Abstract
Previous research suggested that community-level mental health service use was low following the World Trade Center Disaster (WTCD) and that brief interventions were effective. In the current study, we assess service use during a longer follow-up period and compare the effectiveness of brief versus multisession interventions. To assess these, we conducted baseline diagnostic interviews among New York City residents 1 year after the WTCD (N = 2368) and follow-up interviews 2 years afterward (N = 1681). At follow-up, there was an increase in mental health utilization, especially for psychotropic medication use, and a decrease in use of physicians for mental health treatment. The best predictor of service use at follow-up was higher WTCD exposure. Using propensity score matching to control for selection bias, brief mental health interventions appeared more effective than multisession interventions. These intervention findings held even after matching on demographic, stress exposure, mental health history, treatment history, access to care, other key variables. Our study suggested that community-level mental health service use increased in the follow-up period and that brief interventions were more effective than conventional multisession interventions. Since this study was designed to assess treatment outcomes, our findings raise clinical questions.
Keywords: Mental health services, posttraumatic stress disorder, alcohol abuse, depression, treatment outcomes, comparative effectiveness, brief interventions, propensity scores
Although the psychological consequences following disasters often appear brief, studies suggest that events characterized by a large-scale loss of life, economic disruptions, and those related to human intent result in increased psychiatric disorders (Brewin et al., 2000; Bromet and Dew, 1995; Rubonis and Bickman, 1991). All of these were present in the terrorist attacks in New York City (NYC) on September 11, 2001(Centers for Disease Control and Prevention, 2002). Although changes in postdisaster mental health service utilization have been documented before the World Trade Center disaster (WTCD) (Smith et al., 1999), few have focused on population-level mental health utilization and the prospective impact of this on mental health status (Boscarino et al., 2003a,b).
To estimate service use and outcomes in NYC after the WTCD, we conducted structured diagnostic interviews among a random sample of community-based adults by telephone. These interviews were conducted at 12 months (baseline) and at 24 months (follow-up) after the attack (Boscarino and Adams, 2008). Twelve months after the disaster, initial research indicated that despite the availability of federal, state, and local postdisaster mental health services through the federally funded Project Liberty (Donahue et al., 2006a,b; Felton, 2002), increased mental health utilization failed to materialize (American Psychiatric Association, 2002; Boscarino et al., 2004a,b). Project Liberty was a New York State mental health program funded by the Federal Emergency Management Agency. This program was implemented in May 2002 and by August 2003, was reported to have delivered mental health services to a large number of area residents (Donahue et al., 2006a,b; Felton, 2002). In addition, examination of the effectiveness of these mental health services suggested that, with the exception of brief work-site psychosocial interventions, conventional interventions, including psychotherapy sessions and psychotropic medications, appeared ineffective (Boscarino and Adams, 2008). The objectives of the current study are as follows: (i) To describe trends in service use from the predisaster through the follow-up period, and (ii) To assess the comparative effectiveness of brief mental health interventions received compared with conventional multisession therapeutic interventions.
METHODS
Sample Selection and Data Collection
All English or Spanish-speaking adults, 18 years old or more, living in NYC at the time of the attack with telephone access were eligible for this study. Using random-digit dialing, a baseline telephone survey was conducted 1-year after the WTCD attack. As part of the study design, residents who reported receiving mental health treatment a year after the attack were over-sampled at the beginning of the survey (Boscarino et al., 2004a). The baseline survey was also stratified by the 5 NYC boroughs and sampled proportionately. Interviews were conducted in English and Spanish. The baseline interview was conducted between October and December 2002, and the follow-up was conducted between October 2003 and February 2004. Experienced interviewers using computer-assisted telephone interviewing technology conducted the interviews. The institutional review board (IRB) of the New York Academy of Medicine approved the study’s original protocol and the Geisinger Health System IRB serves as the IRB of current record for this study.
For the baseline survey, 2368 residents completed the interview. We were able to reinterview 1681 of these respondents in the follow-up survey. Using standard survey definitions (American Association for Public Opinion Research, 2008), our baseline cooperation rate was 63% and our completion rate for the follow-up survey was 71% (Adams and Boscarino, 2006), consistent with previous epidemiological investigations (Galea et al., 2002). Sampling weights were developed for baseline and follow-up interviews, respectively. These adjusted for potential selection bias related to the number of telephone numbers/persons per household and for the over-sampling of treatment-seeking respondents (Boscarino et al., 2004a). Demographic weights also were used with the follow-up data, to adjust for slight variations in response rates by different demographic groups, a common practice in panel surveys (Groves et al., 2004). With these survey adjustments, the study data are representative of adults who were living in NYC on the day of the WTCD attack (Adams et al., 2006).
Conventional Mental Health Interventions
For our mental health intervention measures, we adopted those used in the National Comorbidity Survey (Kessler et al., 1999). For both the baseline and follow-up surveys, we surveyed participants about receiving counseling from a helping professional (e.g., psychiatrist, counselor, physician, self-help group, etc.) for 30 minutes or more for “problems with emotions or nerves or use of alcohol or drugs” at 1 year and 2 years after the attack. Following this, respondents were asked how many sessions they received and the therapeutic content of these sessions (Boscarino et al., 2004a). Finally, respondents who had postdisaster visits were asked if these were related to the WTCD. As reported elsewhere, these service-use questions were also pretested before implementation and had been used in earlier WTCD surveys (Boscarino et al., 2002). In both our baseline and follow-up surveys, psychotropic medication use was pretested and assessed in a similar manner and also adapted from the National Comorbidity Survey (Kessler et al., 1999). More specifically, respondents were asked if they had taken any medications prescribed by a doctor, such as antidepressants, tranquilizers, or sleeping pills for emotional or mental health problems within the past 2 years. The specific psychotropic medications taken were also recorded. It is noted that these same mental health utilization and medication questions are now used worldwide as part of the Composite International Diagnostic Interview (Kessler and Ustun, 2004).
Brief Mental Health Interventions
Following survey data collection related to conventional therapeutic interventions as described earlier in the text, respondents were asked if they attended any brief sessions related to coping with the WTCD conducted by a mental health professional or counselor that was arranged by an employer, a community group, religious group, or some other organization, which was common after the WTCD (Boscarino et al., 2005). They were then asked to characterize how many sessions they attended and the content of these sessions. As described elsewhere, approximately 10% of NYC adults (560,000 persons) received these brief interventions in the immediate postdisaster period, with 78% of residents reporting receiving 3 sessions or fewer (Boscarino et al., 2005, 2006). In the current study, those who reported receiving these brief interventions at a worksite, community center, place of worship, or at similar sites, were classified as the “brief intervention” group.
Mental Health Outcomes Assessed
We assessed 8 outcomes associated with mental health status at follow-up, including those related to posttraumatic stress disorder (PTSD), depression, alcohol misuse, and anxiety disorders. PTSD was based on the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (American Psychiatric Association, 2000). This measure was used in the National Women’s Study, developed for telephone administration, and used in previous surveys (Galea et al., 2002; Resnick et al., 1993). To have PTSD, the person had to meet the full diagnostic criteria (A–F) for PTSD (Boscarino and Adams, 2009). This scale was also used as a continuous measure, where the severity of each PTSD symptom in the past month (on a 4-point scale) was summed to produce a severity score (Boscarino et al., 2006). Cronbach alpha for the symptoms used in this scale was 0.90 (Boscarino et al., 2004a), and the validity of this PTSD scale has been reported to be good (Kilpatrick et al., 1998). Versions of this diagnostic scale have been used in mental health surveys involving approximately 15,000 telephone interviews, including several WTCD surveys (Boscarino et al., 2003b, 2004a,b; Boscarino and Adams, 2008; Galea et al., 2002, 2003; Kilpatrick et al., 2003; Resnick et al., 1993).
For depression, we used a version of a major depressive disorder scale (Spitzer et al., 1987), which also has been used in previous population surveys (Kilpatrick et al., 2003). Consistent with Diagnostic and Statistical Manual of Mental Disorders, fourth edition criteria (American Psychiatric Association, 2000), respondents met criteria for depression if they had 5 or more depression symptoms for at least 2 weeks or more. This scale also had been used in previous WTCD surveys (Boscarino et al., 2002, 2004a,b; Galea et al., 2002). Studies have reported that this scale has good reliability and validity (Boscarino et al., 2004a,b). We also used this scale as a continuous variable by summing the number of symptoms experienced in the past 12 months (Boscarino et al., 2006).
To assess binge drinking (Allen and Columbus, 1995), we asked respondents in the survey to report how many times in the past year they had 6 or more alcoholic drinks on 1 occasion and coded this as a binary variable, classified as monthly or more versus less than monthly. We also inquired about the respondent’s drinking behaviors based on the CAGE dependence scale (King, 1986), a widely used and validated measure (O’Brien, 2008). We defined alcohol dependence as present, if respondents had 2 or more positive answers on this scale (King, 1986).
For anxiety disorder, we included the Brief Symptom Inventory-18 anxiety scale (Derogatis, 2001). We used a T-score of 65 or higher to define an anxiety disorder, representing a symptom score above the 90th percentile. We also used the T-score value of this scale as a continuous variable to measure anxiety symptom burden. As noted elsewhere, the reliability and validity of this scale are reported to be good (Boscarino et al., 2004a; Derogatis, 2001).
Psychological Stressors
Our analyses included 3 psychological stressor measures. One was related to the WTCD, which was the sum of 14 WTCD-related events potentially experienced during or after the attacks (e.g., saw persons killed or injured, was evacuated, lost possessions, etc.). For descriptive purposes, since we had no a priori method to judge the severity of events (Stamm, 1996), we categorized these into low (0–1 event), moderate (2–3 events), high (4–5 events), and very high (6+ events), based on a count of different exposures experienced. For multivariate propensity analyses, we used this measure as a continuous variable. This scale was developed from other disaster studies, had been used in previous WTCD research, and has been described in detail elsewhere (Adams et al., 2006; Boscarino et al., 2004a,b; Freedy et al., 1993; Galea et al., 2002).
A life event scale also was used, which was the sum of 8 negative experiences (e.g., divorce, problems at work, etc.) that could have happened in the past 12 months. This scale was also developed from previous disaster studies, used in earlier WTCD research, and had good reliability and validity (Adams et al., 2006; Boscarino et al., 2004a,b; Freedy et al., 1993; Galea et al., 2002). For descriptive purposes, this scale was collapsed into following categories: 0 event, 1 event, and 2 or more events. For multivariate propensity analyses, we used this measure as a continuous variable.
The third stressor measure assessed 10 traumatic events, other than the WTCD (e.g., forced sexual contact, a serious accident, etc.) (Freedy et al., 1993). Again, since we had no a priori method to judge the severity of these events (Stamm, 1996), for descriptive purposes, we collapsed these exposures into following categories: 0 to 1 event, 2 to 3 events, and 4 or more events. For multivariate analyses, we used this exposure as a continuous variable. As noted elsewhere, this traumatic event scale also was developed from other disaster studies, used in previous research, and had good reliability and validity (Adams et al., 2006; Boscarino et al., 2004a,b; Freedy et al., 1993; Galea et al., 2002).
Psychosocial Resources
Our study also included measures for social support and self-esteem. The social support scale used was a modified version of the measure used in the Medical Outcomes Study (Sherbourne and Stewart, 1991), which has been included in other WTCD studies and considered a highly reliable and valid scale (Adams et al., 2006; Boscarino et al., 2004a,b; Galea et al., 2002). This scale was used as a categorical measure in descriptive analysis (classified as low, medium, and high) and as a continuous variable in multivariate propensity analyses. Self-esteem was measured by the Rosenberg self-esteem (RSE) scale (Rosenberg, 1979). The RSE scale is a widely used measure with good reported reliability and validity, which has been incorporated into hundreds of studies (Blascovich and Tomaka, 1991). For descriptive purposes, we divided this self-esteem measure into 3 categories: low, medium, and high, similar to the social support scale. The RSE scale was also used as a continuous variable in multivariate analyses.
Demographic Variables
Our study also included the following demographic variables: age, education, gender, marital status, ethnicity, income, NYC borough, insurance status, and primary care physician status. Age was collected in years and used as a categorical variable for descriptive purposes and as a continuous variable for multivariate analyses. Education, gender, and marital status, were coded as binary variables, with college graduate, female, and married coded as the indicator variable. Income was coded into categories (from <$29,999 to >$100,000). For multivariate analyses, income was coded as a 5-point ordinal scale. Ethnicity was coded as follows: White, African American, Hispanic, Asian, and “other.” Borough was coded as: Manhattan, Bronx, Brooklyn, Queens, and Staten Island. Having health insurance and having a regular physician were coded as binary measures, respectively.
Additional Measures for Propensity Matching
Our study also included additional measures to enhance propensity score matching of intervention with nonintervention controls (Boscarino et al., 2006). These included history of mental health treatments, attention deficit disorder, depression, and history of antisocial personality disorder. Mental health treatment history included a measure indicating if the respondent was ever treated as an inpatient for mental health problems and used as binary variables. A second measure was based on the number of mental health treatments received by the respondent 12 months before the WTCD and used as an ordinal variable. Attention deficit disorder was based on medical history and used as a binary measure. History of depression was based on having met the criteria for major depression before the WTCD and used as a binary measure. Antisocial personality disorder was based on having screened positive for this disorder at baseline and used as a binary measure. These study measures have been described elsewhere and have been shown to be reliable and valid indicators (Boscarino and Adams, 2008, 2009). To enhance propensity matching, the following 2 additional demographic measures were also included: immigrant status (foreign born vs. not) and language of interview (Spanish vs. English).
Statistical Analyses
Since baseline data were presented in detail elsewhere (Boscarino et al., 2004a; Boscarino and Adams, 2008), we only provide an overview of these results. Next, we describe mental health disorders and service utilization during the 2-year follow-up period. Following this, we report population-level service utilization in the predisaster, baseline, and follow-up periods, respectively. We used the survey estimator commands in Stata, version 9.2 (StataCorp, College Station, TX) (Stata Corporation, 2007), to generate point estimates. This software adjusts for the sampling design, which included case weights to adjust for over-representing persons in households with more telephone lines per adult, the treatment over-sample, and potential response bias (Adams et al., 2006). We also used the survey estimator in Stata to undertake multivariate logistic regressions to predict service utilization. Next, using a propensity score matching algorithms (Boscarino et al., 2006), we assessed the comparative effectiveness of 2 types of treatment interventions after the WTCD (Boscarino and Adams, 2008), including brief emergency mental health interventions (n = 222) and multisession psychotherapeutic sessions (n = 175). This propensity method compares the differences in outcomes between intervention and matched-nonintervention cases at follow-up (Rosenheck et al., 2000). Thus, in our study, the propensity variables predicting “selection” to intervention and consequently used in intervention-control matching, included the following: age, gender, marital status, immigrant status, language, education, income, race, ethnicity, NYC borough, WTCD exposure, recent negative life events, lifetime trauma exposure, social support, self-esteem, antisocial personality, history of depression before WTCD, hospitalized for mental health problems before WTCD, times treated for mental health problems before WTCD, history of attention deficit disorder, health insurance status, and physician status. The statistical objective of using these propensity variables is to remove the residual bias between the study intervention and control groups (Klungel et al., 2004; Rosenheck et al., 2000). Different methods are available for matching (Rosenheck et al., 2000); however, to maximize use of study data, we used 1:5 matching, with 1 intervention case matched to 5 nonintervention controls (Klungel et al., 2004). We used an optimal matching method, whereby the smallest distance (i.e., “nearest neighbor” method) between all possible pairs was specified (Klungel et al., 2004). For analyses, we used Stata, version 9.2 (Stata Corporation, 2007), to generate propensity scores for matching, and for statistical tests. For this propensity matching, as reported elsewhere, we first used the pscore program in Stata to assess the adequacy of propensity matching (Becker and Ichino, 2002; Boscarino et al., 2006). For our final matching algorithm, however, we used nnmatch in Stata to match intervention to controls (Abadie et al., 2004). The nnmatch procedure in Stata is considered superior to other methods, because it permits bias correction and different matching ratios for intervention versus controls (Becker and Ichino, 2002). The final results show the average treatment effects (percent or mean) for the intervention compared with nonintervention group (Boscarino et al., 2006). All p values presented are based on 2-tail tests.
RESULTS
The weighted baseline demographic profile of this study population was the same as the reported NYC census demographics for the year 2000, as previously reported (Adams et al., 2006). As seen in Table 1, the majority of the study population is under 45 years old, did not graduate college, is not married, is non-White, has a household income of less than $100,000 per year, has health insurance coverage, and has a regular physician (Table 1). In addition, the majority of those surveyed had moderate to very high exposure to the WTCD, but had low exposure to other recent negative life events and low exposure to other lifetime traumatic events. About ⅓ of the study sample is classified as having low social support and about ⅓ is classified as having low self-esteem at baseline (Table 1).
TABLE 1.
Baseline Study Profile and Demographic Characteristics (N = 2368)
| Study Variables | Unweighted Na |
Weighted % of Total |
|---|---|---|
| Age | ||
| 18–29 | 483 | 27.22 |
| 30–44 | 866 | 34.21 |
| 45–64 | 726 | 28.75 |
| 65+ | 247 | 9.82 |
| Gender | ||
| Male | 1016 | 46.20 |
| Female | 1352 | 53.80 |
| Education | ||
| Non-college graduate | 1304 | 59.88 |
| College graduate | 1053 | 40.12 |
| Marital status | ||
| Not married | 1433 | 53.32 |
| Married | 935 | 46.68 |
| Race | ||
| White | 1015 | 39.25 |
| African American | 606 | 26.32 |
| Latino | 559 | 25.72 |
| Asian | 99 | 5.20 |
| Other | 89 | 3.51 |
| Household income | ||
| Less than $29,999 | 769 | 30.91 |
| $30,000–$99,999 | 1004 | 40.44 |
| $100,000+ | 317 | 14.02 |
| Not reported | 278 | 14.63 |
| Health insurance | ||
| No | 330 | 16.70 |
| Yes | 2030 | 83.30 |
| Regular doctor | ||
| No | 284 | 14.89 |
| Yes | 2080 | 85.11 |
| Exposure to WTCD | ||
| Low (0–1 events) | 510 | 26.50 |
| Moderate (2–3 events) | 1003 | 43.96 |
| High (4–5 events) | 594 | 22.00 |
| Very high (6+ events) | 261 | 7.53 |
| Recent negative life events | ||
| None | 1197 | 56.19 |
| One | 642 | 26.97 |
| 2 or more | 529 | 16.83 |
| Lifetime traumatic events | ||
| 0, 1 event | 1222 | 57.03 |
| 2, 3 events | 667 | 26.19 |
| 4+ events | 479 | 16.78 |
| Current social support | ||
| Low | 668 | 29.36 |
| Moderate | 825 | 34.14 |
| High | 829 | 36.50 |
| Current self-esteem | ||
| Low | 890 | 34.52 |
| Moderate | 573 | 24.52 |
| High | 893 | 40.96 |
All N are unweighted. Percentages shown represent the weighted data, adjusted for the number of telephone lines and adults in the household, the treatment over-sample, and survey stratification.
WTCD indicates World Trade Center disaster.
The prevalence of PTSD, depression, treatment visits, and psychotropic medication use in the follow-up period is shown in Table 2. As seen, at follow-up, the prevalence of current PTSD over the past 2 years was 8.3% and 5.4% over the past 12 months, respectively. For major depression, these figures were 17.9% and 11.6%, respectively. In addition, nearly 31% of adults had a mental health visit over the past 2 years and 18.6% reported that this was related to the WTCD (Table 2). At follow-up, over the past 12 months, 20.7% reported a treatment visit and 11.6% reported that this visit was related to the WTCD. The results for psychotropic medication use in the follow-up period, while not as prevalent as mental health visits, show a similar pattern (Table 2).
TABLE 2.
Overview of Psychological Disorders and Mental Health Services Utilization at Follow-Up 2 Years After World Trade Center Disaster in New York City (N = 1681)
| Outcomes | Unweighted Na |
Weighted % |
95% CI |
|---|---|---|---|
| Mental health status | |||
| PTSD past 2 yr | 213 | 8.27 | 6.93–9.84 |
| PTSD past 12 mo | 134 | 5.36 | 4.29–6.67 |
| Depression past 2 yr | 421 | 17.87 | 15.83–20.12 |
| Depression past 12 mo | 277 | 11.56 | 9.94–13.41 |
| Mental health treatment visits | |||
| Treatment past 2 yr | 727 | 30.63 | 28.07–33.63 |
| Treatment past 12 mo | 506 | 20.70 | 18.54–23.04 |
| Treatment related to WTCD past 2 yr | 509 | 18.58 | 16.64–20.70 |
| Treatment related to WTCD past 12 mo | 306 | 11.55 | 9.98–13.32 |
| Psychotropic medication use | |||
| Psychotropic medications past 2 yr | 407 | 14.45 | 12.74–16.34 |
| Psychotropic medications past 12 mo | 344 | 12.01 | 10.47–13.75 |
| Psychotropic medications related to WTCD past 2 yr | 235 | 6.94 | 5.92–8.13 |
| Psychotropic medications related to WTCD past 12 mo | 163 | 5.03 | 4.16–6.07 |
All N’s are unweighted; percentages and confidence intervals shown represent weighted data (i.e., after adjustments for the number of telephone lines/adults per household, treatment over-sample, etc.).
CI indicates confidence interval; WTCD, World Trade Center disaster; PTSD, posttraumatic stress disorder.
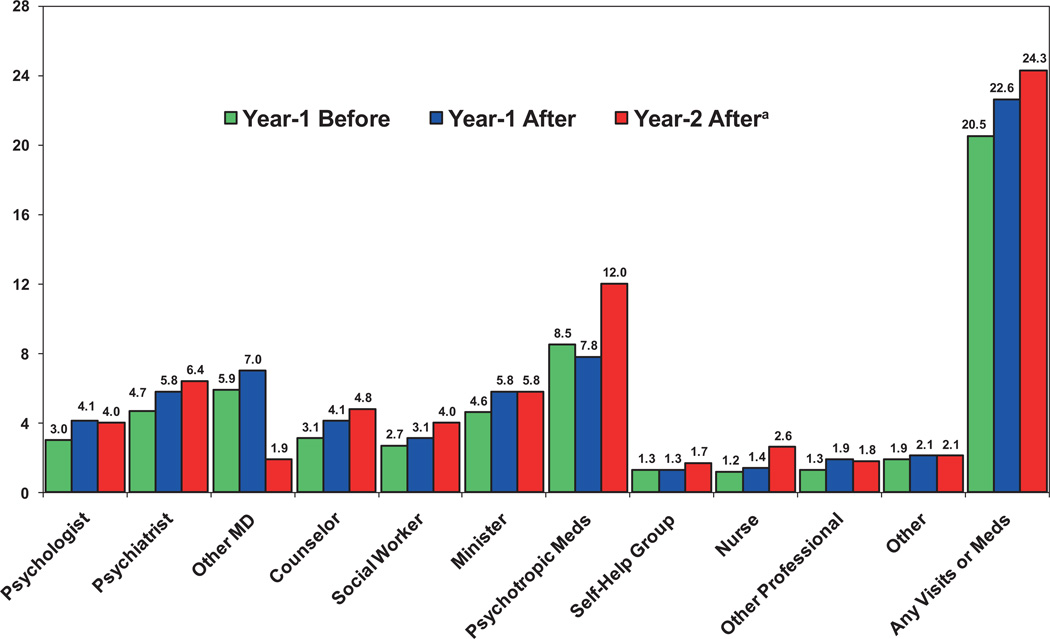
The trends in treatment seeking from predisaster through to year-2 postdisaster are presented in Figure 1. Two findings are noteworthy. First, there appears to be a decrease in mental health treatment provided by medical doctors (predisaster = 5.9%, year-2 postdisaster = 1.9%; p < 0.05). Second, there appears to be an increase in psychotropic medication use during this same period (predisaster = 8.5%, year-2 postdisaster = 12%; p < 0.05). In addition, overall, there appears to be a population-level increase in mental health treatments and psychotropic medication use in NYC during the postdisaster follow-up period, compared with the predisaster period (predisaster = 20.5%, year-2 postdisaster = 24.3%; p < 0.05). These results also show that services were delivered by a broad range of providers in the pre- and postdisaster periods (Fig. 1).
FIGURE 1.
Percent mental health service use year-1 before, year-1 after, and year-2 after the World Trade Center disaster in New York City (N = 1681). aAll predisaster versus year-2 postdisaster differences shown are statistically significant (p < 0.05), except for self-help group, other professional and “other” visits, based on both pre versus follow-up McNemar and the Wilcoxon signed-rank tests, respectively. Percentages shown represent weighted data to adjust the sample for the number of telephone lines and adults in the household, the treatment over-sample, and survey stratification (see methods section). Other professional included alternative health professionals, such as chiropractors, acupuncturists, etc. “Other” included all other nonmedical/nonconventional providers, such as native healers, spiritualists, etc.
Multivariate logistic regression analyses predicting post-WTCD mental health service use over the past 2 years suggested that the best predictor of utilization was level of exposure to the WTCD event (Table 3). As seen in Table 3, however, WTCD exposure was most strongly associated with WTCD-related visits, with an odds ratio of 4.32 (p < 0.001) for those in the high exposure group, compared with those in the low WTCD exposure group. The next best predictors were having an anxiety disorder or major depression. Finally, those in the 30 to 44 age group were more likely to report WTCD-related service use (odds ratio = 3.09, p < 0.001), compared with those in the 65+ age group.
TABLE 3.
Multivariate Logistic Regression Predicting Mental Health Service Visits in Past 2 Years (N = 1681)a
| Any Visitsc (N = 727) |
Increased Visitsc (N = 289) |
WTCD Visitsc (N = 509) |
|||||
|---|---|---|---|---|---|---|---|
| Independent Variablesb | N (%) | Adjusted OR |
Adjusted 95% CI |
Adjusted OR |
Adjusted 95% CI |
Adjusted OR |
Adjusted 95% CI |
| Age | |||||||
| 18–29 | 284 (22.72) | 1.05 | 0.61–1.81 | 0.75 | 0.35–1.61 | 1.74 | 0.92–3.31 |
| 30–44 | 596 (32.88) | 1.52 | 0.92–2.51 | 1.23 | 0.61–2.48 | 3.09* | 1.78–5.36 |
| 45–64 | 586 (32.54) | 1.47 | 0.89–2.42 | 1.03 | 0.53–2.00 | 2.48** | 1.45–4.26 |
| 65+ | 215 (11.87) | 1.00 | — | 1.00 | — | 1.00 | — |
| Gender | |||||||
| Male | 693 (46.20) | 1.00 | — | 1.00 | — | 1.00 | — |
| Female | 988 (53.80) | 1.34*** | 1.01–1.80 | 1.44 | 0.98–2.12 | 1.27 | 0.92–1.76 |
| Race | |||||||
| White | 782 (42.95) | 1.00 | — | 1.00 | — | 1.00 | — |
| African American | 422 (25.96) | 0.69 | 0.37–1.20 | 0.61 | 0.35–1.06 | 0.96 | 0.61–1.51 |
| Latino | 367 (24.09) | 1.30 | 0.76–2.10 | 1.22 | 0.76–1.96 | 1.45 | 0.93–2.27 |
| Asian | 62 (4.56) | 0.47*** | 0.23–0.95 | 0.13*** | 0.27–0.66 | 0.69 | 0.32–1.48 |
| Other | 48 (2.43) | 1.19 | 0.58–2.43 | 1.21 | 0.43–3.40 | 1.23 | 0.55–2.74 |
| Health insurance | |||||||
| No | 200 (14.27) | 0.77 | 0.48–1.23 | 0.49*** | 0.25–0.95 | 0.75 | 0.43–1.31 |
| Yes | 1481 (85.73) | 1.00 | — | 1.00 | — | 1.00 | — |
| Exposure to WTCD | |||||||
| None/low | 362 (26.73) | 1.00 | — | 1.00 | — | 1.00 | — |
| Moderate | 719 (43.93) | 1.96** | 1.33–2.90 | 1.93*** | 1.12–3.35 | 2.95* | 1.77–4.90 |
| High | 416 (21.76) | 1.97** | 1.27–3.06 | 1.83*** | 1.01–3.32 | 4.34* | 2.49–7.55 |
| Very high | 184 (7.58) | 2.08*** | 1.16–3.73 | 1.50 | 0.71–3.19 | 4.32* | 2.26–8.26 |
| Negative life events 2+ | |||||||
| No | 1045 (69.19) | 1.00 | — | 1.00 | — | 1.00 | — |
| Yes | 636 (30.81) | 1.64** | 1.20–2.26 | 1.44 | 0.97–2.15 | 1.26 | 0.88–1.81 |
| Lifetime traumatic events 2+ | |||||||
| No | 838 (55.16) | 1.00 | — | 1.00 | — | 1.00 | — |
| Yes | 843 (44.84) | 1.23 | 0.92–1.63 | 1.15 | 0.78–1.68 | 0.95 | 0.68–1.31 |
| WTCD panic attack | |||||||
| No | 1451 (89.67) | 1.00 | — | 1.00 | — | 1.00 | — |
| Yes | 230 (10.33) | 0.99 | 0.63–1.55 | 0.83 | 0.53–1.31 | 1.50 | 0.94–2.41 |
| Anxiety disorder | |||||||
| No | 1348 (85.88) | 1.00 | — | 1.00 | — | 1.00 | — |
| Yes | 333 (14.12) | 2.34* | 1.48–3.69 | 3.12* | 1.93–5.06 | 3.20* | 2.03–5.06 |
| Low self-esteem | |||||||
| No | 831 (51.82) | 1.00 | — | 1.00 | — | 1.00 | — |
| Yes | 850 (48.18) | 1.04 | 0.77–1.42 | 1.08 | 0.71–1.63 | 0.94 | 0.65–1.34 |
| PTSD | |||||||
| No | 1468 (91.73) | 1.00 | — | 1.00 | — | 1.00 | — |
| Yes | 213 (8.27) | 1.22 | 0.66–1.94 | 1.44 | 0.87–2.39 | 1.37 | 0.82–2.28 |
| Depression | |||||||
| No | 1260 (82.13) | 1.00 | — | 1.00 | — | 1.00 | — |
| Yes | 421 (17.87) | 2.14* | 1.44–3.20 | 1.57 | 0.97–2.53 | 2.26* | 1.48–3.46 |
All odds ratios and confidence intervals shown represent the weighted data, adjusted for the number of telephone lines and adults in the household, the treatment over-sample, and survey stratification.
Other variables in the model, but not shown are marital status, education, income, access to a regular doctor, and level of social support.
Any visits, any visits since WTCD; Increased visits, increase in visits since WTCD; WTCD visits, visits related to WTCD.
p < 0.001.
p < 0.01.
p < 0.05.
WTCD indicates World Trade Center disaster; OR, odds ratio; CI, confidence interval; PTSD, post-traumatic stress disorder.
As suggested, to assess the effectiveness of the post-WTCD interventions we used propensity score matching among those who received brief mental health counseling immediately after this event (n = 222). We then used propensity matching among those who received multisession therapy related to the WTCD in the 12 months after the attack (n = 175). For both interventions, treatment outcomes were assessed at follow-up, 24 months after the WTCD.
As seen for the brief interventions, 5 of the 8 outcomes assessed at follow-up were significantly improved (p < 0.05) for this treatment (Table 4). For example, there was about a 0.8 reduction in mean PTSD symptoms at follow-up for the brief treatment group versus the matched controls (i.e., b = −0.834, p = 0.014). Also noteworthy is that for 2 of the other 3 outcomes assessed, while these were not statistically significant, they were in the negative direction, suggesting that these mental health outcomes trended better for the brief treatment versus the control group. For the multisession psychotherapy group, the results appeared to be opposite. Using the same propensity matching method described, 5 outcomes assessed were significantly worse at follow-up for this intervention group versus the matched control group (all p < 0.05). These included significantly worse outcomes for PTSD diagnosis (p < 0.0001), PTSD symptom level (p = 0.023), depression diagnosis (p = 0.022), anxiety diagnosis (p < 0.0001), and anxiety symptom levels (p < 0.0001).
TABLE 4.
Propensity Score Results Showing Outcome Differences at Follow-Up (Compared to Baseline) for Brief Intervention and Conventional Therapy, Respectively (N = 1681)a
| Brief Intervention (n = 222) |
Conventional Therapy (n = 175) |
||||||
|---|---|---|---|---|---|---|---|
| Treatment Outcomes Examined | Entire Sample %/Mean (N) |
Adjusted b Coefficient |
Adjusted 95% CI |
p | Adjusted b Coefficient |
Adjusted 95% CI |
p |
| % PTSD diagnosis—past 12 mo | 7.97 (134) | 0.002 | −0.032 to 0.035 | 0.910 | 0.149 | 0.088 to 0.210 | <0.0001 |
| Mean PTSD symptoms | 2.39 (1681) | −0.834 | −1.500 to −0.167 | 0.014 | 1.121 | 0.153 to 2.089 | 0.023 |
| % Major depression–past 12 mo | 16.48 (277) | −0.055 | −0.103 to −0.007 | 0.026 | 0.087 | 0.012 to 0.162 | 0.022 |
| Mean depression symptoms—past 12 mo | 2.28 (1681) | −0.385 | −0.741 to −0.030 | 0.033 | 0.409 | −0.079 to 0.896 | 0.101 |
| % Alcohol dependence—past 12 mo | 3.33 (56) | −0.029 | −0.054 to −0.004 | 0.025 | −0.003 | −0.036 to 0.031 | 0.878 |
| % Binge drinking—past mo | 13.86 (233) | −0.023 | −0.073 to 0.028 | 0.378 | −0.026 | −0.087 to 0.035 | 0.403 |
| % Anxiety diagnosis—past 30 d (BSI-18) | 12.91 (217) | −0.055 | −0.095 to −0.015 | 0.007 | 0.131 | 0.065 to 0.197 | <0.0001 |
| Mean anxiety symptoms—past 30 d (BSI-18) | 50.98 (1681) | −0.963 | −2.343 to 0.417 | 0.171 | 3.46 | 1.860 to 5.231 | <0.0001 |
All propensity models were matched 1:5 (intervention to controls) on the following: age, gender, marital status, immigrant status, language, education level, income level, race/ethnicity, NYC borough, insurance status, physician status, WTCD exposures level, negative life events, lifetime trauma exposure, social support, self-esteem, antisocial personality, history of depression before WTCD, hospitalized for mental health problems before WTCD, number of times treated for mental health problems before WTCD, and history of attention deficit disorder.
CI indicates confidence interval; PTSD, posttraumatic stress disorder; BSI-18, brief symptom inventory-18; NYC, New York City; WTCD, World Trade Center disaster.
DISCUSSION
The results of our study suggest that while mental health services did not increase substantially in the 12-month postdisaster period, they did increase somewhat 24 months after the WTCD. This was especially true for use of psychotropic medications (Fig. 1). Conversely, use of medical doctors for mental health support appeared to decrease 24 months after the WTCD. In terms of comparative effectiveness, brief interventions appeared to be superior to conventional psychotherapy interventions. Using robust propensity score matching to assess brief and multisession therapeutic interventions, respectively, indicated that multisession interventions had poorer outcomes. Of course, a key question is could these findings be confounded by indication?
Confounding by indication is a type of selection bias, whereby those who receive a certain treatment might be more ill than those who did not receive that treatment (Grobbee and Hoes, 1997). In clinical effectiveness research, the randomized controlled trial is considered the ideal design, since it enables many sources of bias to be removed from the observed outcomes (Grobbee and Hoes, 1997; Hulley et al., 2007). In observational studies, allocation to treatment is not random. This means that the prognoses of the patient groups studied may not be comparable. Propensity methods were developed to specifically address this problem (Boscarino et al., 2006). In the current study, we used 1:5 matching, with 1 intervention case matched to 5 nonintervention controls. We used an optimal matching method, whereby the smallest distance between all possible pairs was selected. For propensity matching, as suggested, we first used the pscore program in Stata to assess the adequacy of propensity matching. For our final matching algorithm, we used the nnmatch program, which includes additional bias correction adjustments.
It has been noted that while confounding by indication can create problems in assessing treatment effects in nonexperimental studies, these problems are not insurmountable (Guo and Fraser, 2010; Rubin, 2006). Valid inferences can be drawn when the residual dissimilarities in patients receiving treatments can be accounted for or adjusted (Grobbee and Hoes, 1997; Guo and Fraser, 2010; Rubin, 2006). Thus, the effect of confounding can be removed by measuring patient characteristics that formed the basis of this confounding and then by matching for these in the analyses. In the current study, information related to potential confounding was comprehensive. Consequently, the rate/severity of baseline disorders in the treated versus untreated patients was more likely similar. In addition, 2 treatment interventions were compared (e.g., brief vs. conventional treatments) using the same propensity methods. As shown, the brief intervention group exhibited improvement, while the conventional intervention group did not.
Observations drawn from this study, of course, should be interpreted with some caution. We used self-reported data collected by telephone among adult householders, raising the possibility of respondent recall and selection bias. In addition, we surveyed only those who spoke either English or Spanish. However, it is noteworthy that while the differences found for the brief intervention group were not always large, they were consistent and multifaceted. As was seen, these included reductions in PTSD symptoms, major depression, depression symptoms, alcohol dependence, and anxiety disorder at follow-up. Conversely, the results for the psychotherapeutic intervention group were generally worse in these same clinical domains, suggesting that those who received brief interventions benefited as many as 2 years after the WTCD, while those receiving conventional therapy did not.
Postdisaster crisis interventions have been in used in the past. However, the effectiveness and safety of these interventions have been debated (Gist and Devilly, 2002; Roberts et al., 2009; van Emmerik et al., 2002). Our research suggests that emergency mental health services may be associated with better outcomes up to 2 years after a disaster. It is important to stress that this study does not suggest that brief, single-session interventions are effective (van Emmerik et al., 2002). Rather, it suggests that brief mental health interventions conducted by professionals at the worksite, community center, and other places may be effective following a large-scale traumatic event. However, as noted elsewhere, the reasons for this association are unclear (Boscarino et al., 2005, 2006), but may be due to indirect effects, such as later treatment-seeking or by facilitating professional referrals, or by some other indirect treatment effect.
These findings will require replication. A question to be addressed in future research will relate to the effectiveness of brief interventions versus conventional therapy. In particular, it needs to be determined if the differences found are due to residual confounding, such as by selection bias, whereby sicker patients received conventional therapy, or to the iatrogenic effects of receiving delayed, less focused treatments after a traumatic event. Given our results and recent reports stressing the need for additional comparative effectiveness studies (Committee on Comparative Effectiveness Research, 2009), it would be unwise to ignore these findings. Since this research is based on an observational study, it is tempting to suggest that the results are confounded. For example, it is still possible that our results are biased by some unmeasured variable, a limitation with all observational research (Boscarino et al., 2006). However, recent research suggests that early post-trauma interventions may be more effective in eliminating longer-term stress disorders by preventing memory consolidation and accelerating fear extinction (Schiller et al., 2010). Delayed interventions may not have this same impact. Biologically, it is plausible that early interventions may prevent consolidation of fear conditioning and stimulus generalization simply by enhancing better sleep (Lavie, 2001). PTSD is linked to heighted arousal and sleep disturbances, symptoms that define the core syndromes of this disorder. If the latter is correct, then this could, in part, explain the findings reported for brief interventions. Further research is recommended.
Finally, it is important to emphasize that because Project Liberty was available during our study period, which promoted the availability of free crisis counseling, this factor may have affected our results. It is unusual for this type of federally funded mental health care to be made widely available (Felton, 2002). However, as previously suggested, for some reason Project Liberty failed to have a major impact on service use among community-based NYC adults (American Psychiatric Association, 2002; Boscarino et al., 2004). As demonstrated in the current study, there was no huge surge in mental health service use in NYC among community-based adults during Project Liberty. Furthermore, during our follow-up survey we asked respondents, specifically, if they “…ever had any contact with or received any services from Project Liberty.” Less than 5% of NYC adults said that they did have contact with or received services from this program. Thus, while this low percentage could be partly due to recall bias and/or to the ineffective marketing of the Project Liberty “brand name,” it does not appear that the Project Liberty intervention had a major impact on our study population. Alternative explanations and further research are required.
Acknowledgments
Supported (in part) by the National Institute of Mental Health (R01-MH-66403 and R21-MH-086317) and Pennsylvania Department of Health (Contract 4100042573).
REFERENCES
- Abadie A, Drukker D, Herr JL, Imbens GW. Implementing matching estimators for average treatment effects in stata. Stata J. 2004;4:290–311. [Google Scholar]
- Adams RE, Boscarino JA. Predictors of PTSD and delayed PTSD after disaster: The impact of exposure and psychosocial resources. J Nerv Ment Dis. 2006;194:485–493. doi: 10.1097/01.nmd.0000228503.95503.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA, Galea S. Social and psychological resources and health outcomes after the World Trade Center disaster. Soc Sci Med. 2006;62:176–188. doi: 10.1016/j.socscimed.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen JP, Columbus M, editors. Assessing Alcohol Problems: A Guide for Clinicians and Researchers. Bethesda (MD): National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Arlington (VA): American Psychiatric Publishing; 2000. Text Revision. [Google Scholar]
- American Psychiatric Association. Mental illness crisis fails to materialize. Psychiatr News. 2002;37:23. [Google Scholar]
- American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 5th ed. Lenexa (KS): American Association for Public Opinion Research; 2008. [Google Scholar]
- Becker SO, Ichino A. Estimation of average treatment effects based on propensity scores. Stata J. 2002;2:358–377. [Google Scholar]
- Blascovich J, Tomaka J. Measures of self-esteem. In: Robinson JP, Shaver PR, Wrightsman LS, editors. Measures of Personality and Social Psychological Attitudes. San Diego (CA): Academic Press; 1991. p. 115. Measures of Social Psychological Attitudes. [Google Scholar]
- Boscarino JA, Adams RE. Overview of findings from the World Trade Center Disaster Outcome Study: Recommendations for future research after exposure to psychological trauma. Int J Emerg Ment Health. 2008;10:275–290. [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE. PTSD onset and course following the World Trade Center disaster: Findings and implications for future research. Soc Psychiatry Psychiatr Epidemiol. 2009;44:887–898. doi: 10.1007/s00127-009-0011-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. Mental health service use 1-year after the World Trade Center disaster: Implications for mental health care. Gen Hosp Psychiatry. 2004a;26:346–358. doi: 10.1016/j.genhosppsych.2004.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. A prospective cohort study of the effectiveness of employer-sponsored crisis interventions after a major disaster. Int J Emerg Ment Health. 2005;7:9–22. [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Foa EB, Landrigan PJ. A propensity score analysis of brief worksite crisis interventions after the World Trade Center disaster: Implications for intervention and research. Med Care. 2006;44:454–462. doi: 10.1097/01.mlr.0000207435.10138.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Figley CR, Adams RE. Fear of terrorism in New York after the September 11 terrorist attacks: Implications for emergency mental health and preparedness. Int J Emerg Ment Health. 2003a;5:199–209. [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Adams RE, Ahern J, Resnick H, Vlahov D. Mental health service and medication use in New York City after the September 11, 2001, terrorist attack. Psychiatr Serv. 2004b;55:274–283. doi: 10.1176/appi.ps.55.3.274. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Ahern J, Resnick H, Vlahov D. Utilization of mental health services following the September 11th terrorist attacks in Manhattan, New York City. Int J Emerg Ment Health. 2002;4:143–155. [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Ahern J, Resnick H, Vlahov D. Psychiatric medication use among Manhattan residents following the World Trade Center disaster. J Trauma Stress. 2003b;16:301–306. doi: 10.1023/A:1023708410513. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for post-traumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bromet E, Dew MA. Review of psychiatric epidemiologic research on disasters. Epidemiol Rev. 1995;17:113–119. doi: 10.1093/oxfordjournals.epirev.a036166. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Community needs assessment of lower Manhattan residents following the World Trade Center attacks—Manhattan, New York City, 2001. Morb Mortal Wkly Rep. 2002;51(special issue):10–13. [PubMed] [Google Scholar]
- Committee on Comparative Effectiveness Research. Initial National Priorities for Comparative Effectiveness Research. Washington (DC): National Academy Press; 2009. [Google Scholar]
- Derogatis LR. Brief Symptom Inventory 18 (BSI-18) Manual. Minnetonka (MN): NCS Assessments; 2001. [Google Scholar]
- Donahue SA, Covell NH, Foster MJ, Felton CJ, Essock SM. Demographic characteristics of individuals who received Project Liberty crisis counseling services. Psychiatr Serv. 2006a;57:1261–1267. doi: 10.1176/ps.2006.57.9.1261. [DOI] [PubMed] [Google Scholar]
- Donahue SA, Lanzara CB, Felton CJ, Essock SM, Carpinello S. Project Liberty: New York’s crisis counseling program created in the aftermath of September 11, 2001. Psychiatr Serv. 2006b;57:1253–1258. doi: 10.1176/ps.2006.57.9.1253. [DOI] [PubMed] [Google Scholar]
- Felton CJ. Project liberty: A public health response to New Yorkers’ mental health needs arising from the World Trade Center terrorist attacks. J Urban Health. 2002;79:429–433. doi: 10.1093/jurban/79.3.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedy JR, Kilpatrick DG, Resnick HS. Natural disasters and mental health: Theory, assessment and intervention. J Soc Behav Pers. 1993;8:49–103. [Google Scholar]
- Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med. 2002;346:982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- Galea S, Boscarino JA, Resnick H, Vlahov D. Mental health in New York City after the September 11 terrorist attacks: Results from two population surveys. In: Manderscheid RW, Henderson MJ, editors. Mental Health, United States, 2001. Washington (DC): Government Printing Office; 2003. [Google Scholar]
- Gist R, Devilly GJ. Post-trauma debriefing: The road too frequently travelled. Lancet. 2002;360:741–742. doi: 10.1016/S0140-6736(02)09947-6. [DOI] [PubMed] [Google Scholar]
- Grobbee DE, Hoes AW. Confounding and indication for treatment in evaluation of drug treatment for hypertension. BMJ. 1997;315:1151–1154. doi: 10.1136/bmj.315.7116.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Survey Methodology. New York (NY): Wiley; 2004. [Google Scholar]
- Guo S, Fraser MW. Propensity Score Analysis: Statistical Methods and Applications. Los Angeles (CA): Sage Publications; 2010. [Google Scholar]
- Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB. Designing Clinical Research. 3rd ed. Philadelphia (PA), Baltimore (MD), New York, London, Buenos Aires (Argentina), Hong Kong (China), Sydney (Australia), Tokyo (Japan): Wolters Kluwer Health/Lippincott Williams & Wilkins; 2007. [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry. 1999;156:115–123. doi: 10.1176/ajp.156.1.115. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Freedy JR, Pelcovitz D, Resick P, Roth S, van der Kolk B. The posttraumatic stress disorder field trial: Evaluation of the PTSD construct— criteria A through E. In: Widiger T, Frances A, Pincus H, Ross R, First M, Davis W, editors. DSM-IV Sourcebook. Washington (DC): American Psychiatric Association Press; 1998. pp. 803–844. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence and comorbidity: Results from the National Survey of Adolescents. J Consul Clin Psychol. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- King M. At risk drinking among general practice attenders: Validation of the CAGE questionnaire. Psychol Med. 1986;16:213–217. doi: 10.1017/s0033291700002658. [DOI] [PubMed] [Google Scholar]
- Klungel OH, Martens EP, Psaty BM, Grobbee DE, Sullivan SD, Stricker BH, Leufkens HG, de Boer A. Methods to assess intended effects of drug treatment in observational studies are reviewed. J Clin Epidemiol. 2004;57:1223–1231. doi: 10.1016/j.jclinepi.2004.03.011. [DOI] [PubMed] [Google Scholar]
- Lavie P. Sleep disturbances in the wake of traumatic events. N Engl J Med. 2001;345:1825–1832. doi: 10.1056/NEJMra012893. [DOI] [PubMed] [Google Scholar]
- O’Brien CP. The CAGE questionnaire for detection of alcoholism: A remarkably useful but simple tool. JAMA. 2008;300:2054–2056. doi: 10.1001/jama.2008.570. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Systematic review and meta-analysis of multiple-session early interventions following traumatic events. Am J Psychiatry. 2009;166:293–301. doi: 10.1176/appi.ajp.2008.08040590. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Conceiving the Self. New York: Basic Books; 1979. [Google Scholar]
- Rosenheck R, Stolar M, Fontana A. Outcomes monitoring and the testing of new psychiatric treatments: Work therapy in the treatment of chronic post-traumatic stress disorder. Health Serv Res. 2000;35(1 pt 1):133–151. [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Matched Sampling for Causal Effects. New York: Cambridge University Press; 2006. [Google Scholar]
- Rubonis AV, Bickman L. Psychological impairment in the wake of disaster: The disaster-psychopathology relationship. Psychol Bull. 1991;109:384–399. doi: 10.1037/0033-2909.109.3.384. [DOI] [PubMed] [Google Scholar]
- Schiller D, Monfils MH, Raio CM, Johnson DC, Ledoux JE, Phelps EA. Preventing the return of fear in humans using reconsolidation update mechanisms. Nature. 2010;463:49–53. doi: 10.1038/nature08637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Smith DW, Christiansen EH, Vincent R, Hann NE. Population effects of the bombing of Oklahoma City. J Okla State Med Assoc. 1999;92:193–198. [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M. Structured Clinical Interview for DSM-III-R—Non-Patient Version. New York: New York State Psychiatric Institute; 1987. [Google Scholar]
- Stamm BH. Contextualizing death and trauma: A preliminary endeavor. In: Figley CR, editor. Death and Trauma. New York: Brunner/ Mazel; 1996. pp. 3–21. [Google Scholar]
- Stata Corporation. Stata Version 9.2. College Station (TX): Stata Publishing; 2007. [Google Scholar]
- van Emmerik AA, Kamphuis JH, Hulsbosch AM, Emmelkamp PM. Single session debriefing after psychological trauma: A meta-analysis. Lancet. 2002;360:766–771. doi: 10.1016/S0140-6736(02)09897-5. [DOI] [PubMed] [Google Scholar]