Abstract
Safety concerns have been raised about nocturnal and weekend patient care, but it is unknown if these issues effect liver transplantation. We sought to identify the impact of nighttime and weekend liver transplants on graft and patient survival. We utilized the United Network of Organ Sharing database to review adult liver transplants from 1987 to 2010. Comparisons were made between nighttime and daytime operations, and weekday and weekend operations. Cox proportional hazard ratios were determined at 30, 90 and 365 days post-transplant after controlling for relevant factors. 94,768 transplants were included in the analysis. Patient survival at 30, 90 and 365 days for nighttime operations was 96%, 93% and 86%. Patient survival at 30, 90 and 365 days for weekend operations was 95%, 92% and 86%. This was no different from daytime or weekday operations, respectively. Graft failure was unchanged at 30 and 90 days for weekend transplants, but was modestly increased at 365 days (HR: 1.05 (1.01-1.11). Graft survival was unaffected by nighttime transplant. Nighttime and weekend operations for liver transplantation do not impact patient or graft survival, testifying to patient safety measures in place.
Keywords: Liver transplantation, outcomes, time of day, survival, quality
Introduction
In 1999, the Institute of Medicine issued a report highlighting the substantial burden of medical errors, which were estimated to result in up to 98,000 deaths annually with an overall cost of $29 billion.(1) These figures sparked considerable interest in systems-based initiatives to reduce medical errors and promote patient safety in various aspects of healthcare. Among the possible contributors to medical errors, one that has garnered particular attention is the provision of medical care outside of regular daytime and weekday hours, which may be associated with an increased risk of medical errors because of provider fatigue and lack of full available resources.
The associations among nighttime care, weekend care, and patient outcomes have been examined in multiple healthcare settings, with conflicting results. (2-9) Notably, organ transplantation has been the subject of multiple investigations, as these procedures are commonly performed after-hours because of the timing of organ availability. The deleterious effect of nighttime kidney transplantation on patient outcomes has been seen inconsistently,(10, 11) whereas the single study examining this relationship in the context of thoracic organ transplant showed no difference.(12) The only study to evaluate the effect of time-of-day on liver transplant outcomes showed no difference among various postoperative complications, but did demonstrate an increased risk of early death in the group who received nighttime transplants.(13) Although helpful, many of these are single center reviews and are limited by relatively small sample sizes and short study duration.
We therefore undertook this study utilizing the United Network for Organ Sharing (UNOS) standard transplant analysis and research files, which contain information on all liver transplants performed in the US since 1987, in order to determine whether operative time-of-day and weekend operations are associated with adverse patient outcomes such as reduced patient and graft survival.
Methods
We utilized the UNOS standard transplant analysis and research dataset files for liver transplants as of March 4, 2011, which contain extensive patient-level data on all deceased and living donor transplants in the US reported to the Organ Procurement and Transplantation Network between October 1, 1987, and December 31, 2010. Nighttime operations were defined as those started after 7pm or before 7am. Operative start times were determined by adding the cold ischemia time to the cross clamp time at procurement. Weekend operations were defined as those started between 5pm Friday and 8am Monday. The MELD era was defined as the time period after February 27, 2002, the date when the model for end-stage liver disease (MELD) scoring system was implemented as the method of allocation for liver transplants. All statistical analyses were performed with Stata version 11 (Statacorp, College Station, TX). Approval for the study was granted by the University of North Carolina Institutional Review Board.
Bivariate analyses were used to compare daytime and nighttime operations as well as weekday and weekend operations. Chi-square tests were used for categorical variables, Student’s T test was used for normally distributed continuous variables, and Kruskal-Wallis test was used for non-normal continuous variables where appropriate. Kaplan-Meier analysis was used to generate survival tables.
Multivariate analysis with Cox proportional hazards modeling was used to calculate hazard ratios (HR) adjusted for potential confounding and relevant recipient, donor and operative factors. The main outcomes were all cause mortality at 30, 90, and 365 days post-transplant, and graft failure at the same time points. Results of the bivariate analyses were used to select candidate variables for the models. These included recipient race, sex, age, diabetes, body mass index (BMI), vasopressor support, dialysis at transplant, prior upper abdominal surgery, and portal vein thrombosis, pre MELD vs. MELD era, warm and cold ischemia time, donor age, split liver donation, donation after cardiac death, donor cause of death, donor gender, donor location (local, regional, national, or foreign), and re-transplantation. Prior to modeling, potential interactions were assessed and no significant effect modifiers were identified. Variables with greater than 33% missing data were also excluded from multivariate analyses. The models were reduced using a backwards elimination strategy, a priori retaining variables that were significant at a p<0.10 level or those thought to be clinically important. Post-hoc sensitivity analyses were performed using different definitions of day, night and weekend and for the MELD era so that MELD score could be included as a measure of pre-transplant disease severity.
Results
Study Population Characteristics
After excluding patients transplanted under the age of 18, data from 94,768 liver transplants performed at 150 unique centers from 1987 to 2010 were analyzed (Table 1). 51,717 (55%) of these transplants occurred during the MELD era. The mean age at transplant was 51 +/−11 years, 64% of the population was male and 76% was Caucasian. Viral hepatitis (including hepatitis B and C) was the indication for 34% of the transplants followed by alcoholic cirrhosis (13%) and cryptogenic cirrhosis/non-alcoholic steatohepatitis (11%). Fulminant hepatic failure comprised 6% of the population while “other”, a category including diagnoses such as autoimmune hepatitis, primary biliary cirrhosis and primary sclerosing cholangitis accounted for 36% of the population. The mean MELD score at transplant was 21 +/− 9 for those patients transplanted in the MELD era. 21% of the population had diabetes, and the median body mass index (BMI) was 27 kg/m2 (24-31 interquartile range). The majority of the donor population (60%) was male; the mean donor age was 38 +/− 17 years. Median cold ischemia time was 7.6 hours (5.6-10 interquartile range). Overall post transplant survival was 96% at 30 days, 92% at 90 days and 86% at one year.
Table 1.
Characteristics of the Adult UNOS Liver Transplant Data Base 1987 to 2010
| Recipient characteristics | |
| Transplants, total | 94768 |
| MELD era | 51717 (55) |
| Mean Age at Transplant | 51 +/− 10.9 |
| n (%) male | 60176 (64) |
| n (%) Caucasian | 71739 (76) |
| Mean MELD at Transplant* | 21 +/− 9.4 |
| Indications for transplant, n (%) | |
| ALF | 5945 (6) |
| Viral hepatitis | 31763 (34) |
| Cryptogenic/NASH | 10342 (11) |
| Alcohol | 12494 (13) |
| Other | 34224 (36) |
| Re-transplant | 9491 (10) |
| ABO blood group | |
| A | 36978 (39) |
| AB | 4613 (5) |
| B | 12200 (13) |
| O | 40964 (43) |
| Diabetes, n (%) | 15975 (21) |
| Dialysis | 6716 (8) |
| Median Body Mass Index | 26.9 (23.6 – 31.0 IQR) |
| Donor characteristics | |
| Male Donors, n (%) | 57124 (60) |
| Donor Age, mean +/− SD | 38 +/−17 |
| Donor type, n (%) | |
| Deceased Donor | 75493 (97) |
| DCD | 2242 (3) |
| Split Liver | 3932 (4) |
| Donor Cause of Death, n (%) | |
| Anoxia | 10455 (11) |
| CVA | 37517 (41) |
| Trauma | 36983 (40) |
| CNS tumor | 661 (1) |
| Other | 6078 (7) |
| Donor Location | |
| Local | 64508 (68) |
| Regional | 21518 (23) |
| National | 8599 (9) |
| Foreign | 143 (0) |
| Operative characteristics | |
| Nighttime procurement | 56665 (60) |
| Nighttime transplant | 31143 (38) |
| Weekend operation | 32079 (35) |
| Median Warm Ischemia Time, min | 45 (35-60 IQR) |
| Median Cold Ischemia Time, hours | 7.6 (5.6-10 IQR) |
| Prior abdominal surgery | 31928 (42) |
| Portal Vein Thrombosis | 3267 (5) |
| Multiple Vasopressors | 1893 (2) |
| Survival | |
| Overall Graft Survival (%) | |
| 30 day | 92 |
| 90 day | 88 |
| One year | 81 |
| Overall Patient Survival (%) | |
| 30 day | 96 |
| 90 day | 92 |
| One year | 86 |
MELD for patient in post MELD era only
Nighttime Operation and Effect on Survival
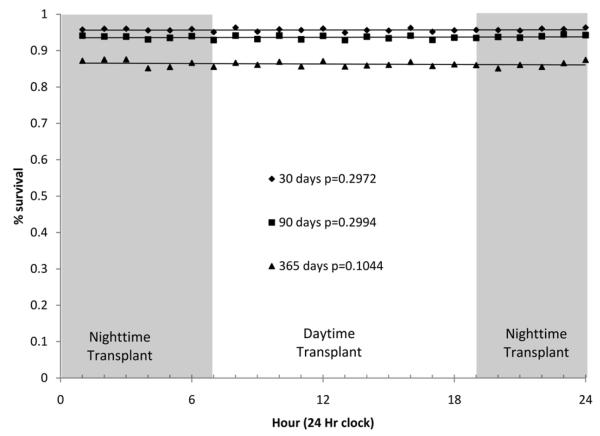
Bivariate analysis of the nocturnal and daytime populations is shown in Table 2. A higher proportion of operations were performed at night during the MELD era (60% vs. 50% p<0.001). For patients transplanted in the MELD era, there was no difference in MELD score at the time of transplant (21.2 vs. 21.3, p=0.58). Although statistically significant, the mean age of patients transplanted at night was not clinically different from that of the daytime group (51.1 vs. 50.7, p<0.001). This clinically insignificant but statistically significant difference also held for diabetes (21% vs. 20%, p=0.003), BMI (27.1 vs. 26.9, p=0.0001), and warm ischemia time (45 vs. 46 minutes, p<0.001). Cold ischemia time was shorter for nighttime operations compared to daytime operations (7 (5.2-9.4 IQR) vs. 8 (6-10.5 IQR) hours, p<0.001). Daytime transplants were more likely to have nighttime organ procurements (70% vs. 40%, p<0.001). There was a statistically significant difference in the number of nighttime compared to daytime liver transplants during the weekend (30% vs. 42%, p<0.001) due to the definition of “weekend”. Patient and graft survival were not different for daytime vs. nighttime transplants at 30 days (96% for patient and 92% vs. 93% for graft), 90 days (92% vs. 93% for patient and 88% vs. 89% for graft), and 365 days (86% for patient and 81% for graft). Timing of transplants was also compared on an hourly basis, and no differences in patient survival were seen at 30, 90 and 365 days (Figure 1).
Table 2.
Bivariate Analysis of Day Time and Night Time Procedures
| Day Time | Night Time | p | |
| Transplants, total | 51543 (62) | 31143 (38) | |
| Recipient characteristics | |||
| MELD era | 25717 (50) | 18549 (60) | <0.001 |
| Mean Age at Transplant | 50.7 +/− 11 | 51.1 +/− 11 | <0.001 |
| n (%) male | 32773 (64) | 19864 (64) | 0.56 |
| n (%) Caucasian | 38987 (76) | 23706 (76) | 0.023 |
| Mean MELD at Transplant* | 21.2 +/− 10 | 21.3 +/− 9 | 0.58 |
| Indications for transplant, n (%) | |||
| ALF | 3057 (6) | 2072 (7) | |
| Viral hepatitis | 17399 (34) | 10250 (33) | |
| Cryptogenic/NASH | 5616 (11) | 3484 (11) | <0.001 |
| Alcohol | 7041 (13) | 4048 (13) | |
| Other | 18430 (36) | 11289 (36) | |
| Re-transplant | 5181 (10) | 3244 (10) | 0.09 |
| Diabetes, n (%) | 8298 (20) | 5534 (21) | 0.003 |
| Dialysis | 3546 (8) | 2355 (9) | 0.07 |
| Median Body Mass Index | 26.9 | 27.1 | 0.0001 |
| Donor characteristics | |||
| Male Donors, n (%) | 31118 (60) | 18119 (61) | 0.32 |
| Donor Age | 38.3 +/− 17 | 38.1 +/− 17 | 0.048 |
| Donor type, n (%) | |||
| Deceased Donor | 41581 (98) | 25869 (96) | <0.001 |
| DCD | 971 (2) | 1033 (4) | |
| Split Liver | 514 (1) | 366 (1) | 0.42 |
| Donor Cause of Death, n (%) | |||
| Anoxia | 5564 (11) | 3888 (12) | |
| CVA | 21410 (41) | 12380 (40) | |
| Trauma | 20468 (40) | 12684 (41) | <0.001 |
| CNS tumor | 340 (1) | 237 (1) | |
| Other | 3746 (7) | 1948 (6) | |
| Donor Location | |||
| Local | 34,605 (67) | 20,555 (66) | |
| Regional | 12,314 (24) | 7,141 (23) | <0.001 |
| National | 4,548 (9) | 3,413 (11) | |
| Foreign | 76 (0) | 34 (0) | |
| Operative characteristics | |||
| Nighttime procurement | 35859 (70) | 12364 (40) | <0.001 |
| Weekend operation | 15279 (30) | 13084 (42) | <0.001 |
| Median Warm Ischemia Time, min | 46 (36-60 IQR) | 45 (35-60 IQR) | <0.001 |
| Median Cold Ischemia Time, hr | 8 (6-10.5 IQR) | 7 (5.2-9.4 IQR) | <0.001 |
| Prior abdominal surgery | 16868 (41) | 11088 (43) | <0.001 |
| Portal Vein Thrombosis | 1628 (5) | 1197 (6) | 0.08 |
| Multiple Vasopressors | 977(2) | 676 (2) | 0.006 |
| Survival | |||
| Overall Graft Survival (%) | |||
| 30 day | 92 | 93 | |
| 90 day | 88 | 89 | 0.39 |
| One year | 81 | 81 | |
| Overall Patient Survival (%) | |||
| 30 day | 96 | 96 | |
| 90 day | 92 | 93 | 0.89 |
| One year | 86 | 86 | |
IQR = inter quartile range
MELD at transplant for those performed after 2-27-2002.
Figure 1.
Short term survival by time of liver transplant. Data points represent the percent survival for transplants begun during each hour of the day.
Unadjusted Cox Proportional Hazard modeling showed that as compared to daytime liver transplant patients, nighttime liver transplants had a 0.96 (0.89-1.03 95% CI) hazard of death at 30 days, 0.97 (0.92-1.02 95% CI) hazard of death at 90 days and a 0.99 (0.95-1.03 95% CI) hazard of death at 365 days. A fully adjusted model was created, controlling for age, race, sex, diabetes, BMI, vasopressor support, dialysis, prior upper abdominal surgery, portal vein thrombosis, re-transplantation, donor location, pre MELD vs. MELD era, diagnosis, donor age, cold and warm ischemia time, nighttime organ procurement, donor cause of death and weekday vs. weekend operation. This model was then reduced by backwards elimination. Other models were created altering the daytime and nighttime definitions (e.g. 3am-3pm per Lonze et al(13)) and substituting variables that were not included by the original a priori methodology . Additionally a separate analysis was done for the MELD era so that MELD score could be included as a measure of disease severity. The results for each of these models were unchanged from the unadjusted model (data not shown). The final model, which controlled for weekend operations, night time procurement, cold ischemia time, donor age, split livers, donation after cardiac death, diagnosis, recipient age, gender, dialysis, vasopressor use, prior upper abdominal surgery, portal vein thrombosis, re-transplantation, donor location, and pre MELD versus MELD era, also showed no difference in graft or patient survival at 30, 90 and 365 days (Table 4).
Table 4.
Unadjusted and Adjusted Hazard Ratios for Graft Failure and Death
| Hazard Ratio (95% CI) | ||||
|---|---|---|---|---|
| Graft Failure | Death | |||
| Unadjusted | Adjusted* | Unadjusted | Adjusted* | |
| Night time transplant | ||||
| 30 Days | 0.93 (0.88 0.98) | 1.00 (0.92 1.08) | 0.96 (0.89 1.03) | 0.94 (0.85 1.05) |
| 90 Days | 0.94 (0.90 0.98) | 1.00 (0.94 1.06) | 0.97 (0.92 1.02) | 0.98 (0.90 1.06) |
| 1 year | 0.96 (0.94 1.00) | 1.01 (0.96 1.06) | 0.99 (0.95 1.03) | 0.99 (0.94 1.05) |
| Weekend transplant | ||||
| 30 Days | 1.03 (0.98 1.08) | 1.04 (0.96 1.13) | 0.99 (0.93 1.07) | 0.93 (0.84 1.04) |
| 90 Days | 1.03 (0.98 1.07) | 1.04 (0.97 1.10) | 1.01 (0.96 1.06) | 0.98 (0.91 1.06) |
| 1 year | 1.02 (0.99 1.06) | 1.05 (1.01 1.11) | 1.02 (0.98 1.06) | 1.02 (0.97 1.08) |
The model was adjusted for night time procurement, cold ischemia time, donor age, split liver grafts, donation after cardiac death, recipient gender, recipient age, indication for transplant, donor location, dialysis, vasopressor use, portal vein thrombosis, prior abdominal surgery, re-transplantation and pre MELD vs. MELD era
Weekend Operation and Effect on Survival
Bivariate analyses of the weekday and weekend populations are shown in Table 3. Although there were statistically significant differences, none of the differences were clinically meaningful. A higher proportion of weekend operations were performed in the MELD era (55% vs. 54% p=0.012). For patients transplanted in the MELD era, MELD scores at the time of transplant were higher during the weekend (21.6 vs. 21.2, p=0.0002). There were no differences in the median BMI or proportions of patients with diabetes when weekend vs. weekday transplants were compared. On weekends, organ procurement was less likely to occur at night (53% vs. 61%, p<0.001) but transplants were more likely to occur at night (46% vs. 33%, p <0.001) due to the definition of “weekend”. Warm ischemia time was not different on weekends vs. weekdays. Cold ischemia time was shorter on weekends (7.5 hours vs. 8.0 hours, p<0.001). Patient and graft survival were not different at 30, 60 or 365 days for weekend versus weekday transplants.
Table 3.
Bivariate Analysis of Weekday and Weekend* Procedures
| Weekday | Weekend | p | |
| Transplants, total | 59580 (65) | 32079 (35) | |
| Recipient characteristics | |||
| MELD era | 32019 (54) | 17517 (55) | 0.012 |
| Mean Age at Transplant | 50.9 +/− 11 | 50.8 +/− 11 | 0.80 |
| n (%) male | 37969 (64) | 20431 (64) | 0.91 |
| n (%) Caucasian | 44921 (75) | 24315 (76) | 0.039 |
| Mean MELD at Transplant** | 21.2 +/−9 | 21.6 +/− 10 | 0.0002 |
| Indications for transplant, n (%) | |||
| ALF | 3698 (6) | 2141 (7) | |
| Viral hepatitis | 20051 (34) | 10678 (33) | |
| Cryptogenic/NASH | 6520 (11) | 3516 (11) | 0.075 |
| Alcohol | 7922 (13) | 4302 (13) | |
| Other | 21389 (36) | 11442(36) | |
| Re-transplant | 6079 (10) | 3339 (10) | 0.33 |
| Diabetes, n (%) | 9966 (21) | 5487 (21) | 0.32 |
| Dialysis | 4233 (9) | 2439 (9) | 0.011 |
| Median Body Mass Index | 27 (24-31 IQR) | 27 (24-31 IQR) | 0.99 |
| Donor characteristics | |||
| Male Donors, n (%) | 40274 (61) | 15212 (60) | 0.71 |
| Donor Age | 38.3 +/− 17 | 37.9 +/− 17 | 0.0006 |
| Donor type, n (%) | |||
| Deceased Donor | 48883 (97) | 26608 (97) | 0.08 |
| DCD | 1192 (3) | 750 (3) | |
| Split Liver | 762 (1) | 336 (1) | 0.002 |
| Donor Cause of Death, n (%) | |||
| Anoxia | 6944 (12) | 3509 (11) | |
| CVA | 24514 (41) | 12981 (40) | |
| Trauma | 23683 (40) | 13270 (41) | <0.001 |
| CNS tumor | 406 (1) | 254(1) | |
| Other | 4018 (6) | 2059 (6) | |
| Donor Location | |||
| Local | 40110 (67) | 21353(67) | |
| Regional | 13947 (23) | 7546 (23) | 0.011 |
| National | 5451 (9) | 3136 (10) | |
| Foreign | 72 (0) | 44 (0) | |
| Operative characteristics | |||
| Nighttime procurement | 36346 (61) | 17210 (53) | <0.001 |
| Nighttime transplant | 18059 (33) | 13084 (46) | <0.001 |
| Median Warm Ischemia Time, min | 45 (36-60 IQR) | 46 (35-60 IQR) | 0.09 |
| Median Cold Ischemia Time, hr | 8.0 (6-10 IQR) | 7.5 (5.6-10 IQR) | <0.001 |
| Prior abdominal surgery | 19926 (42) | 10871 (42) | 0.24 |
| Portal Vein Thrombosis | 2089 (6) | 1084 (5) | 0.17 |
| Multiple Vasopressors | 1195 (2) | 696 (2) | 0.10 |
| Survival | |||
| Overall Graft Survival (%) | |||
| 30 day | 92 | 92 | |
| 90 day | 88 | 88 | 0.21 |
| One year | 81 | 80 | |
| Overall Patient Survival (%) | |||
| 30 day | 95 | 95 | |
| 90 day | 92 | 92 | 0.26 |
| One year | 86 | 86 | |
IQR = inter quartile range
Weekend defined as 5pm Friday until 8am Monday
MELD at transplant for those performed after 2-27-2002.
Unadjusted Cox Proportional Hazard modeling showed that as compared to weekday liver transplant patients, weekend liver transplants had a 0.99 (0.93-1.07 95% CI) hazard of death at 30 days, 1.01 (0.96-1.06 95% CI) at 90 days and 1.02 (0.98-1.06 95% CI) at 365 days. A fully adjusted model was created, controlling for age, race, sex, diabetes, BMI, vasopressor support, dialysis, prior upper abdominal surgery, portal vein thrombosis, re-transplantation, donor location, pre vs. MELD era, diagnosis, donor age, cold and warm ischemia time, nighttime organ procurement, donor cause of death and daytime vs. nighttime operation. Other models were created in a similar fashion as above. The results for each of these models were unchanged from the unadjusted model (data not shown). The final model showed no difference in patient survival at 30, 90 and 365 days. The final model, which controlled for nighttime operations, nighttime procurement, cold ischemia time, donor age, split livers, donation after cardiac death, diagnosis, recipient age, gender, dialysis, vasopressor use, prior upper abdominal surgery, portal vein thrombosis, re-transplantation, donor location, and pre MELD versus MELD era, showed a small increase in the hazard of graft failure at 365 days only [1.05 (1.01-1.11 95 % CI)] (Table 4). Timing of transplants was also compared on a daily basis, and no differences in patient or graft survival were seen at 30, 90 and 365 days.
Discussion
This retrospective review of nearly 100,000 liver transplants performed over more than two decades shows no difference in graft or patient survival when operations are performed during the daytime versus nighttime hours. For weekend transplants, there were no differences in patient survival at any time point or in graft survival after 30 and 90 days, although we did detect a slight decline in graft survival after 1 year. This study shows similar findings to the recent UNOS registry study by George et al,(12) for thoracic transplants but has contradictory findings compared with smaller studies performed by Lonze et al,(13) for liver transplant and Fechner et al, for kidney transplant.(10)
Our study provides reassurance to the transplant community and those patients awaiting transplant regarding their outcomes. It highlights that patient safety mechanisms of having appropriate numbers of surgeons and ancillary staff available after hours and on weekends. These call schedules already in place allow patients undergoing after-hours and weekend liver transplants to benefit from the same survival outcomes as those having procedures performed during the standard workday. As the timing of transplant can rarely be predicted or scheduled, the lack of a decline in safety at night and on weekends is reassuring.
When analyzing a dataset of this size, care must be taken to not misinterpret statistically significant results that are not clinically important. Many variables are trivially different (e.g. age at transplant for night vs. daytime operations; 51.1 vs. 50.7, p<0.001), yet due to the large sample size and tremendous power, they are highly statistically significant.
There was a statistically significant decline (5%) in graft survival at 365 days post-transplant when the surgery occurred on the weekend. One plausible explanation may be the surgical team’s call schedule. Both patient and graft survival decline when the primary surgeon has performed a high volume of transplants within a short period of time (14). In centers where the primary surgical team takes call for a week at a time or for the whole weekend, there may be a resultant decrease in graft survival later in the weekend when they have performed many operations in the preceding days. Presumably, such a decrease would be due to impaired technical performance or perioperative decision making, both of which could affect 1 year outcomes. Another explanation for a decline in graft survival at one year could involve the surgical services support staff. During the weekend these individuals may be a cross-disciplinary team who are involved in a heterogeneous set of operative cases including trauma, orthopedics, or surgical emergencies. During the weekday the surgical team is likely to be comprised of dedicated transplant personnel. Procurements may be left to local surgical teams at a non-liver transplant center more often on weekends as opposed to transplant teams traveling to the donor on weekdays and weeknights. Perioperative support (e.g. dedicated transplant pharmacists) including the physical presence of multiple medical experts may be less available on weekends. Therefore, there are plausible reasons for weekend transplants to have worse graft survival.
However, one might expect such effects to manifest earlier at 30 and 90 days as well as at one year. Also, our study examined multiple outcomes at various time points (a total of 12 adjusted HRs were measured). In this circumstance, it is not unusual to find a statistically significant result by chance (i.e. type I error) or epiphenomenon.
Data are collected within the UNOS database on the reasons for graft failure. No differences in the etiologies of graft failure were seen in bivariate analyses of biliary complications, acute or chronic rejection, de novo hepatitis, primary disease recurrence, or infection when weekday transplants were compared to weekend transplants. However, these data must be interpreted with caution, and the analyses are not presented due to the large number of missing data.
Other studies have raised concern over nighttime and weekend procedures as well as nighttime and weekend admissions for a variety of medical problems. Studies of gastrointestinal bleeding (5, 15, 16), intensive care unit admission (17), stroke admission (3), and renal failure(4), have all found deleterious impact of either night or weekend admission. Most of these studies are from single centers and relative to this study, are markedly smaller.
Database registry research has its limitations. Lacking within the UNOS database is the granular patient information that many single center studies are able to access. Inclusion of such factors may alter the results, and thus residual confounding is a concern. Additionally, coding or data entry errors cannot be resolved at the level of individual patients. If these errors occur in a non-random fashion, the results may be biased, but there is no strong reason to suspect this.
Our definition of start time may be subject to scrutiny. UNOS does not record the actual time that the recipient surgery is started, so we chose to add the cold ischemia time to the donor cross-clamp time as an approximation of start time. In practice, this would reflect the time that the graft is placed into the recipient and would therefore exclude the hepatectomy, which may be the most difficult part of the operation and can take several hours. The assignment of daytime versus nighttime operations is arbitrary as well. The decision to use 7am to 7pm to define daytime was based on the study by George et al,(12) in an attempt to provide some consistency across our investigations. In an attempt to overcome this arbitrary day/night definition, other divisions were analyzed to facilitate comparisons with other relevant studies such as Lonze et al.(13) The bivariate hour-by-hour analysis also showed no differences (Figure 1), mitigating any variability that could be attributed to either the start time definition or the day/night definition. The fact that there were no differences in the outcomes no matter how the data were analyzed gives some strength to our ultimate conclusions.
In sum, in a large multicenter registry database containing nearly 100,000 liver transplants and spanning over twenty years, neither nighttime liver transplantation nor weekend liver transplantation has an adverse impact on patient or graft survival. The lack of differences found in patient and graft outcomes are a testament to current practices covering off hour and weekend transplants. Such data should provide some reassurance to patients and transplant centers that post-transplant outcomes are not significantly affected by the timing of surgery. With an increasing public focus on patient safety, collecting more precise data on time of transplant and available personnel may be warranted to provide better vigilance of off-hour transplants in the future.
Acknowledgement
This work was supported in part by Health Resources and Services Administration contract 231-00-0115. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Grant Support: This work was supported, in part, by the National Institutes of Health, 1KL2-RR025746-03 (Barritt) and T32 DK07634 (Orman).
Abbreviations
- MELD
model for end stage liver disease
- DCD
donation after cardiac death
- UNOS
United Network for Organ Sharing
- BMI
body mass index
- CI
confidence interval
- CVA
cerebral vascular accident
- NASH
non alcoholic fatty liver disease
Footnotes
Author Contributions: Eric S. Orman, MD: Study concept and design; acquisition of data; drafting of the manuscript; critical revision of the manuscript
Paul H. Hayashi, MD, MPH: interpretation and analysis of data; critical revision of the manuscript
Evan S. Dellon, MD, MPH: Study concept and design; statistical analysis; interpretation and analysis of data; critical revision of the manuscript
David A Gerber, MD: interpretation and analysis of data; critical revision of the manuscript
A. Sidney Barritt IV, MD, MSCR: Study concept and design; statistical analysis; interpretation and analysis of data; drafting of the manuscript; critical revision of the manuscript
Disclosures: The Authors have no relevant conflicts of interest to disclose Key Words: Liver transplantation, outcomes, time of day
References
- 1.Kohn LT, Corrigan JM, Donaldson MS. To err is human: Building a safer health stsyem. National Academy Press; Washington, D.C.: 1999. [PubMed] [Google Scholar]
- 2.Cavallazzi R, Marik PE, Hirani A, Pachinburavan M, Vasu TS, Leiby BE. Association between time of admission to the ICU and mortality: a systematic review and metaanalysis. Chest. 2010;138(1):68–75. doi: 10.1378/chest.09-3018. [DOI] [PubMed] [Google Scholar]
- 3.Crowley RW, Yeoh HK, Stukenborg GJ, Medel R, Kassell NF, Dumont AS. Influence of weekend hospital admission on short-term mortality after intracerebral hemorrhage. Stroke. 2009;40(7):2387–2392. doi: 10.1161/STROKEAHA.108.546572. [DOI] [PubMed] [Google Scholar]
- 4.James MT, Wald R, Bell CM, Tonelli M, Hemmelgarn BR, Waikar SS, et al. Weekend hospital admission, acute kidney injury, and mortality. J Am Soc Nephrol. 2010;21(5):845–851. doi: 10.1681/ASN.2009070682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dorn SD, Shah ND, Berg BP, Naessens JM. Effect of weekend hospital admission on gastrointestinal hemorrhage outcomes. Dig Dis Sci. 2010;55(6):1658–1666. doi: 10.1007/s10620-009-0914-1. [DOI] [PubMed] [Google Scholar]
- 6.Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356(11):1099–1109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 7.Arabi Y, Alshimemeri A, Taher S. Weekend and weeknight admissions have the same outcome of weekday admissions to an intensive care unit with onsite intensivist coverage. Crit Care Med. 2006;34(3):605–611. doi: 10.1097/01.ccm.0000203947.60552.dd. [DOI] [PubMed] [Google Scholar]
- 8.Komen N, Dijk JW, Lalmahomed Z, Klop K, Hop W, Kleinrensink GJ, et al. After-hours colorectal surgery: a risk factor for anastomotic leakage. Int J Colorectal Dis. 2009;24(7):789–795. doi: 10.1007/s00384-009-0692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelz RR, Freeman KM, Hosokawa PW, Asch DA, Spitz FR, Moskowitz M, et al. Time of day is associated with postoperative morbidity: an analysis of the national surgical quality improvement program data. Ann Surg. 2008;247(3):544–552. doi: 10.1097/SLA.0b013e31815d7434. [DOI] [PubMed] [Google Scholar]
- 10.Fechner G, Pezold C, Hauser S, Gerhardt T, Muller SC. Kidney’s nightshift, kidney’s nightmare? Comparison of daylight and nighttime kidney transplantation: impact on complications and graft survival. Transplant Proc. 2008;40(5):1341–1344. doi: 10.1016/j.transproceed.2008.02.072. [DOI] [PubMed] [Google Scholar]
- 11.Seow YY, Alkari B, Dyer P, Riad H. Cold ischemia time, surgeon, time of day, and surgical complications. Transplantation. 2004;77(9):1386–1389. doi: 10.1097/01.tp.0000122230.46091.e2. [DOI] [PubMed] [Google Scholar]
- 12.George TJ, Arnaoutakis GJ, Merlo CA, Kemp CD, Baumgartner WA, Conte JV, et al. Association of operative time of day with outcomes after thoracic organ transplant. JAMA. 2011;305(21):2193–2199. doi: 10.1001/jama.2011.726. [DOI] [PubMed] [Google Scholar]
- 13.Lonze BE, Parsikia A, Feyssa EL, Khanmoradi K, Araya VR, Zaki RF, et al. Operative start times and complications after liver transplantation. Am J Transplant. 2010;10(8):1842–1849. doi: 10.1111/j.1600-6143.2010.03177.x. [DOI] [PubMed] [Google Scholar]
- 14.Halldorson JB, Bakthavatsalam R, Reyes JD, Perkins JD. The impact of consecutive operations on survival after liver transplantation. Liver Transpl. 2009;15(8):907–914. doi: 10.1002/lt.21734. [DOI] [PubMed] [Google Scholar]
- 15.Ananthakrishnan AN, McGinley EL, Saeian K. Outcomes of weekend admissions for upper gastrointestinal hemorrhage: a nationwide analysis. Clin Gastroenterol Hepatol. 2009;7(3):296–302e291. doi: 10.1016/j.cgh.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 16.Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2009;7(3):303–310. doi: 10.1016/j.cgh.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 17.Barnett MJ, Kaboli PJ, Sirio CA, Rosenthal GE. Day of the week of intensive care admission and patient outcomes: a multisite regional evaluation. Med Care. 2002;40(6):530–539. doi: 10.1097/00005650-200206000-00010. [DOI] [PubMed] [Google Scholar]