papers* | 126 |
| Acute diseases / conditions | |
| Pneumonia | 4 |
| Stroke | 8 |
| Accidental injury | 7 |
| Automated External Defibrillators | 4 |
| Influenza | 2 |
| Total papers* | 20 |
| Other themes | |
| Pediatric | 84 |
| Elderly | 22 |
| African American | 33 |
| Hispanic | 33 |
| Medicare/Medicaid/uninsured | 37 |
| Violence and abuse | 10 |
| Physical fitness/sports | 35 |
| Online interventions | 7 |
| TV/media | 4 |
| Total papers* | 165 |
Note: one student project can cover multiple topics. Within a subgroup, each project was counted only once, regardless of the number of topics covered.
Projects that are longitudinal (carried out over time by one or more students and/or picked up by subsequent students where previous students have left off) are seen as “sustainable” and, therefore, beneficial to a target community because of the multiple opportunities over time to address a particular issue, and the additional opportunities for evaluating the intervention’s long-term impact on health behaviors. These benefits may not always be evident when there are gaps of months or years between student projects addressing a specific intervention, but our goal is at least to have the curriculum structure in place to encourage and carry out such sustainable projects. For example, a series of students developed and implemented in a specific urban area of Rochester conflict resolution workshops, which identified youth violence as an ongoing determinant of injuries and accidental death. The notion of “sustainability” may not have been evident to the target community, who experienced these interventions at unpredictable times over a period of several years. However, subsequent students were able to carefully review and build upon previous student projects to improve the workshops each time in terms of faster connection with key community contacts, refined needs assessments, improved workshop content, and increasingly successful community outreach strategies. The result is a developed intervention that is an ongoing resource available to our local target community.
Project examples
Project 1 (1 month clerkship)
A recent student developed an educational video for lay audiences in target populations at risk for head injury. By partnering with various medical school departments, a local public TV station, and community-based groups, the student created a high-quality video education program for the prevention of traumatic brain injury. The half-hour program highlights a case example of a young boy with traumatic brain injury suffered while riding his skateboard without a helmet. Interviews with the family and members of the health care team who worked with the child present a strong message about the importance of preventing head injuries. The video is available for local and national broadcasting and for internet-based presentations. Of greater impact than one specific educational video was the student’s development of the infrastructure and partnerships necessary for future students to create such programs as part of a digital library for use by both the partnering agencies and the medical school. The benefits of this project included successful partnerships within and outside the Medical School, and well-developed strategies for sustainability (involvement of 1st and 2nd year medical students, and grant applications for continuous funding). Through an impressive array of activities and contacts, this project met several key learning objectives: sustainable partnership building, risk behavior change, decreasing barriers to access to health care, program evaluation, and advocacy.
Project 2 (longitudinal clerkship)
Two students participated as investigators in a pilot study using a personalized educational intervention targeting socioeconomically disadvantaged inner-city youth with obesity and metabolic syndrome and their families 19. During their second, third, and fourth years of medical school as part of the longitudinal experience these students accomplished several objectives for the project, including organizing and directing study meetings, partnering with community physicians, contacting referred families, obtaining IRB-approved informed consent, administering a questionnaire, and educating families using an innovative approach that included educational sessions and in-home meal preparation and a grocery shopping trip. The students experienced a variety of barriers and facilitators first-hand, including language barriers, the complex cultural and environmental issues that contribute to obesity, as well as the challenges of recidivism and study recruitment. Through this longitudinal health project experience, the students met their learning goals, confirmed their plans for careers in primary care, and devised constructive ideas for project improvement. The students met the following key learning objectives: sustainable partnership-building, risk behavior change, environmental change, community health assessment, program evaluation, and decreasing barriers to access to health care.
Supervision
The CHIC clerkship directors (who are from the Department of Community and Preventive Medicine) have direct responsibility for supervising and teaching the students. They also have the primary responsibility for providing frequent and timely feedback, including mid-clerkship feedback on progress reported through regular progress notes, direct communications by phone and e-mail, direct observations, and for post-clerkship evaluation of the student. Preceptors (community partners and/or faculty mentors) and clerkship coordinators are responsible for guiding and assisting the clerkship directors and students.
Students who have participated in community service activities in their first three years document all such activities with the medical school’s community service outreach director as well as with the 4th year clerkship director when the students are involved in sustainable projects as part of the longitudinal track. Students in the 4th year clerkship month are responsible for presenting progress reports for their projects to preceptors and directors throughout the four-week program. Students write and submit progress notes weekly. The didactic lectures in the 4th year clerkship are mandatory for all students, including those who have been involved in the longitudinal track. The lectures are presented in the first 3 days of the 4-week experience so students are presented with specific knowledge, skills, and attitudes as early as possible in their experiential month, and to preserve the remainder of the time for project development, implementation, and evaluation. Even longitudinal students, for whom the bulk of community contact has occurred over 2 or 3 years, are encouraged to work more intensively in their target communities during the 4-week clerkship time to implement specific changes (e.g., more intensive interventions), to elicit feedback, and/or to evaluate impact.
Students are required to spend their non-didactic time at their community sites, creating and sustaining partnership relationships, performing project-related tasks, and implementing their projects. Their required final paper is a description of their intervention, and their documentation of measurable progress during the 4-week time period (e.g., impact on community site, impact on student, data collected and analyzed, number of persons who participated in the intervention, etc.). Longitudinal students also spend these four weeks at their community sites during non-didactic time and, as part of their required final paper, additionally report on their community health work throughout their 4 years. These students are also required to present their projects to a community health advisory board as part of their evaluation for consideration of Distinction in Community Service.
Students who pursue the longitudinal track are eligible to receive the honor of Distinction in Community Service on their M.D. diploma if they complete the following required elements:
Forty hours of community service in each of Years 1 and 2, and sixty hours of community service across Years 3 and 4 with a recognized community outreach agency approved by a community service outreach director in the medical school;
Registration of intent to pursue the longitudinal experience with the outreach director by January of their first year;
A grade of “High Pass” or “Honors” in the 4th year CHIC; and
Recommendation from the community health advisory board based on their review of the required final paper and project presentation, considering both effort and impact.
Throughout the entire CHIC a level of ethical behavior and professionalism is expected of the students. The community partners are a resource for our students, but the inverse is also true: students are providing valuable health-care resources for the community, and the community’s needs come first. Emphasizing the sustainability of a project with the students and the community partners helps address the common suspicions and fears associated with a community–medical institution partnership – namely, that the community will be seen as a short-term site for the benefit of education or research, rather than as a long-term beneficiary.
Evaluation of the Clerkship
All students are asked to complete evaluations of the CHIC at the end of their 4-week experience by using standardized online evaluation methods common to all our required courses and clerkships. Students are able to provide feedback anonymously to the medical school about their experience overall in the clerkship, as well as about the faculty, lectures, and structural elements of the clerkship. For specific modules of interest to us, for which we want feedback more specific than that which is available from standardized evaluation requirements, we ask the students to complete surveys anonymously, or to provide us with online feedback (not anonymously) related to some of the online didactic modules.
From the standardized evaluation feedback in a recent academic year, we learned that most respondents who provided ratings as to how well their project improved the health of the social group or community with which they interacted (n=27) rated this positively overall (23% said “a little”, 40% said “a moderate amount”, and 17% said “a lot”). Only 20% stated “not at all”. Of those who provided remarks on their project’s impact on their career (n=30), 94% reported that their clerkship project has impacted their future career favorably (27% said “a little”, 40% said “a moderate amount”, and 27% said “a lot”). Only 6% felt their project had no impact on their future career.
One of the novel features of the clerkship is the use of an interactive website to provide links to scheduling, didactic lectures, online educational modules, partnership contact information, possible clerkship project ideas, evidence-based “toolbox” resources (surveys, audit tools, scientific papers), and uploaded versions of all past clerkship student papers. We wanted to know how these online resources were perceived by the students. Standardized anonymous evaluation data over the past two academic years (n=102) reveals that 91% of the students found this website somewhat helpful (34%), very helpful (44%), or extremely helpful (13%). Only 9% felt it was not helpful.
Despite progress in reducing disparities in some health conditions within some ethnic/racial groups, the magnitude of these disparities has remained fairly constant overall and is actually increasing in certain important areas 23. Such issues are addressed throughout our medical school curriculum, and are specifically presented in our community health-related clerkship as important considerations for any intervention at the community level. Students often report specific project outcomes related to how a marginalized or underserved group (e.g., inner-city population) was able to have health care needs met as a result of a student project. In order to evaluate the impact of teaching students about disparities, 102 students were routinely and anonymously surveyed after the clerkship’s didactic lecture on “Cultural determinants of health”, which demonstrated how any minority population (in our guest lecturer’s example, the Lesbian, Gay, Bisexual, Transgendered, and Intersexed populations) can experience disparities in health care at the personal, provider, and health care system levels (e.g., prejudice, fear, ignorance). When asked “How relevant was the information covered in this training to your role at work/ role as a medical provider?", 92.9% responded in the positive direction (3 or 4 on a four-point Likert-type scale where 4 indicated “very relevant”).
Finally, in order to elicit qualitative feedback from students on the overall clerkship experience, we created an IRB-approved focus group study with a convenience sample of fourth-year medical students during a recent academic year (2006-2007) near the end of the students’ 4-week experience. The focus group comments revealed that students view the clerkship positively, and find it to be valuable to their respective career paths.
Discussion
The Double Helix curriculum, introduced as a new structure to the curriculum at URSMD in 1999, is an effort to better integrate clinical training with basic science across all four years of medical school. Our medical students are expected to be able to translate scientific evidence into practice in a timely manner, and this curriculum structure was designed to facilitate the translation between science and practice by integrating of basic science and clinical work from the beginning of the first year of medical school 20. Consonant with this model, learning objectives that are applicable to community health are also introduced in Years I and II in the curriculum and are applied in CHIC in the fourth year. Learning objectives are interwoven across the 4 years as students gain skills in creating, delivering, and evaluating evidence-based public health approaches at the community level.
At URSMD, CHIC has provided an innovative solution to the need to introduce future medical practitioners to community-based approaches to health promotion. This clerkship has demonstrated its feasibility, its ability to create partnerships between an academic center and community organizations, and its ability to consistently engage faculty from a variety of departments (e.g., Community & Preventive Medicine, Pediatrics, Family Medicine, Orthopedics, Environmental Health, Nursing, Emergency Medicine, Neurology, etc.). Through their participation, students and faculty members have had positive experiences while generating projects that have been sustainable in the community. In addition, the clerkship has served as a catalyst for educational innovation by introducing medical students to public health research methods and practical experience through hands-on projects; creating sustainable partnerships which are already attracting future clerkship students; and expanding career goal paradigms for future medical practitioners. Moreover, the clerkship has provided the students with an opportunity to integrate basic skills in public health research and practice with a meaningful and potentially sustainable project. Such projects have generated professional relationships between the University of Rochester Medical Center and community partners that will have impacts beyond the medical school curriculum. These outcomes fit very well with the community health mission of the Medical Center and those of Healthy People 2010 24 and this type of hands-on education is in accord with the recommendations from the Medicare Payment Advisory Commission, which has stressed the importance of experiential learning and teaching systems-based medicine 25.
The innovative aspects of our clerkship will be explored further, as we compare the educational outcomes resulting from this clerkship to those of more traditional preventive medicine courses, and consider whether the longitudinal track is superior to the one-month experience at achieving educational and health impact goals. Although the one-month format in the fourth year is more easily integrated into the curriculum and students have the luxury of focusing their learning on the topic for a short period of time, the longitudinal experience has tended to create a more involved leadership role and immersion experience for students while challenging them to incorporate community service into their other curricular responsibilities. Given the heterogeneous nature of medical student preferences and interests as well as our responsibility to the mission of community health, we intend to continue to offer both formats.
Room exists for us to improve the format of the CHIC. A challenge in this process is the broad nature of the competencies involved in community health improvement, particularly for students without prior experience. Coordination of student projects with the expertise of public health graduate students, post-doctoral fellows, and faculty from preventive medicine and other specialties with an interest in community health improvement projects would be beneficial, and we plan to pursue this. Opportunities for growth and dissemination are underway and we will continue to pursue evaluation strategies. Elements of the clerkship, such as the online Advocacy Module, are available to other medical schools 23 and will continue to be evaluated and improved.
To our knowledge, this is one of few required U.S. medical school clerkships in which advanced (4th year) medical students develop their own community-based health prevention projects while engaging faculty from a variety of disciplines. The full-time format during their 4th year permits these clinically-trained students to focus their attention on a wide variety of required tasks while participating in an intensive experiential learning process. The longitudinal track spanning all 4 years of medical school permits a more in-depth learning experience for the small but growing number of students who choose this format.
Required clerkships such as ours, with integrated features throughout the curriculum and across all 4 years, proactively involve all students in preventive medicine and population health. We feel this successfully meets the recommended changes in medical education by the World Health Organization and the Pew Health Professions Commission to ensure that all students are competent in community-based care, while at the same time facilitating long-term impact on the health of our community.
Acknowledgements
The authors would like to acknowledge the invaluable contributions of past and present Co-Directors and key contributors (Nancy Bennett, MD, MPH; Richard Kennedy, MD; Noelle Andrus, PhD; Adrienne Morgan; John McCarthy; Erik Libey), guest lecturers, course content developers, community agencies, participating Departments (Community and Preventive Medicine, Pediatrics, Family Medicine, Orthopedics, and the Center for Community Health), and the members of the many target populations who contributed with their cooperation and their expertise. The Clerkship has received financial support from a grant from the New York State Department of Health (W. Varade, PI) and the Regional Medicine-Public Health Education Center Program of the AAMC and Centers for Disease Control and Prevention (T. Pearson, PI). As a current grantee of the Association of American Medical Colleges and the Center for Disease Control and Prevention’s “Regional Medicine-Public Health Education Centers” initiative, the University of Rochester has integrated several of its programs with Regional Medicine–Public Health Education Centers by supporting the efforts of several faculty to participate in this Clerkship and in Grand Rounds presentations on several related issues. The faculty supported include: Nancy Bennett, MD, MPH; Noelle Andrus, PhD; and Scott McIntosh, PhD.
Contributor Information
Dr. Scott McIntosh, Department of Community and Preventive Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York..
Dr. Robert C. Block, Department of Community and Preventive Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York..
Ms. Gabrielle Kapsak, Department of Community and Preventive Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York..
Dr. Thomas A. Pearson, Department of Community and Preventive Medicine and Senior Associate Dean for Clinical Research, University of Rochester School of Medicine and Dentistry, Rochester, New York..
References
- 1.Corbett EC, Whitcomb M, for the Association of American Medical Colleges The AAMC Project on the Clinical Skills Education of Medical Students: Clinical Skills Education. 2004.
- 2.Liddell MJ, Davidson SK, Taub H, Whitecross LE. Evaluation of procedural skills training in an undergraduate curriculum. Med Educ. 2002;36(11):1035–1041. doi: 10.1046/j.1365-2923.2002.01306.x. [DOI] [PubMed] [Google Scholar]
- 3.Wang TS, Schwartz JL, Karimipour DJ, Orringer JS, Hamilton T, Johnson TM. An education theory-based method to teach a procedural skill. Arch Dermatol. 2004;140(11):1357–1361. doi: 10.1001/archderm.140.11.1357. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . Doctors for Health: A WHO Global Strategy for Changing Medical Education and Medical Practice for Health for All. World Health Organization; 1996. [Google Scholar]
- 5.Recreating Health Professional Practice for a New Century. The Fourth Report of the Pew Health Professions Commission; 2006. Pew Health Commission Report. [Google Scholar]
- 6.Pew Health Professions Commission Critical Challenges: Revitalizing the Health Professions for the Twenty-first Century. 1995.
- 7.Pomrehn PR, Davis MV, Chen DW, Barker W. Prevention for the 21st century: Setting the context through undergraduate medical education. Acad Med. 2000;75(7 Suppl):S5–13. doi: 10.1097/00001888-200007001-00002. [DOI] [PubMed] [Google Scholar]
- 8.Association of American Medical Colleges . GQ Graduation Questionnaire. Association of American Medical Colleges; [Accessed 12/6/07]. 2006. http://www.aamc.org/data/gq/allschoolsreports/start.htm. [Google Scholar]
- 9.Brill JR, Ohly S, Stearns MA. Training community-responsive physicians. Acad Med. 2002;77(7):747. doi: 10.1097/00001888-200207000-00036. [DOI] [PubMed] [Google Scholar]
- 10.Davidson RA. Community-based education and problem solving: The community health scholars program at the University of Florida. Teach Learn Med. 2002;14(3):178–181. doi: 10.1207/S15328015TLM1403_8. [DOI] [PubMed] [Google Scholar]
- 11.Kaufman A, Galbraith P, Alfero C, et al. Fostering the health of communities: A unifying mission for the university of new mexico health sciences center. Acad Med. 1996;71(5):432–440. doi: 10.1097/00001888-199605000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Elam CL, Sauer MJ, Stratton TD, Skelton J, Crocker D, Musick DW. Service learning in the medical curriculum: Developing and evaluating an elective experience. Teach Learn Med. 2003;15(3):194–203. doi: 10.1207/S15328015TLM1503_08. [DOI] [PubMed] [Google Scholar]
- 13.Velezis MJ, Endeshaw Y. Learning through community participation: Immunization program at an elementary school. Acad Med. 2001;76(2):195–198. doi: 10.1097/00001888-200102000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Xakellis GC, Jr, Robinson M. A strategy for teaching students concepts of population-based health care for older persons. Acad Med. 2003;78(8):789–792. doi: 10.1097/00001888-200308000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Carney PA, Schifferdecker KE, Pipas CF, et al. A collaborative model for supporting community-based interdisciplinary education. Acad Med. 2002;77(7):610–620. doi: 10.1097/00001888-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Hensel WA, Smith DD, Barry DR, Foreman R. Changes in medical education: The community perspective. Acad Med. 1996;71(5):441–446. doi: 10.1097/00001888-199605000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196(4286):129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 18.Andrus NC, Bennett NM. Developing an interdisciplinary, community-based education program for health professions students: The rochester experience. Acad Med. 2006;81(4):326–331. doi: 10.1097/00001888-200604000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Quinn L, Block R, McIntosh S. Impact of a community health improvement clerkship project. Med Ed. 2007 doi: 10.1111/j.1365-2923.2007.02882.x. in press. [DOI] [PubMed] [Google Scholar]
- 20.Williams GC, Markakis KM, Ossip-Klein DJ, McIntosh S, Tripler S, Grady-Weliky T. Evidence-based behavior change curriculum for the ambulatory clerkship; the double helix. Health Ed. 2005;105(2):142–153. [Google Scholar]
- 21.Greenlick MR. Educating physicians for population-based clinical practice. JAMA. 1992;267(12):1645–1648. [PubMed] [Google Scholar]
- 22.McIntosh S, Kapsak G, Sager R, Clarke H. Understanding Advocacy and Policy Change Module for Medical Students. Association of American Medical Colleges; [Accessed 12/6/07]. MedEDPORTAL < http://www.aamc.org/mededportal,ID=163>. [Google Scholar]
- 23.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 24.Office of Disease Prevention and Health Promotion. U.S. Department of Health and Human Services [Accessed 12/6/07];Healthy People 2010. < http://www.healthypeople.gov/>.
- 25.Medicare Payment Advisory Commission (MedPAC) Hospital inpatient and outpatient services. 2007.