Abstract
Background
Patients with angina pectoris or myocardial infarction frequently present without evidence of cardiac-specific heart enzymes by laboratory analysis or specific pathologic electro-cardiogram findings. The current study analyzed the efficacy of the erythrocyte sedimentation rate as an additional potential indicator for coronary heart disease, the aim being to enable quicker identification of patients with angina pectoris or myocardial infarction so that they can be more rapidly treated.
Methods
Patients with angina pectoris or myocardial infarction who had undergone a heart catheter examination were included in the study. The diagnosis of acute coronary heart disease was made by the physician who performed coronary angiography. Patients without coronary heart disease were used as a control group. The erythrocyte sedimentation rate was measured in all patients. Patients with angina pectoris or myocardial infarction and an inflammatory or tumor disease were excluded.
Results
The erythrocyte sedimentation rate was prolonged in 79 (58.09%) of 136 patients; 69 (50.74%) patients (95% confidence interval ±8.4%, 42.34%–59.14%) had coronary heart disease and a prolonged erythrocyte sedimentation rate. The erythrocyte sedimentation rate was prolonged in ten (7.35%) patients (95% confidence interval ±4.39%, 2.96%–11.74%) without coronary heart disease by coronary angiography. The specificity of the erythrocyte sedimentation rate for coronary heart disease was 70.59% and the sensitivity was 67.65%.
Conclusion
Erythrocyte sedimentation rate may be a useful additional diagnostic criterion for coronary heart disease.
Keywords: erythrocyte sedimentation rate, coronary heart disease, myocardial infarction, coronary angiography
Introduction
Determination of the erythrocyte sedimentation rate is a nonspecific test that constitutes one of the oldest laboratory methods. An accelerated erythrocyte sedimentation rate may be indicative of inflammation or the presence of a tumor. However, a slow erythrocyte sedimentation rate may occur (eg, in polycythemia vera). Despite the critical role of cytokines in inflammatory conditions, the erythrocyte sedimentation rate still plays an important role in the diagnosis and follow-up of rheumatoid arthritis and temporal arthritis, sickle cell disease, and osteomyelitis, as well as in noninflammatory conditions such as stroke, coronary artery disease, and prostate cancer.1
Patients with symptoms of angina pectoris or myocardial infarction frequently present without striking evidence of cardiac-specific enzymes in blood laboratory assessments or specific electrocardiogram findings. The purpose of this study was to assess the efficacy of the erythrocyte sedimentation rate as a potential additional indicator for coronary heart disease so that patients with angina pectoris or myocardial infarction can be more rapidly identified and treated.
This study differs from other studies in that all patients were examined by coronary angiography with multiple blood tests and patients with inflammation and tumor were excluded from this study. This meant that the erythrocyte sedimentation rate and acute coronary heart disease could be studied better by close temporal investigations.
Materials and methods
This was a retrospective study of patients with angina pectoris, non-ST-elevation myocardial infarction, or acute myocardial infarction with ST-segment elevation, as assessed by electrocardiography. All patients included in this study underwent coronary angiography, resulting in the diagnosis of acute coronary heart disease. Patients in whom coronary heart disease was excluded by coronary angiography served as controls. The erythrocyte sedimentation rate was measured over a period of 1 hour and 2 hours; normal values were considered to be <10 mm in the first hour and <20 mm in the second hour. The number of leukocytes was also determined in all patients; the normal number of leukocytes was considered to be 4.000–10.000 cells/μL. C-reactive protein (CRP) level was determined in all patients, with a normal reference value of <6.0 mg/L. The average number with standard deviation of neutrophils, lymphocytes, monocytes, eosinophils, and basophils was determined as a percentage of patients with prolonged erythrocyte sedimentation rate and coronary heart disease. Any inflammatory disease was excluded in all patients by clinical and radiologic assessment and by urine sediment or urine culture. Patients with angina pectoris diagnosed with inflammatory or tumor diseases were excluded from the study.
Statistical analysis
Data are presented as mean ± standard deviation. The χ2 test was used to compare prolonged erythrocyte sedimentation rates between patients with and without coronary heart disease. The specificity and sensitivity of the erythrocyte sedimentation rate as a marker for coronary artery disease and the 95% confidence interval (CI) were calculated.
Results
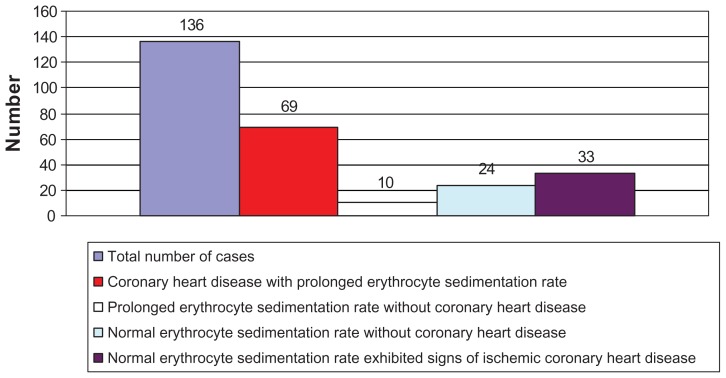
A total of 136 patients with angina pectoris or acute myocardial infarction were included in this study (Figure 1). The cohort included 89 men and 47 women with an average age of 69.31 ± 12.45 years.
Figure 1.
The number of cases in this study.
During cardiac catheterization, 102 (75%) patients were found to have coronary heart disease, including 70 (68.63%) males and 32 (31.37%) females. A total of 52 (38.24%) patients were diagnosed with angina pectoris, 39 (28.67%) with non-ST-elevation myocardial infarction, and ten (7.35%) with acute ST-elevation myocardial infarction. The indication for coronary angiography was performed in 35 (25.74%) patients due to changes in the electrocardiogram such as negative T, R-regression, and pathological ergometry. Further, 59 patients had three-vessel disease, 24 patients had two-vessel disease, and 19 patients had one-vessel disease. No coronary heart disease was seen in 34 (25%) patients, including 19 (55.88%) men and 15 (44.12%) women.
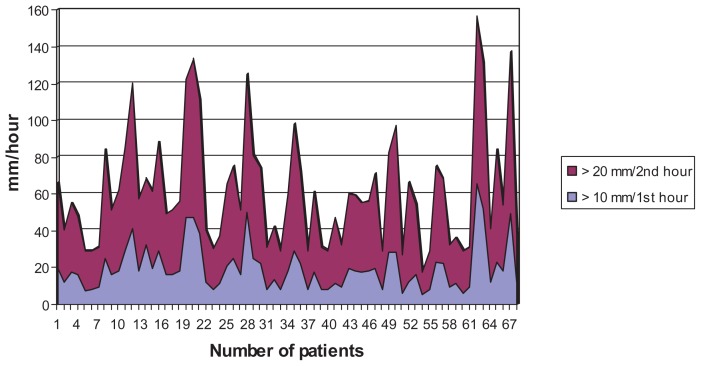
The erythrocyte sedimentation rate was prolonged in 79 (58.09%) patients. Coronary heart disease and a prolonged erythrocyte sedimentation rate were observed in 69 (50.74%) patients (95% CI ±8.4%, 42.34%–59.14%) with an average value of 19.68 ± 12.71 mm in the first hour and 41.88 ± 19.30 mm in the second hour (Figure 2). The erythrocyte sedimentation rate was prolonged in ten (7.35%) patients (95% CI ±4.39%, 2.96%–11.74%) without signs of significant stenosis by coronary angiography. A normal erythrocyte sedimentation rate was seen in 24 (17.65%) patients (95% CI ±6.41%, 11.24%–24.06%) without evidence of coronary heart disease by cardiac catheterization. In contrast, 33 (24.26%) patients (95% CI ± 7.2%, 17.06%–31.46%) with a normal erythrocyte sedimentation rate exhibited signs of ischemic coronary heart disease by left heart catheterization.
Figure 2.
The value and number prolonged erythrocyte sedimentation rate in patients with an acute coronary heart disease.
The specificity of the erythrocyte sedimentation rate for coronary heart disease was 70.59% and the sensitivity was 67.65%. However, the two-sided significance using the χ2 test was not significant for a prolonged erythrocyte sedimentation rate being indicative of coronary heart disease.
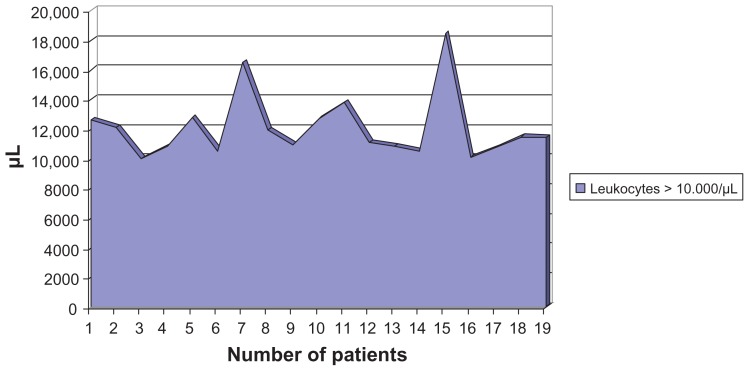
The average number of leukocytes in all patients was 8.596 cells/μL ± 2.578 cells/μL. The average increased leukocyte value in 35 (25.74%) patients was 12.003 ± 2.108 cells/μL and in 19 (13.97%) patients with coronary heart disease and prolonged erythrocyte sedimentation rate 12.072 ± 2.183 cells/μL (Figure 3).
Figure 3.
Leukocytosis in patients with acute coronary heart disease and prolonged erythrocyte sedimentation rate
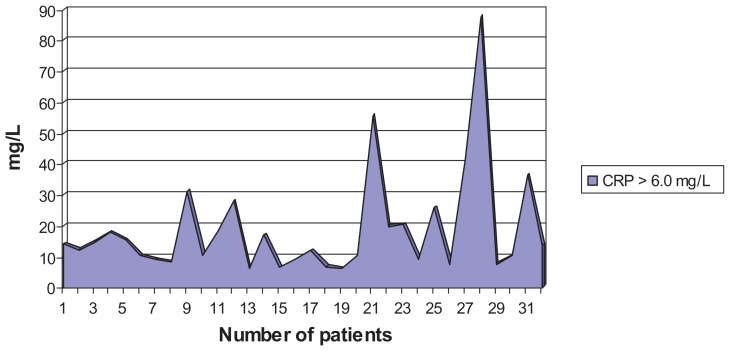
The average elevated CRP value in 49 (36.03%) patients was 19.04 ± 20.77 mg/L; in 32 (23.53%) patients with an acute coronary heart disease and prolonged erythrocyte sedimentation rate 18.67 ± 16.95 mg/L (Figure 4).
Figure 4.
CRP in patients with prolonged erythrocyte sedimentation rate and coronary heart disease.
The average number of neutrophils was 67.14% ± 11.07% (reference range 50%–70%), 22.04% ± 9.70% (20%–52%) lymphocytes, 8.75%±2.57% (3%–7%) monocytes, 1.84% ± 1.28% (1%–4%) eosinophils, and 0.37% ± 0.22% (0%–1%) basophils. The neutrophils were increased in 27 (39.13%) patients from a total of 69 patients with coronary heart disease and prolonged erythrocyte sedimentation rate with coronary heart disease.
Discussion
The findings of this study suggest a possible correlation between a prolonged erythrocyte sedimentation rate and coronary heart disease. Indeed, the erythrocyte sedimentation rate was mostly prolonged in patients with coronary heart disease. However, although the specificity and sensitivity of the erythrocyte sedimentation rate as a marker for coronary heart disease were relatively high, the χ2 test showed a nonsignificant effect.
Erikksen et al2 previously reported that the erythrocyte sedimentation rate may be a good indicator for coronary heart disease, mortality, and the risk of death from coronary heart disease. The relationship between the erythrocyte sedimentation rate and the risk of coronary heart disease was also assessed in a cohort study by Andresdottir et al3 The authors concluded that the erythrocyte sedimentation rate can be used as an independent prognostic factor for coronary heart disease in men and women on the basis of an inflammatory process of atherosclerosis.3 However, it has been shown that the erythrocyte sedimentation rate cannot be used for screening and check-up examinations in asymptomatic patients.4 Nevertheless, Gillum et al5 described that an increased erythrocyte sedimentation rate is a risk factor for coronary heart disease. This relationship between the erythrocyte sedimentation rate and the risk of coronary heart disease was also observed in this study. The other inflammatory parameters were also elevated in this study. Therefore, this assumption of inflammation as a basis for the development of atherosclerosis was also confirmed through this recent study.
A relationship between coronary atherosclerosis and erythrocyte sedimentation rate was found in a clinical observation study by Natali et al.6 In the present study, seven patients were diagnosed with coronary atherosclerosis by cardiac catheterization. In three cases of arteriosclerosis, the erythrocyte sedimentation rate was extended in this study.
Serum levels of myocardial enzymes and inflammatory biomarkers have been shown not only to be increased in the setting of an acute coronary event but also to quantitatively correlate with the extent of myocardial damage and coronary artery disease severity, according to angiographic findings.7,8 CRP is the most widely studied inflammatory marker, and there is now robust evidence that CRP is a strong predictor of cardiovascular risk among apparently healthy individuals, patients undergoing elective revascularization procedures, and patients presenting with acute coronary syndromes.8–13 Circulating levels of CRP rise during the acute-phase response to tissue injury, infection, and inflammation,8–13 and CRP, the prototypic acute-phase protein, and to a lesser extent fibrinogen, have been proven to be reliable and important markers of the risk of ischemic heart disease.7 Also in this study, elevated levels of CRP were observed in about one third of patients with acute coronary heart disease after exclusion of inflammation.
A correlation has also been observed between leukocyte count and acute coronary syndrome; investigations of the utility of the leukocyte count as a risk factor and prognostic indicator in patients with acute coronary syndrome are consistent with the current concept that atherosclerosis is an inflammatory disease.14–17 Leukocytosis induces or worsens coronary heart disease through multiple pathologic mechanisms that mediate inflammation, cause proteolytic and oxidative damage to endothelial cells, plug the microvasculature, induce hypercoagulability, and promote infarct expansion.16 In summary, it has been consistently shown that leukocytosis is an independent risk factor and prognostic indicator of future cardiovascular outcomes, regardless of disease status.16 The leukocyte count is inexpensive to obtain, reliable, easy to interpret, and ordered routinely in inpatient and outpatient settings.16 Also in this study, leukocyte counts in all patients with acute coronary heart disease were increased, on average. Therefore, a relationship between leukocyte account and acute coronary heart disease has also been observed in this study.
The independent association of neutrophil count with the angiographic characteristics of coronary atherosclerosis strongly suggests that granulocytosis may play a role in the development of coronary atherosclerosis.17 The granulocytes from patients with prolonged erythrocyte sedimentation rate with coronary heart disease in this study were not increased, on average, apart from individual elevated values.
Conclusion
The erythrocyte sedimentation rate was found to be frequently prolonged in patients with coronary heart disease. An increase in erythrocyte sedimentation rate provides information about the inflammatory etiology of coronary heart disease. The erythrocyte sedimentation rate may thus be helpful as an additional diagnostic tool for coronary heart disease.
Footnotes
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Saadeh C. The erythrocyte sedimentation rate: old and new clinical application. South Med J. 1998;91(3):220–225. [PubMed] [Google Scholar]
- 2.Erikssen G, Liestol K, Bjornholt JV, Stormorken H, Thaulow E, Erikssen J. Erythrocyte sedimentation rate: a possible marker of atherosclerosis and a strong predictor of coronary heart disease mortality. Eur Heart J. 2000;21(19):1614–1620. doi: 10.1053/euhj.2000.2148. [DOI] [PubMed] [Google Scholar]
- 3.Andresdottir MB, Sigfusson N, Sigvaldason H, Gudnason V. Erythrocyte sedimentation rate, an independent predictor of coronary heart disease in men and women: the Reykjavik Study. Am J Epidemiol. 2003;158(9):844–851. doi: 10.1093/aje/kwg222. [DOI] [PubMed] [Google Scholar]
- 4.Reinhart WH. Erythrocyte sedimentation rate – more than an old fashion? Ther Umsch. 2006;63(1):108–112. doi: 10.1024/0040-5930.63.1.108. [DOI] [PubMed] [Google Scholar]
- 5.Gillum RF, Mussolino ME, Makuc DM. Erythrocyte sedimentation rate and coronary heart disease: the NHANES I epidemiologic follow-up study. J Clin Epidemiol. 1995;48(3):353–361. doi: 10.1016/0895-4356(94)00156-k. [DOI] [PubMed] [Google Scholar]
- 6.Natali A, L’Abbate A, Ferrannini E. Erythrocyte sedimentation rate, coronary atherosclerosis, and cardiac mortality. Eur Heart J. 2003;24(7):639–648. doi: 10.1016/s0195-668x(02)00741-8. [DOI] [PubMed] [Google Scholar]
- 7.Peppes V, Rammos G, Manios E, Koroboki E, Rokas S, Zakopoulos N. Correlation between myocardial enzyme serum levels and markers of inflammation with severity of coronary artery disease and Gensini score: a hospital-based, prospective study in Greek patients. Clin Interv Aging. 2008;3(4):699–710. doi: 10.2147/cia.s3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berk BC, Weintraub WS, Alexander RW. Elevation of C- reactive protein in “active” coronary artery disease. Am J Cardiol. 1990;65(3):168–172. doi: 10.1016/0002-9149(90)90079-g. [DOI] [PubMed] [Google Scholar]
- 9.Danesh J, Muir J, Wong YK, Ward M, Gallimore JR, Pepys MB. Risk factors for coronary heart disease and acute-phase proteins: a population-based study. Eur Heart J. 1999;20(13):954–959. doi: 10.1053/euhj.1998.1309. [DOI] [PubMed] [Google Scholar]
- 10.Neumann FJ, Ott I, Gawaz M, et al. Cardiac release of cytokines and inflammatory responses in acute myocardial infarction. Circulation. 1995;92(4):748–755. doi: 10.1161/01.cir.92.4.748. [DOI] [PubMed] [Google Scholar]
- 11.Mendall MA, Strachan DP, Butland BK, et al. C-reactive protein: relation to total mortality, cardiovascular mortality and cardiovascular risk factors in men. Eur Heart J. 2000;21(19):1584–1590. doi: 10.1053/euhj.1999.1982. [DOI] [PubMed] [Google Scholar]
- 12.Brunetti ND, Troccoli R, Correale M, Pellegrino PL, Di Biase M. C-reactive protein in patients with acute coronary syndrome: correlation with diagnosis, myocardial damage, ejection fraction and angiographic findings. Int J Cardiol. 2006;109(2):248–256. doi: 10.1016/j.ijcard.2005.06.021. [DOI] [PubMed] [Google Scholar]
- 13.Blake GJ, Ridker PM. C-reactive protein and other inflammatory risk markers in acute coronary syndromes. J Am Coll Cardiol. 2003;41(4 Suppl S):37S–42S. doi: 10.1016/s0735-1097(02)02953-4. [DOI] [PubMed] [Google Scholar]
- 14.Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107(3):499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 15.Pai JK, Pischon T, Ma J, et al. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004;351(25):2599–2610. doi: 10.1056/NEJMoa040967. [DOI] [PubMed] [Google Scholar]
- 16.Madjid M, Awan I, Willerson JT, Casscells SW. Leukocyte count and coronary heart disease: implications for risk assessment. J Am Coll Cardiol. 2004;44(10):1945–1956. doi: 10.1016/j.jacc.2004.07.056. [DOI] [PubMed] [Google Scholar]
- 17.Jia EZ, Yang ZJ, Yuan B, et al. Relationship between leukocyte count and angiographical characteristics of coronary atherosclerosis. Acta Pharmacol Sin. 2005;26(9):1057–1062. doi: 10.1111/j.1745-7254.2005.00169.x. [DOI] [PubMed] [Google Scholar]