Abstract
Studies suggest that perievent panic attacks are predictive of future posttraumatic stress disorder (PTSD). Using a population of New York City residents interviewed after the World Trade Center Disaster, the authors measured event exposure, perievent panic, potential confounding, mediating variables, and PTSD. When they estimated a structural equation model, with other stressor events, psychological resources, and Year 1 and Year 2 PTSD as latent variables and adjusted for confounders, the association between perievent panic and Year 2 PTSD was not significant. Results revealed that perievent panic was predictive of Year 1 PTSD, but not Year 2 PTSD. Year 2 stressors and Year 2 psychosocial resources were the best predictors of Year 2 PTSD.
Research suggests that having a history of panic attacks predicts future mental health disorders, including posttraumatic stress disorder (PTSD) Baillie & Rapee, 2005; Goodwin & Hamilton, 2002a, 2002b; Kessler et al., 2006; Lawyer et al., 2006; Nixon, Resick & Griffin, 2004). Community studies suggest a lifetime prevalence of 7–23% for panic attacks, with about 80% of individuals reporting significant stressors in the previous 12 months (Kessler et al., 2006). Understanding the association between trauma exposure, panic attacks, and the onset of psychological disorders, such as PTSD, could be informative for treatment interventions.
Recently, researchers have suggested that perievent panic attacks, that is, panic attacks in temporal proximity to traumatic exposures, have prognostic value for future mental health problems (Goodwin & Hamilton, 2002a, 2002b; Lawyer et al., 2006). Panic attacks, therefore, have become a focus of research related to predicting mental health status (Goodwin, Brook, & Cohen, 2005; Goodwin & Hamilton, 2002a). This research, however, has been inconsistent. Goodwin et al. (2005), for instance, have reported that panic attacks in children predicted increased risk of having a personality disorder 10 years later. A series of studies focusing on the mental health consequences of the World Trade Center Disaster has suggested that experiencing a perievent panic attack was related to PTSD, depression, poorer physical health, and greater use of mental health services (Adams & Boscarino, 2005; Adams, Boscarino, & Galea, 2006; Boscarino, Adams, & Figley, 2004). Other research related to the World Trade Center Disaster has shown little or no association between perievent panic and psychological well-being, once other risk factors were controlled (Boscarino & Adams, 2009).
Limitations of past studies were that investigators have either assessed postevent outcomes on a relatively short-term basis, have not controlled for important pre-exposure and postexposure variables, or have not examined the indirect associations among these variables. Consequently, past findings that linked perievent panic with later psychological problems may have been confounded. To assess this, we examined PTSD among New York City (NYC) adults at 1 and 2 years after the World Trade Center Disaster.
The terrorist attacks in New York City on September 11, 2001, resulted in approximately 2,800 persons killed, thousands injured, and many more residents directly witnessing these events (Boscarino et al., 2004, Centers for Disease Control and Prevention, 2002; Galea et al., 2002). The World Trade Center Disaster had several elements that are well-known to result in long-term mental health problems, including major loss of life, extensive property damage, ongoing financial problems, and a disaster caused by human intent (Norris et al., 2002; North et al., 2004).
Several studies show a relationship between panic attacks soon after the World Trade Center Disaster and later psychological disorders (Boscarino et al., 2004; Galea et al., 2002; Lawyer et al., 2006). More specifically, individuals who report symptoms that meet criteria for a perievent panic attack are more likely to meet criteria for current and future PTSD. A recent study, however, contradicts this reported association and suggests that after controlling for predisaster mental health problems and current psychosocial resources, that the relationship between perievent panic and psychological difficulties becomes nonsignificant (Boscarino & Adams, 2009).
Evidence suggests that perievent panic may be indirectly implicated in poor psychological health in the posttrauma period via its association with social psychological resources (Boscarino & Adams, 2009). That is, perievent panic may function to lower self-esteem or social support, which in turn results in poorer mental health outcomes. Several investigators note that a postdisaster environment can be a period characterized by the loss of social support, legal problems, property loss, as well as decreases in psychological resources (Adams et al., 2006; Hobfoll, 1989; Norris et al., 2002; Picou, Marshall, & Gill, 2004). Thus, it is possible that perievent panic is associated with both lower psychosocial resources and increases in negative life events postdisaster, which in turn affect mental health status. It is known that after stressful event exposures individuals often react physiologically, through changes in the neuroendocrine and stress hormone functions (Boscarino, 2008) and psychologically, often through alterations in cognitive processes (Thoits, 1995), which can impact social relationships and lower self-esteem (Kulka et al., 1990). Perievent panic may also reflect fundamental psychopathologies that are exacerbated by exposure to a traumatic event. Community disaster survivors with perievent panic, thus, may act in ways (e.g., persistent anxiety) that depletes their available social support and/or lowers their self-esteem. Although research by Kaniasty and Norris (2008) is an exception, few studies have assessed the complex associations among interpersonal and psychological variables in the postdisaster period and then relate these to mental health outcomes.
We use structural equation modeling (SEM) to address these past research limitations. There are advantages to this method. First, SEM is fundamentally a hypothesis testing method (i.e., a confirmatory approach), rather than an exploratory approach (e.g., regression analyses). Second, it allows the simultaneous estimation of a series of regression equations to determine if the proposed model accurately reflects the data. Third, SEM can explicitly estimate measurement error, rather than ignore this issue as is done with traditional techniques. Fourth, SEM allows incorporation of both directly measured variables and unobserved (i.e., latent) ones. Fifth, SEM is uniquely suited to assess both direct and indirect associations among variables, including those between perievent panic and PTSD (Byrne 2010; Kline 2005).
Given the hypothesized association between panic attacks and later psychological difficulties, our first research objective was to determine if perievent panic is related to PTSD 1 and 2 years after the World Trade Center Disaster, after controlling for pre- and postdisaster factors. We incorporated both observed (e.g., exposure to the disaster) and latent (e.g., stressor events, psychological resources, PTSD) variables in our model. Our second objective was to assess the impact of perievent panic on stressor events and psychosocial resources 2 years after the World Trade Center Disaster. Specifically, we wanted to determine if experiencing a panic attack after the disaster was associated with increased postdisaster stressful events and/or lower psychological resources, which in turn affected Year 2 PTSD (Boscarino & Adams, 2009). A SEM model relating pre-exposure mental health, disaster exposure, perievent panic, Year 2 stressor events, Year 2 psychosocial resources, and Year 1 and Year 2 PTSD, permits us to assess if perievent panic has both a direct and indirect effect on Year 2 PTSD.
METHOD
Participants
The data for the present study come from a prospective cohort study of adults. Using random digit-dialing, we conducted a baseline telephone survey 1 year after the World Trade Center Disaster (October–December, 2002). A follow-up survey occurred 1 year later, between October 2003, and February 2004. Interviews were conducted in English and Spanish. For the baseline, 2,368 individuals completed the survey. We were able to reinterview 1,681 of these respondents in the follow-up survey. Using standard survey definitions, the baseline cooperation rate was 63% (American Association for Public Opinion Research, 2008), and the reinterview rate was 71% (Adams et al., 2006), consistent with previous investigations (Galea et al., 2002; North et al., 2004).
Sampling weights were developed for each wave to correct for potential selection bias and for the oversampling of treatment-seeking respondents (Groves, Fowler, Couper, & Lepkowski, 2004). Demographic weights also were used to adjust follow-up data for slight differences in response rates by demographic groups (Kessler, Little, & Groves, 1995). With these survey adjustments, our study is representative of adults who were living in NYC on the day of the World Trade Center Disaster (Adams & Boscarino, 2005; Adams et al., 2006). Additional details on these data are available elsewhere (Boscarino & Adams, 2008). The Geisinger Clinic Institutional Review Board (IRB; Danville, PA), currently serves as the IRB of record for this study.
Endogenous Variables
Our Year 1 and Year 2 PTSD variables measure latent variables and are based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, (DSM-IV; American Psychiatric Association [APA], 1994). For the current analyses, we altered the usual PTSD criteria to conform to SEM requirements. Thus, we focus on symptom counts for Criteria B (reexperiencing, five symptoms), C (avoidance, seven symptoms), and D (arousal, five symptoms), rather than on meeting diagnostic criteria. Wording of the symptom questions related them to any traumatic event in the 12 months prior to the Year 1 and the Year 2 surveys, not just the World Trade Center Disaster. Use of symptom counts as manifest indicators for the latent variable, PTSD, is similar to previous studies using SEM to assess models with PTSD as a dependent (endogenous) variable (Kaniasty & Norris 2008). Based on the DSM-IV, 3.8% (weighted) of the sample met full criteria for PTSD at Year 1, whereas 5.4% (weighted) met full criteria at Year 2.
Our study assessed whether respondents met criteria for a perievent panic attack during the World Trade Center Disaster based on the Diagnostic Interview Schedule nomenclature (Robins et al., 1999) and we used this measure as an observed variable in our SEM. For our perievent panic measure, questions were phrased to assess panic symptoms that occurred during or shortly after the World Trade Center Disaster (Galea et al., 2002). The presence of more than four symptoms classified the respondent as having a perievent panic attack, if these reached their peak within10 minutes of onset (Galea et al., 2002). This variable was coded as a binary variable. This measure has been used and validated in previous studies (Adams & Boscarino, 2005; Boscarino & Adams, 2009; Boscarino et al., 2004; Galea et al., 2002) and has demonstrated good reliability and validity.
Our SEM model included an observed variable measuring exposure to the World Trade Center Disaster events that could affect PTSD onset. This construct was assessed during the Year 1 survey and consisted of 12 possible events that the respondent could have experienced during or as a consequence of the terrorist attack (e.g., was at the disaster site during attack, lost family members/friends in the attack, etc.). Due to the positively skewed distribution of this variable, we recoded the number of exposures greater than 7 to 6, creating a variable with a range of 0 to 6. This study measure was validated in previous World Trade Center Disaster studies and is discussed in detail elsewhere (Boscarino et al., 2004; Boscarino & Adams, 2008).
We also developed a latent postdisaster stressor exposure variable using two observed measures. First, the Year 2 negative life events scale (Freedy, Kilpatrick, & Resnick, 1993), was the sum of eight negative experiences that could have occurred in the 12 months prior to the follow-up survey (e.g., divorce, death of spouse, etc.). Due to the positive skewness of this scale, we recoded values 4+ to a value of 3 creating a scale ranging from 0 to 3. Second, the Year 2 traumatic events scale (Freedy et al., 1993), was the sum of 10 traumas that could have occurred in the 12 months prior to the follow-up survey (e.g., forced sexual contact, being attacked with a weapon). Because this variable was also positively skewed, we recoded values 3+ to the value of 2, creating a scale ranging from 0 to 2. Both of these stressor measures were validated in previous studies and are discussed in detail elsewhere (Boscarino et al., 2004; Boscarino & Adams, 2008).
We included Year 2 social and psychological resources as a latent variable composed of two observed measures: Year 2 social support and Year 2 self-esteem. Social support was the mean of four questions about emotional, informational, and instrumental support available to the respondent in the previous year (Sherbourne & Stewart, 1991). This measure was recoded as a 4-point scale ranging from 0 to 3, representing low to high social support. Current self-esteem was measured by a version of the Rosenberg self-esteem scale (Rosenberg, 1979) and consisted of the mean of five items measured on a 5-point scale. Due to the skewed distribution of the scale and the nonwhole number scores due to some respondents not answering all items, we recoded this scale as follows: 1–2.75 = 1; 2.80–3.25 = 2; 3.40–3.75 = 3; 3.80 = 4; 4.0 = 5. Both social support and self-esteem measures were also used and validated in previous studies (Adams & Boscarino, 2005; Boscarino & Adams, 2008; Boscarino et al., 2004).
Exogenous Variables
Our analyses included two observed measures representing demographic status, gender and income, which were used as control variables. These variables are known predictors of stressful events, psychosocial resources, and psychological problems (Thoits, 1995; Turner, Wheaton, & Lloyd, 1995). Female sex was coded as a binary variable, with female = 1 and male = 0. Annual household income was coded on a 7-point scale (coded 1–7), representing < $20,000 to > $100,000. For those who did not answer the income question at baseline, we asked this at follow-up and substituted these answers for baseline income data.
To control for predisaster mental status we used two variables: History of predisaster depression and history of predisaster panic attack. Both of these were based on DSM-IV criteria and were determined based on reported age of onset for these disorders at the baseline interview, respectively.
Data Analysis
In our data analysis, we describe the characteristics of our population and present bivariate correlations among the variables in our SEM (Tables 1 and 2). We examine all of the variables to confirm that our coding decreased both skewness and kurtosis. Next, we present the results of our SEM: standardized coefficients and goodness-of-fit statistics. As noted, our analyses builds on earlier work (Adams & Boscarino, 2005; Boscarino & Adams, 2009), and examines the indirect effect of perievent panic on later PTSD via earlier PTSD, stressor events, and psychosocial resources. Preliminary analyses were conducted using SPSS Version 17 (Norusis, 2009). There were no missing data for gender and, as noted above, we substituted the mean income for those missing information on this variable. We also did not have missing data on World Trade Center Disaster exposure, mental health status (i.e., predisaster panic and depression, perievent panic, Year 1 and Year 2 PTSD), or Year 2 stressor event (i.e., trauma exposure and negative life events) measures. Finally, there were two cases with missing data on social support and three with missing data on self-esteem. For both scales, we substituted the mean for the missing data.
Table 1.
Key Study Variables and Baseline Characteristics
| Variables in the model | % | n |
|---|---|---|
| Gender | ||
| Male | 46.2 | 693 |
| Female | 53.8 | 988 |
| Lifetime depression predisaster | ||
| No | 87.0 | 1366 |
| Yes | 13.0 | 315 |
| Lifetime panic disorder predisaster | ||
| No | 88.0 | 1444 |
| Yes | 12.0 | 237 |
| Perievent panic attack | ||
| No | 89.7 | 1451 |
| Yes | 10.3 | 230 |
| Variables in the model | Mean | SD |
| Income | 3.85 | 2.10 |
| World Trade Center Disaster exposure | 2.02 | 1.31 |
| Year 2 negative life events | 0.52 | 0.79 |
| Year 2 trauma exposures | 0.21 | 0.53 |
| Year 2 self-esteem past year | 3.60 | 1.37 |
| Year 2 social support past year | 1.73 | 0.84 |
| Year 1 reexperiencing symptoms | 0.59 | 1.12 |
| Year 1 avoidance symptoms | 0.88 | 1.49 |
| Year 1 arousal symptoms | 0.96 | 1.35 |
| Year 2 reexperiencing symptoms | 0.61 | 1.21 |
| Year 2 avoidance symptoms | 0.97 | 1.73 |
| Year 2 arousal symptoms | 0.97 | 1.44 |
Note. N = 1,681 for means. All percentages are weighted; all ns are unweighted.
Table 2.
Pearson’s Correlations Among Manifest (Observed) Variables in the Structural Equation Model
| Study variables | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Female | −.14 | −.05 | −.004 | .01 | .08 | .04 | .07 | −.02 | .01 | .07 | .03 | .10 | .09 | .04 | .11 |
| 2. Y1 Income | .12 | .06 | .03 | −.10 | .01 | .03 | .23 | .31 | −.05 | −.07 | −.02 | −.14 | −.13 | −.10 | |
| 3. Y1 WTCD Expos. | .09 | .002 | .20 | .16 | .09 | −.08 | .01 | .19 | .18 | .17 | .15 | .15 | .17 | ||
| 4. Y1 Dep. pre-WTCD | .11 | .09 | .15 | .06 | −.18 | −.01 | .28 | .24 | .28 | .19 | .18 | .19 | |||
| 5. Y1 Panic pre-WTCD | .07 | .04 | .06 | −.04 | .04 | .09 | .07 | .14 | .10 | .06 | .08 | ||||
| 6. Y1 Perievent panic | .16 | .08 | −.16 | −.10 | .25 | .19 | .21 | .21 | .26 | .22 | |||||
| 7. Y2 Negative events | .26 | −.17 | −.05 | .20 | .19 | .21 | .31 | .33 | .32 | ||||||
| 8. Y2 Trauma events | −.11 | −.04 | .09 | .11 | .13 | .21 | .17 | .22 | |||||||
| 9. Y2 Self-esteem | .29 | −.19 | −.21 | −.22 | −.37 | −.40 | −.36 | ||||||||
| 10. Y2 Social support | −.06 | −.10 | −.08 | −.15 | −.17 | −.19 | |||||||||
| 11. Y1 Reexperience | .51 | .56 | .39 | .32 | .35 | ||||||||||
| 12. Y1 Avoid | .51 | .34 | .36 | .34 | |||||||||||
| 13. Y1 Arousal | .36 | .36 | .39 | ||||||||||||
| 14. Y2 Reexperience | .58 | .58 | |||||||||||||
| 15. Y2 Avoid | .65 | ||||||||||||||
| 16. Y2 Arousal | – |
Note. All correlations are from weighted survey data. WTCD = World Trade Center Disaster; Y1 = Year 1; Y2 = Year 2. All correlations greater than .08 are significant at p < .001.
For SEM we created a weighted correlation matrix using the survey weights discussed. We used AMOS Version 17.0 (Arbuckle, 2008), for our SEM modeling and used maximum likelihood estimation. We included PTSD symptom clusters for both Year 1 and Year 2 and began by allowing the error terms for each symptom group from the Year 1 measure to correlate with their counterpart in the Year 2 measure. For assessment of SEM model fit, we used the root mean square error of approximation (RMSEA), Bentler-Bonett normed fit index (NFI), and comparative fit index (CFI; Arbuckle, 2008). Generally, a CFI and NFI greater than .90 and a RMSEA less than .10 indicate adequate model fit (Bryne 2010; 2008; Kline 2005). Finally, we assessed the possibility that Year 2 stressors and psychosocial resources mediate the effect of perievent panic on Year 2 PTSD. Within the SEM framework, an exogenous variable’s association with an endogenous variable contains two components: a direct effect and an indirect or mediated effect. The total effect that an independent variable has on a dependent variable is the sum of the direct and indirect effects (Kline, 2005). We examined the total, direct, and indirect effects of perievent panic on Year 2 PTSD to further examine the associations among these variables. Significant p values in our analyses were defined as those < .05 and were based on two-tailed tests.
RESULTS
As can be seen in Table 1, about 54% of study respondents were female. In addition, in terms of psychological health, Table 1 indicates that 13% of residents had a history of predisaster depression and 12% had a history of predisaster panic attacks. Furthermore, over 10% met the DSM-IV criteria for a perievent panic attack. The means and standard deviations are also given for the other observed SEM study variables.
Bivariate Pearson’s correlation coefficients among the observed variables in the SEM model are presented in Table 2. As can be seen, experiencing a perievent panic attack is associated with all of the PTSD symptom subscales for both Year 1 and Year 2. In particular, perievent panic is associated with Year 1 reexperiencing, avoidance, and arousal symptoms (p < .001), as well as the Year 2 measures of these variables (p < .001). Higher exposure to World Trade Center Disaster events is also associated with these PTSD symptom clusters (p < .001). Finally, having a perievent panic attack is positively associated with greater exposure to World Trade Center Disaster events (p < .001).
SEM Model: Direct Effects
Although these correlations are suggestive, due to confounding, the longer-term direct impact of perievent panic on mental health status cannot be inferred from these data. Therefore, we assessed the direct effects of perievent panic on Year 1 and Year 2 PTSD measured as latent constructs, controlling for other factors. Our SEM contained 4 latent variables (Year 1 and Year 2 PTSD, Year 2 stressors, and Year 2 psychosocial resources) and 16 observed variables. The two PTSD latent variables had three indicator variables: re-experiencing, avoidance, and arousal symptoms. As described, we initially allowed the error terms for each Year 1 symptom group to correlate with its Year 2 counterpart. All of the exogenous variables (i.e., demographic and predisaster mental health measures) were allowed to correlate with each other. We also allowed all of these measures to have direct effects on all of the endogenous variables (e.g., income on exposure, perievent panic, stressor events, psychosocial resources, Year 1 PTSD, and Year 2 PTSD). The model specified direct effects between all Year 1 endogenous and Year 2 endogenous variables (e.g., perievent panic on Year 2 stressor events, Year 2 psychosocial resources, Year 2 PTSD) and contained 4 observed exogenous variables, 12 observed endogenous variables, 4 unobserved endogenous variables, and 16 unobserved endogenous variables, for a total of 36 variables. The model also estimated 9 covariances and 20 variances. With 136 distinct sample moments, 73 parameter estimates, the model had a χ2 = 187.89 (df = 63, p < .001). Although this χ2 indicated a poorly fitting model, other indices suggest an adequate fit, with a root mean square error of approximation (RMSEA) = .034, 90% CI [.029, .040], Bentler-Bonett normed fit index (NFI) = .966, and comparative fit index (CFI) = .977. To improve the model’s parsimony and reduce the possibility that we overcontrolled for the predisaster panic mental health measure, we eliminated non-significant direct pathways for this measure. After these changes, we recalculated all parameter estimates. The new model contained 136 distinct sample moments, 69 parameter estimates, and a χ2 = 189.77 (df = 67, p < .001). Based on the fit statistics, this second specified model fit the data well, with a RMSEA = .033, 90% CI [.028, .039], NFI = .966, and CFI = .977. For this model, we did not add any correlations or make other changes based on the modification indices.
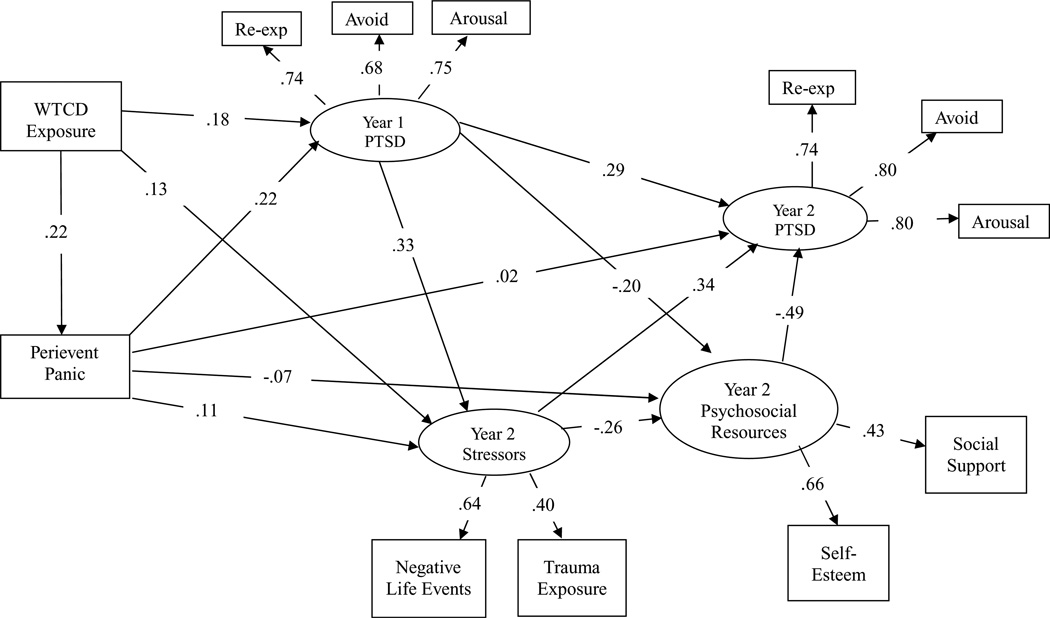
Figure 1 presents a simplified depiction of the final structural model with standardized coefficients, indicating significant direct paths and omitting correlated error terms. (A complete final SEM model is available from the corresponding author.) As can be seen in Figure 1 and Table 3, World Trade Center Disaster exposure increases the likelihood of a perievent panic attack, Year 1 PTSD, and Year 2 stressor events (p < .001). Perievent panic is directly related to Year 1 PTSD (β = .22, p < .001), but not to Year 2 PTSD (β = .02, p = .461). Perievent panic also increases Year 2 stressor events and lowers Year 2 psychological resources (p = .025). Year 1 PTSD is positively related to greater Year 2 stressor events (β = .33, p< .001), negatively related to Year 2 psychological resources (β = −.20, p < .001), and positively related to Year 2 PTSD (β = .29, p < .001). As expected, both Year 2 stressor events and Year 2 psychosocial resources are associated with Year 2 PTSD (β = .34 and −.49, respectively, p < .001).
Figure 1.
Simplified depiction of final structural equation model for posttraumatic stress disorder (N = 1681). WTCD = World Trade Center disaster; PTSD = posttraumatic stress disorder; Year 1 = baseline survey, Year 2 = follow-up survey. Control variables in the model include gender, income, pre-WTCD depression, and pre-WTCD panic. Re-exp = reexperiencing (Criterion B), avoid = avoidance (Criterion C), and arousal = hyperarousal (Criterion D).
Table 3.
Structural Equation Model Showing β Coefficients for Direct Effects Linking Demographic, Pre-WTCD Mental Health, Exposure, Perievent Panic, Stressor Events, Psychosocial Resources, and PTSD
| Variables in the model |
WTCD Exposure β |
Perievent Panic β |
Year 1 PTSD β |
Year 2 Stressor events β |
Year 2 Psychosocial Resources β |
Year-2 PTSD β |
|---|---|---|---|---|---|---|
| Female gender | −.04 | .08** | .08** | .06 | .09** | .05 |
| Y1 Income | .11*** | −.12*** | −.07** | .05 | .44*** | .08* |
| Y1 Depression pre-WTCD | .09*** | .07** | .33*** | .07 | −.10** | −.05 |
| Y1 Panic pre-WTCD | – | .07** | .09*** | – | – | – |
| Y1 WTCD Exposure | – | .22*** | .18*** | .13*** | .01 | – |
| Y1 Perievent panic attack | – | – | .22*** | .11** | −.07* | .02 |
| Y1 PTSD | – | – | – | .33*** | −.20*** | .29*** |
| Y2 Stressor events | – | – | – | – | −.26*** | .34*** |
| Y2 Psychosocial resources | – | – | – | – | – | −.49*** |
| R2 = | .02 | .07 | .25 | .22 | .40 | .71 |
Note. N = 1,681. Only significant results shown, except for key perievent panic pathways. All β coefficients are from weighted survey data. WTCD = World Trade Center Disaster; PTSD = posttraumatic stress disorder; Y1 = Year 1; Y2 = Year 2.
< .05.
< .01.
< .001.
Further examination of variables in the model (Table 3), suggests that income and predisaster depression were associated with greater exposure to the World Trade Center Disaster (p < .001). For perievent panic, income lowered the likelihood of this outcome (p < .001), whereas being female (p = .002), and having predisaster depression (p = .006) and having predisaster panic (p = .004), increased the likelihood of a perievent panic attack. Gender (p = .003), income (p = .008), history of depression (p < .001), and panic predisaster (p < .001) were related to Year 1 PTSD, with income the only predictor to be negatively related to this endogenous variable. None of the demographic or predisaster variables were related to Year 2 stressor events. Being female (p =.007) and having a higher income (p <.001) increased Year 2 psychological resources, whereas predisaster depression decreased these resources (p = .004). Finally, none of the demographics or predisaster mental health measures was associated with Year 2 PTSD, except income (p = .046).
SEM Model: Indirect Effects (Mediation)
Mediation is suggested when an independent variable has an association with a dependent variable and the former also has an association with a mediation variable and, in addition, when the association between the independent and dependent variable is significantly reduced after the mediated variable is included in the model. As suggested, the total effect an independent variable has on a particular dependent variable is the sum of the direct and indirect effects. For brevity, we examine the direct, indirect, and total effects of perievent panic on Year 2 PTSD, as mediated by Year 1 PTSD, Year 2 stressor events, and Year 2 psychological resources.
As noted earlier, our SEM analyses show that perievent panic had no direct effect on Year 2 PTSD (β = .02, ns). The standardized total effect of perievent panic on Year 2 PTSD is β = .22 (p < .001), which means that the indirect or mediated effect of perievent panic on Year 2 PTSD is .20 (.22− .02 = .20). More specifically, individuals who meet criteria for perievent panic have about a .22 standard deviation increase in the probability of having PTSD2 years after the World Trade Center Disaster. However, that increase is almost entirely due to the fact that those individuals who have a perievent panic attack are also more likely to meet criteria for Year 1 PTSD, experience more stressor events between Year 1 and Year 2 postdisaster, and have fewer psychological resources 2 years postdisaster. We examined alternative models, which excluded Year 1 PTSD, Year 2 stressor events, or Year 2 psychological resources, respectively. The direct effect of perievent panic on Year 2 PTSD for these different specifications was .08 (p = .005), .07 (p = .008), and .08 (p = .002). Thus, it appears that perievent panic is about equally mediated by Year 1 PTSD, Year 2 stressor events, and Year 2 psychological resources in its effect on Year 2 PTSD.
DISCUSSION
Recent studies suggested that perievent panic may have prognostic value for predicting mental health disorders (Baillie & Rapee, 2005;Goodwin & Hamilton, 2002a, 2002b). In the current study, although perievent panic was related to Year 1 PTSD, it was not uniquely associated with Year 2 PTSD following the World Trade Center Disaster, confirming an earlier finding (Boscarino & Adams, 2009). The association between perievent panic and Year 2 PTSD was almost completely mediated by Year 1 PTSD and Year 2 stressor events and psychological resources, suggesting that as a predictor, perievent panic offers little additional information beyond predicting shorter-term (i.e., Year 1) PTSD status.
A second finding was that perievent panic directly influenced Year 1 PTSD, and Year 2 stressor events and psychological resources, all of which were directly related to Year 2 PTSD. Thus, though not directly associated with Year 2 PTSD, perievent panic does appear to have indirect effects on this outcome. Therefore, the significance of perievent panic for Year 2 PTSD is important as it relates to subsequent exposure to stressor events and on the availability of future psychological resources.
It has been suggested that the impact of disasters often operates on both an individual and a community level, placing large numbers of persons at potential risk (Kaniasty & Norris, 2008). The interconnection of individual psychological problems within the larger postdisaster context is often discovered in studies of disasters (e.g., Adams & Boscarino, 2006; Adams et al., 2002; Adeola, 2009). Our study suggests a sequence of events with trauma increasing the likelihood of perievent panic onset, which lowers psychological resources and increases stressor events, leading to the onset of later psychological problems. These results support Hobfoll’s conservation of resources theory (Hobfoll 1989) and the stress proliferation theory (Pearlin, Aneshensel, & Leblanc 1997), in that an initial stressful event (i.e., World Trade Center Disaster) leads to a host of other psychological and interpersonal problems, which proliferate into other areas of life. Perievent panic also increases the likelihood of Year 1 PTSD, which also lowers psychological resources and increases stressor events. Although PTSD and perievent panic may reflect underlying psychopathologies (e.g., anxiety/mood disorders), these problems can be exacerbated by social and interpersonal events related to exposure to a major stressful event, like a community-wide disaster. Adeola (2009), in her study of Katrina survivors, for instance, shows that greater exposure to this disaster (as measured by property damage and other financial impacts) is associated with greater psychological distress.
The current study has several strengths and limitations. A major strength was that our study involved a large-scale random survey among a multiethnic urban population. We also assessed a range of psychological and interpersonal measures over a 2-year period using standardized instruments. Finally, we used SEM to examine the multiple pathways in which trauma, psychological resources, and mental health status interrelate.
Potential study limitations include that we omitted individuals without a telephone, those who were in institutions, and those who did not speak either English or Spanish. Given that our study’s final completion rate was lower than desired, nonresponse bias also could have affected our results. Another limitation was that we conducted our study among a population experiencing multiple terrorism events (Boscarino, Adams, Figley, Galea, & Foa, 2006), which may have affected our results. A further limitation was that several of our measures did not cover the exact same timeframe. Our Year 2 measure of social support, for example, covers the year prior to the survey, whereas our other Year 2 psychological resource variable is for “current” self-esteem. Future studies should have variables that measure the same underlying concept assessed for the same period. Finally, as with most disaster studies, we did not have any predisaster measures of mental health status (e.g., PTSD). We did establish several retrospective indicators of panic and depression (e.g., predisaster panic and depression) based on age of onset, but these variables may suffer from recall bias.
Despite these limitations, our study suggests that though perievent panic seems to have a direct association with postdisaster stressor events and psychological resources, it does not have a direct effect on longer-term (i.e., Year 2) PTSD, once other factors are taken into account. Perievent panic does have shorter-term effects on PTSD, which has consequences for stressor events, psychological resources, and long-term PTSD. Given these results, the predictive value of perievent panic may be limited within a psychotherapeutic context as an indicator for interventions directed at long-term PTSD status. The best predictors of Year 2 PTSD was not perievent panic, but Year 1 PTSD, Year 2 stressor events, and Year 2 psychosocial resource variables, similar to what has been reported for delayed PTSD (Adams & Boscarino, 2006). These social and psychological variables are clearly interrelated with mental health status. Perievent panic may reflect more fundamental psychological problems originating prior to the World Trade Center Disaster, but worsened by it. Thus, we suggest caution with respect to making clinical inferences related to intrapsychic processes or therapeutic interventions based on perievent panic alone. Although perievent panic may have shorter-term mental health consequences, our findings suggest that interventions focused on improving psychological resources and reducing stressor events in the posttrauma period may be more beneficial in reducing longer-term mental health problems.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (Grants # R01 MH66403 and R21-MH-086317) and the Pennsylvania Department of Health (Contract #4100042573), to Dr. Boscarino.
Footnotes
A version of this paper was presented at the 137th Annual Meeting of the American Public Health Association, Philadelphia, November 2009.
Contributor Information
Richard E. Adams, Department of Sociology, Kent State University
Joseph A. Boscarino, Center for Health Research, Geisinger Clinic
REFERENCES
- Adams RE, Boscarino JA. Stress and well-being in the aftermath of the World Trade Center attack: The continuing effects of a community-wide disaster. Journal of Community Psychology. 2005;33:175–190. doi: 10.1002/jcop.20030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. Predictors of PTSD and delayed-PTSD after disaster: The impact of exposure and psychological resources. Journal of Nervous and Mental Disease. 2006;194:485–493. doi: 10.1097/01.nmd.0000228503.95503.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA, Galea S. Social and psychological resources and health outcomes after World Trade Center disaster. Social Science & Medicine. 2006;62:176–188. doi: 10.1016/j.socscimed.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Bromet EJ, Panina N, Golovakha E, Goldgaber D, Gluzman S. Stress and well-being after the Chornobyl nuclear power plant accident. Psychological Medicine. 2002;32:143–156. doi: 10.1017/s0033291701004676. [DOI] [PubMed] [Google Scholar]
- Adeola FO .Mental health and psychological distress sequelae of Katrina: An empirical study of survivors. Human Ecology Review. 2009;16:195–210. [Google Scholar]
- American Association for Public Opinion Research. Standard definitions: Final dispositions of case codes and outcomes rates for surveys. Ann Arbor, MI: Author; 2008. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-IV, Fourth Edition. Washington, DC: Author; 1994. [Google Scholar]
- Arbuckle JL. Amos 17.0 user’s guide. Chicago, IL: SPSS Inc.; 2008. [Google Scholar]
- Baillie AJ, Rapee RM. Panic attacks as risk markers for mental disorders. Social Psychiatry and Psychiatric Epidemiology. 2005;40:240–244. doi: 10.1007/s00127-005-0892-3. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Psychobiologic predictors of disease mortality after psychological trauma: Implications for research and clinical surveillance. Journal of Nervous and Mental Disease. 2008;196:100–107. doi: 10.1097/NMD.0b013e318162a9f5. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE. Overview of findings from the World Trade Center Disaster Outcome Study: Recommendations for future research after exposure to psychological trauma. International Journal of Emergency Mental Health. 2008;10:275–290. [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE. Peritraumatic panic attacks and health outcomes two years after psychological trauma: Implications for intervention and research. Psychiatry Research. 2009;167:139–150. doi: 10.1016/j.psychres.2008.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. Mental health service use 1-year after the World Trade Center disaster: Implications for mental health care. General Hospital Psychiatry. 2004;26:346–358. doi: 10.1016/j.genhosppsych.2004.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR, Galea S, Foa EB. Fear of terrorism and preparedness in New York City 2 years after the attacks: Implications for disaster planning and research. Journal of Public Health Management and Practice. 2006;12:505–513. doi: 10.1097/00124784-200611000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. 2nd ed. New York, NY: Routledge; 2010. [Google Scholar]
- Centers for Disease Control and Prevention. Deaths in World Trade Center terrorist attacks—New York City, 2001 [Special issue] Mortality and Morbidity Weekly Report. 2002;51:16–18. [PubMed] [Google Scholar]
- Freedy JR, Kilpatrick DG, Resnick HS. Natural disasters and mental health: Theory, assessment, and intervention [Special issue] Journal of Social Behavior and Personality. 1993;8:49–103. [Google Scholar]
- Galea S, Ahren J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine. 2002;346:982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Brook JS, Cohen P. Panic attack and the risk of personality disorder. Psychological Medicine. 2005;35:227–235. doi: 10.1017/s0033291704003319. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Hamilton SP. Early-onset fearful panic attack: A possible prodrome of early-onset of severe psychopathology. Comprehensive Psychiatry. 2002a;43:22–27. doi: 10.1053/comp.2002.29848. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Hamilton SP. The early onset fearful panic attack as a predictor of severe psychopathology. Psychiatry Research. 2002b;109:71–79. doi: 10.1016/s0165-1781(01)00357-2. [DOI] [PubMed] [Google Scholar]
- Groves RM, Fowler FJ, Couper MP, Lepkowski JM. Survey methodology. New York: Wiley; 2004. [Google Scholar]
- Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist. 1989;44:513–524. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- Kaniasty K, Norris FH. Longitudinal linkages between perceived social support and posttraumatic stress symptoms: Sequential roles of social causation and social selection. Journal of Traumatic Stress. 2008;21:274–281. doi: 10.1002/jts.20334. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Jin R, Ruscio AM, Shear K, Walters EE. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2006;63:415–424. doi: 10.1001/archpsyc.63.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Little RJ, Groves RM. Advances in strategies for minimizing and adjusting for survey nonresponse. Epidemiologic Reviews. 1995;17:192–204. doi: 10.1093/oxfordjournals.epirev.a036176. [DOI] [PubMed] [Google Scholar]
- Kline RE. Principle and practice of structural equation modeling. New York, NY: Guilford Press; 2005. [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. New York: NY: Brunner/Mazel; 1990. [Google Scholar]
- Lawyer SR, Resnick HS, Galea S, Ahern J, Kilpatrick DG, Vlahov D. Predictors of peritraumatic reactions and PTSD following the September 11th terrorist attacks. Psychiatry. 2006;69:130–141. doi: 10.1521/psyc.2006.69.2.130. [DOI] [PubMed] [Google Scholar]
- Nixon RD, Resick PA, Griffin MG. Panic following trauma: The etiology of acute posttraumatic arousal. Journal of Anxiety Disorders. 2004;18:193–210. doi: 10.1016/S0887-6185(02)00290-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- North CS, Pfefferbaum B, Tivis L, Kawasaki A, Reddy C, Spitznagel EL. The course of posttraumatic stress disorder in a follow-up study of survivors of the Oklahoma City bombing. Annals of Clinical Psychiatry. 2004;16:209–215. doi: 10.1080/10401230490522034. [DOI] [PubMed] [Google Scholar]
- Norusis M. SPSS 17.0 Guide to data analysis. New York, NY: Prentice Hall; 2009. [Google Scholar]
- Pearlin LI, Aneshensel CS, Leblanc AJ. The forms and mechanisms of stress proliferation: The case of AIDS caregivers. Journal of Health and Social Behavior. 1997;38:223–236. [PubMed] [Google Scholar]
- Picou JS, Marshall BK, Gill DA. Disaster, litigation and the corrosive community. Social Forces. 2004;82:1493–1522. [Google Scholar]
- Robins LN, Cottler LB, Bucholz KK, Compton WM, North CS, Rourke KM. Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Washington University School of Medicine, Department of Psychiatry; 1999. [Revised January 9, 2002]. [Google Scholar]
- Rosenberg M. Conceiving the self. New York, NY: Basic Books; 1979. [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science in Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Thoits P. Stress, coping and social support processes: Where are we? What next? Journal of Health and Social Behavior. 1995;35:53–79. [PubMed] [Google Scholar]
- Turner RJ, Wheaton B, Lloyd DA. The epidemiology of social stress. American Journal of Sociology. 1995;60:104–125. [Google Scholar]