Abstract
Generalized anxiety disorder (GAD) and substance use disorders (SUDs) are highly comorbid, and GAD-SUD comorbidity is associated with a host of poor psychosocial outcomes, including higher rates of hospitalization, disability, functional impairment, and inferior GAD and SUD treatment outcomes. Despite the noted severity of this group and clinical implications, current research is limited in a few distinct ways; studies have rarely utilized a longitudinal design and non-treatment seeking individuals to examine how GAD comorbidity impacts SUD outcomes over time. The current study utilized a nationally representative sample of individuals in the U.S. assessed in the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) at Wave 1 (2001–2002) and Wave 2 (2004–2005), comparing individuals who met criteria for both DSM-IV past year GAD and SUD (n = 286) and those who met criteria for past year SUD only without GAD (n = 5,730) at Wave 1. Results indicated that GAD-SUD individuals were significantly more severe than the SUD only group across almost all outcomes assessed (with the exception of alcohol frequency); individuals with GAD-SUD had a more severe psychiatric history, worse health-related quality of life at both waves, and greater incidence of new Axis I disorders, higher rates of treatment-seeking, and greater self-reported drug use at the follow-up. The current study is the first to compare individuals with SUD with and without comorbid GAD over time using a nationally representative sample. Findings further support the clinical severity of this group and suggest the need for GAD-SUD treatment options.
Keywords: generalized anxiety disorder, substance use disorder, health-related quality of life, treatment-seeking, substance use outcomes, epidemiology
Introduction
Generalized anxiety disorder (GAD) and substance use disorders (SUDs) are highly comorbid (Conway et al., 2006; Grant et al., 2004; 2005; Kessler et al., 2005), and individuals with GAD-SUD comorbidity have significantly worse outcomes than single-diagnosis counterparts (Smith & Book, 2010). The presence of co-occurring GAD is associated with heavy drinking, poor social adjustment and functioning, greater disability, and frequent hospitalizations (Burns et al., 2005; Grant et al., 2005). Comorbid GAD, particularly excessive worry, also significantly interferes with substance abuse treatment (Smith & Book, 2010). Compared to other anxiety disorders, GAD seems to be more strongly related to current substance use and associated with greater levels of impairment. In an examination of the relationship between 12-month drug dependence and commonly co-occurring anxiety disorders (i.e., GAD, panic disorder with and without agoraphobia, social phobia, specific phobia), only GAD was significantly related to 12-month drug dependence (as opposed to the other anxiety disorders), even after controlling for other comorbid psychiatric disorders (Compton et al., 2007). Further, even in its pure form, GAD is associated with significantly higher rates of disability and impairment compared to other anxiety disorders (Grant et al., 2005). GAD-SUD comorbidity clearly represents a significant clinical challenge due to the severity of symptoms and poor treatment response.
Despite the clinical implications of GAD-SUD comorbidity, a few limitations have hindered research in this area including: (1) studies have largely focused on anxiety disorders more generally and their co-occurrence with SUDs rather than focusing more exclusively on GAD to enable specificity of understanding (cf., Alegria et al., 2010; Grant et al., 2005); and (2) research has been somewhat narrowly focused on clinical samples (Bruce et al., 2005; Smith & Book, 2010). As one step to address these limitations, Alegria et al. (2010) examined psychiatric comorbidity and other clinical correlates in a sample of individuals with GAD, comparing those with and without SUD. The study found that individuals with GAD-SUD demonstrated higher levels of comorbidity, substance use, and disability. This cross-sectional study highlighted the severity of the GAD-SUD group and suggested the need for longitudinal studies to examine outcomes over time. A second important future direction includes testing how comorbid GAD affects substance use outcomes, as studies have largely focused on how SUD comorbidity affects GAD outcomes (Alegria et al., 2010; Bruce et al., 2005).
The current study aims to build on the prior literature to gain a clearer understanding of how GAD impacts psychosocial and treatment outcomes over time among individuals with SUD. We used a nationally representative sample of individuals in the U.S. assessed in the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) at both Wave 1 (2001–2002) and Wave 2 (2004–2005). Specifically, we compared individuals with an SUD-only diagnosis at Wave 1 to those with an SUD-GAD diagnosis at Wave 1. We first compared the lifetime prevalence of psychiatric disorders at Wave 1 across groups. Next, we compared the following from Wave 1 to Wave 2 across both groups: (1) the incidence of Axis I psychiatric disorders; (2) changes in health-related quality of life; and (3) treatment utilization. Finally, we also compared substance use frequency and severity at Wave 2 across groups.
Materials and Methods
Participants and Procedure
Participants were 6,016 respondents assessed in the NESARC at both Wave 1 (2001–2002) and Wave 2 (2004–2005) who were diagnosed with current AUD or SUD at Wave 1 (with or without current GAD). The NESARC target population consisted of civilian, noninstitutionalized adult individuals over 18 years of age residing in households and group quarters. The survey included individuals residing the continental United States, District of Columbia, Alaska, and Hawaii. African Americans, Hispanics, and individuals aged 18 to 24 years of age were oversampled, and data were adjusted to reflect design characteristics of the NESARC survey and to account for oversampling and nonresponse. Face-to-face interviews were conducted by lay interviewers with extensive training and supervision (Grant et al., 2004; 2009). The research protocol and informed consent given to all respondents prior to interviews were approved the U.S. Census Bureau and the U.S. Office of Management and Budget and were in line with the latest version of the Declaration of Helsinki. Informed consent was obtained after the study procedures were fully explained. The Wave 2 interview was conducted approximately 3 years later (mean interval: 36.6 months). Excluding ineligible respondents (e.g., deceased), the Wave 2 response rate was 86.7%, resulting in 34,653 completed interviews. Sample weights were also developed to adjust for Wave 2 nonresponse (Grant et al., 2009). In Wave 1, a total of 351 respondents met criteria for both DSM-IV generalized anxiety disorder (GAD) and substance use disorder (SUD), and 7,074 met criteria for SUD only. Of these, 6,016 participated in Wave 2 (GAD-SUD = 286; SUD only = 5,730) and constitute the sample of the present study.
Assessments
The diagnostic interview used to determine DSM-IV Axis I and II disorders was the Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV; Grant et al., 2001). The AUDADIS-IV is a structured diagnostic interview designed for lay professional interviewers to measure substance use and mental disorders in large-scale surveys. Computer algorithms were used to diagnose all DSM-IV Axis I and II disorders.
Across all Axis I disorders assessed at Wave 1, criteria were assessed according to two time frames: 1) current (past 12 months); and 2) prior to the past 12 months. At Wave 2, criteria for all Axis I disorders were assessed spanning the time period in between Waves 1 and 2, again distinguishing two distinct time frames: 1) current (past 12 months); and 2) prior to the last 12 months but since Wave 1. Test-retest reliability and validity of the AUDADIS-IV measures of the DSM-IV disorders are adequate and have been reported in detail elsewhere (Canino et al., 1999; Compton et al., 2005; Cottler et al., 1997; Grant et al., 2004; 2005).
Substance use disorders (SUDs)
The AUDADIS-IV operationalizes DSM-IV criteria for alcohol and drug abuse and dependence for 10 drug classes (aggregated in this report) (Grant et al., 2004). Consistent with the DSM-IV, diagnoses of alcohol and substance abuse using the AUDADIS-IV require at least 1 of the 4 abuse criteria either in the 12-month period preceding the interview or prior. For dependence (alcohol and other substances), diagnoses require at least 3 of the 7 DSM-IV criteria for dependence during the past 12 months or prior; for the prior diagnoses, the 3 dependence criteria must have occurred within a 1-year period, as outlined in the DSM-IV. We subdivided the sample of individuals with SUD between those with current GAD comorbidity at Wave 1 (GAD-SUD) and those without current GAD comorbidity at Wave 1 (SUD only). The assessment of GAD is described in more detail in the following section. The AUDADIS-IV has shown good to excellent inter-rater and test-retest reliability (k = 0.70–0.84) and validity (Canino et al., 1999) for SUD diagnoses.
Generalized anxiety disorder (GAD)
DSM-IV GAD was diagnosed when individuals reported excessive anxiety and worry across a number of events or activities more days than not for at least 6 months, accompanied by difficulty controlling worry and at least 3 of the other 6 DSM-IV GAD symptoms, including the clinical significance criterion to be met (i.e. the symptoms caused clinically significant distress or impairment). The DSM-IV GAD diagnosis excludes substance-induced episodes or episodes due to a general medical condition. To differentiate between substance-induced and independent disorders, the AUDADIS-IV uses specific questions about chronological relationships between intoxication, withdrawal effects, and the anxiety symptoms, which has been shown to improve reliability and validity of anxiety disorder diagnoses among substance using individuals (Hasin et al., 2006). Test-retest reliability, as reported in detail elsewhere (Canino et al., 1999; Grant et al., 2004; 2005), is fair (k = 0.42).
Other mood and anxiety disorders
The AUDADIS-IV was also used to assess other mood (major depressive disorder, dysthymia, bipolar I, bipolar II) and anxiety (panic disorder, social anxiety disorder, specific phobia) diagnoses at Waves 1 and 2. All diagnoses reported were “primary” such that they exclude disorders characterized as “substance induced” or due to a general medical condition, and they all met the clinical significance criterion.
Personality disorders
The AUDADIS-IV was used to assess all 10 DSM-IV personality disorders in Clusters A, B, and C using algorithms requiring specific numbers of diagnostic criteria as well as long-term maladaptive patterns of cognition, emotion, and functioning (Grant et al., 2004; 2005; 2008; Stinson et al., 2008). Further, at least one symptom reported had to cause distress or social or occupational dysfunction. Avoidant, dependent, histrionic, obsessive-compulsive, paranoid, and schizoid personality disorders were assessed in Wave 1, and borderline, narcissistic, and schizotypal disorders were assessed in Wave 2. Previously published NESARC studies have documented test-retest reliability ranging from fair (paranoid, histrionic, avoidant; k = 0.40–0.45) to good (schizotypal, antisocial, narcissistic, borderline; k = 0.67–0.71) (Grant et al., 2003; Ruan et al., 2008) with good convergent validity (Compton et al., 2005; Grant et al., 2004; 2005; 2008; Stinson et al., 2008).
Health-related quality of life
Health-related quality of life was assessed for both Waves 1 and 2 using the Medical Outcomes Study 12-Item Short-Form Health Survey, Version 2 (SF-12; Ware et al., 1996; 2002), a reliable and valid measure of health-related quality of life used in population surveys. The norm for this measure is 50, with higher scores reflecting higher health-related quality of life (Ware et al., 1996; 2002).
Treatment utilization
Treatment utilization from Wave 1 to Wave 2 assessment was ascertained for both GAD and SUD. Treatment seeking for GAD was assessed by asking participants whether since the last interview they had gone to a professional, ER, or hospital overnight or had been prescribed any medication in the past year to calm them because they were feeling tense, nervous or worried. For SUD, respondents were also asked whether since the last interview they had received treatment for substance use through any of the following: 12-step programs; detoxification, inpatient, or emergency room services; outpatient, rehabilitation or methadone maintenance; a halfway house, crisis center, employment assistance program, or family services agency; clergy; or private physician. Respondents were also asked whether since the last interview there was a time they thought they should see someone for their substance use but did not.
Substance use frequency
Frequency of use of alcohol and other substances was assessed at Waves 1 and 2. At Wave 2, individuals were classified based upon whether they used drugs since the last interview (yes/no), and regarding alcohol use, they were asked about frequency of drinking any kind of alcoholic beverage in the last 12 months. Response options were collapsed across categories to capture as full a spread of scores as possible but to also avoid categories with few members; categories included the following: 1) every day to two times per week; 2) once per week to 2 to 3 times per month; and 3) once per month to 1–2 times in the last year.
Statistical analyses
Weighted percentages and means were computed to derive sociodemographic characteristics, lifetime prevalence of Axis I and II disorders, incidence of Axis I disorders, health-related quality of life, treatment utilization, and substance use frequency at Wave 1 and Wave 2 for respondents with SUD with and without comorbid GAD at Wave 1. A set of logistic regression analyses yielded odds ratios (ORs) and 95% confidence intervals (CIs) indicating measures of association between SUD-GAD and SUD only and lifetime comorbid psychiatric disorders, incidence of Axis I disorders, treatment utilization, and substance use frequency. Odds ratios were further adjusted (AOR) for those sociodemographic characteristics of the sample at Wave 1 that were significantly different between the groups in the univariate analyses. Paired t-tests were used to test change in health-related quality of life over time in both groups. Analyses were estimated using SUDAAN to adjust for the design effects of the NESARC.
Results
Sociodemographic characteristics
Table 1 shows the sociodemographic characteristics of individuals with current SUD with and without current GAD at Wave 1. Individuals with GAD-SUD at Wave 1 were significantly more likely than individuals with SUD only to have less than or equal to a high school education, to be unemployed, to be separated/widowed/divorced, and to have public insurance. Individuals with GAD-SUD at Wave 1 were significantly less likely to be male and to have income ≥ 35,000 compared to individuals with SUD only.
Table 1.
Sociodemographic characteristics at Wave 1 among all individuals
| Wave 1 Characteristic | All SUD subjects (at Wave 1 past year) | GAD-SUD (Wave 1 past year) | SUD only (at Wave 1 past year)(ref) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N=6016 | N=286; total %=4.45 | N=5730; total %=95.55 | |||||||
| col % | SE | col % | SE | col % | SE | OR | 95%CI | ||
| Sex | |||||||||
| Male | 58.67 | 0.76 | 37.12 | 3.67 | 59.67 | 0.77 | 0.40 | 0.29 | 0.55 |
| Female* | 41.33 | 0.76 | 62.88 | 3.67 | 40.33 | 0.77 | 1.00 | 1.00 | 1.00 |
| Race/Ethnicity | |||||||||
| White* | 76.87 | 1.23 | 78.86 | 2.64 | 76.77 | 1.27 | 1.00 | 1.00 | 1.00 |
| Black | 8.94 | 0.67 | 8.50 | 1.72 | 8.96 | 0.69 | 0.92 | 0.59 | 1.46 |
| Native American | 3.58 | 0.39 | 2.70 | 1.03 | 3.63 | 0.40 | 0.72 | 0.33 | 1.60 |
| Asian | 1.98 | 0.34 | 2.31 | 1.46 | 1.96 | 0.34 | 1.15 | 0.31 | 4.22 |
| Hispanic | 8.64 | 0.95 | 7.62 | 1.49 | 8.68 | 0.98 | 0.85 | 0.54 | 1.35 |
| Nativity | |||||||||
| US-born* | 93.59 | 0.65 | 94.09 | 1.73 | 93.57 | 0.65 | 1.00 | 1.00 | 1.00 |
| Foreign-born | 6.41 | 0.65 | 5.91 | 1.73 | 6.43 | 0.65 | 0.91 | 0.50 | 1.66 |
| Age | |||||||||
| 18–29* | 32.17 | 0.87 | 31.02 | 3.71 | 32.22 | 0.89 | 1.00 | 1.00 | 1.00 |
| 30–44 | 36.02 | 0.80 | 44.47 | 3.74 | 35.62 | 0.81 | 1.30 | 0.88 | 1.90 |
| 45–64 | 27.33 | 0.75 | 22.11 | 2.79 | 27.57 | 0.77 | 0.83 | 0.55 | 1.26 |
| 65+ | 4.49 | 0.30 | 2.40 | 0.89 | 4.59 | 0.31 | 0.54 | 0.24 | 1.24 |
| Education | |||||||||
| < High School | 15.70 | 0.66 | 19.77 | 3.03 | 15.51 | 0.67 | 1.66 | 1.09 | 2.55 |
| High School | 32.65 | 0.82 | 40.24 | 3.73 | 32.30 | 0.83 | 1.63 | 1.16 | 2.29 |
| College* | 51.65 | 0.89 | 39.99 | 3.78 | 52.20 | 0.89 | 1.00 | 1.00 | 1.00 |
| Individual Income | |||||||||
| 0–19K* | 47.32 | 0.84 | 60.21 | 3.49 | 46.72 | 0.86 | 1.00 | 1.00 | 1.00 |
| 20–34K | 24.35 | 0.74 | 23.96 | 3.36 | 24.37 | 0.76 | 0.76 | 0.52 | 1.12 |
| 35–69K | 21.67 | 0.72 | 13.95 | 2.36 | 22.03 | 0.73 | 0.49 | 0.33 | 0.73 |
| >70K | 6.66 | 0.51 | 1.87 | 1.05 | 6.88 | 0.53 | 0.21 | 0.07 | 0.67 |
| Employment Status | |||||||||
| Employed* | 73.89 | 0.70 | 59.01 | 3.38 | 74.58 | 0.72 | 1.00 | 1.00 | 1.00 |
| Unemployed | 26.11 | 0.70 | 40.99 | 3.38 | 25.42 | 0.72 | 2.04 | 1.52 | 2.73 |
| Marital Status | |||||||||
| Married* | 23.43 | 0.88 | 48.72 | 3.86 | 53.64 | 0.90 | 1.00 | 1.00 | 1.00 |
| Widowed/Divorced | 18.38 | 0.58 | 27.00 | 2.58 | 17.98 | 0.60 | 1.65 | 1.20 | 2.28 |
| Never Married | 28.19 | 0.90 | 24.28 | 3.28 | 28.37 | 0.92 | 0.94 | 0.62 | 1.42 |
| Urbanicity | |||||||||
| Urban* | 76.09 | 1.81 | 76.17 | 3.62 | 76.09 | 1.82 | 1.00 | 1.00 | 1.00 |
| Rural | 23.91 | 1.81 | 23.83 | 3.62 | 23.91 | 1.82 | 1.00 | 0.69 | 1.43 |
| Region | |||||||||
| Northwest | 17.98 | 2.79 | 19.55 | 3.90 | 17.90 | 2.81 | 0.93 | 0.58 | 1.48 |
| Midwest | 28.33 | 3.07 | 27.08 | 4.21 | 28.39 | 3.09 | 0.81 | 0.53 | 1.24 |
| South | 33.56 | 2.81 | 29.81 | 4.04 | 33.73 | 2.84 | 0.75 | 0.50 | 1.12 |
| West* | 20.13 | 2.67 | 23.56 | 4.11 | 19.97 | 2.66 | 1.00 | 1.00 | 1.00 |
| Insurance | |||||||||
| Private* | 65.50 | 0.85 | 52.97 | 3.69 | 66.09 | 0.88 | 1.00 | 1.00 | 1.00 |
| Public | 11.56 | 0.50 | 21.64 | 3.01 | 11.09 | 0.50 | 2.43 | 1.66 | 3.56 |
| No insurance | 22.94 | 0.78 | 25.39 | 3.39 | 22.83 | 0.81 | 1.39 | 0.94 | 2.05 |
reference group
Lifetime prevalence of psychiatric comorbidity
Table 2 shows the lifetime prevalence of Axis I and II disorders at Wave 1 among individuals with SUD with and without GAD. In the unadjusted models, individuals with GAD-SUD were significantly more likely than individuals with SUD only to have a lifetime history of any psychiatric disorder, any Axis I disorder, alcohol dependence, any drug use disorder, drug abuse, drug dependence, nicotine dependence, any mood disorder, major depressive disorder, bipolar I and II disorder, dysthymia, any anxiety disorder, panic disorder, social anxiety disorder, specific phobia, any Axis II disorder, and any Cluster A and B Axis II disorder. Individuals with GAD-SUD were significantly less likely than individuals with SUD only to have a lifetime history of alcohol abuse.
Table 2.
Lifetime prevalence of Axis I and II disorders at Wave 1 among individuals with SUD with and without GAD
| GAD-SUD (at Wave 1 past year) | SUD only (at Wave 1 past year) (ref) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Psychiatric Comorbidity | col % | SE | col % | SE | OR | 95%CI | AOR* | 95%CI | ||
| Any psychiatric disorder | 96.15 | 1.09 | 51.44 | 0.81 | 23.57 | 13.06 | 42.56 | 20.49 | 11.30 | 37.14 |
| Any Axis I disorder | 93.70 | 1.45 | 41.95 | 0.82 | 20.58 | 12.53 | 33.80 | 17.54 | 10.55 | 29.18 |
| Alcohol use disorder | 72.27 | 3.41 | 71.53 | 0.86 | 1.04 | 0.73 | 1.47 | 1.39 | 0.94 | 2.05 |
| Alcohol abuse | 21.61 | 2.71 | 33.16 | 0.84 | 0.56 | 0.40 | 0.77 | 0.65 | 0.46 | 0.91 |
| Alcohol dependence | 50.67 | 3.51 | 38.37 | 0.87 | 1.65 | 1.24 | 2.19 | 1.86 | 1.35 | 2.55 |
| Drug use disorder | 50.94 | 3.66 | 30.44 | 0.81 | 2.37 | 1.77 | 3.18 | 2.48 | 1.82 | 3.36 |
| Drug abuse | 37.58 | 3.39 | 27.40 | 0.80 | 1.60 | 1.18 | 2.16 | 1.66 | 1.19 | 2.30 |
| Drug dependence | 29.19 | 3.44 | 8.06 | 0.48 | 4.70 | 3.40 | 6.50 | 4.48 | 3.19 | 6.31 |
| Nicotine dependence | 81.86 | 3.04 | 70.31 | 0.89 | 1.91 | 1.24 | 2.92 | 1.51 | 0.97 | 2.35 |
| Mood disorder | 83.60 | 2.83 | 29.23 | 0.77 | 12.34 | 8.10 | 18.80 | 10.56 | 6.92 | 16.10 |
| Major depressive disorder | 41.63 | 3.51 | 18.99 | 0.63 | 3.04 | 2.24 | 4.13 | 2.51 | 1.83 | 3.44 |
| Bipolar I | 32.73 | 3.74 | 6.96 | 0.46 | 6.50 | 4.47 | 9.44 | 5.48 | 3.74 | 8.00 |
| Bipolar II | 6.75 | 1.86 | 2.47 | 0.24 | 2.86 | 1.52 | 5.38 | 2.60 | 1.35 | 5.02 |
| Dysthymia | 22.10 | 2.90 | 4.14 | 0.33 | 6.57 | 4.51 | 9.59 | 5.56 | 3.76 | 8.22 |
| Any anxiety disorder | 68.14 | 3.56 | 22.95 | 0.70 | 7.18 | 5.13 | 10.05 | 6.13 | 4.35 | 8.62 |
| Panic disorder | 43.24 | 3.92 | 8.30 | 0.44 | 8.42 | 6.01 | 11.79 | 6.93 | 4.84 | 9.93 |
| Social anxiety disorder | 37.49 | 3.55 | 7.22 | 0.46 | 7.71 | 5.54 | 10.72 | 6.71 | 4.74 | 9.50 |
| specific phobia | 45.75 | 3.47 | 14.42 | 0.63 | 5.00 | 3.74 | 6.69 | 4.11 | 3.05 | 5.55 |
| Any Axis II disorder | 70.91 | 3.22 | 27.24 | 0.75 | 6.51 | 4.70 | 9.03 | 6.20 | 4.44 | 8.67 |
| Cluster A | 45.59 | 3.50 | 11.66 | 0.56 | 6.35 | 4.69 | 8.59 | 5.42 | 3.92 | 7.50 |
| Cluster B | 33.03 | 3.13 | 13.91 | 0.54 | 3.05 | 2.29 | 4.08 | 3.09 | 2.28 | 4.17 |
AOR: adjusted OR, adjusted for wave 1 sociodemographic variables (sex, race, native, age, individual income, employment, marital status, urbanicity)
After adjusting for sociodemographic characteristics (sex, race/ethnicity, nativity, age, individual income, employment, marital status, urbanicity), individuals with GAD-SUD continued to be more likely than those with SUD only to have a lifetime history of any psychiatric disorder, any Axis I disorder, alcohol dependence, any drug use disorder, drug abuse, drug dependence, any mood disorder, major depressive disorder, bipolar I and II disorder, dysthymia, any anxiety disorder, panic disorder, social anxiety disorder, specific phobia, any Axis II disorder, and any Cluster A and B Axis II disorder, but the differences on the prevalence of nicotine dependence failed to reach significance. Individuals with GAD-SUD continued to be significantly less likely than individuals with SUD only to have a lifetime history of alcohol abuse.
Incidence of Axis I disorders
Table 3 shows the incidence of Axis I disorders from Wave 1 to Wave 2 among individuals with SUD with and without GAD. Individuals with GAD-SUD had significantly higher incidence than individuals with SUD only of any Axis I disorder, a mood disorder, bipolar I and II disorder, any anxiety disorder, panic disorder, social anxiety disorder, and specific phobia from Wave 1 to Wave 2.
Table 3.
Incidence of Axis I disorders from Wave 1 to Wave 2 among individuals with SUD with and without GAD
| GAD-SUD (at Wave 1 past year) | SUD only (at Wave 1 past year)(ref) | ||||||
|---|---|---|---|---|---|---|---|
| New Axis I disorder since Wave 1 (incidence after wave 1) | N=286; total %=4.45 | N=5730; total %=95.55 | |||||
| col % | SE | col % | SE | OR | 95%CI | ||
| Any new Axis I disorder | 46.15 | 3.40 | 36.31 | 0.85 | 1.50 | 1.14 | 1.98 |
| Substance Use Disorders | 20.18 | 2.91 | 20.78 | 0.70 | 0.96 | 0.67 | 1.39 |
| Alcohol use disorder | 9.63 | 2.07 | 14.14 | 0.59 | 0.65 | 0.40 | 1.05 |
| Alcohol abuse | 8.65 | 1.94 | 12.91 | 0.63 | 0.64 | 0.38 | 1.06 |
| Alcohol dependence | 5.77 | 2.39 | 8.93 | 0.71 | 0.62 | 0.25 | 1.54 |
| Drug use disorder | 8.17 | 1.91 | 6.12 | 0.47 | 1.36 | 0.81 | 2.31 |
| Drug abuse | 5.54 | 1.68 | 3.85 | 0.32 | 1.46 | 0.76 | 2.81 |
| Drug dependence | 3.04 | 1.07 | 2.84 | 0.33 | 1.07 | 0.50 | 2.29 |
| Nicotine dependence | 24.96 | 8.42 | 12.26 | 1.06 | 2.38 | 0.96 | 5.93 |
| Mood disorder | 15.61 | 2.91 | 9.25 | 0.51 | 1.81 | 1.18 | 2.79 |
| Major depressive disorder | 3.38 | 1.36 | 5.50 | 0.43 | 0.60 | 0.25 | 1.42 |
| Bipolar I | 15.67 | 3.56 | 3.47 | 0.32 | 5.17 | 3.02 | 8.85 |
| Bipolar II | 2.68 | 1.01 | 1.02 | 0.15 | 2.67 | 1.19 | 6.02 |
| Dysthymia | 1.54 | 0.96 | 0.84 | 0.16 | 1.84 | 0.49 | 6.91 |
| Any anxiety disorder | 25.37 | 3.41 | 14.66 | 0.66 | 1.98 | 1.35 | 2.89 |
| GAD | N/A | N/A | 5.36 | 0.37 | N/A | N/A | N/A |
| Panic disorder | 15.38 | 3.96 | 3.59 | 0.33 | 4.88 | 2.57 | 9.25 |
| Social anxiety disorder | 9.56 | 2.35 | 3.58 | 0.35 | 2.85 | 1.61 | 5.03 |
| Specific phobia | 15.97 | 3.45 | 8.28 | 0.46 | 2.11 | 1.23 | 3.60 |
Health-related quality of life
Table 4 shows health-related quality of life at Wave 1 and Wave 2 among individuals with SUD with and without GAD. From Wave 1 to Wave 2, individuals with GAD-SUD showed significant improvements in general health, the mental health component summary, the social functioning scale, and the mental health scale of the SF-12, and significant worsening from Wave 1 to Wave 2 on the role-physical scale of the SF-12. Individuals with SUD only showed significant decreases in almost all SF-12 scales (including the physical health component summary, general health scale, physical functioning scale, role-physical scale, bodily pain, mental health component summary, social functioning scale, and role-emotional scale) from Wave 1 to Wave 2, indicating a worse health-related quality of life at Wave 2 across these scales. Only the mental health scale did not show a significant change from Wave 1 to Wave 2 in the SUD only group.
Table 4.
Health-related quality of life at Wave 1 and Wave 2 among individuals with SUD with and without GAD
| SF-12 scores | GAD-SUD | SUD only | Comparison of Groups and Group × Time Interaction | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N=286; Total %=39.07 | Time difference comparison | N=5730; Total %=65.06 | Time difference comparison | Group | Group × time interaction | |||||||||||
| Mean Wave 1 | SE | Mean Wave 2 | SE | Paired T-test | P | Mean Wave 1 | SE | Mean Wave 2 | SE | Paired T-test | P | Beta | P-value | Beta | P-value | |
| PCS | 46.80 | 1.08 | 45.38 | 1.08 | −1.63 | 0.1049 | 50.89 | 0.18 | 50.35 | 0.21 | −3.36 | 0.0008 | −4.09 | 0.0004 | −0.89 | 0.3265 |
| General health | 41.03 | 1.13 | 42.60 | 1.07 | 1.98 | 0.0485 | 49.55 | 0.22 | 48.90 | 0.22 | −3.80 | 0.0001 | −8.53 | <0.0001 | 2.23 | 0.0081 |
| Physical functioning | 45.78 | 1.04 | 45.20 | 1.04 | −0.64 | 0.5212 | 51.82 | 0.16 | 50.98 | 0.18 | −5.33 | <0.0001 | −6.04 | <0.0001 | 0.26 | 0.7782 |
| Role-physical | 45.09 | 0.95 | 43.23 | 0.98 | −2.14 | 0.0331 | 51.24 | 0.17 | 49.78 | 0.19 | −8.26 | <0.0001 | −6.15 | <0.0001 | −0.40 | 0.6597 |
| Bodily pain | 42.06 | 1.00 | 42.65 | 1.12 | 0.51 | 0.6099 | 49.31 | 0.21 | 49.91 | 0.22 | 2.73 | 0.0064 | −7.24 | <0.0001 | −0.02 | 0.9845 |
| MCS | 37.04 | 1.02 | 40.42 | 0.94 | 3.02 | 0.0028 | 50.49 | 0.16 | 49.66 | 0.18 | −4.59 | <0.0001 | −13.45 | <0.0001 | 4.21 | 0.0005 |
| Social functioning | 39.13 | 1.12 | 42.04 | 1.06 | 2.30 | 0.0223 | 50.99 | 0.17 | 50.54 | 0.19 | −2.45 | 0.0143 | −11.87 | <0.0001 | 3.36 | 0.0108 |
| Role-emotional | 38.07 | 1.14 | 39.21 | 0.98 | 0.92 | 0.3563 | 50.36 | 0.17 | 48.34 | 0.19 | −10.04 | <0.0001 | −12.29 | <0.0001 | 3.15 | 0.0142 |
| Mental health | 37.14 | 0.90 | 41.04 | 0.95 | 4.08 | 0.0001 | 49.89 | 0.17 | 50.17 | 0.20 | 1.31 | 0.1898 | −12.75 | <0.0001 | 3.63 | 0.0005 |
There was a significant group by time interaction on the general health scale and the four mental health-related scales (the mental health component summary, social functioning, role-emotional, and mental health scales), indicating that the GAD-SUD group demonstrated significant improvements across these scales from Wave 1 to Wave 2 compared to the SUD only group. Despite these changes over time at both time points the GAD-SUD group had significantly poorer health-related quality of life across all SF-12 subscales.
Treatment utilization
Table 5 shows patterns in treatment utilization between the two waves among individuals with SUD with and without GAD. Individuals with GAD-SUD were significantly more likely to have sought treatment for substance use at a 12-step program, detoxification/inpatient/ER, halfway house/crisis center/employment assistance program/family services agency, clergy, and private physician compared to individuals with SUD only. Individuals with GAD-SUD were also significantly more likely to report having a time when they thought they should have seen someone but did not go compared to individuals with SUD only. Not surprisingly, individuals with GAD-SUD were significantly more likely to report going to a professional due to feelings of being tense, nervous, or worried, having a doctor prescribe medication to calm oneself, or seeking any type of treatment for GAD compared to individuals with SUD only.
Table 5.
Treatment utilization between Wave 1 and Wave 2 among individuals with SUD with and without GAD
| Since Wave 1 Treatment Utilization | GAD-SUD | SUD only (ref) | |||||
|---|---|---|---|---|---|---|---|
| N=286; total %=4.45 | N=5730; total %=95.55 | ||||||
| col % | SE | col % | SE | OR | 95%CI | ||
| Substance Use | |||||||
| Since last interview gone anywhere for help for your substance use? | |||||||
| 12-step | 16.03 | 4.00 | 9.00 | 0.73 | 1.93 | 1.05 | 3.54 |
| Detox/inpatient/ER | 11.15 | 3.31 | 5.53 | 0.66 | 2.14 | 1.05 | 4.36 |
| Outpatient/rehab/methadone maintenance | 10.55 | 3.45 | 7.05 | 0.71 | 1.56 | 0.73 | 3.31 |
| Halfway house/crisis center/EAP/family services agency | 11.18 | 3.56 | 4.78 | 0.57 | 2.51 | 1.19 | 5.30 |
| Clergy | 9.35 | 3.10 | 2.04 | 0.40 | 4.95 | 2.13 | 11.50 |
| Private physician | 20.40 | 4.96 | 7.55 | 0.75 | 3.14 | 1.68 | 5.88 |
| Time that you thought you should see someone but didn’t go? | 26.34 | 5.01 | 12.68 | 0.88 | 2.46 | 1.44 | 4.22 |
| Anxiety | |||||||
| Did you go to professional because you were feeling tense, nervous or worried? | 58.26 | 7.39 | 32.61 | 3.04 | 2.88 | 1.50 | 5.56 |
| Go to an ER because you were feeling tense, nervous or worried? | 9.65 | 3.74 | 5.17 | 1.44 | 1.96 | 0.66 | 5.79 |
| Hospital overnight because of tense, nervous, worried? | 4.17 | 2.18 | 3.41 | 1.10 | 1.23 | 0.35 | 4.41 |
| Doctor prescribe medication to calm you? | 52.14 | 7.33 | 34.27 | 3.01 | 2.09 | 1.06 | 4.11 |
| Any treatment seeking for GAD | 66.38 | 7.48 | 43.69 | 3.44 | 2.54 | 1.20 | 5.42 |
Substance use frequency
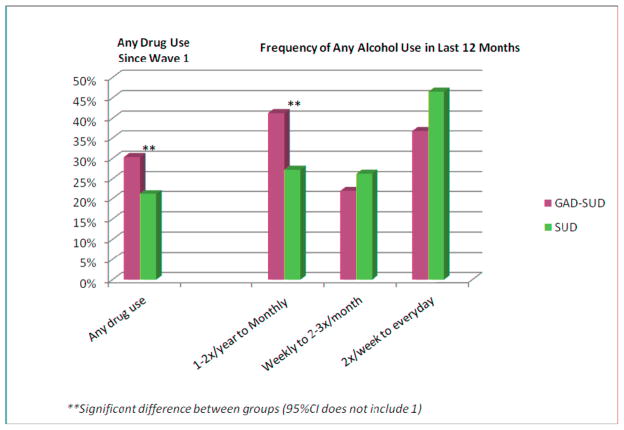
Figure 1 shows substance use frequency at Wave 2 among individuals with SUD with and without GAD. Individuals with GAD-SUD were significantly more likely to report drug use since Wave 1 compared to the SUD only group (OR = 1.62, 95% CI = 1.18–2.22). Regarding alcohol use frequency, individuals with GAD-SUD were significantly more likely to report a lower frequency of drinking (once per month to 1 to 2 times in the last year) compared to the SUD only group (OR = 1.92, 95% CI = 1.32–2.81).
Figure 1.
Alcohol and drug use frequency at Wave 2 among individuals with SUD with and without GAD
Discussion
Previous research has consistently demonstrated a strong association between GAD and SUD (Grant et al., 2005), and GAD-SUD comorbidity is associated with significant impairment and poor psychosocial outcomes (Smith & Book, 2010). The current study is the first to compare individuals with SUD with and without comorbid GAD over time using a nationally representative sample of the general population. We compared the GAD-SUD and SUD only groups on psychiatric comorbidity, health-related quality of life, treatment utilization, and substance use frequency over a three year period. Our study found that compared to the SUD only group, GAD-SUD individuals (1) were significantly worse off at Wave 1 in terms of sociodemographic characteristics and psychiatric comorbidity; (2) had significantly higher prevalence (at Wave 1) and higher incidence (from Wave 1 to Wave 2) of almost all Axis I disorders compared to the SUD only group; (3) had significantly worse health-related quality of life at both waves compared to SUD only; (4) were more likely to seek treatment between waves compared to the SUD only group; and (5) were significantly more likely to report drug use since Wave 1 compared to the SUD only group, yet tended to use alcohol less often.
The finding that GAD-SUD individuals were worse off across sociodemographic characteristics is consistent with other studies that have demonstrated impairment associated with GAD comorbidity more generally (Kessler et al., 1999; Wittchen, 2002), as well as comorbidity of GAD with SUD specifically (Alegria et al., 2010; Smith & Book, 2010). This may be due to the impact of GAD on work productivity, employment status, and overall daily functioning (Bobes et al., 2011; Henning et al., 2007), or the overall higher levels of impairment associated with greater comorbidity.
GAD-SUD individuals had a more severe psychiatric history and were also more likely to develop a new Axis I disorder by the second assessment compared to the SUD only group. This higher rate of psychiatric comorbidity in the GAD-SUD group, particularly for internalizing disorders, may reflect a few different possibilities. GAD symptoms may contribute directly to symptoms of other disorders, in line with other studies demonstrating that GAD confers increased risk for other internalizing symptoms (Bruce et al., 2005; Grant et al., 2005). Regarding SUD comorbidity specifically, engaging in substance use may provide temporary relief for anxiety for individuals with GAD, but then may lead to greater impairment and increased risk for other forms of psychopathology. There may also be a shared vulnerability underlying GAD and other internalizing disorders, such that comorbidity may reflect different representations of a single latent factor (Krueger, 1999).
The GAD-SUD group had significantly worse health-related quality of life at both times compared to SUD only. The GAD-SUD group, even after improving from Wave 1 to Wave 2 in mental health-related quality of life, had scores consistently below 50, which was the mean across most scales for the SUD only group. These findings are consistent with other evidence suggesting GAD comorbidity confers increased risk for impairment, poor functioning, and quality of life (Grant et al., 2005), which may be due to the somatic manifestations of GAD and impact on physical discomfort and pain (Bobes et al., 2011), as well as the impact of GAD on numerous areas of one’s life, including work performance (Kessler et al., 1999; Wittchen, 2002) and social functioning (Henning et al., 2007) that often subsists even following treatment for individuals with GAD (Bobes et al., 2011).
Individuals with GAD-SUD had higher rates of treatment seeking across mental health and SUD treatment services compared to individuals with SUD only. Lower health-related quality life, greater impairment associated with numerous comorbidities and presence of internalizing disorders may encourage individuals to seek treatment (Bland et al., 1997; Mojtabai et al., 2002), and increase the likelihood of being referred to specialized treatment services if these diagnoses are detected in primary care. Treatment-seeking may be another indicator of severity for GAD-SUD individuals, also contributing to significant societal costs from frequent service utilization. However, it could also be viewed as adaptive particularly given the higher rates of impairment and distress in this group. Treatment seeking may have contributed to improvements in functioning from Wave 1 to Wave 2; yet it is noteworthy that despite seeking treatment, this group was still worse off at Wave 2 (e.g., regarding health-related quality of life) compared to the SUD only group.
Individuals with GAD-SUD were significantly more likely to report drug use since Wave 1 compared to the SUD only group, consistent with other studies in this area indicating that GAD is associated with high rates of co-occurring drug dependence (Grant et al., 2005). By contrast, individuals with GAD-SUD were significantly more likely to report a lower frequency of drinking than the SUD only group. These findings may be interpreted in line with our findings that individuals with GAD-SUD were more likely to meet criteria for lifetime drug abuse and dependence at Wave 1 but there were no significant differences in rates of lifetime alcohol use disorders at Wave 1 across groups or in the incidence of alcohol abuse or dependence between Waves 1 and 2. Overall, our data suggest that in this sample, individuals with GAD-SUD and those with SUD only did not have as distinct differences in severity for alcohol as opposed to other substances; however, future research is needed that separates AUD and SUD diagnoses to further clarify these relationships.
Our findings should be interpreted in light of both study strengths and limitations. Strengths include the use of epidemiological sampling to obtain a large nationally representative sample of adults with SUD and GAD ascertained independently of treatment seeking, a prospective design, and high retention rates over a 3-year follow up period. Limitations include reliance on a single follow-up period, modest reliability of the GAD diagnoses assessed with the AUDADIS-IV, and inclusion of only civilian households and group quarters of adults 18 years and older. Despite these limitations, these findings have important implications. The severity of the GAD-SUD group suggests the need to incorporate treatment of GAD into substance abuse treatment, for instance using psychosocial approaches and/or selective serotonin reuptake inhibitors (SSRIs) that have been shown to be efficacious in treating GAD yet do not share the same risk for abuse as benzodiazepines (Back & Brady, 2008). Continued longitudinal work is also necessary to inform etiological understanding, particularly studies that span the life course and incorporate a comprehensive assessment of environmental and biological factors to better understand the sequencing of these disorders and shared vulnerabilities. This work may inform clinical approaches by providing a framework for treatment to target underlying vulnerabilities that cut across diagnostic categories rather than addressing the symptoms of GAD, SUD, and other comorbid conditions in isolation.
Acknowledgments
The National Epidemiologic Survey on Alcohol and Related Conditions was sponsored by the National Institute on Alcohol Abuse and Alcoholism with supplemental support from the National Institute on Drug Abuse.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jessica F. Magidson, Email: jmagidso@umd.edu, Center for Addictions, Personality, and Emotion Research, 2103 Cole Field House, University of Maryland, College Park, College Park, MD 20742, Phone: (301) 405-8441, Fax: (301) 405-3223
Shang-Min Liu, New York State Psychiatric Institute, 1051 Riverside Drive, New York, NY 10032
C.W. Lejuez, Center for Addictions, Personality, and Emotion Research, 2103 Cole Field House, University of Maryland, College Park, College Park, MD 20742
Carlos Blanco, Department of Psychiatry, Columbia University, New York State Psychiatric Institute, 1051 Riverside Drive, New York, NY 10032
References
- Alegria AA, Hasin DS, Nunes EV, Liu SM, Davies C, Grant BF, Blanco C. Comorbidity of generalized anxiety disorder and substance use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2010;71:1187–1195. doi: 10.4088/JCP.09m05328gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back SE, Brady KT. Anxiety disorders with comorbid substance use disorders: diagnostic and treatment considerations. Psychiatric Annals. 2008;38:724–729. doi: 10.3928/00485713-20081101-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland RC, Newman SC, Orn H. Help-seeking for psychiatric disorders. The Canadian Journal of Psychiatry. 1997;42:935–942. doi: 10.1177/070674379704200904. [DOI] [PubMed] [Google Scholar]
- Bobes J, Caballero L, Vilardaga I, Rejas J. Disability and health-related quality of life in outpatients with generalised anxiety disorder treated in psychiatric clinics: is there still room for improvement? Annals of General Psychiatry. 2011;10:7. doi: 10.1186/1744-859X-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, Shea MT, Keller MB. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. The American Journal of Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns L, Teesson M, O’Neill K. The impact of comorbid anxiety and depression on alcohol treatment outcomes. Addiction. 2005;100:787–796. doi: 10.1111/j.1360-0443.2005.001069.x. [DOI] [PubMed] [Google Scholar]
- Canino G, Bravo M, Ramirez R, Febo VE, Rubio-Stipec M, Fernandez RL, Hasin D. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. Journal of Studies on Alcohol. 1999;60:790–799. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Grant BF, Blaine J, Mavreas V, Pull C, Hasin D, Compton WM, Rubio-Stipec M, Mager D. Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug and Alcohol Dependence. 1997;47:195–205. doi: 10.1016/s0376-8716(97)00090-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, Smith SM, Dawson DA, Pulay AJ, Pickering RP, Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B, Dawson D, Hasin D. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–IV (AUDADIS–IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Ruan J, Goldstein RB, Smith SM, Saha TD, Huang B. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2005;35:1747–1759. doi: 10.1017/S0033291705006069. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders; Results from the national Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hasin D, Samet S, Nunes E, Meydan J, Matseoane K, Waxman R. Diagnosis of comorbid psychiatric disorders in substance users assessed with the Psychiatric Research Interview for Substance and Mental Disorders for DSM-IV. American Journal of Psychiatry. 2006;163:689–696. doi: 10.1176/ajp.2006.163.4.689. [DOI] [PubMed] [Google Scholar]
- Henning ER, Turk CL, Mennin DS, Fresco DM, Heimberg RG. Impairment and quality of life in individuals with generalized anxiety disorder. Depression and Anxiety. 2007;24:342–349. doi: 10.1002/da.20249. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, DuPont RL, Burglund P, Wittchen HU. Impairment in pure and comorbid generalized anxiety disorder and major depression at 12 months in two national surveys. American Journal of Psychiatry. 1999;156:1915–1923. doi: 10.1176/ajp.156.12.1915. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Lenox-Smith AJ, Reynolds A. A double-blind, randomised, placebo controlled study of venlafaxine XL in patients with generalised anxiety disorder in primary care. The British Journal of General Practice. 2003;53:772–777. [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JP, Book SW. Comorbidity of generalized anxiety disorder and alcohol use disorders among individuals seeking outpatient substance abuse treatment. Addictive Behaviors. 2010;35:42–45. doi: 10.1016/j.addbeh.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stinson FS, Dawson DA, Goldstein RB, Chou P, Huang B, Smith SM, Ruan J, Pulay AJ, Saha TD, Pickering RP, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV Narcissistic Personality Disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:1033–1045. doi: 10.4088/jcp.v69n0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J, Jr, Kosinski M, Keller SD. A 12-item Short Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Ware JEKM, Turner-Bowker DM, Gandek B. How to score Version 2 of the SF-12 Health Survey. Lincoln, RI: Quality Metrics; 2002. [Google Scholar]
- Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depression and Anxiety. 2002;16:162–171. doi: 10.1002/da.10065. [DOI] [PubMed] [Google Scholar]