Abstract
Introduction
Several reports have shown marked heterogeneity of antibiotic pharmacokinetics (PK) in patients admitted to ICUs, which might potentially affect outcomes. Therefore, the pharmacodynamic (PD) parameter of the efficacy of β-lactam antibiotics, that is, the time that its concentration is above the bacteria minimal inhibitory concentration (T > MIC), cannot be safely extrapolated from data derived from the PK of healthy volunteers.
Methods
We performed a full review of published studies addressing the PK of intravenous β-lactam antibiotics given to infected ICU patients. Study selection comprised a comprehensive bibliographic search of the PubMed database and bibliographic references in relevant reviews from January 1966 to December 2010. We selected only English-language articles reporting studies addressing β-lactam antibiotics that had been described in at least five previously published studies. Studies of the PK of patients undergoing renal replacement therapy were excluded.
Results
A total of 57 studies addressing six different β-lactam antibiotics (meropenem, imipenem, piperacillin, cefpirome, cefepime and ceftazidime) were selected. Significant PK heterogeneity was noted, with a broad, more than twofold variation both of volume of distribution and of drug clearance (Cl). The correlation of antibiotic Cl with creatinine clearance was usually reported. Consequently, in ICU patients, β-lactam antibiotic half-life and T > MIC were virtually unpredictable, especially in those patients with normal renal function. A better PD profile was usually obtained by prolonged or even continuous infusion. Tissue penetration was also found to be compromised in critically ill patients with septic shock.
Conclusions
The PK of β-lactam antibiotics are heterogeneous and largely unpredictable in ICU patients. Consequently, the dosing of antibiotics should be supported by PK concepts, including data derived from studies of the PK of ICU patients and therapeutic drug monitoring.
Keywords: administration, dosage, β-lactam antibiotics, microdialysis, pharmacodynamics, pharmacokinetics, ICU
Introduction
Infection and sepsis, whether community- or hospital-acquired, are important causes of morbidity and mortality in ICU patients [1,2]. Despite all of the research, sepsis therapy continues to depend on supportive management of the different organ dysfunctions and failures and on specific therapy for infection with timely and appropriate antibiotics and/or focus control.
The β-lactam antibiotics, because of their large antimicrobial spectrum and low toxicity, are among the first-line therapies for critically ill patients, especially when a Gram-negative infection is suspected. However, the efficacy of antibiotics is not easily evaluated, since the clinical response is usually unnoticeable before 48 hours of therapy [3]. Moreover, the unavailability of routine therapeutic drug monitoring for the great majority of these drugs makes it difficult to distinguish clinical failure due to underdosing from lack of in vivo organism susceptibility.
Considerable evidence demonstrates that free drug time above bacteria minimal inhibitory concentration (f T > MIC) is the measure of drug exposure most closely linked to the ability of β-lactam antibiotics to kill the target bacteria [4]. T > MIC is dependent on the half-life (T1/2) of β-lactam antibiotics and their serum concentration.
The serum concentration of an antibiotic depends on the dose delivered, its bioavailability and its volume of distribution (Vd). Vd is a mathematical construct and refers to the size of a compartment necessary to account for the total amount of the drug, assuming that its concentration in the whole body is equal to that measured in plasma. Drugs that distribute essentially in the extracellular fluid (mainly hydrophilic) have low Vd, whilst drugs that have rapid cellular uptake (lipophilic) have high Vd[5,6].
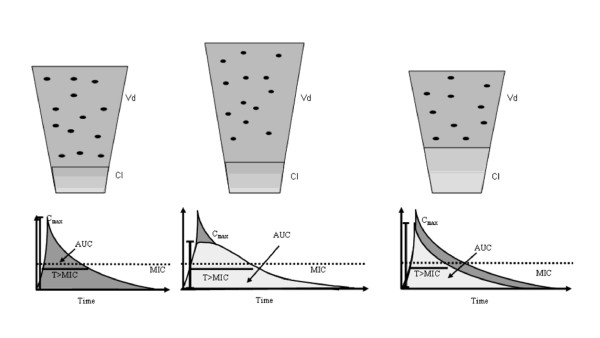
Both Vd and drug clearance (Cl) may be increased in ICU patients [7]. Therapeutic procedures, notably large-volume and blood products infusions, positive pressure ventilation, surgical procedures, capillary leak and reduction in albumin serum concentration all contribute to alter the concentration-time relationship of many drugs. A rise in the Vd, although it reduces drug concentration, might proportionally increase T1/2, since T1/2 = Vd/(Cl × 0.693) [7]. On the contrary, a high Cl may reduce the exposure of antibiotics to bacteria (Figure 1).
Figure 1.
ICU patients present pharmacokinetic changes of antibiotics that may alter bacterial exposure. Concentration-time curve of antibiotics in healthy volunteers (left panel). A large volume of distribution (Vd) (middle panel) is often present in ICU patients, leading to decreased maximum concentration (Cmax) but a longer half-life (T1/2) and eventually higher time that the antibiotic concentration is above the bacteria minimum inhibitory concentration (T > MIC). The antibiotic area under the concentration time curve (AUC) remains virtually the same. An increase in drug clearance (Cl) (right) is associated with decreases in AUC, T1/2 and T > MIC. Straight dotted lines-bacteria minimum inhibitory concentration.
Renal Cl may be increased in septic patients because of increased renal blood flow. This has recently been shown to be a common finding in ICU patients, particularly surgical and trauma patients [8] but also septic medical patients [9]. Besides, in the study by Baptista et al. [9], the authors showed that commonly used formulas used to calculate glomerular filtration rate usually underestimate creatinine (Cr) Cl. Consequently, these authors recommended direct Cr Cl measurement.
Moreover in ICU patients, maldistribution of blood flow in the microcirculation [10], namely, in patients in septic shock, may further decrease the drug concentration in the infected tissue [11]. These pharmacokinetic (PK) changes are sometimes influenced by the clinical course of the infection itself [12]. Consequently, PK parameters measured in healthy volunteers may not correctly predict concentrations in septic ICU patients, particularly early in the course of a severe infection [13,14].
Ideally, individualized dosing strategies should account for the altered PK and pathogen susceptibility in each patient. Despite the fact that some studies addressed this issue, this information had not yet been aggregated. Furthermore, β-lactam antibiotic PK are rarely analysed outside clinical trials. Therefore, we performed a systematic review of studies that addressed the PK parameters of β-lactam antibiotics in ICU patients to assess the relationship between dose and schedule of β-lactam antibiotics and their adequacy according to pharmacodynamic (PD) end points. We also reviewed studies assessing the concentrations of β-lactam antibiotics in different tissues. Our primary intention was to aggregate PK information in this particular population and to contribute to the design of individualized dosing regimens of these drugs.
We also included studies that involved the development of PD models using PK of ICU patients and bacterial MICs. These techniques allow the calculation of the presumed T > MIC and therefore the percentage of patients in which the antibiotic will achieve its PD target: that is, the antibiotic's probability of target attainment (PTA) [15,16]. The cumulative fraction of response (CFR) is calculated by multiplying the PTA obtained for each MIC by the MIC distribution according to a microbiological database [16].
Materials and methods
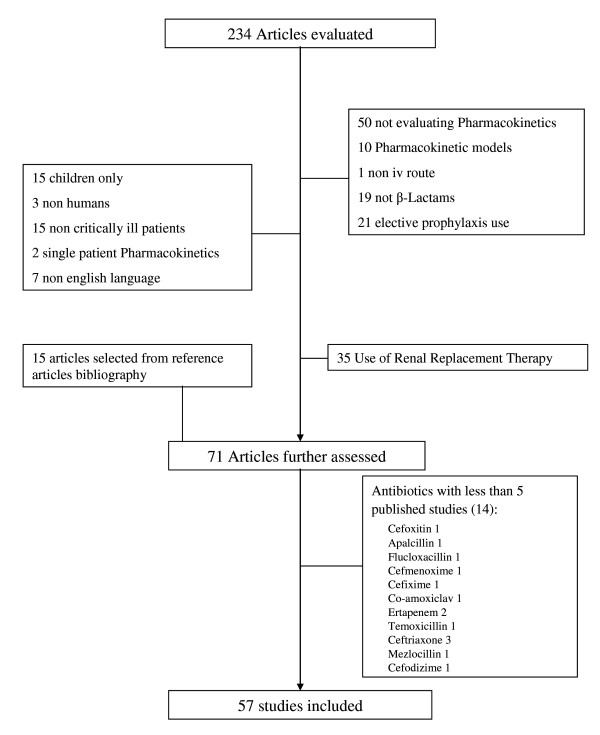
The data for this review were identified by a search of PubMed (January 1966 to December 2010) as well as bibliographic references from relevant articles, including reviews on this subject and all selected studies. The search terms used were 'antibiotic' or 'carbapenem' or 'penicillins' or 'cephalosporins', and 'intensive care' or 'critically ill' or 'critical care' or 'severe sepsis' or 'septic shock', and 'pharmacokinetics' or 'pharmacodynamics'. All relevant studies in the English-language literature that described antibiotic PK in critically ill patients were assessed (Figure 2).
Figure 2.
Flow diagram illustrating the selection of studies included in this review.
Only studies that described PK of antibiotics given intravenously to infected patients were selected. Studies referring to prophylactic antibiotics or to PK in patients under any type of renal replacement therapy were excluded. In fact, these studies are mainly directed to the measurement of Cl during renal replacement therapy to determine the ideal antibiotic dose and therefore are not easily compared with studies addressing the intrinsic PK of ICU patients. Furthermore, a full revision of those studies has recently been published [17].
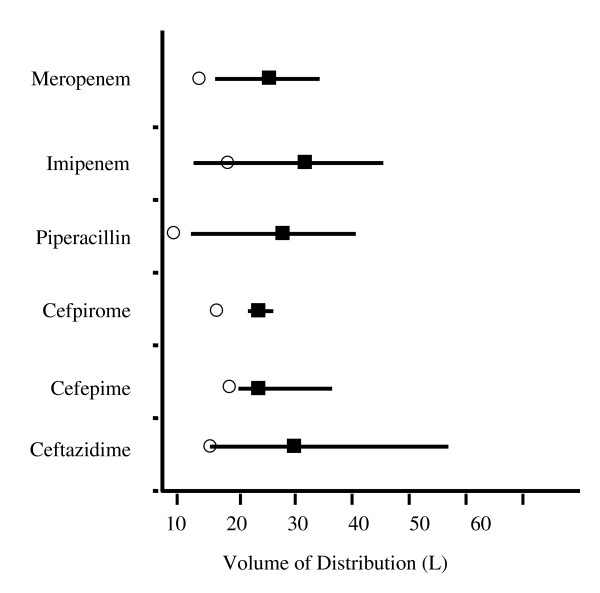
For the purpose of our systematic review, we analysed only studies of antibiotics with at least five published references. This threshold of five referenced studies was arbitrarily chosen so that we could derive more representative and consistent data on the PK of each antibiotic. The weighted mean of the Vd was calculated so that we could present a graphic representation of each analysed antibiotic (Figure 3).
Figure 3.
Heterogeneity of volume of distribution in litres of β-lactam antibiotics in ICU patients. Open circles: volume of distribution in healthy volunteers [44,51,89-92]; filled squares: weighted means of volume of distribution in the studies; straight lines: ranges of the means of volume of distribution in the studies.
Results
A total of 57 studies assessing an aggregate of six different β-lactam antibiotics were selected.
Carbapenem
Meropenem
Several studies have addressed meropenem PK in ICU septic patients. High Vd and Cl have usually been reported, as well as a low binding fraction: < 10% [18]. Consequently, a large heterogeneity of PK parameters was found, exceeding a twofold variation (Table 1 and Figure 3). The larger reported Vd, a mean of 34.4 L, was noted on the second day of therapy in eight ventilator-associated pneumonia (VAP) patients [19] with a mean body weight of 73 kg. In a Thai VAP population (N = 9) with a lower mean body weight (only 54.2 kg), the mean Vd was 6.0 L despite also being measured after 48 hours of therapy with meropenem [20]. This supports the hypothesis of a potential relationship between body weight and Vd.
Table 1.
Pharmacokinetic parameters of β-lactam antibioticsa
| PK parameters | Study | |||||
|---|---|---|---|---|---|---|
| Antibiotic drug classes and drugs | Vd, L | Cl, L/hour | T1/2, hours | Patient demographics | Study types [93] | References |
| Carbapenems | ||||||
| Meropenem | 21.2 ± 4.7b | 11.3 ± 4b | 1.4 ± 0.4b |
N = 11 Age 63.1 years [23 to 81] Mild to severe intraabdominal sepsis |
Descriptive | Lovering et al., 1995 [22] |
| Meropenem | 26.6 ± 3.2c | 9.4 ± 1.2c | 2.0 |
N = 15 Age 55.3 ± 14.3 years Severe sepsis |
Randomized, controlled cross-over | Thalhammer et al., 1999 [27] |
| Meropenem | 34.4 ± 15.9 | 11 ± 4.3 | 0.4 ± 0.12 |
N = 8 Age 55 ± 8 years VAP |
Descriptive | de Stoppelaar et al., 2000 [19] |
| Meropenem | 19.7 ± 5 | 7.3 ± 3.1 | 3.1 ± 1.5 |
N = 14 Age 73.3 ± 8.1 years Severe sepsis |
Descriptive | Kitzes-Cohen et al., 2002 [21] |
| Meropenem | 16.0 ± 3.7d | 8.5 ± 3.2d | 1.4 ± 0.6d |
N = 9 Age 39.6 ± 15.7 years VAP |
Not randomized, controlled cross-over | Jaruratanasirikul et al., 2005 [20] |
| Imipenem | Imipenem 17.7 ± 4 |
Imipenem 7.0 ± 2.5 |
Imipenem 2 ± 0.3 |
Imipenem N = 10 Age 65 ± 19 years |
Randomized, parallel controlled | Novelli et al., 2005 [29] |
| Meropenem | Meropenem 27.1 ± 7.7 |
Meropenem 11.5 ± 3.1 |
Meropenem 2.1 ± 0.5 |
Meropenem N = 10 Age 67 ± 19 years Severe sepsis |
||
| Meropenem | 23.8 ± 4.9 | 6.7 ± 4.2 | 3.7 ± 1.9 |
N = 6 Age 65.7 ± 11.2 years Peritonitis |
Descriptive | Karjagin et al., 2008 [25] |
| Meropenem | 22.7 | 13.6 ± 1.3 | NR |
N = 10 Age range 48 to 63 years Severe sepsis |
Randomized, parallel controlled | Roberts et al., 2009 [24] |
| Meropenem | Meropenem 30.1 [21.7 to 53.9]e |
Meropenem 8 [5 to 10.99e |
Meropenem 2.1 [1.7 to 3.4] |
Meropenem N = 16 |
Cross-sectional | Taccone et al., 2010 [23] |
| Piperacillin | Piperacillin 26.6 [20.3 to 30.1]e |
Piperacillin 8.4 [5.5 to 18.1]e |
Piperacillin 2.6 [1.5 to 3.8] |
Piperacillin N = 27 |
||
| Ceftazidime | Ceftazidime 33.6 [25.2 to 49.7]e |
Ceftazidime 3.8 [2.5 to 5.5]e |
Ceftazidime 5.8 [4.1 to 7.4] |
Ceftazidime N = 18 |
||
| Cefepime | Cefepime 25.2 [23.1 to 30.8]e |
Cefepime 5.5 [4.6 to 8.4]e |
Cefepime 3.4 [2.3 to 5.3] |
Cefepime N = 19 All patients: median age 63 years Severe sepsis or septic shock |
||
| Imipenem | 31.4 ± 11.7 | 14.4 ± 4.5 | 1.6 ± 1.3 |
N = 10 Age 44 ± 12.2 years Severe sepsis |
Descriptive | McKindley et al., 1996 [34] |
| Imipenem | 18.5 | 6.3 ± 0.8 | 2.0 |
N = 6 Age 63.5 ± 16.7 years Severe sepsis |
Not randomized, parallel, controlled | Tegeder et al., 2002 [32] |
| Imipenem | 45.5 ± 47.2 | 12.1 ± 12.0 | 2.9 ± 1.7 |
N = 50 Age 45.2 ± 17 years Presumed Gram-negative sepsis |
Cross-sectional | Belzberg et al., 2004 [28] |
| Imipenem | 12.2 ± 9.9f | 12.3 ± 4.2 | NR |
N = 20 Age 60.5 years VAP |
Randomized, parallel, controlled | Sakka et al., 2007 [31] |
| Imipenem | 27.2 ± 6.5 | 13.3 ± 5.2 | 1.4 ± 0.2 |
N = 6 Age 53.3 ± 19.9 years Severe sepsis |
Not randomized, parallel, controlled | Dahyot et al., 2008 [33] |
| Imipenem | 16.7 ± 5.3g | 8.7 ± 5.3g | 1.5 ± 0.7g |
N = 9 Age 63.3 ± 14.9 years VAP |
Not randomized, controlled, cross-over | Jaruratanasirikul and Sudsai, 2009 [30] |
| Penicillins | ||||||
| Piperacillin | 25.0 ± 17.2 | 23.8 ± 17.2 | 1.5 ± 2.1 |
N = 11 Age 43.6 ± 15.9 years Surgical patients |
Descriptive | Shikuma et al., 1990 [36] |
| Piperacillin | 19.5 ± 3.4b | 8.4 ± 1.4b | 1.8 ± 0.3b |
N = 10 Age 37.7 ± 2.8 years Burn patients |
Descriptive | Bourget et al., 1996 [38] |
| Piperacillin | 40.7 ± 8.7 | 8.2 ± 2 | 4.1 ± 1.3 |
N = 6 Age 64 ± 7 years Septic shock |
Not randomized, parallel, controlled | Joukhadar et al., 2001 [44] |
| Piperacillin | 34.6 ± 6.8c | 11.8 ± 4.3c | 2.4 ± 1.2c |
N = 7 Age range 45 to 76 years Severe sepsis |
Not randomized, controlled, cross-over | Langgartner et al., 2007 [39] |
| Piperacillin | 11.7f | 17.2 | 0.4 |
N = 13 Age 37.5 ± 19.4 years Severe sepsis |
Randomized, parallel, controlled | Roberts et al., 2009 [45] |
| Cephalosporins | ||||||
| Cefpirome | 23.6 ± 8.0 | 8.0 ± 3.0 | 2.2 ± 0.5 |
N = 9 Age 31 years [19 to 53] Severe sepsis |
Not randomized, parallel, controlled | Jacolot et al., 1999 [47] |
| Cefpirome | 26.4 ± 7.9 | 8.8 ± 3.4 | 3.1 ± 1.2 |
N = 12 Age 41.2 ± 19 years Severe sepsis |
Descriptive | Lipman et al., 2001 [48] |
| Cefpirome | 25.9 ± 7.1 | 4.5 ± 0.7 | 3.3 ± 0.5 |
N = 12 Age 67.2 ± 8.1 years Severe sepsis or septic shock |
Not randomized, parallel, controlled | Joukhadar et al., 2002 [52] |
| Cefpirome | 21.9 ± 4.5 | 4.8 ± 1.6 | 3.1 ± 0.9 |
N = 11 Age 66 ± 8 years Severe sepsis |
Not randomized, parallel, controlled | Sauermann et al., 2005 [51] |
| Cefepime | 32.6 ± 17.5 | 7.5 ± 3.1 | 3.5 ± 1.1 |
N = 7 Age 73.7 ± 4.9 years Severe sepsis |
Descriptive | Kieft et al., 1993 [53] |
| Cefepime | 21.8 ± 5.1 | 7.6 ± 2.0 | 3 ± 1.2 | N = 13 Age 55 years Severe sepsis |
Descriptive | Lipman et al., 1999 [56] |
| Cefepime | 36.1 ± 11.8 | 8.8 ± 2.4 | 2.8 ± 0.6 |
N = 12 Age 41 ± 13 years Burn patients |
Descriptive | Bonapace et al., 1999 [57] |
| Cefepime | 26.0b | 9.1 ± 1.5b | 2.5 ± 0.6b |
N = 6 Age 39.8 ± 11.3 years Burn patients |
Descriptive | Sampol et al., 2000 [61] |
| Cefepime | Cefepime 19.6 | Cefepime 7.1 ± 3.6 | Cefepime 2.9 ± 3.2 | Cefepime N = 13 Age 48.2 ± 21.2 years |
Cross-sectional | Conil et al., 2007 [54] |
| Ceftazidime | Ceftazidime 28.8 | Ceftazidime 7.5 ± 3.8 | Ceftazidime 3.1 ± 2.1 | Ceftazidime N = 17 Age 62.9 ± 22.4 years Burn patients |
||
| Cefepime | 28.7 ± 13.3d | 9.1 ± 5.6d | 4.3 ± 4.2 |
N = 21 Age 55.1 years (median) Nosocomial pneumonia |
Cross-sectional | Chapuis et al., 2010 [55] |
| Ceftazidime | 24.5 | 7.5 | 2.1 |
N = 16 Age range 18 to 70 years Pseudomonas infection |
Descriptive | Rondanelli et al., 1986 [64] |
| Ceftazidime | 49.3 ± 18.2e | 15.5 ± 2.5e | 1.8 ± 0.5e |
N = 5 Age 52.3 years [21 to 69] VAP |
Not randomized, controlled, cross-over | Langer et al., 1991 [76] |
| Ceftazidime | 29.5 ± 8.7 | 4.2 ± 1.9 | 6.1 ± 2.5 |
N = 12 Age 60 ± 13 years VAP |
Not randomized, controlled, cross-over | Bressolle et al., 1992 [77] |
| Ceftazidime | 18.9 ± 9c | 5.1c | 3.5 ± 1.6c |
N = 12 Age 57 ± 12 years Suspected Gram-negative sepsis |
Not randomized, controlled, cross-over | Benko et al., 1996 [67] |
| Ceftazidime | 15.0 ± 4.3 | 5.2 ± 2.2 | 1.3 ± 1.2 |
N = 10 Age 48 ± 15.1 years Severe sepsis |
Descriptive | Young et al., 1997 [65] |
| Ceftazidime | 56.9 ± 25.9 | 9.1 ± 4.8 | 4.8 ± 1.9 |
N = 15 Age 59.3 ± 14.6 years Severe sepsis |
Descriptive | Gómez et al., 1999 [66] |
| Ceftazidime | 22.9 [11.8 to 28.1] | 2.8 [0.2 to 7.8] | 7.7 [2 to 44.7] |
N = 21 Age range 27 to 73 years Melioidosis |
Not randomized, parallel, controlled | Angus et al., 2000 [71] |
| Ceftazidime | 25.6 ± 11.2c | 11.0 ± 5.3c | 1.7 ± 0.7c |
N = 14 Age 36.1 ± 12.8 years Gram-negative nosocomial pneumonia |
Not randomized, parallel, controlled | Hanes et al., 2000 [70] |
| Ceftazidime | 19.6 [14 to 28]c, e | 5.1 [2.3 to 8.9]c | 4.2 [1.3 to 12.3]c |
N = 6 Age 64 years [42 to 87] Surgical peritonitis |
Not randomized, parallel, controlled | Buijk et al., 2002 [74] |
aCl: clearance; NR: not reported; PK: pharmacokinetics; T1/2: half-life; VAP: ventilator-associated pneumonia; Vd: volume of distribution. bfirst-day PK; cPK after bolus dosing; dPK after 1-g bolus dosing; efor 70 kg; fcentral compartment; gPK after 500-mg bolus dosing. Except where otherwise indicated, data are means, means ± standard deviations or medians [interquartile ranges].
Meropenem Cl ranged from a mean of 4.7 L/hour to a mean of 15.4 L/hour and was generally found to be closely correlated to Cr Cl. In fact, in patients with severe sepsis, the six patients with the lower Cr Cl (< 50 mL/minute) had the higher T > MIC and area under the concentration time curve (AUC) (230.2 mg × hour/L vs. 119.4 mg × hour/L; P = 0.001), despite a reduction in the dose administered, from 1 g every 8 h (tid) to 1 g every 12 h (bid) [21].
One study addressed the variability of individual meropenem PK between the first and fourth days of therapy in 11 surgical patients [22]. Despite an increase in Cr Cl from a mean of 63.9 to 79.1 mL/minute during the study period, meropenem Vd, Cl and AUC remain unchanged. Nevertheless, in another study, by Taccone et al. [23], predefined targets were reached in only 75% of severe sepsis and septic shock patients after the first dose of 1 g of meropenem (Table 2), despite the inclusion of patients with acute renal failure (22%) who did not receive renal replacement therapy. These authors concluded that PK changes induced by sepsis were largely unpredictable and that none of the evaluated clinical parameters were predictive of PK adequacy: namely, age, severity, presence of shock, use of vasopressors and mechanical ventilation. Also, Roberts et al. [24] showed that the Vd in patients with severe sepsis had great variability, both in the same patient (especially the central compartment: roughly 45%) and in different patients (nearly 27%). In their study, despite the fact that all patients had a serum Cr < 1.36 mg/dL, the meropenem Cl variability (in the same patient and between patients) still ranged between 10% and 20%.
Table 2.
Pharmacodynamic targets of β-lactam antibioticsa
| Antibiotics | PD targets | Percentage of patients achieving targets | References |
|---|---|---|---|
| Meropenem, 1 g tid or 3 g/day CI | 40% f T > MIC, with f assumed to be 98%. CFR according to Mystic database |
PTA for MIC = 2 mg/L: bolus 100%, CI 100% | Roberts et al., 2009 [24] |
| PTA for MIC = 8 mg/L: bolus 70%, CI 100% | |||
| CFR for EC: bolus 100%, CI 100% | |||
| CFR for PA: bolus 40.6%, CI 100% | |||
| Ceftazidime, 2 g | 70% T > 4 × EUCAST breakpoint of PA | 28% | Taccone et al., 2010 [23] |
| Cefepime, 2 g | 70% T > 4 × EUCAST breakpoint of PA | 16% | |
| Meropenem, 1 g | 40% T > 4 × EUCAST breakpoint of PA | 75% | |
| Piperacillin/tazobactam, 4.5 g | 50% T > 4 × EUCAST breakpoint of PA | 44% | |
| Imipenem 1 g tid or 2 g/day CI | 40% f T > MIC, with f assumed to be 80% | MIC = 2 mg/L bolus dosing 88%, CI 100% | Sakka et al., 2007 [31] |
| MIC = 4 mg/L bolus 75%, CI 86% | |||
| Piperacillin/tazobactam 4.5 g qid or 13.5 g CI | 50% f T > MIC. CFR according to Mystic database |
PTA for MIC = 0.25 mg/L bolus 79.2%, CI 100% | Roberts et al., 2009 [46] |
| PTA for MIC = 1 mg/L bolus 60%, CI 100% | |||
| CFR for 18 g/day: bolus 53.4%, CI 92.5% | |||
| CFR for 13.5 g/day: bolus 40%, CI 92.4% | |||
| Cefpirome 2 g bid | 60% T > MIC | PTA for MIC = 4 mg/L: bolus 60%, CI (4 g/day) 100% | Lipman et al., 2001 [48] |
| PTA for MIC = 16 mg/L: bolus 10%, CI (4 g/day) 50% | |||
| Cefpirome 2 g tid | 60% T > MIC plasma and tissue | PTA for MIC = 4 mg/L: plasma 100%, tissue 100% | Sauermann et al., 2005 [51] |
| PTA for MIC = 16 mg/L: plasma 87.5%, tissue 75% | |||
| Cefpirome 2 g bid | 65% f T > MIC, with f assumed to be 90%. CFR according to EUCAST database |
CFR for EC: bolus 99.9%, CI (4 g/day) 100% | Roos et al., 2007 [50] |
| CFR for PA: bolus 56.1%, CI (4 g/day) 84.4% | |||
| Cefepime 2 g | 60% T > MIC MIC = 8 mg/L (NCCLS break point of PA) |
PTA with 1 g bid 45% PTA with 2 g bid 68% |
Bonapace et al., 1999 [57] |
| PTA for MIC = 4 mg/L: 1 g bid 68%, 2 g bid 89% | |||
| Cefepime 2 g | 65% f T > MIC, with f assumed to be 90%. CFR according to Queensland Health Pathology Service |
CFR for EC: 2 g bid 78.9%, CI (4 g/day) 96.9% | Roos et al., 2006 [60] |
| CFR for PA: 2 g bid 54%, CI (4 g/day) 91.7% | |||
| Ceftazidime 1 g every 4 hours | 100% T > 4 × MIC (isolated pathogens; if negative cultures 100% T > 16 mg/L) | Ceftazidime 47.8% PTA with 1 g every 3 hours 88.2% |
Conil et al., 2007 [54] |
| Cefepime 2 g tid | Cefepime 20% PTA with 1 g every 4 hours 88.2% |
||
| Cefepime 2 g tid | 50% f T > MIC, with f assumed to be 85% | PTA for MIC = 8 mg/L 91.8% | Nicasio et al., 2009 [59] |
| PTA for MIC = 32 mg/L 50.3% | |||
| Cefepime 2 g (each 12 to 36 hours) | 50% T > MIC MIC = 8 mg/L |
First dose 67%; steady-state 44% | Chapuis et al., 2010 [55] |
| Ceftazidime 2 g tid | 100% T > 5 × MIC MIC = 8 mg/L (PA break point) |
10% | Young et al., 1997 [65] |
| PTA for CI (6 g/day) 60% | |||
| Ceftazidime 2 g tid or 6 g/day CI | 100% T > 5 × MIC MIC = 8 mg/L (PA break point) |
Bolus 20% | Lipman et al., 1999 [68] |
| CI 100% | |||
| Ceftazidime 1.5 g tid or 4.5 g/day CI | T > 4 × MIC plasma and peritoneum (isolated pathogens) | Plasma: bolus dosing 100%, CI 100% | Buijk et al., 2002 [74] |
| Peritoneum: bolus 88%, CI 100% | |||
| Ceftazidime 2 to 6 g/day CI | 100% T > 5 × MIC MIC = 8 mg/L (PA break point) Target concentration 40 ± 10 mg/L |
35.9% | Aubert et al., 2010 [72] |
| Percentage of time on target (mean) | |||
| Meropenem 2 g tid or 3 g CI | T > MIC (isolated susceptible pathogens) | Bolus T = 100%; CI T = 100% | Thalhammer et al., 1999 [27] |
| Meropenem 1 g tid | T > MIC (isolated pathogens) | T = 90.8% | de Stoppelaar et al, 2000 [19] |
| T > 4 × MIC T = 52% | |||
| Meropenem 1 g bid or 1 g tid | T > MIC (isolated pathogens) | T = 80.9% (Cr Cl > 50 mL/minute; 1 g tid) | Kitzes-Cohen et al, 2002 [21] |
| T = 91.7% (Cr Cl < 50 mL/minute; 1 g bid) | |||
| Imipenem 1 g tid | T > MIC (isolated sensitive [MIC ≤ 2 mg/L] pathogens) | T = 100%; T > 4 × MIC T = 87.5% | Novelli et al., 2005 [29] |
| Meropenem 1 g tid | T > MIC (isolated sensitive [MIC ≤ 2 mg/L] pathogens) | T = 100%; T > 4 × MIC T = 87.5% | |
| Meropenem 1 g tid (bolus or 3-hour infusion) or 2 g tid (3-hour infusion) | T > MIC | For MIC = 1 mg/L: 1 g tid bolus T = 74.7%, 1 g tid 3 hours T = 93.6%, 2 g tid 3 hours T = 98.6%s | Jaruratanasirikul et al., 2005 [20] |
| For MIC = 16 mg/L: 1 g tid bolus T = 28.3%, 1 g tid 3 hours T = 37.8%, 2 g tid 3 hours T = 57.9% | |||
| Meropenem 1 g tid | T > MIC | For MIC = 4 mg/L: plasma T = 87%, peritoneum T = 87% | Karjagin et al., 2008 [25] |
| For MIC = 16 mg/L: plasma T = 55%, peritoneum T = 43% | |||
| Imipenem 500 mg qid (30 minutes or 2-hour infusion) or 1 g qid (2-hour infusion) | T > MIC | For MIC = 1 mg/L: 500 mg qid 30 minutes T = 64.7%, 500 mg qid 2 hours T = 76.5%, 1 g qid 2 hours T = 93.4% | Jaruratanasirikul and Sudsai, 2009 [30] |
| For MIC = 4 mg/L: 500 mg qid 30 minutes T = 20.3%, 500 mg qid 2 hours T = 17.7%, 1 g qid 2 hours T = 60.3% | |||
| Piperacillin 3 g qid or 8 g/day CI | T > MIC | For MIC = 16 mg/L: bolus dosing T = 62%, CI T = 100% | Rafati et al., 2006 [40] |
| For MIC = 32 mg/L: bolus T = 39%, CI T = 65% | |||
| Cefepime 2 g bid | T > MIC MIC = 7 mg/L (MIC90 of PA) |
T = 80% | Kieft et al., 1993 [53] |
| Ceftazidime 2 g tid or 3 g/day CI | T > MIC MIC = 4 mg/L (MIC of one isolated PA) |
Bolus T = 92%; CI T = 100% | Benko et al., 1996 [67] |
| Ceftazidime 2 g tid or 60 mg/kg/day CI | T > MIC (isolated pathogens) | Bolus T = 92.9%; CI T = 100% | Hanes et al., 2000 [70] |
aAB: Acinetobacter baumanii; bid: dose every 12 hours; CFR: cumulative fraction of response; CI: continuous infusion; Cr Cl: creatinine clearance; EC: Escherichia coli; EUCAST: European Committee on Antimicrobial Susceptibility Testing; f: free drug fraction; KP: Klebsiella pneumoniae; MIC: minimal inhibitory concentration; MIC90: 90th percentileof MIC in a bacteria population; NCCLS: National Committee for Clinical Laboratory Standards; PA: Pseudomonas aeruginosa; PD: pharmacodynamics; PTA: probability of target attainment; qid: dose every 6 hours; SA: Staphylococcus aureus; T > MIC: time that antibiotic concentration is above bacteria MIC; tid: dose every 8 hours.
The time of infusion of meropenem has also been shown to influence its T > MIC. In a cross-over study of nine Thai VAP patients [20], after 48 hours of therapy, 1 g of meropenem tid in 30-minute infusions provided an adequate T > MIC in 74.7% of the patients, for a MIC of 1 mg/L. However, with a MIC of 16 mg/L, only the meropenem regimen of 2 g tid given in an extended infusion (two hours) led to a T > MIC > 40% [20].
Meropenem tissue PK have been evaluated by microdialysis in several studies (Table 3). The tissue-to-plasma meropenem mean ratio on the first day of antibiotic therapy was found to be 0.74 in the peritoneum [25] and 0.44 in subcutaneous fat [24]. The meropenem CFR was calculated for the 10 patients for whom serum levels were measured in this study according to the Mystic microbiological database [26]. The CFRs were 100% for Enterobacteriaceae and 40.6% for Pseudomonas aeruginosa after bolus dosing, whilst with continuous infusion they were 100% for both bacteria, despite the use of a small daily dose (2 g/day) [27].
Table 3.
Tissue penetration of β-lactamsa
| Antibiotics | Samples | Patient demographics | Concentration ratiosb | References |
|---|---|---|---|---|
| Muscle and subcutaneous tissue | ||||
| Meropenem | Microdialysis in subcutaneous tissue | N = 10 severe sepsis, 5 continuous infusion | Bolus 0.44 Continuous infusion 0.57 (day 2) |
Roberts et al., 2009 [24] |
| Imipenem | Microdialysis in muscle and subcutaneous tissue |
N = 11 (6 patients) Severe sepsis |
Patients | Tegeder et al., 2002 [32] |
| • Muscle 0.1 | ||||
| • Subcutaneous 0.14 | ||||
| Volunteers | ||||
| • Muscle 0.5 | ||||
| • Subcutaneous 0.43 | ||||
| Imipenem | Microdialysis in muscle |
N = 12 (6 patients) Severe sepsis |
Patients 1 Volunteers 0.97 |
Dahyot et al., 2008 [33] |
| Piperacillin | Microdialysis in muscle and subcutaneous tissue |
N = 12 (6 patients) Septic shock |
Patients | Joukhadar et al., 2001 [44] |
| • Muscle 0.19 | ||||
| • Subcutaneous 0.1 | ||||
| Volunteers | ||||
| • Muscle 0.55 | ||||
| • Subcutaneous 0.31 | ||||
| Piperacillin | Microdialysis in subcutaneous tissue |
N = 13 Severe sepsis |
Bolus 0.21 Continuous infusion 0.2 |
Roberts et al., 2009 [45] |
| Cefpirome | Microdialysis in muscle |
N = 18 (12 patients) Severe sepsis or septic shock |
Patients 0.63 Volunteers 0.83 |
Joukhadar et al., 2002 [52] |
| Cefpirome | Microdialysis in subcutaneous tissue |
N = 18 (11 patients) Severe sepsis |
Patients 0.43 Volunteers 0.79 |
Sauermann et al., 2005 [51] |
| Burned skin | ||||
| Cefepime | Biopsy of burned area |
N = 6 Burn patients |
Day 3 1.52 (point concentration 3 to 5 hours after dose) | Sampol et al., 2000 [61] |
| Peritoneum | ||||
| Meropenem | Microdialysis in peritoneum |
N = 6 Surgical peritonitis |
0.74 | Karjagin et al., 2008 [25] |
| Ceftazidime | Peritoneal drainage |
N = 18 Surgical peritonitis |
Day 2 • Continuous infusion 0.56 |
Buijk et al., 2002 [74] |
| • Bolus 0.35 | ||||
| Imipenem | ELF (bronchoscopy) |
N = 8 Pneumonia |
0.20 (point concentration ratio 2 hours after dose) | Muller-Serieys et al., 1987 [35] |
| Imipenem | Bronchial secretions (tracheal aspirate) |
N = 10 Trauma patients with VAP |
NR | McKindley et al., 1996 [34] |
| Piperacillin | ELF (bronchoscopy) |
N = 10 VAP |
0.57 (point concentration ratio 5 hours after dose) | Boselli et al., 2004 [41] |
| Piperacillin | ELF (bronchoscopy) |
N = 40 VAP |
0.44 (point concentration ratio 4 hours after dose) | Boselli et al., 2008 [43] |
| Piperacillin | Bronchial secretions (tracheal aspirate) |
N = 8 VAP |
0.36 | Jehl et al., 1994 [42] |
| Cefepime | ELF (bronchoscopy) |
N = 20 VAP |
1.04 (point concentration ratio) | Boselli et al., 2003 [63] |
| Cefepime or ceftazidime | Bronchial secretions (tracheal aspirate) |
N = 5 cefepime VAP |
Cefepime < 0.02 | Klekner et al., 2006 [62] |
|
N = 4 ceftazidime VAP |
Ceftazidime < 0.05 | |||
| Ceftazidime | Bronchial secretions (tracheal aspirate) |
N = 5 Pneumonia |
0.12 | Langer et al., 1991 [76] |
| Ceftazidime | Bronchial secretions (tracheal aspirate) |
N = 12 Nosocomial pneumonia |
0.76 | Bressolle et al., 1992 [77] |
| Ceftazidime | ELF (bronchoscopy) |
N = 15 VAP |
0.21 (point concentration ratio at steady state) | Boselli et al., 2004 [69] |
aELF: epithelial lining fluid; NR: not reported. bMean area under the concentration time curve (AUC) tissue-to-plasma ratio unless otherwise stated.
Imipenem
In ICU patients, increased Vd and Cl of imipenem have also been reported (Table 1). Therefore, its T1/2 and T > MIC may be difficult to predict, depending on the relative changes of these two parameters. This difficulty was shown by Belzberg et al. [28] in a cohort of ICU surgical and trauma patients with presumed Gram-negative sepsis. In this relatively young population (mean age 45.2 ± 17 years and mean body weight 79.7 ± 17.7 kg), 44% of patients presented trough levels lower than the intended 4 mg/L at steady state. A mean Cr Cl of 103.8 mL/minute was found, but with large variability: two patients had renal failure and nineteen patients had a Cr Cl > 120 mL/minute. Nevertheless, no correlation was found between PK parameters and body weight, severity of disease, blood pressure or renal function [28].
Another study compared meropenem and imipenem first-dose PK in patients with normal renal function (serum Cr < 1.5 mg/dL). Again, both Vd and Cl were significantly elevated, although more so in the meropenem group [29]. However, their T > MIC for sensitive isolated pathogens were similar. Again, there was a relationship between Cr Cl and T1/2: Patients with a Cr Cl < 50 mL/minute had a significantly longer T1/2 for both antibiotics.
The PD efficacy of imipenem is also influenced by the dose and the time of infusion [30]. Using PK data from a cross-over steady-state study of VAP patients, Jaruratanasirikul and Sudsai [30] showed by modelling of imipenem PD that, for a MIC of 4 mg/L, a 500-mg dose delivered every 6 hours (qid) for 30 minutes achieved a T > MIC of 64.7% and increased to 76.5% with a 2-hour infusion. However, this study excluded shock and renal failure patients (Cr Cl < 60 mL/minute). With PD modelling of PK data derived from another 20 VAP patients [31], continuous infusion led to improved PTA despite the use of lower dosages (Table 2). In this latter study, all patients had f imipenem T > MIC of 100%, but three patients died.
Tissue microdialysis had been used to assess imipenem PK, but with very dissimilar results (Table 3): namely, the tissue-to-plasma ratio. This has been found to be markedly depressed in a cohort of severe critically ill patients compared to healthy volunteers (subcutaneous tissue-to-plasma 0.14 vs. 0.43 and muscle tissue-to-plasma 0.11 vs. 0.5, respectively) [32]. However, Dahyot et al. [33] disputed these results and found f imipenem in plasma and muscle to be virtually superimposed at any time, both in patients and in healthy volunteers. Some differences exist between these two studies. In the Tegeder et al. study [32], the patients had lower Cr Cl (medians 32.8 mL/minute vs. 156 mL/minute) and samples were collected at steady state and not after the first dose. Moreover, Dahyot et al. [33] accounted only for the f imipenem in plasma and found higher imipenem Vd and Cl. Different methods of calculating in vivo microdialysis recovery rates may also explain some of the diverse observed results. Nevertheless, low imipenem penetration ratios, as low as 0.06 [34,35], in bronchial secretions were reported in pneumonia patients (Table 3).
Penicillins
Piperacillin
Similarly to other β-lactams, piperacillin Vd and Cl have generally been found to be increased in ICU patients (Table 1). However, most studies have excluded renal failure patients.
Piperacillin Cl and trough concentrations were strongly related to Cr Cl [36-38]. Taccone et al. [23] showed that only 15% of patients with high Cr Cl (> 50 mL/minute) maintained piperacillin concentrations > 50% of T > 4 × MIC after the first antibiotic dose, as opposed to 71% of patients with lower Cr Cl (P = 0.03). In contrast, in 10 young burn patients (mean total burned area 40.8 ± 3.1%) with a mean Cr Cl of 119.8 mL/minute and Pseudomonas aeruginosa infection, the authors found a 20% increase in T1/2 after the first dose of antibiotic compared to the third day of therapy, which was related to a larger Vd (mean of 19.6 L vs. 16.4 L) [38]. Overall, the piperacillin AUC was similar in the two measurements (mean of 640 mg × hour/L vs. 622 mg × hour/L).
Piperacillin is stable for at least 24 hours at room temperature, making it a suitable choice for continuous infusion. With this strategy, higher steady-state concentrations are expected, theoretically providing a higher T > MIC even with the use of a lower daily dose [39]. A study by Rafati et al. [40] also supports this strategy. These authors showed that, for a MIC = 16 mg/L, the T > MIC was higher with continuous infusions (8 g/day) than with bolus dosing (3 g tid) (100% vs. 62%, respectively). However, the mortality rate was similar.
In VAP patients, piperacillin showed good penetration in bronchial secretions [41-43]. Nevertheless, its epithelial lining fluid (ELF) steady-state concentration was lower than the MIC for Pseudomonas aeruginosa after a 4.5-g tid dose [41]. With continuous infusion, an increase in pulmonary concentration was found, at least in the subset of patients with moderate renal failure (measured Cr Cl < 50 mL/minute), about three times higher than in the patients with normal renal function [43]. However, no relationship was found between ELF piperacillin concentration and clinical success. Similar concentrations were found in the eight patients who died or had persistent infections and in those who experienced therapeutic success [43].
Subcutaneous tissue-to-plasma ratio and PK have been assessed in microdialysis studies. In six septic shock patients (mean norepinephrine dose 0.8 μg/kg/minute) [44], the subcutaneous tissue-to-plasma AUC ratio was only 0.1, one-third of that measured in healthy volunteers. Peak tissue concentration was also delayed in patients (122 minutes in patients compared with 27 minutes in healthy volunteers), and T1/2 in tissues was nearly nine times longer. In 13 younger patients with less severe sepsis [45], the AUC tissue-to-plasma ratio was roughly 0.2. In accordance with their serum PK (as well as PK of another five patients) [46], piperacillin/tazobactam CFR was calculated to be 92.3% with continuous infusion (13.5 g/day) and 53.4% with bolus dosing (4.5 g qid, or 18 g/day). Again, no correlation was found between tissue concentration and outcomes. Despite the low tissue concentration levels, all patients in both groups survived [45].
Cephalosporins
Cefpirome
Cefpirome PK studies have produced heterogeneous results. A 2-g dose was adequate in young trauma patients (Cr Cl ≥ 50 mL/minute) and in similar healthy volunteers. After the first dose, the mean T > MIC were 75% and 80%, respectively (with a MIC of 4 mg/L, P = 0.76) [47]. However, in 12 similar patients, a lower T > MIC (60%) was found, which was probably related to higher cefpirome Cl [48]. After four days of therapy, the cefpirome mean PK parameters remained similar (T > MIC 67% and AUC 242 mg × hour/L vs. 306 mg × hour/L at steady state). Further analyses [49] showed a strong correlation between Cr Cl and either cefpirome or cefepime Cl (r2 = 0.81). Patients with the lower range of T > MIC had a higher Cr Cl, usually above 144 mL/minute [49]. According to these measured PK data, the authors performed a simulation to demonstrate improved CFR of cefpirome given as a continuous infusion to treat Pseudomonas aeruginosa infection, from 56.1% to 84.4% (Table 2) [50].
Cefpirome tissue PK were evaluated on the basis of microdialysis. Sauermann et al. [51] found a low subcutaneous tissue concentration in patients with severe sepsis, almost half of healthy volunteers, despite a longer plasma T1/2 (183 minutes vs. 95 minutes; P < 0.05). Similar results were reported by Joukhadar et al. [52], who found muscle-to-plasma ratios of 0.63 in patients and 0.83 in healthy volunteers (Table 3).
Cefepime
Roughly a twofold variation of cefepime Vd has been reported in PK studies (Table 1) of severe sepsis and septic shock patients [23], elderly septic patients [53], young burn patients [54] and nosocomial pneumonia patients [55]. Cefepime Cl has also been found to be closely correlated with Cr Cl in this last listed cohort (r2 = 0.77) [55], in another cohort of septic patients (r2 = 0.74) [56] and in burn patients (r2 = 0.58) [57]. Therefore, patients with renal dysfunction may experience toxicity.
In 21 septic patients receiving cefepime at a dose of 2 g bid, more than twofold peak variations and roughly 40-fold trough variations were observed. Again, the cefepime Cl correlated with Cr Cl (r2 = 0.77). Two patients with low Cr Cl (19 and 12 mL/minute) had trough levels > 20 mg/L despite dosage adjustment. They both had neurologic symptoms (namely, confusion and muscle jerks) that were not identified as toxicity but resolved promptly after drug arrest [55].
A cefepime bolus of 2 g bid was found to be insufficient to reach a high PD target after the first dose (Table 2), both in 80% of young burn patients (burn area 21.8%) with high mean Cr Cl (119.2 mL/minute) [54] and in the Taccone et al. study [23], in which only 16% of patients achieved the intended target.
Two other studies have evaluated cefepime PK, one of which addressed the first day of therapy for 55 nosocomial pneumonia or bacteraemia patients (67% trauma) [58] and the other of which described the status of 32 VAP patients on the second day of cefepime treatment [59]. Both studies unveiled a relationship between Vd and total body weight as well as between excretion, either elimination rate constant [59] or Cl [58], and Cr Cl. However, significant interpatient variability was again observed, with regard to both cefepime Cl (58%) and central compartment Vd (67%) [58].
A PD model was developed with this VAP population PK data: despite a 2-g tid dose, PTA > 90% was achieved only with a MIC ≤ 8 mg/L [59]. In another cefepime PD model, the CFR of a 2-g bid dose, used to treat both Escherichia coli and Klebsiella pneumoniae, was 78.9%. However, for Pseudomonas aeruginosa, CFR was only 53.6% (Table 2) and increased with either 2 g tid or continuous infusion (4 g/day or 6 g/day) to 84.9%, 91.7% and 94.8% respectively. Nevertheless, the CFR for Acinetobacter baumanii [60], even with a continuous infusion of 6 g/day, was only 75%, reemphasizing the importance of appropriate dosing and the potential benefit of continuous infusion against difficult-to-treat bacteria.
Also, the cefepime tissue concentration was assessed in biopsy samples collected from the skin of burn patients three to five hours after a bolus dose on day 3 of antibiotic therapy. A mean biopsy-to-plasma cefepime ratio of 1.5 (range 0.4 to 5.1) was found [61]. Klekner et al. [62] were unable to detect cefepime in bronchial secretions from any of the five studied patients six hours after an 80 mg/kg dose. However, using continuous infusion (4 g/day) to treat VAP patients, Boselli et al. [63] found, at steady state, higher and similar plasma and ELF concentrations (mean of 13.5 mg/L and 14.1 mg/L, respectively). Although different sampling methods may have influenced these differences, continuous infusion seems to prolong T > MIC in the lungs. Nevertheless, no correlation with therapeutic outcomes was reported.
Ceftazidime
Several studies have shown ceftazidime PK heterogeneity in ICU septic patients with Pseudomonas infections (mostly nosocomial pneumonia) [64], severe sepsis [65,66] and burns [54]. Similarly to other β-lactams, the authors noted a large variation of both Vd and Cl (Table 1) and consequently significant interpatient variability in T1/2 and trough concentrations. Also, a correlation between Cl and Cr Cl was usually reported [65,66].
Continuous infusion of ceftazidime was compared with bolus dosing in five different studies [67-71]. In all, there was an increase in T > MIC with continuous infusion despite lower daily doses. However, only in severe melioidosis was this strategy associated with lower mortality (3 of 10 patients vs. 9 of 11 patients) [71]. Those patients had low Cr Cl (26.6 mL/minute) and received ceftazidime dosages adjusted to their body weight (4 mg/kg/hour or 40 mg/kg tid, for a mean body weight of 49.4 kg). Ceftazidime steady-state concentration was measured in another cohort of 92 patients receiving continuous infusions [72]. Therapeutic drug monitoring was performed on the second day of therapy. The mean serum concentration was 46.9 mg/L, but again with a very wide range of serum concentrations (7.4 to 162.3 mg/L). Therefore, dosage modification was common because of low serum levels (36.9%) and high serum levels (27.2%), with the latter being associated with lower Cr Cl (mean of 51 mL/minute compared with 103 mL/minute for patients with low serum levels). Similar results were shown in another large ceftazidime PK study assessing a mixed septic population with a higher mean Cr Cl (123 mL/minute) [73]. The lower T > MIC was found in patients with the higher Cr Cl, especially after bolus dosing (Table 2).
Continuous infusion of ceftazidime (4.5 g/day) was also associated with a higher peritoneal AUC at day 2 compared to bolus dosing (1.5 g tid) in surgical patients with peritonitis (522 mg × hour/L vs. 316 mg × hour/L; P = 0.01) [74], despite similar serum AUC (and Cr Cl > 30 mL/minute). Therefore, although serum T > 4 × MIC was > 90% in all patients, peritoneal T > 4 × MIC was still > 90% with continuous infusion but only 44% with bolus dosing. Nevertheless, no difference in mortality was noted (25% vs. 33%; P = 1.0). A PD model of ceftazidime in ICU patients also showed higher PTA with continuous infusion (100% for MIC ≤ 8 mg/L) than with bolus dosing [75].
Ceftazidime concentration in bronchial secretions was measured in four studies of VAP patients. Very low concentrations, < 0.5 mg/L and < 0.3 mg/L, were found in two of them [62,76]. Bressole et al. [77] found a higher ratio between bronchial secretions and plasma concentration (0.76) in patients infected after abdominal surgery. A longer T1/2 (6.1 hours) and a lower Cl (4.2 L/hour) may explain some of these differences. With continuous infusion, a ratio of 0.21 between ELF and serum was observed [69].
Discussion
In our systematic review, we have aggregated information from 57 prospective studies related to the PK of β-lactam antibiotics, which are among the most often agents used to treat sepsis in ICU patients [78]. Overall, an increased Vd of all the studied antibiotics was reported (Figure 3), which was related to total body weight [58,73], but with significant variability. Drug Cl was also increased and usually related to Cr Cl. Those changes were largely unpredictable, with important interpatient variability. However, the higher Cl values were noted in studies that excluded patients with renal dysfunction, a common strategy, which may limit the interpretation of the data reported.
Therapeutic drug monitoring was rarely performed. In addition, data on the daily variation of PK parameters in ICU patients, as well as the ideal frequency of this monitoring, are currently limited. Nevertheless, two of the reviewed studies [55,72] showed that inadequate dosing may be common in this population and may jeopardize β-lactam antibiotics efficacy or even lead to toxicity [79]. Roberts et al. [80] measured piperacillin/tazobactam concentrations and found that 50.4% of patients first measurement were low. The clinical efficacy of using drug levels to achieve adequate concentrations had never been properly evaluated. In a recent study, PD modelling was used to empirically treat 94 VAP in critically ill patients at high risk of infection with antibiotic-resistant Pseudomonas aeruginosa [81]. A three-hour infusion regimen of either cefepime or meropenem at a high dosage (2 g tid) was initiated, followed by both antibiotic and dose de-escalation whenever bacteria with a low MIC were identified. The infection-related mortality decreased from 21.6% to 8.5% (P = 0.029).
The PD targets of β-lactam antibiotics may be different in patients with severe bacterial infections. McKinnon et al. [82] evaluated ceftazidime and cefepime PD by using PK data from previous clinical trials [83]. Maintaining a T > MIC as high as 100% was associated with a significantly greater clinical cure and bacteriologic eradication than a shorter time (cefatzidime: 82% vs. 33%, P = 0.002; cefepime: 97% vs. 44%, P = 0.001). Also, in a febrile neutropenia population of 60 patients treated with meropenem, a calculated T > MIC of 83% was found in responders, whilst those with a poor clinical response had a T > MIC of only 60% [84]. It has also been suggested that, at least in vivo, maximum killing of bacteria is achieved at higher concentrations, four to five times MIC [85], accounting for antibiotic penetration in infected tissues. As such, concentrations of β-lactam antibiotics may need to be maintained well above the MIC for extended periods, especially in patients with life-threatening infections. Accordingly, different PD targets have been proposed in the different studies addressing ICU patients, which sometimes make their comparison difficult.
An improved PD profile of β-lactams may be obtained by promoting a longer exposure with more frequent dosing, extended infusions or continuous infusions [86,87]. Several of the studies that we reviewed reported PD benefits of continuous infusions (even using small daily doses) (Table 2). Also, PD modelling tends to support this strategy. Nevertheless, almost none of the studies addressed reported a decrease in mortality. In addition, a recently published meta-analysis of 14 prospective studies did not show a significant benefit of using this strategy (odds ratio 1.00, 95% confidence interval 0.48 to 2.06; P = 1.00) [88].
An increasing number of studies have addressed β-lactam antibiotic tissue concentration. Despite the theoretical advantage of analysing the drug concentration at the site of infection, there are no data to support a relationship between these concentrations and outcomes. Furthermore, there are still controversial issues involved in interpreting these data, namely, microdialysis [32,33]. Therefore, we think that, at present, no recommendation can be made regarding antibiotic tissue PK.
Conclusions
The PK of β-lactam antibiotics are significantly changed in septic ICU patients. Dosage and schedule regimens based on data from healthy volunteers may be misleading. Therapeutic drug monitoring and PD modelling according to measured PK previously showed promising results. Continuous infusion, although theoretically useful, has not been shown to lead to improved outcomes. The clinical significance of tissue PK monitoring remains to be determined.
Key messages
• Among ICU patients, the PK of β-lactam antibiotics are markedly unpredictable.
• A large volume of distribution is commonly observed in ICU patients and contributes to a lower antibiotic concentration, but also to a greater exposure time.
• An increased glomerular filtration rate is usually associated with a short half-life of β-lactam antibiotics, whilst renal failure is associated with a greater exposure and increased risk of accumulation.
• Continuous infusion of β-lactam antibiotics commonly increases the time that the antibiotic concentration exceeds its MIC and may therefore increase efficacy.
• Therapeutic drug monitoring of β-lactam antibiotic concentration may help to improve its efficacy and prevent toxicity, but currently is unavailable in most clinical settings.
Abbreviations
AUC: area under the concentration time curve; bid: dose every 12 hours; CFR: cumulative fraction of response; Cl: drug clearance; Cr Cl: creatinine clearance; ELF: epithelial lining fluid; f: free drug fraction; Kel: elimination rate constant; MIC: minimum inhibitory concentration; MIC90: 90th percentile of MIC in a bacteria population; PD: pharmacodynamics; PK: pharmacokinetics; PTA: probability of target attainment; qid: dose every six hours; T1/2: half-life; tid: dose every eight hours; T > MIC: antibiotic concentration time over bacteria MIC; VAP: ventilator-associated pneumonia; Vd: volume of distribution.
Competing interests
JGP has received honoraria from and served as an advisor for Pfizer, AstraZeneca, Gilead Sciences Inc., Abbott Laboratories, Wyeth Lederle, Janssen-Cilag and Merck Sharp & Dohme Corp. JGP also has received an unrestricted research grant from AstraZeneca. PP has received honoraria from and served as an advisor for AstraZeneca, Ely Lilly and Co., Gilead Sciences Inc., Janssen-Cilag, Merck Sharp & Dohme Corp., Novartis and Pfizer Inc.
Authors' contributions
Both JGP and PP searched the literature, analysed the data and wrote the manuscript. Both authors read and approved the final manuscript for publication.
Contributor Information
Joao Gonçalves-Pereira, Email: joaogpster@gmail.com.
Pedro Póvoa, Email: povoap@netcabo.pt.
References
- Brun-Buisson C. The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000;26(Suppl 1):S64–S74. doi: 10.1007/s001340051121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y. EPIC II Group of Investigators. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302:2323–2329. doi: 10.1001/jama.2009.1754. [DOI] [PubMed] [Google Scholar]
- Póvoa P. Serum markers in community-acquired pneumonia and ventilator-associated pneumonia. Curr Opin Infect Dis. 2008;21:157–162. doi: 10.1097/QCO.0b013e3282f47c32. [DOI] [PubMed] [Google Scholar]
- Craig WA. Basic pharmacodynamics of antibacterials with clinical applications to the use of β-lactams, glycopeptides, and linezolid. Infect Dis Clin North Am. 2003;17:479–501. doi: 10.1016/S0891-5520(03)00065-5. [DOI] [PubMed] [Google Scholar]
- Estes L. Review of pharmacokinetics and pharmacodynamics of antimicrobial agents. Mayo Clin Proc. 1998;73:1114–1122. doi: 10.4065/73.11.1114. [DOI] [PubMed] [Google Scholar]
- Pea F, Viale P, Furlanut M. Antimicrobial therapy in critically ill patients: a review of pathophysiological conditions responsible for altered disposition and pharmacokinetic variability. Clin Pharmacokinet. 2005;44:1009–1034. doi: 10.2165/00003088-200544100-00002. [DOI] [PubMed] [Google Scholar]
- Mehrotra R, De Gaudio R, Palazzo M. Antibiotic pharmacokinetic and pharmacodynamic considerations in critical illness. Intensive Care Med. 2004;30:2145–2156. doi: 10.1007/s00134-004-2428-9. [DOI] [PubMed] [Google Scholar]
- Fuster-Lluch O, Gerónimo-Pardo M, Peyró-García R, Lizán-García M. Glomerular hyperfiltration and albuminuria in critically ill patients. Anaesth Intensive Care. 2008;36:674–680. doi: 10.1177/0310057X0803600507. [DOI] [PubMed] [Google Scholar]
- Baptista JP, Udy AA, Sousa E, Pimentel J, Wang L, Roberts JA, Lipman J. A comparison of estimates of glomerular filtration in critically ill patients with augmented renal clearance. Crit Care. 2011;15:R139. doi: 10.1186/cc10262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdant C, De Backer D. How monitoring of the microcirculation may help us at the bedside. Curr Opin Crit Care. 2005;11:240–244. doi: 10.1097/01.ccx.0000158849.94225.11. [DOI] [PubMed] [Google Scholar]
- Levitt DG. The pharmacokinetics of the interstitial space in humans. BMC Clin Pharmacol. 2003;3:3. doi: 10.1186/1472-6904-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Triginer C, Izquierdo I, Fernandez R, Rello J, Torrent J, Benito S, Net A. Gentamicin volume of distribution in critically ill septic patients. Intensive Care Med. 1990;16:303–306. doi: 10.1007/BF01706354. [DOI] [PubMed] [Google Scholar]
- Hansen M, Christrup LL, Jarløv JO, Kampmann JP, Bonde J. Gentamicin dosing in critically ill patients. Acta Anaesthesiol Scand. 2001;45:734–740. doi: 10.1034/j.1399-6576.2001.045006734.x. [DOI] [PubMed] [Google Scholar]
- Roberts JA, Lipman J. Antibacterial dosing in intensive care: pharmacokinetics, degree of disease and pharmacodynamics of sepsis. Clin Pharmacokinet. 2006;45:755–773. doi: 10.2165/00003088-200645080-00001. [DOI] [PubMed] [Google Scholar]
- Drusano GL. Pharmacokinetics and pharmacodynamics of antimicrobials. Clin Infect Dis. 2007;45(Suppl 1):S89–S95. doi: 10.1086/518137. [DOI] [PubMed] [Google Scholar]
- Mouton JW. Impact of pharmacodynamics on breakpoint selection for susceptibility testing. Infect Dis Clin North Am. 2003;17:579–598. doi: 10.1016/S0891-5520(03)00062-X. [DOI] [PubMed] [Google Scholar]
- Choi G, Gomersall CD, Tian Q, Joynt GM, Li AM, Lipman J. Principles of antibacterial dosing in continuous renal replacement therapy. Blood Purif. 2010;30:195–212. doi: 10.1159/000321488. [DOI] [PubMed] [Google Scholar]
- Shah PM. Parenteral carbapenems. Clin Microbiol Infect. 2008;14:175–180. doi: 10.1111/j.1469-0691.2007.01868.x. [DOI] [PubMed] [Google Scholar]
- de Stoppelaar F, Stolk L, van Tiel F, Beysens A, van der Geest S, de Leeuw P. Meropenem pharmacokinetics and pharmacodynamics in patients with ventilator-associated pneumonia. J Antimicrob Chemother. 2000;46:150–151. doi: 10.1093/jac/46.1.150. [DOI] [PubMed] [Google Scholar]
- Jaruratanasirikul S, Sriwiriyajan S, Punyo J. Comparison of the pharmacodynamics of meropenem in patients with ventilator-associated pneumonia following administration by 3-hour infusion or bolus injection. Antimicrob Agents Chemother. 2005;49:1337–1339. doi: 10.1128/AAC.49.4.1337-1339.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzes-Cohen R, Farin D, Piva G, De Myttenaere-Bursztein SA. Pharmacokinetics and pharmacodynamics of meropenem in critically ill patients. Int J Antimicrob Agents. 2002;19:105–110. doi: 10.1016/S0924-8579(01)00474-5. [DOI] [PubMed] [Google Scholar]
- Lovering AM, Vickery CJ, Watkin DS, Leaper D, McMullin CM, White LO, Reeves DS, MacGowan AP. The pharmacokinetics of meropenem in surgical patients with moderate or severe infections. J Antimicrob Chemother. 1995;36:165–172. doi: 10.1093/jac/36.1.165. [DOI] [PubMed] [Google Scholar]
- Taccone FS, Laterre PF, Dugernier T, Spapen H, Delattre I, Witebolle X, De Backer D, Layeux B, Wallemacq P, Vincent JL, Jacobs F. Insufficient β-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care. 2010;14:R126. doi: 10.1186/cc9091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JA, Kirkpatrick CM, Roberts MS, Robertson TA, Dalley AJ, Lipman J. Meropenem dosing in critically ill patients with sepsis and without renal dysfunction: intermittent bolus versus continuous administration? Monte Carlo dosing simulations and subcutaneous tissue distribution. J Antimicrob Chemother. 2009;64:142–150. doi: 10.1093/jac/dkp139. [DOI] [PubMed] [Google Scholar]
- Karjagin J, Lefeuvre S, Oselin K, Kipper K, Marchand S, Tikkerberi A, Starkopf J, Couet W, Sawchuk RJ. Pharmacokinetics of meropenem determined by microdialysis in the peritoneal fluid of patients with severe peritonitis associated with septic shock. Clin Pharmacol Ther. 2008;83:452–459. doi: 10.1038/sj.clpt.6100312. [DOI] [PubMed] [Google Scholar]
- Rhomberg PR, Jones RN. Contemporary activity of meropenem and comparator broad-spectrum agents: MYSTIC program report from the United States component (2005) Diagn Microbiol Infect Dis. 2007;57:207–215. doi: 10.1016/j.diagmicrobio.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Thalhammer F, Traunmüller F, El Menyawi I, Frass M, Hollenstein UM, Locker GJ, Stoiser B, Staudinger T, Thalhammer-Scherrer R, Burgmann H. Continuous infusion versus intermittent administration of meropenem in critically ill patients. J Antimicrob Chemother. 1999;43:523–527. doi: 10.1093/jac/43.4.523. [DOI] [PubMed] [Google Scholar]
- Belzberg H, Zhu J, Cornwell EE, Murray JA, Sava J, Salim A, Velmahos GC, Gill MA. Imipenem levels are not predictable in the critically ill patient. J Trauma. 2004;56:111–117. doi: 10.1097/01.TA.0000056164.26493.28. [DOI] [PubMed] [Google Scholar]
- Novelli A, Adembri C, Livi P, Fallani S, Mazzei T, De Gaudio AR. Pharmacokinetic evaluation of meropenem and imipenem in critically ill patients with sepsis. Clin Pharmacokinet. 2005;44:539–549. doi: 10.2165/00003088-200544050-00007. [DOI] [PubMed] [Google Scholar]
- Jaruratanasirikul S, Sudsai T. Comparison of the pharmacodynamics of imipenem in patients with ventilator-associated pneumonia following administration by 2 or 0.5 h infusion. J Antimicrob Chemother. 2009;63:560–563. doi: 10.1093/jac/dkn543. [DOI] [PubMed] [Google Scholar]
- Sakka SG, Glauner AK, Bulitta JB, Kinzig-Schippers M, Pfister W, Drusano GL, Sörgel F. Population pharmacokinetics and pharmacodynamics of continuous versus short-term infusion of imipenem-cilastatin in critically ill patients in a randomized, controlled trial. Antimicrob Agents Chemother. 2007;51:3304–3310. doi: 10.1128/AAC.01318-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tegeder I, Schmidtko A, Bräutigam L, Kirschbaum A, Geisslinger G, Lötsch J. Tissue distribution of imipenem in critically ill patients. Clin Pharmacol Ther. 2002;71:325–333. doi: 10.1067/mcp.2002.122526. [DOI] [PubMed] [Google Scholar]
- Dahyot C, Marchand S, Bodin M, Debeane B, Mimoz O, Couet W. Application of basic pharmacokinetic concepts to analysis of microdialysis data: illustration with imipenem muscle distribution. Clin Pharmacokinet. 2008;47:181–189. doi: 10.2165/00003088-200847030-00004. [DOI] [PubMed] [Google Scholar]
- McKindley DS, Boucher BA, Hess MM, Croce MA, Fabian TC. Pharmacokinetics of aztreonam and imipenem in critically ill patients with pneumonia. Pharmacotherapy. 1996;16:924–931. [PubMed] [Google Scholar]
- Muller-Serieys C, Bergogne-Berezin E, Rowan C, Dombret MC. Imipenem penetration into bronchial secretions. J Antimicrob Chemother. 1987;20:618–619. doi: 10.1093/jac/20.4.618. [DOI] [PubMed] [Google Scholar]
- Shikuma LR, Ackerman BH, Weaver RH, Solem LD, Strate RG, Cerra FB, Zaske DE. Effects of treatment and the metabolic response to injury on drug clearance: a prospective study with piperacillin. Crit Care Med. 1990;18:37–41. doi: 10.1097/00003246-199001000-00010. [DOI] [PubMed] [Google Scholar]
- Conil JM, Georges B, Mimoz O, Dieye E, Ruiz S, Cougot P, Samii K, Houin G, Saivin S. Influence of renal function on trough serum concentrations of piperacillin in intensive care unit patients. Intensive Care Med. 2006;32:2063–2066. doi: 10.1007/s00134-006-0421-1. [DOI] [PubMed] [Google Scholar]
- Bourget P, Lesne-Hulin A, Le Reveillé R, Le Bever H, Carsin H. Clinical pharmacokinetics of piperacillin-tazobactam combination in patients with major burns and signs of infection. Antimicrob Agents Chemother. 1996;40:139–145. doi: 10.1128/aac.40.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langgartner J, Lehn N, Glück T, Herzig H, Kees F. Comparison of the pharmacokinetics of piperacillin and sulbactam during intermittent and continuous intravenous infusion. Chemotherapy. 2007;53:370–377. doi: 10.1159/000107725. [DOI] [PubMed] [Google Scholar]
- Rafati MR, Rouini MR, Mojtahedzadeh M, Najafi A, Tavakoli H, Gholami K, Fazeli MR. Clinical efficacy of continuous infusion of piperacillin compared with intermittent dosing in septic critically ill patients. Int J Antimicrob Agents. 2006;28:122–127. doi: 10.1016/j.ijantimicag.2006.02.020. [DOI] [PubMed] [Google Scholar]
- Boselli E, Breilh D, Cannesson M, Xuereb F, Rimmelé T, Chassard D, Saux MC, Allaouchiche B. Steady-state plasma and intrapulmonary concentrations of piperacillin/tazobactam 4 g/0.5 g administered to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004;30:976–979. doi: 10.1007/s00134-004-2222-8. [DOI] [PubMed] [Google Scholar]
- Jehl F, Muller-Serieys C, de Larminat V, Monteil H, Bergogne-Berezin E. Penetration of piperacillin-tazobactam into bronchial secretions after multiple doses to intensive care patients. Antimicrob Agents Chemother. 1994;38:2780–2784. doi: 10.1128/aac.38.12.2780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boselli E, Breilh D, Rimmelé T, Guillaume C, Xuereb F, Saux MC, Bouvet L, Chassard D, Allaouchiche B. Alveolar concentrations of piperacillin/tazobactam administered in continuous infusion to patients with ventilator-associated pneumonia. Crit Care Med. 2008;36:1500–1506. doi: 10.1097/CCM.0b013e318170ba21. [DOI] [PubMed] [Google Scholar]
- Joukhadar C, Frossard M, Mayer BX, Brunner M, Klein N, Siostrzonek P, Eichler HG, Müller M. Impaired target site penetration of β-lactams may account for therapeutic failure in patients with septic shock. Crit Care Med. 2001;29:385–391. doi: 10.1097/00003246-200102000-00030. [DOI] [PubMed] [Google Scholar]
- Roberts JA, Roberts MS, Robertson TA, Dalley AJ, Lipman J. Piperacillin penetration into tissue of critically ill patients with sepsis: bolus versus continuous administration? Crit Care Med. 2009;37:926–933. doi: 10.1097/CCM.0b013e3181968e44. [DOI] [PubMed] [Google Scholar]
- Roberts JA, Kirkpatrick CM, Roberts MS, Dalley AJ, Lipman J. First-dose and steady-state population pharmacokinetics and pharmacodynamics of piperacillin by continuous or intermittent dosing in critically ill patients with sepsis. Int J Antimicrob Agents. 2009;35:156–163. doi: 10.1016/j.ijantimicag.2009.10.008. [DOI] [PubMed] [Google Scholar]
- Jacolot A, Incagnoli P, Edouard AR, Tod M, Petitjean O, Samii K, Mimoz O. Pharmacokinetics of cefpirome during the posttraumatic systemic inflammatory response syndrome. Intensive Care Med. 1999;25:486–491. doi: 10.1007/s001340050885. [DOI] [PubMed] [Google Scholar]
- Lipman J, Wallis SC, Rickard CM, Fraenkel D. Low cefpirome levels during twice daily dosing in critically ill septic patients: pharmacokinetic modelling calls for more frequent dosing. Intensive Care Med. 2001;27:363–370. doi: 10.1007/s001340000741. [DOI] [PubMed] [Google Scholar]
- Lipman J, Wallis SC, Boots RJ. Cefepime versus cefpirome: the importance of creatinine clearance. Anesth Analg. 2003;97:1149–1154. doi: 10.1213/01.ANE.0000077077.54084.B0. [DOI] [PubMed] [Google Scholar]
- Roos JF, Lipman J, Kirkpatrick CM. Population pharmacokinetics and pharmacodynamics of cefpirome in critically ill patients against Gram-negative bacteria. Intensive Care Med. 2007;33:781–788. doi: 10.1007/s00134-007-0573-7. [DOI] [PubMed] [Google Scholar]
- Sauermann R, Delle-Karth G, Marsik C, Steiner I, Zeitlinger M, Mayer-Helm BX, Georgopoulos A, Müller M, Joukhadar C. Pharmacokinetics and pharmacodynamics of cefpirome in subcutaneous adipose tissue of septic patients. Antimicrob Agents Chemother. 2005;49:650–655. doi: 10.1128/AAC.49.2.650-655.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joukhadar C, Klein N, Mayer BX, Kreischitz N, Delle-Karth G, Palkovits P, Heinz G, Müller M. Plasma and tissue pharmacokinetics of cefpirome in patients with sepsis. Crit Care Med. 2002;30:1478–1482. doi: 10.1097/00003246-200207000-00013. [DOI] [PubMed] [Google Scholar]
- Kieft H, Hoepelman AI, Knupp CA, van Dijk A, Branger JM, Struyvenberg A, Verhoef J. Pharmacokinetics of cefepime in patients with the sepsis syndrome. J Antimicrob Chemother. 1993;32(Suppl B):117–122. doi: 10.1093/jac/32.suppl_b.117. [DOI] [PubMed] [Google Scholar]
- Conil JM, Georges B, Lavit M, Seguin T, Tack I, Samii K, Chabanon G, Houin G, Saivin S. Pharmacokinetics of ceftazidime and cefepime in burn patients: the importance of age and creatinine clearance. Int J Clin Pharmacol Ther. 2007;45:529–538. doi: 10.5414/cpp45529. [DOI] [PubMed] [Google Scholar]
- Chapuis TM, Giannoni E, Majcherczyk PA, Chioléro R, Schaller MD, Berger MM, Bolay S, Décosterd LA, Bugnon D, Moreillon P. Prospective monitoring of cefepime in intensive care unit adult patients. Crit Care. 2010;14:R51. doi: 10.1186/cc8941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipman J, Wallis SC, Rickard C. Low plasma cefepime levels in critically ill septic patients: pharmacokinetic modeling indicates improved troughs with revised dosing. Antimicrob Agents Chemother. 1999;43:2559–2561. doi: 10.1128/aac.43.10.2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonapace CR, White RL, Friedrich LV, Norcross ED, Bosso JA. Pharmacokinetics of cefepime in patients with thermal burn injury. Antimicrob Agents Chemother. 1999;43:2848–2854. doi: 10.1128/aac.43.12.2848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georges B, Conil JM, Seguin T, Dieye E, Cougot P, Decun JF, Lavit M, Samii K, Houin G, Saivin S. Cefepime in intensive care unit patients: validation of a population pharmacokinetic approach and influence of covariables. Int J Clin Pharmacol Ther. 2008;46:157–164. doi: 10.5414/cpp46157. [DOI] [PubMed] [Google Scholar]
- Nicasio AM, Ariano RE, Zelenitsky SA, Kim A, Crandon JL, Kuti JL, Nicolau DP. Population pharmacokinetics of high-dose, prolonged-infusion cefepime in adult critically ill patients with ventilator-associated pneumonia. Antimicrob Agents Chemother. 2009;53:1476–1481. doi: 10.1128/AAC.01141-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos JF, Bulitta J, Lipman J, Kirkpatrick CM. Pharmacokinetic-pharmacodynamic rationale for cefepime dosing regimens in intensive care units. J Antimicrob Chemother. 2006;58:987–993. doi: 10.1093/jac/dkl349. [DOI] [PubMed] [Google Scholar]
- Sampol E, Jacquet A, Viggiano M, Bernini V, Manelli JC, Lacarelle B, Durand A. Plasma, urine and skin pharmacokinetics of cefepime in burns patients. J Antimicrob Chemother. 2000;46:315–317. doi: 10.1093/jac/46.2.315. [DOI] [PubMed] [Google Scholar]
- Klekner A, Bágyi K, Bognár L, Gáspár A, Andrási M, Szabó J. Effectiveness of cephalosporins in the sputum of patients with nosocomial bronchopneumonia. J Clin Microbiol. 2006;44:3418–3421. doi: 10.1128/JCM.00893-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boselli E, Breilh D, Duflo F, Saux MC, Debon R, Chassard D, Allaouchiche B. Steady-state plasma and intrapulmonary concentrations of cefepime administered in continuous infusion in critically ill patients with severe nosocomial pneumonia. Crit Care Med. 2003;31:2102–2106. doi: 10.1097/01.CCM.0000069734.38738.C8. [DOI] [PubMed] [Google Scholar]
- Rondanelli R, Dionigi RV, Regazzi MB, Maurelli M, Calvi M, Mapelli A. Ceftazidime in the treatment of Pseudomonas infections in intensive-care patients. Int J Clin Pharmacol Ther Toxicol. 1986;24:457–459. [PubMed] [Google Scholar]
- Young RJ, Lipman J, Gin T, Gomersall CD, Joynt GM, Oh TE. Intermittent bolus dosing of ceftazidime in critically ill patients. J Antimicrob Chemother. 1997;40:269–273. doi: 10.1093/jac/40.2.269. [DOI] [PubMed] [Google Scholar]
- Gómez CM, Cordingly JJ, Palazzo MG. Altered pharmacokinetics of ceftazidime in critically ill patients. Antimicrob Agents Chemother. 1999;43:1798–1802. doi: 10.1128/aac.43.7.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benko AS, Cappelletty DM, Kruse JA, Rybak MJ. Continuous infusion versus intermittent administration of ceftazidime in critically ill patients with suspected gram-negative infections. Antimicrob Agents Chemother. 1996;40:691–695. doi: 10.1128/aac.40.3.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipman J, Gomersall CD, Gin T, Joynt GM, Young RJ. Continuous infusion ceftazidime in intensive care: a randomized controlled trial. J Antimicrob Chemother. 1999;43:309–311. doi: 10.1093/jac/43.2.309. [DOI] [PubMed] [Google Scholar]
- Boselli E, Breilh D, Rimmelé T, Poupelin JC, Saux MC, Chassard D, Allaouchiche B. Plasma and lung concentrations of ceftazidime administered in continuous infusion to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004;30:989–991. doi: 10.1007/s00134-004-2171-2. [DOI] [PubMed] [Google Scholar]
- Hanes SD, Wood GC, Herring V, Croce MA, Fabian TC, Pritchard E, Boucher BA. Intermittent and continuous ceftazidime infusion for critically ill trauma patients. Am J Surg. 2000;179:436–440. doi: 10.1016/S0002-9610(00)00388-3. [DOI] [PubMed] [Google Scholar]
- Angus BJ, Smith MD, Suputtamongkol Y, Mattie H, Walsh AL, Wuthiekanun V, Chaowagul W, White NJ. Pharmacokinetic-pharmacodynamic evaluation of ceftazidime continuous infusion vs intermittent bolus injection in septicaemic melioidosis. Br J Clin Pharmacol. 2000;50:184–191. doi: 10.1111/j.1365-2125.2000.00179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aubert G, Carricajo A, Coudrot M, Guyomarc'h S, Auboyer C, Zeni F. Prospective determination of serum ceftazidime concentrations in intensive care units. Ther Drug Monit. 2010;32:517–519. doi: 10.1097/FTD.0b013e3181e60ca6. [DOI] [PubMed] [Google Scholar]
- Georges B, Conil JM, Seguin T, Ruiz S, Minville V, Cougot P, Decun JF, Gonzalez H, Houin G, Fourcade O, Saivin S. Population pharmacokinetics of ceftazidime in intensive care unit patients: influence of glomerular filtration rate, mechanical ventilation, and reason for admission. Antimicrob Agents Chemother. 2009;53:4483–4489. doi: 10.1128/AAC.00430-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buijk SL, Gyssens IC, Mouton JW, Van Vliet A, Verbrugh HA, Bruining HA. Pharmacokinetics of ceftazidime in serum and peritoneal exudate during continuous versus intermittent administration to patients with severe intra-abdominal infections. J Antimicrob Chemother. 2002;49:121–128. doi: 10.1093/jac/49.1.121. [DOI] [PubMed] [Google Scholar]
- Mouton JW, Punt N, Vinks AA. A retrospective analysis using Monte Carlo simulation to evaluate recommended ceftazidime dosing regimens in healthy volunteers, patients with cystic fibrosis, and patients in the intensive care unit. Clin Ther. 2005;27:762–772. doi: 10.1016/j.clinthera.2005.06.013. [DOI] [PubMed] [Google Scholar]
- Langer M, Cantoni P, Bellosta C, Boccazzi A. Penetration of ceftazidime into bronchial secretions in critically ill patients. J Antimicrob Chemother. 1991;28:925–932. doi: 10.1093/jac/28.6.925. [DOI] [PubMed] [Google Scholar]
- Bressolle F, de La Coussaye JE, Ayoub R, Fabre D, Gomeni R, Saissi G, Eledjam JJ, Galtier M. Endotracheal and aerosol administrations of ceftazidime in patients with nosocomial pneumonia: pharmacokinetics and absolute bioavailability. Antimicrob Agents Chemother. 1992;36:1404–1411. doi: 10.1128/aac.36.7.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridkin SK, Steward CD, Edwards JR, Pryor ER, McGowan JE Jr, Archibald LK, Gaynes RP, Tenover FC. Project Intensive Care Antimicrobial Resistance Epidemiology (ICARE) Hospitals. Surveillance of antimicrobial use and antimicrobial resistance in United States hospitals: Project ICARE Phase 2. Clin Infect Dis. 1999;29:245–252. doi: 10.1086/520193. [DOI] [PubMed] [Google Scholar]
- Chatellier D, Jourdain M, Mangalaboyi J, Ader F, Chopin C, Derambure P, Fourrier F. Cefepime-induced neurotoxicity: an underestimated complication of antibiotherapy in patients with acute renal failure. Intensive Care Med. 2002;28:214–217. doi: 10.1007/s00134-001-1170-9. [DOI] [PubMed] [Google Scholar]
- Roberts JA, Ulldemolins M, Roberts MS, McWhinney B, Ungerer J, Paterson DL, Lipman J. Therapeutic drug monitoring of β-lactams in critically ill patients: proof of concept. Int J Antimicrob Agents. 2010;36:332–339. doi: 10.1016/j.ijantimicag.2010.06.008. [DOI] [PubMed] [Google Scholar]
- Nicasio AM, Eagye KJ, Nicolau DP, Shore E, Palter M, Pepe J, Kuti JL. Pharmacodynamic-based clinical pathway for empiric antibiotic choice in patients with ventilator-associated pneumonia. J Crit Care. 2010;25:69–77. doi: 10.1016/j.jcrc.2009.02.014. [DOI] [PubMed] [Google Scholar]
- McKinnon PS, Paladino JA, Schentag JJ. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T > MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents. 2008;31:345–351. doi: 10.1016/j.ijantimicag.2007.12.009. [DOI] [PubMed] [Google Scholar]
- Gentry LO, Rodriguez-Gomez G. Randomized comparison of cefepime and ceftazidime for treatment of skin, surgical wound, and complicated urinary tract infections in hospitalized subjects. Antimicrob Agents Chemother. 1991;35:2371–2374. doi: 10.1128/aac.35.11.2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariano RE, Nyhlén A, Donnelly JP, Sitar DS, Harding GK, Zelenitsky SA. Pharmacokinetics and pharmacodynamics of meropenem in febrile neutropenic patients with bacteremia. Ann Pharmacother. 2005;39:32–38. doi: 10.1345/aph.1E271. [DOI] [PubMed] [Google Scholar]
- Mouton JW, Vinks AA, Punt NC. Pharmacokinetic-pharmacodynamic modeling of activity of ceftazidime during continuous and intermittent infusion. Antimicrob Agents Chemother. 1997;41:733–738. doi: 10.1128/aac.41.4.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolau DP. Pharmacodynamic optimization of β-lactams in the patient care setting. Crit Care. 2008;12:S2. doi: 10.1186/cc6818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasiakou SK, Sermaides GJ, Michalopoulos A, Soteriades ES, Falagas ME. Continuous versus intermittent intravenous administration of antibiotics: a meta-analysis of randomised controlled trials. Lancet Infect Dis. 2005;5:581–589. doi: 10.1016/S1473-3099(05)70218-8. [DOI] [PubMed] [Google Scholar]
- Roberts JA, Webb S, Paterson D, Ho KM, Lipman J. A systematic review on clinical benefits of continuous administration of β-lactam antibiotics. Crit Care Med. 2009;37:2071–2078. doi: 10.1097/CCM.0b013e3181a0054d. [DOI] [PubMed] [Google Scholar]
- Ljungberg B, Nilsson-Ehle I. Pharmacokinetics of meropenem and its metabolite in young and elderly healthy men. Antimicrob Agents Chemother. 1992;36:1437–1440. doi: 10.1128/aac.36.7.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drusano GL, Standiford HC, Bustamante C, Forrest A, Rivera G, Leslie J, Tatem B, Delaportas D, MacGregor RR, Schimpff SC. Multiple-dose pharmacokinetics of imipenem-cilastatin. Antimicrob Agents Chemother. 1984;26:715–721. doi: 10.1128/aac.26.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradis D, Vallée F, Allard S, Bisson C, Daviau N, Drapeau C, Auger F, LeBel M. Comparative study of pharmacokinetics and serum bactericidal activities of cefpirome, ceftazidime, ceftriaxone, imipenem, and ciprofloxacin. Antimicrob Agents Chemother. 1992;36:2085–2092. doi: 10.1128/aac.36.10.2085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbhaiya RH, Forgue ST, Gleason CR, Knupp CA, Pittman KA, Weidler DJ, Movahhed H, Tenney J, Martin RR. Pharmacokinetics of cefepime after single and multiple intravenous administrations in healthy subjects. Antimicrob Agents Chemother. 1992;36:552–557. doi: 10.1128/aac.36.3.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson-Saunders B, Trapp RG. Basic & Clinical Biostatistics. 2. Chicago: Appleton & Lange; 1994. [Google Scholar]