Abstract
Chronic hepatitis B affects Asian Americans at a much higher rate than the general US population. Appropriate care can limit morbidity and mortality from hepatitis B. However, access to care for many Asian Americans and other immigrant groups is limited by their lack of knowledge about the disease, as well as cultural, linguistic, and financial challenges. This article describes the results of BfreeNYC, a New York City pilot program that, from 2004 to 2008, provided hepatitis B community education and awareness, free screening and vaccinations, and free or low-cost treatment primarily to immigrants from Asia, but also to residents from other racial and ethnic minority groups. The program was the largest citywide screening program in the United States, reaching nearly 9,000 people, and the only one providing comprehensive care to those who were infected. During the program, new hepatitis B cases reported annually from predominantly Asian neighborhoods in the city increased 34 percent. More than two thousand people were vaccinated; 57 percent of the 1,162 patients who tested positive for hepatitis B and were evaluated by program clinical services were still in care at the end of the program. Our analysis found that the program was effective in reaching the target population and providing care. Although follow-up care data will be needed to demonstrate long-term costeffectiveness, the program may serve as a useful prototype for addressing hepatitis B disparities in communities across the United States.
Hepatitis B, a virus that has infected one-third of the world’s population, can persist in certain individuals as a chronic infection with serious health consequences. More than 350 million people worldwide, including more than a million Americans, have chronic hepatitis B infection.1 Chronic hepatitis B is particularly prevalent in Asia, and more than half of the chronically infected people in the United States are Asian American, Native Hawaiian, or Pacific Islander.2 The rate of chronic infection in Asian Americans is approximately 10 percent, compared to 0.2 percent in Caucasians, making chronic hepatitis B a major health disparity for Asian Americans.3
Nearly a quarter of chronically infected people may die of hepatitis B complications, including end-stage liver disease and liver cancer. Chronic hepatitis B is the leading cause of primary liver cancer–cancer in which the liver is the primary tumor site–worldwide.1 An Institute of Medicine expert review committee recently concluded that both the general public and health care providers have poor knowledge about and awareness of chronic hepatitis B,2 and nearly two-thirds of infected people are unaware of their status.4
In this article we describe an innovative fouryear pilot program in New York City that provided a comprehensive approach to screening and treatment of hepatitis B in at-risk groups. We analyze data on the program’s effectiveness and share key lessons learned to inform local and national initiatives addressing hepatitis B.
Hepatitis B Screening And Treatment Program
The Beginnings
In 2003 community leaders, clinicians, researchers, and politicians formed a coalition to develop a program to address the burden of hepatitis B in New York City.5 Multiple small screening programs targeting Chinese immigrants during the preceding years had demonstrated a high need for such services in the city.6 The goal was to expand these screening activities into a more comprehensive program. Alan Gerson, who represented lower Manhattan–including Chinatown–on the New York City Council, was a strong advocate for the program and instrumental in garnering council support and funding.7 The program’s initial name, the Asian American Hepatitis B Program, was changed to BfreeNYC because its reach was expanded to immigrants from other areas–such as Africa and the Caribbean–where hepatitis B rates are also high.
Approach And Planning
A coalition of stakeholders– including community health centers, social service groups, community-based organizations, city council members, public hospitals, physician groups, and academic institutions– created a comprehensive, citywide, no-cost hepatitis B screening and treatment program (Appendix Exhibit 1).8 BfreeNYC’s components included free community-based screenings, vaccination, and care. People who were not infected were given vaccinations, and infected individuals were given free clinical evaluation and care at program sites. A central executive committee, including representatives from all of the stakeholder groups, administered the program and standardized procedures. Reimbursement–at rates higher than those provided by Medicaid to cover the additional costs to institutions participating in the program–was negotiated with community-based partners and health care facilities for screening, vaccination, care and treatment visits, and laboratory tests.
Program Components
MEDIA AND EDUCATIONAL OUTREACH
A multimedia campaign was developed with assistance from a NewYork–based advertising agency that focused on reaching Asian Americans. The campaign was then refined in focus groups. Advertisements appeared in Chinese and Korean publications throughout the four years of program, along with radio spots and announcements on Korean cable television. Educational workshops were developed and implemented at community screenings, and a website was established to host information about screenings and educational materials.
COMMUNITY-BASED SCREENING
Free screening services were planned and organized with community-based partners. Screening surveys assessed participants’ knowledge about hepatitis B, the barriers to care that they faced, and how they had learned about BfreeNYC.
Procedures for testing and follow-up were standardized. Test results were provided to participants during follow-up visits at their screening sites. In year 2 of the program, a case management component was added for participants who required vaccination or treatment.
VACCINATION
People whose tests showed that they were uninfected were offered a threeshot immunization series. The shots were delivered at the screening site.3
CARE AND TREATMENT
People whose tests showed that they were infected and who had insurance were referred to their own health care provider. Uninsured infected people were referred either to a newly established viral hepatitis clinic at Bellevue Hospital, funded by the program and staffed by infectious disease and gastroenterology specialists, or to one of two community-based clinics located in Chinatown in Manhattan. One of the clinics was the Charles B. Wang Community Health Center, a federally qualified health center that serves the Asian American community. The other was Gouverneur Healthcare Services, a public outpatient center. Both were staffed by primary care providers. Providers received training and updates from program specialists to evaluate, monitor, and treat hepatitis B. Hepatology specialists at Bellevue Hospital and New York University’s School of Medicine were available for consultation with primary care providers at the centers. All patients with complex problems, including liver failure or liver cancer, were referred to the viral hepatitis clinic at Bellevue Hospital.
Evaluation and treatment protocols based on published hepatitis B management guidelines9,10 provided a standard of care at each site. Initial evaluation included tests of liver function, of hepatitis B blood levels, and for liver cancer. Customized templates for history taking, flow sheets tracking clinical tests related to hepatitis B, and lab ordering bundles were developed to assist primary care physicians in coordinating care at the community health center in year 2, when an electronic health record system was installed.
DATA COLLECTION AND ANALYSIS
An online database was customized to coordinate all program activities, collect data, track specimens, and report results to partners and the program directors. Institutional Review Board approval was obtained from all participating institutions to allow deidentified data to be placed in a research database for analysis. Standardized forms were created for data exchange between screening sites, labs, clinical sites, and the data management center.
Program Results
Population Screened
From March 2004 to June 2008, 8,888 participants were screened by BfreeNYC. Eighty-four percent were foreignborn Asian Americans, the majority of whom were Chinese. Sixty-two percent had a high school education or less, and almost two-thirds were uninsured (Exhibit 1). A map showing participant distribution by ZIP code and country of birth is provided in Appendix Exhibit 2.8
Exhibit 1.
Sociodemographic Characteristics Of People Screened By BfreeNYC, 2004–08
| Characteristic | Number | Percent |
|---|---|---|
| Sex | ||
| Male | 4,279 | 48.1 |
| Female | 4,548 | 51.2 |
| Unknown | 61 | 0.7 |
| Age (years) | ||
| <20 | 303 | 3.4 |
| 20–39 | 3,341 | 37.6 |
| 40–59 | 3,911 | 44.0 |
| >59 | 1,316 | 14.8 |
| Unknown | 17 | 0.2 |
| Race | ||
| Asian/Pacific Islander | 7,873 | 88.6 |
| Black | 341 | 3.8 |
| Hispanic | 332 | 3.7 |
| White/other | 94 | 1.1 |
| Unknown | 248 | 2.8 |
| Birthplace | ||
| China | 3,772 | 42.4 |
| Korea | 2,734 | 30.8 |
| Malaysia | 637 | 7.2 |
| Caribbean | 289 | 3.3 |
| Other Asian country | 278 | 3.1 |
| United States | 272 | 3.1 |
| Central/South America | 187 | 2.1 |
| Africa | 116 | 1.3 |
| Other | 27 | 0.3 |
| Unknown | 576 | 6.4 |
| Years in United States | ||
| <5 | 1,543 | 17.4 |
| 5–10 | 2,633 | 29.6 |
| >10 | 3,290 | 37.0 |
| Born in United States | 272 | 3.1 |
| Unknown | 1,150 | 12.9 |
| Education | ||
| Less than high school graduate | 2,716 | 30.6 |
| High school/technical school graduate | 2,757 | 31.0 |
| College/university graduate | 2,303 | 25.9 |
| Unknown | 1,112 | 12.5 |
| Income | ||
| Less than $18,600 | 3,804 | 42.8 |
| $18,600–$24,899 | 1,328 | 14.9 |
| $24,900–$50,399 | 1,639 | 18.4 |
| $50,400 or above | 198 | 2.2 |
| Unknown | 1,919 | 21.6 |
| Insurance | ||
| Uninsured | 5,615 | 63.2 |
| Insured | 1,805 | 20.3 |
| Unknown | 1,468 | 16.5 |
SOURCE Authors’ analysis.
Participants reported poor knowledge of hepatitis B. Fewer than 10 percent correctly reported that hepatitis B is typically asymptomatic, and only 50 percent knew that vaccination could protect against infection (Appendix Exhibit 3).8 Results also suggested that hepatitis B stigma persists: Only 44 percent of the participants said that they would tell their family if they learned they were infected.
SEROLOGICAL RESULTS
The participants were divided into three categories. Infected people–18 percent of the participants–tested positive for hepatitis B surface antigen. Protected people–46 percent–had antibodies to hepatitis B, indicating immunity by resolved past infection or prior immunization. Susceptible people–36 percent–lacked evidence of hepatitis B antibodies (Appendix Exhibit 4).8
About 40 percent of those screened reported being previously tested. It is likely that people who knew or suspected that they were infected chose to participate so they could confirm their diagnosis or obtain free care.We performed an analysis on the 5,077 participants who were newly screened to obtain a more representative population estimate.11 The rate of infection in newly screened individuals was 12 percent, a figure closer to published data.11
SCREENING FOLLOW-UP
Eighty-three percent of the people who were screened returned for care; results and recommendations were mailed to those who did not return. Eighty percent of those who were protected or susceptible returned, and 95 percent of the chronically infected returned (Exhibit 2). Those who received results in the mail showing that they were infected may have been more motivated to return for care than others were.
Exhibit 2.
Follow-Up Results, By Hepatitis B Infection Status
| Infection statusa | Number | Group effectiveness rate (%) |
Overall effectiveness rate (%) |
|---|---|---|---|
| Infected individuals (n=1,632) | |||
| Returned for results | 1,553 | 95.2 | 95.2 |
| Referred to program clinical siteb | 1,365 | 87.9 | 83.6 |
| Returned for clinical evaluation | 1,162 | 85.1 | 71.1 |
| Received full evaluation | 1,031 | 88.7 | 63.1 |
| In care at program’s end | 658 | 56.6 | 40.3 |
| Susceptible individuals (n=3,156) | |||
| Returned for results | 2,384 | 75.5 | 75.5 |
| Received first vaccination | 2,253 | 94.5 | 71.4 |
| Received second vaccination | 1,972 | 82.7 | 62.5 |
| Received third vaccination | 1,652 | 69.2 | 52.3 |
| Protected individuals (n=4,080) | |||
| Returned for results | 3,431 | 84.1 | 84.1 |
SOURCE Authors’ analysis. NOTES The group effectiveness rate is the percentage of those who participated in the next stage of the program. For example, of the 1,553 individuals who returned for their results, 1,365, or 87.9 percent, returned for their results. The overall effectiveness rate is the percentage of those in each infection status who participated in a stage of the program.
Twenty individuals had indeterminate results and could not be placed into an infection status.
Insured screening participants were referred back to their primary care provider.
Exhibit 3 shows that in multivariate analyses that adjust for interactions among each of the factors examined, people who were of Asian race, uninsured, and infected, and who visited a screening facility with a predominantly Asian clientele, were significantly more likely to return for results than other screened individuals (Appendix Exhibits 5 and 6).8 Appendix Exhibit 5 further demonstrates the higher rate of return at screening facilities with largely Asian clienteles by infection status. Higher return rates were seen among those with increased incentive to obtain care: people who were infected and had limited means of obtaining care elsewhere. It is likely that the higher rate of returnamongAsians reflects the greater availability of facilities in this program with outreach practices specifically catering to their unique care needs.
Exhibit 3.
Probability Of Receiving Follow-Up Care Among Those Who Screened For Hepatitis B (Odds Ratios)
| Variable | Predicting return for results among all screened |
Predicting follow-up visit among the infected |
Predicting third vaccine among the susceptible |
|---|---|---|---|
| Previously testeda | 1.2 | 0.8 | 1.1 |
| Asianb | 5.2b | — c | 9.4b |
| Uninsuredd | 1.4b | 5.3b | 1.3b |
| Infectede | 3.2b | — f | — g |
| Asian clientele at screening facilityh | 2.6b | 1.4 | 2.1b |
SOURCE Authors’ analysis. NOTE All of the results were adjusted for age and sex, which were not significant.
Reference group is not previously tested or not sure if previously tested.
Reference group is not Asian.
Ninety-nine percent of those infected were Asian/Pacific Islander, and race did not predict follow-up care among the infected.
Reference group is insured.
Reference group is not infected.
Infection status could not be used to predict follow-up because the group included only infected individuals.
Infection status could not be used to predict follow-up, because the group included only uninfected individuals.
Reference group is non-Asian clientele at screening facility.
p < 0:01
VACCINATION
Of the 3,156 susceptible individuals, 2,253 received the first vaccination, and 1,652 received all three vaccinations (Exhibit 2). Adjusting for other factors in multivariate analyses, Asian race, being uninsured, and visiting a screening facility with a predominantly Asian clientele were significantly related to receiving all three vaccines among susceptible individuals (Exhibit 3).
REFERRAL TO CARE
Of the 1,632 infected individuals, 1,553 returned for test results (Exhibit 2). Twelve percent of individuals had insurance and were referred to their primary care provider. Eighty-eight percent of the infected participants lacked insurance and were referred to trained providers at program sites.
CARE AND TREATMENT
A total of 1,162 individuals (85 percent of those referred) were seen at program clinics (Exhibit 2): forty-nine percent at Bellevue Hospital, 33 percent at the Charles B. Wang Community Health Center, and 16 percent at Gouverneur Healthcare Services (data not shown). More than 90 percent completed a full clinical evaluation; 80 percent had evidence of active infection, and 15 percent–who met clinical guidelines for the treatment–began treatment with antiviral medication according to the program’s protocol.9,10
Costs
Evaluation and follow-up care, in addition to treatment with antiviral medication for infected people accounted for the largest portion (39.6 percent) of the four-year cost of BfreeNYC (Exhibit 4). The average screening and vaccination cost was $273 per person, and education and awareness outreach cost another $139 per person.
Exhibit 4. Cost Of The BfreeNYC Hepatitis B Screening Program, By Type Of Expenditure, 2004–08.
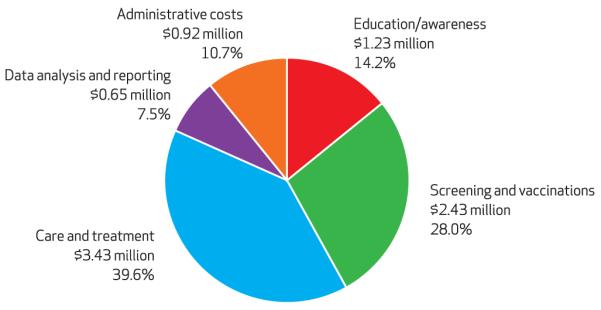
SOURCE Authors’ analysis. NOTE The total cost was $8,664,600.
The average cost of identifying an infected participant was $2,243. The average annual cost of care per infected participant was $1,598. However, the true program cost was $1,344 per year because most medications were provided through pharmaceutical companies’ patient assistance programs.
Program Assessment
Reaching The At-Risk Population
Although Asian media outlets in New York City, including newspapers and radio stations, report reaching an audience of around 900,000 each, and Korean cable television reports reaching 200,000, no direct assessment of the awareness campaign was conducted during the program period. Our analysis of 900 randomly surveyed New York City Asian Americans in the 2009 REACH US Survey12 found that approximately 10 percent had heard about BfreeNYC two years after the program ended.
The screening surveys asked participants where they had heard about BfreeNYC. Thirtynine percent reported hearing about the program from ethnic newspapers, 10 percent from posters or fliers in the community, 5 percent from advertisements on ethnic radio, and 3 percent from television ads. Some participants reported hearing about BfreeNYC from multiple sources; other people did not indicate how they had heard about the program. These findings corresponded to program budget allocations: Almost twice as much money was spent on newspapers compared to other media channels. An additional 24 percent of the participants were informed about the program by their friends or family.
Estimating The Program’s Effectiveness
SCREENING AND VACCINATION PROGRAM
More people were screened through BfreeNYC than through any other citywide screening program in the United States at that time. The number of participants in BfreeNYC far exceeded those of prior screening initiatives in the city.6
In addition to screening, the program provided access to care and collected valuable epidemiologic data. For example, BfreeNYC screened more than 3,700 Chinese (Exhibit 1), approximately 1–2 percent of the adult Chinese population in the city. Approximately 13 percent of the Chinese screened were uninsured,12 and we estimated that as many as 10 percent of uninsured Chinese adults were screened by the program.
These impact estimates take into account only those screened directly by BfreeNYC, but the program’s awareness campaign may also have motivated additional people to be screened by other health care providers. The New York City Department of Health’s surveillance statistics on newly diagnosed hepatitis B cases provided indirect support for BfreeNYC’s local impact.13 Three percent percent of the 51,465 cases of chronic hepatitis B infection reported between2005 and 2008in the city were directly screened by BfreeNYC. During that period, the number of new cases reported per year from neighborhoods predominantly populated by Asians increased by 34 percent, from 2,997 to 4,010 cases, which suggests an expanded reach of the program’s message. New case reports declined by 10 percent in 2009, one year after the program ended.14
VACCINATION RATES
A good measure of the effectiveness of a hepatitis B vaccination program is the rate of completion of the full three-dose vaccination series. Completion rates were high compared to rates published by other groups [please provide].15,16 The results suggest that the program’s case management and followup protocols were effective.
RETENTION IN CARE
In year 1 of the program, patient retention rates were low. Rates increased in subsequent years with increased staffing and case management. The mean length of time for follow-up care for patients at the community health center was longer than at the specialty clinic (forty months versus twenty-six months, respectively). Fifty-seven percent of patients who had hepatitis B and were evaluated were still in care at the end of the program; the retention rate was 72 percent at the community health center and 49 percent at the two public clinics.
At the end of the program, patients were provided with continuing care at both Bellevue Hospital’s specialty clinic and the Charles B. Wang Community Health Center at the standard sliding-scale out-of-pocket fee for uninsured patients. Retention rates dropped in both facilities. However, the decline was less steep at the community health center (13 percent versus 31 percent), in part because of additional funding for support services.
Although appropriate evaluations and surveillance tests were delivered to almost all infected participants, retaining patients in care was difficult. However, the lost-to-follow-up rate was comparable to general outpatient turnover rates in the two public clinic sites.
EFFECT ON MORBIDITY AND MORTALITY
Given the slow progression of chronic hepatitis B disease to end-stage liver disease and liver cancer, the effect of this short-term pilot program on morbidity and mortality is difficult to assess.
Six patients were diagnosed with liver cancer by routine screening over the course of the program and were treated according to the standard of care. Twenty-two cases of end-stage liver disease were detected, and those patients were started on antiviral medication. Survival rates are higher when cancer and end-stage liver disease are diagnosed and treated at earlier stages, and published studies show that the delivery of appropriate care reduces morbidity and mortality.17–20 Thus, the identification and provision of early care would seem likely to reduce long-term morbidity and mortality.
COST OF CARE
Costs of evaluation, care, and treatment with antiviral medication were high, largely because of the fixed costs of laboratory tests, radiologic procedures, and antiviral medications. The program’s average cost of care– $1,598 per year per infected patient–is comparable to that cited in other published reports.17 Providing care and treatment to people with hepatitis B infection has been shown to be a highly cost-effective use of health care spending, “buying” additional years of healthy, productive life at a lower cost than required for many comparable interventions.17,18 However, because of the chronic nature and slow progression of the disease, we were unable to assess our program’s cost-effectiveness.
Local And National Impact
Through its education and screening campaigns, annual epidemiological reports to the New York City Council and Department of Health, and citations in the ethnic press, BfreeNYC increased hepatitis B awareness among city residents, policy makers, and health care providers. The program’s visibility was further raised after it was showcased on PBS’s NewsHour21 and the front page of the New York Times.14
BfreeNYC was the first US program to use a comprehensive approach that included providing care to people infected with hepatitis B. The prior national strategy for preventing hepatitis B transmission had focused on vaccination programs for at-risk groups. This shift from vaccination to care has become more generalized, as is shown in the recently updated hepatitis B screening and vaccination recommendations issued by the Centers for Disease Control and Prevention (CDC).3
In 2006 BFreeNYC, in collaboration with the CDC, reported rates of chronic hepatitis B at around 15 percent in New York City’s Asian American population. These rates were based on an analysis of newly screened participants– a group that was found to provide more generalizable prevalence estimates.4,11 These estimates, which were higher than rates reported in other areas of the United States,22,23 have been cited in the CDC recommendations3 and the Institute of Medicine report.2
In 2008 the CDC awarded BfreeNYC a grant to establish, in collaboration with community partners, the National Center of Excellence in the Elimination of Hepatitis B Disparities (B Free CEED), housed at New York University’s School of Medicine.24 The aim of the center is to identify, develop, and disseminate effective strategies for addressing hepatitis B–related health disparities and to provide pilot funding and technical assistance to underserved, at-risk communities across the country to assist them in reducing hepatitis B disparities.
Lessons Learned And Policy Implications
BfreeNYC devised an innovative and inclusive pilot program to address an important health disparity. To succeed, the program required an infrastructure to support the training of providers, delivery of culturally and linguistically tailored services, and referral services for specialty care. Implementation was time- and resourceintensive and required fair reimbursement rates to obtain institutions’ participation.
BfreeNYC benefited from visionary community leaders; expert physicians; a policy maker champion in the form of Alan Gerson, the New York City Council member; and a thriving city economy. Although these conditions are difficult to reproduce, the lessons learned from BfreeNYC can inform current national hepatitis B efforts, such as the national viral hepatitis action plan released by the Department of Health and Human Services in May 2011.16
Raising Awareness
Lack of knowledge, widespread misinformation, and cultural stigma that persist in the community are important obstacles to hepatitis B prevention and treatment that need to be addressed by education and awareness campaigns. Campaigns involving the community and addressing cultural perceptions about disease are key to raising awareness and dismantling stigma at the community level.
Although BfreeNYC’s findings indicate that the use of ethnic media channels can be an effective way to reach the ethnic community, additional studies are needed to assess the most effective use of this media.
Providing Comprehensive Care
Hepatitis B requires long-term, costly care. Most participants were uninsured, and costs represented a significant barrier to care. Reduced-rate fees were provided, but a drop-off in patient retention occurred at the program’s end.
The Affordable Care Act of 2010 should provide access to care and offset out-of-pocket costs for a significant proportion of people infected with hepatitis B. However, it is essential that basic hepatitis B services–including screening tests and vaccination–be covered as preventive care, along with laboratory tests and medication. Even with the Affordable Care Act, some at-risk and infected people will continue to be uninsured.
To obtain the benefits of care, adherence to the treatment regimen is critical. Delivering culturally appropriate care ensures better communication between patient and provider and better understanding and compliance on the part of the patient. Previous studies have found that the best compliance was obtained by trusted community-based organizations and medical centers with established culturally appropriate services.25,26 Reproducing these results on a larger scale will require additional studies to uncover the key factors that result in compliance and a collaborative approach involving diverse stakeholders.
Building The Capacity For Care
Main-streaming hepatitis B diagnosis and treatment into primary care is crucial to effectively reaching those at risk, and additional education of primary care providers will help improve hepatitis B care. Community screening programs are generally inefficient because care is complex and expensive. Training of primary care providers was crucial for effectiveness of this program. Similar models, such as the Extension for Community Healthcare Outcomes program for hepatitis C,27 also support the increased collaboration between primary care providers and specialists to reach underserved populations with complicated health problems. The customization of the electronic health records carried out at the community health center allowed delivery of standardized care through programmed protocols and reminders for physicians. It also gave care managers and providers the clinical data critical to improving patient retention.
Strengthening The Collection Of Epidemiologic Data
Currently there is no systematic surveillance of chronic hepatitis B, nor are there adequate data on the prevalence of chronic hepatitis B among high-risk groups such as Asian Americans. Until that situation changes, pooled data of hepatitis B screening programs that collect standard demographic data are a valuable source of information for estimating the prevalence and burden of disease in Asian Americans– a group that is underrepresented in national surveys such as the National Health and Nutrition Examination Survey.16,28
Conducting Program Evaluations
Evaluation, facilitated by a central or linked electronic database as used by BfreeNYC, is critical for understanding and assessing any program. It allows for the development of effective evidence-based strategies and increases the ability to conduct comparative effectiveness studies to further enhance service delivery and patient outcomes.
Conclusion
Hepatitis B infection continues to remain a large problem in US Asian American immigrant populations, heightened by the lack of knowledge and misinformation about the disease, as well as by the limited financial and linguistic resources of this population. Reducing hepatitis B–related health disparities requires a comprehensive approach. Screening is important, but linking screening to care and providing care for the infected are crucial.
The lessons learned from BfreeNYC may help inform current and future initiatives. Wellplanned and well-organized community screening projects involving strategic partnerships can be effective in mobilizing populations and reducing disparities. More important, they demonstrate an effective way to raise awareness about hepatitis B at the community level, using culturally appropriate and meaningful ways to reach populations that are most affected. However, this effort needs to be coupled with system-level and policy changes to establish an infrastructure for the delivery of effective care to those who are at risk or affected by hepatitis B.
Implementing that infrastructure will require substantial funds. But only with such changes will we see the long-term benefits of early comprehensive care and a reduction in the national burden of hepatitis B.
BfreeNYC devised an innovative and inclusive pilot program to address an important health disparity.
It is essential that basic hepatitis B services be covered as preventive care.
Acknowledgments
This article was made possible by grants from the National Center on Minority Health and Health Disparities (NCMHD) (No. P60 MD000538) and the Centers for Disease Control and Prevention (CDC) (No. U58DP001022). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCMHD and the CDC. A grant from the New York City Office of the City Council supported the program development and implementation and dissemination efforts of BfreeNYC. The authors thank all of the partner organizations of BfreeNYC, which are listed in Appendix Exhibit 1 (see Note 8 in text), for their important contributions to this program. The authors also thank Thomas Tsang, Alex Sherman, M. Ruchel Ramos, Hillel Tobias, and Mariano Rey, who played crucial roles in developing and steering BfreeNYC.
Biography
Henry Pollack is an associate professor at the New York University School of Medicine and Bellevue Hospital.
In this month’s Health Affairs, Henry Pollack and coauthors, many of them from the New York University (NYU) School of Medicine, describe the results of an evaluation of BfreeNYC. This was a New York City pilot program that, from 2004 to 2008, provided hepatitis B community education and awareness, free screening and vaccinations, and free or low-cost treatment, primarily to immigrants from Asia, Africa, and the Caribbean. The authors’ assessment is that the program was effective in reaching the target population and could be a model for addressing hepatitis B disparities across the United States.
Pollack is an associate professor of pediatrics in the Division of Infectious Diseases and Immunology, NYU School of Medicine and Bellevue Hospital. He is also director of hepatitis research at the university’s Center for the Study of Asian American Health and scientific director of the Center for Excellence in the Elimination of Hepatitis B Disparities in Asian Americans.
Pollack has been a member of the executive committee of the National Task Force on Hepatitis B and of the steering committee of the National Viral Hepatitis Roundtable. He received his medical degree from Université Louis Pasteur, in Strasbourg, France.

Su Wang is the assistant director of medical affairs at the Charles B. Wang Community Health Center.
Su Wang is the assistant director of medical affairs at the Charles B. Wang Community Health Center, which serves the Asian population of the greater New York City area. Wang directs the center’s hepatitis B activities. She trained in internal medicine and pediatrics at Georgetown University and has a master of public health degree from the Johns Hopkins Bloomberg School of Public Health.

Laura Wyatt is the research data manager at the NYU Center for the Study of Asian American Health.
Laura Wyatt is the research data manager at the NYU Center for the Study of Asian American Health. She provides epidemiological and biostatistical support for grant development activities in the center. Wyatt received a master of public health degree in epidemiology from Columbia University’s Mailman School of Public Health.

Chia-hui Peng is a data manager in the Division of Pediatric Infectious Diseases, NYU School of Medicine.
Chia-hui Peng is a data manager in the Division of Pediatric Infectious Diseases at the New York University School of Medicine. She holds a master of public health degree in epidemiology from the Mailman School.

Kejia Wan is a research coordinator in the Division of Pediatric Infectious Diseases, NYU School of Medicine.
Kejia Wan has been a research coordinator in the Division of Pediatric Infectious Diseases at the NYU School of Medicine since 2004. She obtained a master of public health degree with a concentration in health policy and management from the Mailman School.

Chau Trinh-Shevrin is the director and one of the founders of the NYU Center for the Study of Asian American Health.
Chau Trinh-Shevrin is the director and one of the founders of the NYU Center for the Study of Asian American Health. Trinh-Shevrin is a social epidemiologist with a master’s degree in health policy and management from the State University of New York at Albany and a doctorate in public 12 health from the Mailman School.

Kay Chun is the program director of the Public Health and Research Center at Korean Community Services.
Kay Chun is the program director of the Public Health and Research Center at Korean Community Services. She received her bachelor’s degree in chemistry from Creighton University and her medical degree from Yonsei University College of Medicine, in Seoul, Korea.

Simona Kwon is an assistant professor at the NYU School of Medicine.
Simona Kwon is an assistant professor in the Department of General Internal Medicine at the NYU School of Medicine and the director of the National Center of Excellence in the Elimination of Hepatitis B Disparities. She earned a master of public health degree in epidemiology from Yale University 13 and a doctorate in public health from the Division of Sociomedical Sciences at the Mailman School.
Contributor Information
Henry Pollack, (henry.pollack@gmail.com) is an associate professor of pediatrics in the Division of Infectious Diseases and Immunology, New York University School of Medicine and Bellevue Hospital, in New York City..
Su Wang, is the assistant director of medical affairs at the Charles B. Wang Community Health Center, in New York City..
Laura Wyatt, is the research data manager at the New York University Center for the Study of Asian American Health, in New York City..
Chia-hui Peng, is a data manager in the Division of Pediatric Infectious Diseases, New York University School of Medicine..
Kejia Wan, is a research coordinator in the Division of Pediatric Infectious Diseases, New York University School of Medicine..
Chau Trinh-Shevrin, is the director and one of the original founders of the New York University Center for the Study of Asian American Health..
Kay Chun, is the program director of the Public Health and Research Center at the Korean Community Services, 2 in New York City.
Simona Kwon, is an assistant professor in the Department of General Internal Medicine, New York University School of Medicine..
NOTES
- 1.El-Serag HB, Mason AC. Risk factors for the rising rates of primary liver cancer in the United States. Arch Intern Med. 2000;160(21):3227–30. doi: 10.1001/archinte.160.21.3227. [DOI] [PubMed] [Google Scholar]
- 2.Colvin HM, Mitchell AE, editors. Hepatitis and liver cancer: a national strategy for prevention and control of hepatitis B and C. National Academies Press; Washington (DC): 2010. [PubMed] [Google Scholar]
- 3.Weinbaum CM, Williams I, Mast EE, Wang SA, Finelli L, Wasley A, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;57(RR-8):1–20. [PubMed] [Google Scholar]
- 4.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46(4):1034–40. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 5.Trinh-Shevrin C, Pollack HJ, Tsang T, Park J, Ramos MR, Islam N, et al. The Asian American Hepatitis B Program: building a coalition to address hepatitis B disparities. Prog Community Health Partners. 2011 doi: 10.1353/cpr.2011.0039. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poon E. Findings from hepatitis B screenings among Chinese children in New York City. Asian Am Pac Isl J Health. 1998;6(2):219. [PubMed] [Google Scholar]
- 7.New York City Council . City Council fiscal 2004 adopted expense budget. The Council; New York (NY): Jun, 2004. p. 830. [Google Scholar]
- 8.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 9.Lok AS, McMahon BJ. Practice Guidelines Committee, American Association for the Study of Liver Diseases. Chronic hepatitis B. Hepatology. 2001;34(6):1225–41. doi: 10.1053/jhep.2001.29401. [DOI] [PubMed] [Google Scholar]
- 10.Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2007;45(2):507–39. doi: 10.1002/hep.21513. [DOI] [PubMed] [Google Scholar]
- 11.Screening for chronic hepatitis B among Asian/Pacific Islander populations– New York City, 2005. MMWR Morb Mortal Wkly Rep. 2006;55(18):505–9. [PubMed] [Google Scholar]
- 12.Liao Y, Bang D, Cosgrove S, Dulin R, Harris Z, Taylor A, et al. Surveillance of health status in minority communities– Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. MMWR Surveill Summ. 2011;60(6):1–44. [PubMed] [Google Scholar]
- 13.New York City Department of Health and Mental Hygiene, Division of Disease Control Bureau of Communicable Diseases . Hepatitis A, B, and C surveillance report: New York City, 2008 and 2009. The Department; New York (NY): 2010. [Google Scholar]
- 14.Perez-Pena R. Hepatitis risk for East Asians in New York. New York Times. 2006 May 11; [Google Scholar]
- 15.Bailey MB, Shiau R, Zola J, Fernyak SE, Fang T, So SK, et al. San Francisco hep B free: a grassroots community coalition to prevent hepatitis B and liver cancer. J Comm Health. 2010;36(4):538–51. doi: 10.1007/s10900-010-9339-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of Health and Human Services. Combating the silent epidemic of viral hepatitis: action plan for the prevention, care, and treatment of viral hepatitis [Internet] HHS; Washington (DC): 2011. [cited 2011 Sep 7]. Available from: http://www.hhs.gov/ash/initiatives/hepatitis/actionplan_viralhepatitis2011.pdf. [Google Scholar]
- 17.Eckman MH, Kaiser TE, Sherman KE. The cost-effectiveness of screening for chronic hepatitis B infection in the United States. Clin Infect Dis. 2011;52(11):1294–306. doi: 10.1093/cid/cir199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Post SE, Sodhi NK, Peng CH, Wan K, Pollack HJ. A simulation shows that early treatment of chronic hepatitis B infection can cut deaths and be cost-effective. Health Aff (Millwood) 2011;30(2):340–8. doi: 10.1377/hlthaff.2008.0905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong WW, Woo G, Heathcote EJ, Krahn M. Cost effectiveness of screening immigrants for hepatitis B. Liver Int. 2011;31(8):1179–90. doi: 10.1111/j.1478-3231.2011.02559.x. [DOI] [PubMed] [Google Scholar]
- 20.Veldhuijzen IK, Toy M, Hahne SJ, De Wit GA, Schalm SW, de Man RA, et al. Screening and early treatment of migrants for chronic hepatitis B virus infection is cost-effective. Gastroenterology. 2010;138(2):522–30. doi: 10.1053/j.gastro.2009.10.039. [DOI] [PubMed] [Google Scholar]
- 21.PBS NewsHour. Vaccination, education key to stemming Asian hepatitis outbreaks. Public Broadcasting Service; New York (NY): 2010. [Google Scholar]
- 22.Chang ET, Sue E, Zola J, So SK. Three for Life: a model pilot program to prevent hepatitis B virus infection and liver cancer in Asian and Pacific Islander Americans. Am J Health Promot. 2009;23(3):176–81. doi: 10.4278/ajhp.071025115. [DOI] [PubMed] [Google Scholar]
- 23.Kim WR. Epidemiology of hepatitis B in the United States. Hepatology. 2009;49(5 Suppl):S28–34. doi: 10.1002/hep.22975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.B Free CEED: National Center of Excellence in the Elimination of Hepatitis B Disparities [home page on the Internet] New York University Langone Medical Center; New York (NY): [cited 2011 Sep 20]. Available from: http://hepatitis.med.nyu.edu/ [Google Scholar]
- 25.Ngo-Metzger Q, Massagli MP, Clarridge BR, Manocchia M, Davis RB, Iezzoni LI, et al. Linguistic and cultural barriers to care. J Gen Intern Med. 2003;18(1):44–52. doi: 10.1046/j.1525-1497.2003.20205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee H, Tom C. Asian American and Pacific Islander provider and community concerns with rapid managed care growth. Asian Am Pac Isl J Health. 1996;4(1-3):222. [PubMed] [Google Scholar]
- 27.Arora S, Thornton K, Murata G, Deming P, Kalishman S, Dion D, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199–207. doi: 10.1056/NEJMoa1009370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pollack H. Oral presentation at: White House Initiative on Asian Americans and Pacific Islanders. Washington, DC: Dec 10, 2010. Informing hepatitis B policy through the development of a national data screening repository. [Google Scholar]


